Abstract
Background/Aims:
Metal stent insertion is a common palliative treatment for distal malignant biliary obstruction (MBO) but whether placement across the sphincter of Oddi (SO) causes more complications or shorter survival is in question. The aim of this study was to compare the clinical outcomes of percutaneous uncovered self-expandable metal stent placement above and across the SO in patients with distal MBO.
Patients and Methods:
We retrospectively studied 59 patients who underwent uncovered metal stent placement for distal MBO between January 2012 and March 2016. Stents were placed above the SO for 22 subjects (group A) and across the SO for 37 subjects (group B). Early cholangitis, stent occlusion, and overall survival time were compared between the two groups.
Results:
Clinical success was 90.9 and 86.5% for groups A and B, respectively. Early cholangitis occurred in 2 patients (9.1%) in group A and in 6 patients (16.2%) in group B (P = 0.645). Median stent patency and median survival time was 105 and 140 days for group A, 120 and 160 days for group B, respectively. The stent occlusion (31.8% in group A and 21.6% in group B, P = 0.454) and the cumulative stent patency times (P = 0.886) did not differ between the two groups. There was no significant difference in cumulative patient survival between the two groups (P = 0.810).
Conclusion:
Uncovered metal stent placement across the SO did not significantly affect early cholangitis, stent patency, or patient survival.
Keywords: Distal biliary obstruction, metal stent, outcome, sphincter of Oddi
INTRODUCTION
Patients with distal malignant biliary obstruction (MBO) usually have no curative therapy available, so a self-expandable, uncovered metal stent is offered as palliative treatment for biliary decompression. The stent can help with symptom regression and improvements in quality of life.[1,2,3,4] The anti-reflux capacity of the sphincter is thought to be sacrificed if the stent is placed across the sphincter of Oddi (SO).[5,6] Currently, concerns exist over whether stent placement above SO causes more early cholangitis, stent occlusion, or reduced survival. Studies to compare efficiency of placement to treat MBO [6,7,8,9,10,11] have not been conclusive with regard to impaired SO function and resulting cholangitis.[5,12]
Many variables can influence patient outcomes: tumor type; stent type; and percutaneous or endoscopic approaches, especially the biliary stricture level. Endoscopic techniques may increase early infection due to retrograde passage through papillary route with or without sphincterectomy.[5] At the biliary stricture level, patients with biliary strictures shorter than 2 cm from the papillary mound were likely to be treated with a transpapillary approach. Those with hilar strictures were treated with a suprapapillary method.[6,8,13,14] Study data so far cannot be easily compared, so no conclusion exists to suggest the optimal stent placement, especially for those with distal biliary obstruction ≥2 cm from the SO.[5,7]
Thus, we retrospectively assessed clinical outcomes of percutaneous transhepatic uncovered metal stent placement above or across the SO for treating distal MBO.
PATIENTS AND METHODS
Study procedures followed the guidelines of the World Medical Association Declaration of Helsinki and were approved by the Ethics Committee of our institution. For this retrospective study, formal consent was not required.
Patients
From January 2012 to March 2016, percutaneous transhepatic metal stents were placed in 368 patients with MBO at our institution. We excluded patients with previous biliary tract surgery, hilar lesions, bile duct obstruction <2 cm proximal to the papilla, patients who had double metal stents, Eastern Cooperation Oncology Group (ECOG) Scale of Performance Status grade 3 or 4, or patients lost to follow-up. Ultimately, 59 patients were included in the study.
According to the location of the distal end of the stent, patients were divided into two groups. In group A (n = 22), the distal end of the stent was above the SO. In group B (n = 37), the distal end of the stent protruded into the duodenum. Case diagnosis was based on laboratory and radiology results, with or without pathological findings. Of these 59 patients, 41 patients were diagnosed based on pathological results, and 18 patients were diagnosed by laboratory or imaging findings and history of disease progression. Patient clinical data from medical records and telephone follow-up were collected retrospectively from the time of procedure until death or last follow up visit.
Stent placement
Before stent insertion, contrast-enhanced abdominal computed tomography (CT) and/or magnetic resonance imaging (MRI) were performed. Antibiotics were given to the patients who had infectious symptoms and adjusted according to cultured blood data.
Percutaneous transhepatic stent placement was performed under fluoroscopic guidance. If there were no combined infections or hemobilia during percutaneous transhepatic biliary drainage (PTBD) procedure, the stent was inserted at the same time. If the patient suffered from infection or hemobilia, external drainage was performed 2–7 days before stent insertion. When a cholangiogram was obtained, the length of the stricture and the distance from the end of the stricture to the papilla were measured. The stent was chosen according to the length of the stricture and then deployed across the obstructed segment. A space was left at the end of the proximal and distal margins of the obstructed segment to prevent tumor overgrowth. Besides, an external drainage catheter was placed in some cases to check stent function after stent placement. Uncovered stents used were E-Luminexx stents (Bard, Karlsruhe, Germany), 8 mm in diameter, and 6 or 8 cm in length.
Study definitions and follow-up
Major study endpoints included evaluation of early cholangitis, stent patency, and survival. Early cholangitis was diagnosed when a fever >38°C continued >24 h with cholestasis and leukocytosis observed within 30 days after stent insertion. Stent dysfunction was defined as recurrent jaundice, increased serum bilirubin, and/or biliary dilation observed on imaging findings.[15] Stent patency was defined as duration from initial stent placement to recurrent jaundice. If recurrent jaundice was not observed during a patient's life, stent patency was considered equal to the survival time. Survival time was defined as duration from initial stent placement to death or the last follow up visit. Clinical success was defined as decreased serum bilirubin to <75% of pretreatment values within 1 month after stent placement.[16] Complications were considered major or minor according to guidelines of the Society of Interventional Radiology Standards of Practice Committee.[17]
Patients were followed at outpatient clinics and advised to report to the hospital if fever or jaundice developed. In patients presenting with recurrent jaundice, blood tests and enhanced abdominal CT scanning were performed. When stent dysfunction was detected, PTBD was performed if possible. All patients were followed until August 31, 2016.
Statistical analysis
Quantitative data are presented as means ± standard deviation (SD) and comparisons were analyzed using a χ2- test or a Student's t-test. Cumulative stent patency and patient survival were calculated using the Kaplan-Meier method. A log-rank test was used to compare stent patency and patient survival between groups. Statistical analysis was performed with Statistical Package for the Social Sciences (version 19.0, Chicago, IL) and P value <0.05 was considered statistically significant.
RESULTS
Procedure outcomes
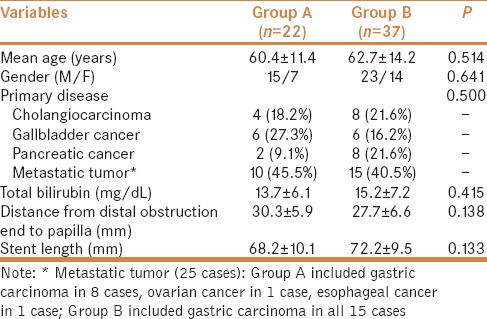
Clinical characteristics of patients are summarized in Table 1. There were no significant differences in gender, age, initial serum bilirubin, primary disease, and distance from distal obstruction to papilla or length of stent between groups. Clinical success was achieved in 20 patients in group A and 32 patients in group B. Serum bilirubin increased in 1 person in group B and cholangiogram confirmed sludge in the stent so that contrast medium could not easily pass through the bile duct. For this case, a reserved external catheter was opened for external drainage. Two patients who did not have clinical success died one month later after initial stent insertion. For 4 other four patients, no further interventions were required. No procedure-related deaths occurred in this cohort.
Table 1.
Patient clinical characteristics in two groups
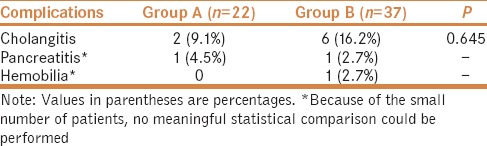
Complications
Self-limiting hemobilia occurred in one patient in group B, and pancreatitis occurred in two patients in each group. Early cholangitis was observed in 8 cases (2 in group A; 6 in group B). All subjects recovered after conservative treatment for 5–7 days. There was no statistically significant difference between the groups for cholangitis (P = 0.645) [Table 2].
Table 2.
Comparison of complications between two groups
Stent patency and patient survival
Stent occlusion occurred in seven patients in group A and eight in group B, but there was no statistically significant difference (P = 0.561). Cumulative median stent patency was 105 days for group A and 120 days for group B. Kaplan-Meier analysis showed no significant difference in the two groups (P = 0.886). Seven patients with recurrent jaundice in group A underwent external drainage and of the 8 patients in group B, only 5 patients had external drainage.
At 3, 6, and 12 months, the cumulative survival rates were 72.2, 31.8, and 4.5%, respectively, in group A; for group B, the cumulative survival rates were 67.6, 37.8, and 8.1%, respectively, at those similar time points. Median survival for group A subjects was 140 days and for group B, it was 160 days and these numbers were not statistically significant (P = 0.810) [Figure 1].
Figure 1.
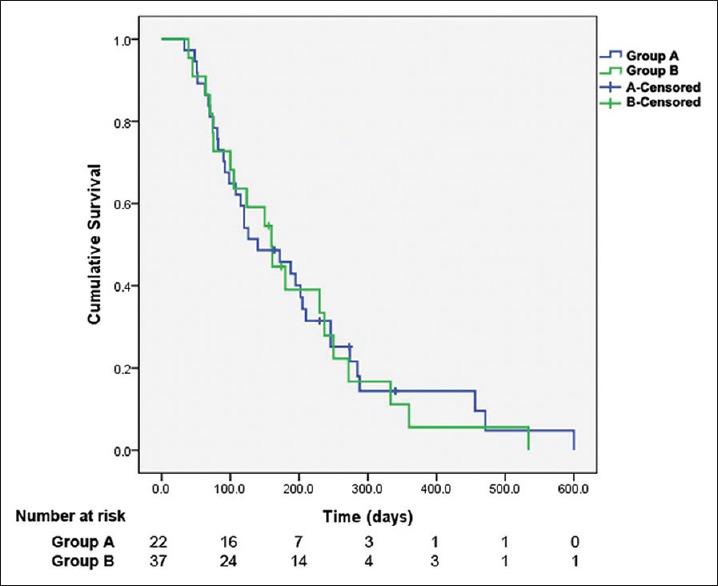
Kaplan-Meier analysis of overall survivals in two groups. Median survival after placing the stent above the SO was 140 days and for placing the stent across the SO was 160 days. There was no significant difference in cumulative patient survival between groups (P = 0.810)
DISCUSSION
For patients with distal common bile duct obstruction, insertion of a metal stent above or across the SO is controversial. In this study, the distance between the distal end of the stricture and the duodenal papilla was initially marked and comparable (without a statistically significant difference) between the 2 groups. The results suggested that uncovered metal stent insertion above and across the SO offered similar safety and limited early cholangitis. Stent patency and patient survival were also similar irrespective of the position.
Patient survival is dependent on tumor type, metastasis, and eventual comorbidities. There was no statistically significant difference between primary diseases in either group. Overall survival at 3, 6, and 12 months was similar. These data agreed with published reports that palliative stent placement could alleviate obstructive jaundice, without remarkably influencing patient survival and that stent location did not seem to matter.[6,8] For patients with a life expectancy equal to or less than 3 months, transpapillary stenting may also be recommended to reduce postprocedural morbidity.[18]
The incidence of stent dysfunction for patients with MBO was reported in 15 - 31% following placement of uncovered metal stents [8,19] and this is largely due to tumor ingrowth through the mesh.[20,21] Given that tissue ingrowth was the major cause of stent dysfunction and clogging only modestly contributes to stent dysfunction,[19,22,23] stent insertion location did not affect stent patency. Metal stent placement across the SO did not increase stent occlusion or shorten patency time compared with metal stent placement above the SO.[8] In our study, stent occlusion was 31.8 and 21.6% for groups A and B, respectively, and these data were consistent with previous studies.[8,19]
Cholangitis limits the efficacy of metal stent placement for alleviating distal biliary obstruction [12] and frequent early cholangitis is reported to occur after the insertion of a transpapillary metallic stent.[5,6] It is thought that either the content reflux back from the duodenum or a poorly functioning stent is an important etiologic factor for cholangitis. In contrast, we found no significant difference in early cholangitis after stent insertion between the two groups. According to the previous study, reflux of duodenal content was a universal phenomenon after stent placement across the main duodenal papilla but no features of acute cholangitis developed due to reflux.[24] In fact, for most subjects, placing a stent across the SO did not cause early cholangitis when the bile was drained easily.[7,25] Cholangitis was mostly caused by impairment of bile flow and subsequent bacterial overgrowth. Recent studies suggest that stent-related cholangitis after transpapillary stent insertion is uncommon.[8] From our experience and previous studies, relief of jaundice after stent insertion improves liver function and assists resistance against pathogens; cholangitis was not a problem for most patients who underwent stent insertion across the SO for MBO.[24,26]
The study was limited in that it was retrospective and thus had some inevitable bias. Also, we did not analyze the causes of stent dysfunction due to difficulty of distinguishing stent clogging or tumor growth. In addition, percutaneous external drainage prior to stent insertion was performed in 18 patients (30.5%) in the current study, which may change clinical outcomes, even though data show that stent placement with or without preoperative biliary drainage did not significantly affect therapeutic success, major complications, or stent patency.[27] However, these results are limited by the small sample size. Further randomized controlled studies with larger sample size is needed to confirm these findings.
CONCLUSION
In conclusion, insertion of an uncovered metal stent across the SO was as safe and effective as SO functional preservation for patients with distal MBO. Early cholangitis, stent patency, and survival after uncovered metal stent insertion across the SO are comparable to outcomes with stent insertion above the SO.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schoder M, Rossi P, Uflacker R, Bezzi M, Stadler A, Funovics MA, et al. Malignant biliary obstruction: Treatment with ePTFE-FEP- covered endoprostheses initial technical and clinical experiences in a multicenter trial. Radiology. 2002;225:35–42. doi: 10.1148/radiol.2251011744. [DOI] [PubMed] [Google Scholar]
- 2.Han YH, Kim MY, Kim SY, Kim YH, Hwang YJ, Seo JW, et al. Percutaneous insertion of Zilver stent in malignant biliary obstruction. Abdom Imaging. 2006;31:433–8. doi: 10.1007/s00261-005-8017-8. [DOI] [PubMed] [Google Scholar]
- 3.van Delden OM, Lameris JS. Percutaneous drainage and stenting for palliation of malignant bile duct obstruction. Eur Radiol. 2008;18:448–56. doi: 10.1007/s00330-007-0796-6. [DOI] [PubMed] [Google Scholar]
- 4.Choe JW, Hyun JJ. Is there room for improvement in increasing the stent patency of biliary plastic stents? Gut Liver. 2016;10:499–501. doi: 10.5009/gnl16251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okamoto T, Fujioka S, Yanagisawa S, Yanaga K, Kakutani H, Tajiri H, et al. Placement of a metallic stent across the main duodenal papilla may predispose to cholangitis. Gastrointest Endosc. 2006;63:792–6. doi: 10.1016/j.gie.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Huang X, Shen L, Jin Y, Chen L, Zhou D, Xu G, et al. Comparison of uncovered stent placement across versus above the main duodenal papilla for malignant biliary obstruction. J Vasc Interv Radiol. 2015;26:432–7. doi: 10.1016/j.jvir.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Li SY, Kim CW, Jeon UB, Lee NK, Kim S, Kang DH, et al. Early infectious complications of percutaneous metallic stent insertion for malignant biliary obstruction. AJR Am J Roentgenol. 2010;194:261–5. doi: 10.2214/AJR.09.2474. [DOI] [PubMed] [Google Scholar]
- 8.Jo JH, Park BH. Suprapapillary versus transpapillary stent placement for malignant biliary obstruction: Which is better. J Vasc Interv Radiol. 2015;26:573–82. doi: 10.1016/j.jvir.2014.11.043. [DOI] [PubMed] [Google Scholar]
- 9.Pedersen FM, Lassen AT, de Muckadell OBS. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest Endosc. 1998;48:574–9. doi: 10.1016/s0016-5107(98)70038-0. [DOI] [PubMed] [Google Scholar]
- 10.Uchida N, Tsutsui K, Ezaki T, Fukuma H, Kamata H, Kobara H, et al. Estimation of the stent placement above the intact sphincter of Oddi against malignant bile duct obstruction. J Gastroenterol. 2005;40:291–6. doi: 10.1007/s00535-004-1535-2. [DOI] [PubMed] [Google Scholar]
- 11.Cosgrove N, Siddiqui AA, Adler DG, Shahid H, Sarkar A, Sharma A, et al. A comparison of bilateral side-by-side metal stents deployed above and across the sphincter of Oddi in the management of malignant hilar biliary obstruction. J Clin Gastroenterol. 2017;51:528–33. doi: 10.1097/MCG.0000000000000584. [DOI] [PubMed] [Google Scholar]
- 12.Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, Nakai Y, et al. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: A randomized multicenter trial. Am J Gastroenterol. 2013;108:1713–22. doi: 10.1038/ajg.2013.305. [DOI] [PubMed] [Google Scholar]
- 13.Gwon DI, Ko GY, Kim JH, Yoon HK, Lee IS, Kim KA, et al. A comparative analysis of PTFE-covered and uncovered stents for palliative treatment of malignant extrahepatic biliary obstruction. AJR Am J Roentgenol. 2010;195:W463–9. doi: 10.2214/AJR.10.4658. [DOI] [PubMed] [Google Scholar]
- 14.Kim JW, Gwon D, Han YM, Won JH, Hong HP, Ko GY, et al. A prospective, multicenter study of a double stent system for palliative treatment of malignant extrahepatic biliary obstructions. Acta Radiol. 2015;56:1209–15. doi: 10.1177/0284185114550702. [DOI] [PubMed] [Google Scholar]
- 15.Isayama H, Hamada T, Yasuda I, Itoi T, Ryozawa S, Nakai Y, et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27:259–64. doi: 10.1111/den.12379. [DOI] [PubMed] [Google Scholar]
- 16.Gwon DI, Ko GY, Sung KB, Yoon HK, Shin JH, Kim JH, et al. A novel double stent system for palliative treatment of malignant extrahepatic biliary obstructions: A pilot study. AJR Am J Roentgenol. 2011;197:W942–7. doi: 10.2214/AJR.11.6813. [DOI] [PubMed] [Google Scholar]
- 17.Cardella JF, Kundu S, Miller DL, Millward SF, Sacks D. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2009;20:S189–91. doi: 10.1016/j.jvir.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 18.Hatzidakis AA, Tsetis D, Chrysou E, Sanidas E, Petrakis J, Gourtsoyiannis NC. Nitinol stents for palliative treatment of malignant obstructive jaundice: Should we stent the sphincter of Oddi in every case. Cardiovasc Intervent Radiol. 2001;24:245–8. doi: 10.1007/s00270-001-0030-x. [DOI] [PubMed] [Google Scholar]
- 19.Dumonceau JM, Tringali A, Blero D, Deviere J, Laugiers R, Heresbach D, et al. Biliary stenting: Indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277–98. doi: 10.1055/s-0031-1291633. [DOI] [PubMed] [Google Scholar]
- 20.Cho JH, Jeon TJ, Park JY, Kim HM, Kim YJ, Park SW, et al. Comparison of outcomes among secondary covered metallic, uncovered metallic, and plastic biliary stents in treating occluded primary metallic stents in malignant distal biliary obstruction. Surg Endosc. 2011;25:475–82. doi: 10.1007/s00464-010-1196-6. [DOI] [PubMed] [Google Scholar]
- 21.Lee HJ, Chung MJ, Park JY, Park SW, Nam CM, Song SY, et al. A prospective randomized study for efficacy of an uncovered double bare metal stent compared to a single bare metal stent in malignant biliary obstruction. Surg Endosc. 2017;31:3159–67. doi: 10.1007/s00464-016-5341-8. [DOI] [PubMed] [Google Scholar]
- 22.Kullman E, Frozanpor F, Soderlund C, Linder S, Sandstrom P, Lindhoff-Larsson A, et al. Covered versus uncovered self-expandable nitinol stents in the palliative treatment of malignant distal biliary obstruction: Results from a randomized, multicenter study. Gastrointest Endosc. 2010;72:915–23. doi: 10.1016/j.gie.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Krishna SG, Singh A, Ladha HS, Slack RS, Ramireddy S, et al. Comparison of the utility of covered metal stents versus uncovered metal stents in the management of malignant biliary strictures in 749 patients. Gastrointest Endosc. 2013;78:312–24. doi: 10.1016/j.gie.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 24.Misra SP, Dwivedi M. Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest Endosc. 2009;70:317–21. doi: 10.1016/j.gie.2008.12.054. [DOI] [PubMed] [Google Scholar]
- 25.Lee DH, Yu JS, Hwang JC, Kim KH. Percutaneous placement of self-expandable metallic biliary stents in malignant extrahepatic strictures: Indications of transpapillary and suprapapillary methods. Korean J Radiol. 2000;1:65–72. doi: 10.3348/kjr.2000.1.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamada T, Isayama H, Nakai Y, Togawa O, Takahara N, Uchino R, et al. Antireflux metal stent as a first-line metal stent for distal malignant biliary obstruction: A pilot study. Gut Liver. 2017;11:142–8. doi: 10.5009/gnl15579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li M, Bai M, Qi X, Li K, Yin Z, Wang J, et al. Percutaneous transhepatic biliary metal stent for malignant hilar obstruction: Results and predictive factors for efficacy in 159 patients from a single center. Cardiovasc Intervent Radiol. 2015;38:709–21. doi: 10.1007/s00270-014-0992-0. [DOI] [PubMed] [Google Scholar]


