Short abstract
Objectives
The aim of this network meta-analysis is to assess the effectiveness of therapeutic strategies for patients with radiculopathy, including physical, medical, surgical, and other therapies.
Methods
We electronically searched electronic databases including PubMed and Embase for randomized controlled trials. The response rate and visual analog scale of pain change were considered as primary outcomes. The outcomes were measured by odds ratio (OR) value and corresponding 95% credible intervals (CrIs) or standardized mean difference (MD) with 95% CrIs. Besides, surface under cumulative ranking curve (SUCRA) were performed to rank efficacy and safety of treatments on each end points.
Results
A total of 16 eligible studies with 1071 subjects were included in this analysis. Our results showed that corticosteroid was significantly more effective than control regarding the response rate (OR = 3.86, 95% CrI: 1.16, 12.55). Surgery had a better performance in pain change compared with control (MD = −1.92, 95% CrI: −3.58, −0.15). According to the SUCRA results, corticosteroid, collar, and physiotherapy ranked the highest concerning response rate (SUCRA = 0.656, 0.652, and 0.610, respectively). Surgery, traction, and corticosteroid were superior to others in pain change (SUCRA = 0.866, 0.748, and 0.589, respectively).
Conclusion
According to the network meta-analysis result, we recommended surgery as the optimal treatment for radiculopathy patients; traction and corticosteroids were also recommended for their beneficial interventions.
Keywords: Radiculopathy, treatment, response rate, pain change, network meta-analysis
Introduction
Radiculopathy is a set of neuropathic conditions caused by compressed nerves in the spine at or near the level of the nerve root.1 The location of radiculopathy occurrence depends on which nerve root is affected.2 Common symptoms of radiculopathy include radicular pain, numbness, tingling, and weakness in the muscles.3 Cervical and lumbar radiculopathy can be induced by factors such as disc herniation, bone spurs, trauma, osteoarthritis, inflammation, and tumor or diabetes in some rare cases.4,5 Important risk factors associated with the incidence of radiculopathy include aging, race and hereditary factors, poor posture, and spinal abnormalities.6 Some studies have also shown that occupation is related to radiculopathy, for example, one study states that people involved in heavy labor, sports, or military service are more likely to develop radiculopathy than those who live a sedentary lifestyle.7 The prevalence of lumbar radiculopathy was 3% to 5%8 while cervical radiculopathy showed an incidence of 83.2 per 100,000 persons annually.9
Lumbar and cervical radiculopathy can be diagnosed through physical examination, imaging, and electrodiagnostics.10,11 Most patients with radiculopathy respond well to non-surgical, conservative treatment such as medication (corticosteroids, non-steroidal anti-inflammatory, tricyclic antidepressants, analgesics, and muscle relaxants), physical therapy, chiropractic treatment, spinal manipulation, traction, and corticosteroid injections.10 The injection of corticosteroids into various structures in and around the spine is a common procedure used to reduce inflammation and lower back pain;12 75% to 90% of patients’ symptoms are improved after non-operative care. However, for patients with persistent pain or severe functional deficit, surgical options are necessary and more beneficial when the pathology has been clearly identified.13 In clinical practice, several procedures are usually adopted by surgeons, such as anterior and posterior decompression, anterior cervical discectomy, laminectomy, and minotomy.14
Despite various kinds of non-surgical and surgical therapies were widely used for patients with radiculopathy, the relative efficacy of each treatment option was still unclear. One of the main causes was the deficiency of multiple-arm comparisons in clinical trials. Although a few meta-analyses have been published, the results from different studies for the same comparators have demonstrated controversial and contradictory results. Therefore, there was no recognized conclusion that has been obtained with respect to efficacy of these treatments. Moreover, currently published studies mainly focus on pairwise comparisons. Thus, it was more difficult for clinical practitioners to comprehensively integrate all of the evidence regarding all therapies and make the ideal choice. Our group conducted the first network meta-analysis (NMA) that synthesized the data from eligible randomized controlled trials (RCTs) in order to overcome the abovementioned shortages. We intended to illustrate the effectiveness of different strategies in radiculopathy treatment and provide more comprehensive and authentic evidence for the selection of treatments.
Methods
Search strategy and literature selection criteria
Two independent reviewers conducted the literature selection by searching electronic databases (PubMed and Embase). They restricted the search standard to articles published in English. The key search term was “radiculopathy,” and other subordinate entry terms (such as “cervical radiculopathy” and “lumbosacral radicular syndrome”) as well as different treatment strategies (corticosteroid, collar, physiotherapy, traction, surgery, serotonin, non-steroidal anti-inflammatory drugs, chemonucleolysis, and pulsed radiofrequency) were also included in the search query. All search terms were searched with Boolean operators AND or OR. Conference proceedings, bibliographies of the identified articles, and registries of clinical trials were not considered during searching progress.
The inclusion criteria of RCTs were (1) RCTs evaluating the efficacy of two or more different treatment therapies for radiculopathy patients, (2) RCTs with post-therapy response rates or changes in pain score as the outcome measurements, and (3) patients diagnosed with radiculopathy. (1) Studies that do not have relevant outcomes and (2) conferences or unpublished studies were excluded. The eligibility of papers retrieved was checked by two experienced reviewers independently. Any disagreements between the two reviewers would reach unanimity through consultation. If certain disagreements still remained, a third reviewer would be asked to intervene.
Data extraction
The characteristics and data were extracted from all 16 included studies. The following contents were considered in data extraction: (1) baseline characteristics of each study, including author, published year, blind condition, and study size; (2) basic patient information, including age and gender; (3) interventions in study and control groups; and (4) outcome data including the binary variable response rate and continuous variable pain score change.
Statistical analysis
Meta-analysis has been utilized to pool data from clinical trials and calculate estimates of drug efficacy.15 Yet medical professionals may face more than one option when making decisions and pairwise comparisons might not be enough to figure out which treatment is more effective. Hence, NMA would be a wise choice when related regimens have not been compared directly. By combining direct and indirect evidence in clinical trials, NMA could execute evidence synthesis.16
Two outcomes, response rate and pain score change, were considered to be equally vital in the systematic data analysis. Response rate was evaluated using odds ratio (OR) with 95% confidence intervals (CIs) in direct pairwise comparisons, which were generated using random-effects model. Further standardization of pain scores was conducted before data processing to explain variations in the evaluation scales accepted by individual studies. After standardization, a standard mean difference was computed on the comparisons. Data analyses were processed using STATA 13.0 and R 3.2.3 software; 95% credible intervals of outcomes were calculated in NMA. Pairwise comparisons from NMA were further presented visually using forest plots. The consistency between direct and indirect comparisons was evaluated using node-splitting results and heat plots (blue color represents higher inconsistency). In this case, p value < 0.05 was considered as a significant inconsistency. Furthermore, surface under cumulative ranking curve (SUCRA) was used to represent and evaluate the relative rank of each treatment under different outcomes.
Results
Selection and baseline information of included studies and network structure
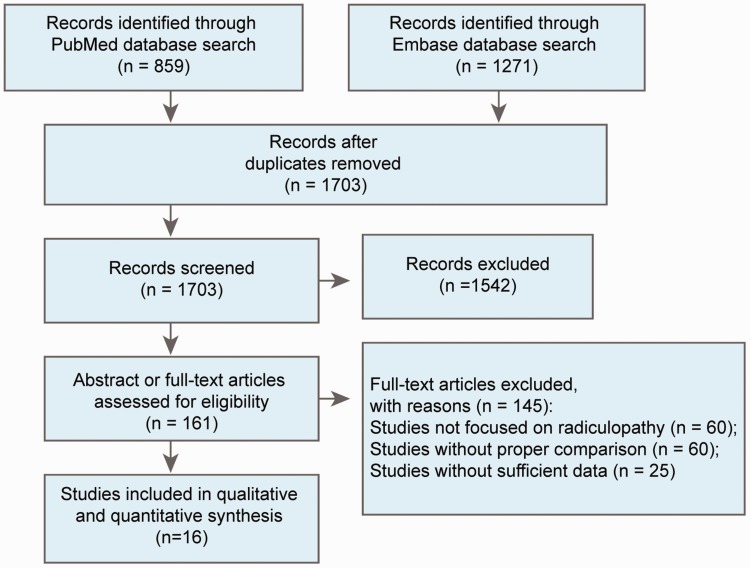
The PRISMA flow diagram in Figure 1 illustrates the literature selection process. Two independent reviewers identified a total of 1703 eligible studies, which were selected for further screening. Of these, 161 studies were selected for abstract or full-text assessment, which ensured that irrelevant and insufficient articles were discarded. Finally, 16 studies were selected for data extraction and statistical analysis.17–32
Figure 1.
PRISMA flow diagram.
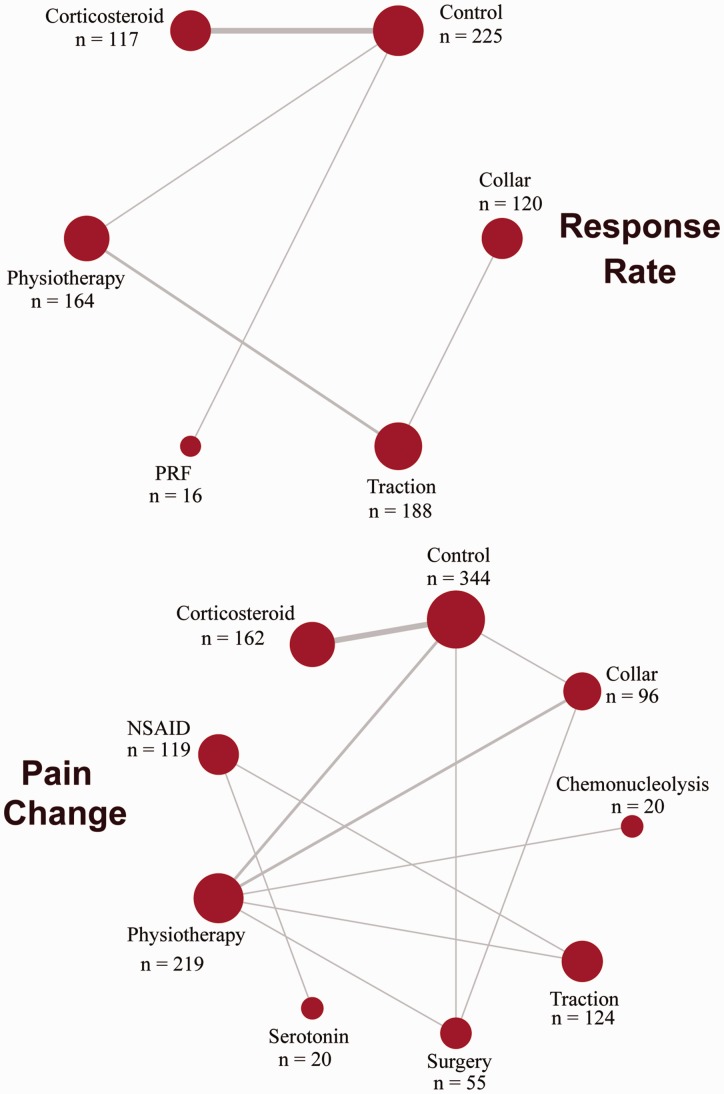
Basic information from the 16 included studies was organized and displayed in Table 1. The studies were published between 1966 and 2014. The outcome of response rate was included in 8 of these studies, and the outcome of pain score was included in 12 of these studies. Therapies in all studies included corticosteroid, collar, physiotherapy, traction, surgery, serotonin, non-steroidal anti-inflammatory drugs, chemonucleolysis, pulsed radiofrequency, and control. All the treatments and their direct comparisons formed the networks as shown in Figure 2. Each node represented a different treatment, and the size of node corresponded to the number of patients studied with respect to the treatment represented. The lines between two nodes indicated the existence of direct evidence. Jadad scale for the 16 included studies is shown in Table S1.
Table 1.
Basic characteristics of included studies.
| Author(s) | Year | Blinding |
Intervention 1 |
Intervention 2 |
Outcomes |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | Mean age | Male | Size | Treatment | Mean age | Male | Size | Response rate | Pain change | |||
| Ghahreman et al.20 | 2010 | 1 | Corticosteroid | 49 | 60.7% | 28 | Control | 44 | 51.4% | 37 | ✓ | ✓ |
| – | Corticosteroid | 49 | 53.6% | 30 | Control | 46 | 70.0% | 28 | ✓ | ✓ | ||
| Kuijper et al.24 | 2009 | 0 | Collar | 47.0 | 69.1% | 69 | Physiotherapy | 46.7 | 69.4% | 70 | ✓ | |
| Control | 47.7 | 66.7% | 66 | |||||||||
| Ozturk et al.27 | 2006 | – | Traction | 40.2 | 58.3% | 24 | Physiotherapy | 52.7 | 36.4% | 22 | ✓ | ✓ |
| Osterman et al.26 | 2006 | – | Surgery | 37 | 53.6% | 28 | Control | 38 | 67.9% | 28 | ✓ | |
| Kanayama et al.22 | 2005 | – | Serotonin | 31.6 | 45.0% | 20 | NSAID | 33.9 | 55.0% | 20 | ✓ | |
| Vad et al.32 | 2002 | 0 | Corticosteroid | 41.3 | – | 25 | Control | 42.1 | – | 23 | ✓ | |
| Shakoor et al.29 | 2002 | – | Traction | 46.66 | 55.8% | 100 | NSAID | 47.66 | 55.8% | 99 | ✓ | |
| Karppinen et al.23 | 2001 | 2 | Corticosteroid | 43.8 | 64.0% | 79 | Control | 43.7 | 58.0% | 79 | ✓ | |
| Hofstee et al.21 | 2002 | – | Physiotherapy | 38.0 | 54.2% | 80 | Control | 41.9 | 62.7% | 83 | ✓ | ✓ |
| Liu and Zhang25 | 2000 | – | Physiotherapy | – | 72.6% | 62 | Traction | – | 34.0% | 50 | ✓ | ✓ |
| Burton et al.18 | 2000 | 1 | Physiotherapy | 41.9 | 47.5% | 20 | Chemonucleolysis | 41.9 | 47.5% | 20 | ✓ | |
| Persson et al.28 | 1997 | – | Surgery | 45 | 59.0% | 27 | Physiotherapy | 48 | 41.0% | 27 | ✓ | |
| Collar | 49 | 63.0% | 27 | |||||||||
| Dilke et al.19 | 1973 | 2 | Corticosteroid | 38.7 | 53.0% | 35 | Control | 42.3 | 58.0% | 36 | ✓ | |
| Snoek et al.31 | 1977 | 2 | Control | 46.5 | 54.2% | 27 | Corticosteroid | 43.8 | 48.1% | 24 | ✓ | |
| Brewerton17 | 1966 | – | Traction | 20–80 | 41.2% | 114 | Collar | – | – | 120 | ✓ | |
| Shanthanna et al.30 | 2014 | 3 | PRF | 62 | 62.5% | 16 | Control | 57 | 53.3% | 14 | ✓ | |
NSAID: non-steroidal anti-inflammatory drugs; PRF: pulsed radiofrequency.
Figure 2.
Network of response rate and pain change. Lines represent direct comparisons between two interventions. The thicker the line is, the greater the number of existing direct comparisons between the two interventions. Numbers above dots show the total number of patients for each intervention.
NSAID: non-steroidal anti-inflammatory drugs; PRF: pulsed radiofrequency.
Response rate and pain score change from NMA results
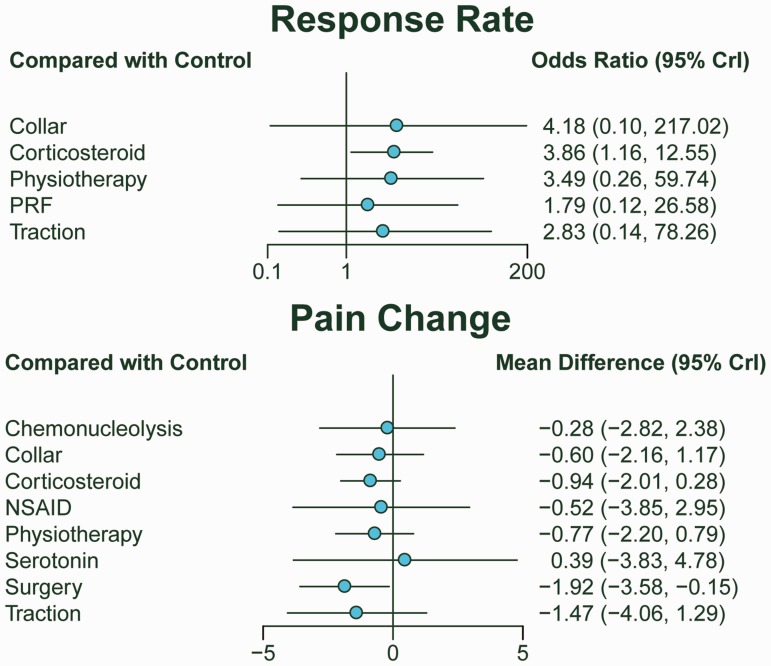
The network results in Table 2 showed that corticosteroid treatment had a significantly better response rate than control (OR = 3.86, 95% CrI: 1.16, 12.55). In addition, surgery displayed higher efficacy in pain change compared with control (MD = −1.92, 95% CrI: −3.58, −0.15). The results can be further proved by the forest plots as displayed in Figure 3.
Table 2.
Network meta-analysis results of response rate and pain change.
| Response rate | Control | −0.60 (−2.16, 1.17) | −0.94 (−2.01, 0.28) | −0.77 (−2.20, 0.79) | −1.47 (−4.06, 1.29) | −0.28 (−2.82, 2.38) | −0.52 (−3.85, 2.95) | 0.39 (−3.83, 4.78) | −1.92 (−3.58, −0.15) | – | Pain change |
| 4.18 (0.10, 217.02) | Collar | −0.35(−2.38, 1.65) | −0.18 (−1.70, 1.31) | −0.88 (−3.54, 1.79) | 0.32 (−2.32, 2.91) | 0.08 (−3.35, 3.45) | 0.99 (−3.31, 5.23) | −1.34 (−3.15, 0.44) | – | ||
| 3.86 (1.16, 12.55) | 0.92 (0.01, 43.38) | Corticosteroid | 0.17 (−1.72, 2.04) | −0.53 (−3.43, 2.36) | 0.66 (−2.16, 3.51) | 0.42 (−3.16, 4.03) | 1.32 (−3.12, 5.78) | −0.99 (−3.06, 1.06) | – | ||
| 3.49 (0.26, 59.74) | 0.85 (0.05, 11.94) | 0.91 (0.05, 20.09) | Physiotherapy | −0.70 (−2.93, 1.52) | 0.49 (−1.62, 2.62) | 0.26 (−2.80, 3.30) | 1.17 (−2.85, 5.17) | −1.15 (−2.92, 0.59) | – | ||
| 2.83 (0.14, 78.26) | 0.67 (0.08, 5.81) | 0.73 (0.03, 25.03) | 0.79 (0.16, 4.31) | Traction | 1.19 (−1.90, 4.27) | 0.96 (−1.17, 3.06) | 1.87 (−1.53, 5.20) | −0.45 (−3.30, 2.35) | – | ||
| Chemonucleolysis | −0.23 (−3.96, 3.47) | 0.69 (−3.88, 5.21) | −1.65 (−4.40, 1.11) | – | |||||||
| – | – | – | – | – | – | NSAID | 0.91 (−1.73, 3.51) | −1.40 (−4.97, 2.08) | – | ||
| – | – | – | – | – | – | – | Serotonin | −2.31 (−6.71, 2.05) | – | ||
| – | – | – | – | – | – | – | – | Surgery | – | ||
| 1.79 (0.12, 26.58) | 0.42 (0.00, 40.45) | 0.46 (0.03, 8.94) | 0.50 (0.01, 21.33) | 0.63 (0.01, 35.87) | – | – | – | – | PRF |
NSAID: non-steroidal anti-inflammatory drugs; PRF: pulsed radiofrequency.
Odds ratio (OR) or mean difference (MD) with 95% credible intervals (CrIs) were used to measure the relative efficacy. The network meta-analysis results are in the form of OR and 95% CrIs for response rate and MD and 95% CrIs for pain change. Boldfaced numbers indicate significant results (p < 0.05).
Figure 3.
Forest plot of response rate and pain change. Odds ratio (OR) and 95% credible intervals (CrIs) for response rate and mean difference (MD) and 95% CrIs for pain change.
NSAID: non-steroidal anti-inflammatory drugs; PRF: pulsed radiofrequency.
Ranking probability from SUCRA
SUCRA was evaluated in Table 3 for the purpose of rationally ranking the treatments with respect to each outcome. Concerning response rate, corticosteroid, collar, and physiotherapy held the top three rankings (SUCRA = 0.656, 0.652, and 0.610, respectively). Surgery, traction, and corticosteroid were superior to the others in pain change (SUCRA = 0.866, 0.748, and 0.589, respectively). Surgery has been recommended as the optimal treatment due to its high effectiveness in pain change. This is because that response rate and pain change were the most important primary outcomes of this study, and only 6 out of 10 treatments were available for response rate efficacy ranking, making this outcome lack comprehensiveness. Traction and corticosteroid can also be considered beneficial interventions regarding the two outcomes.
Table 3.
Surface under cumulative ranking curve of response rate and pain change.
| Treatment | Response rate | Pain change |
|---|---|---|
| Control | 0.182 | 0.237 |
| Collar | 0.652 | 0.454 |
| Corticosteroid | 0.656 | 0.589 |
| Physiotherapy | 0.610 | 0.530 |
| Traction | 0.490 | 0.748 |
| PRF | 0.410 | – |
| Chemonucleolysis | – | 0.367 |
| NSAID | – | 0.448 |
| Serotonin | – | 0.262 |
| Surgery | – | 0.866 |
NSAID: non-steroidal anti-inflammatory drugs; PRF: pulsed radiofrequency.
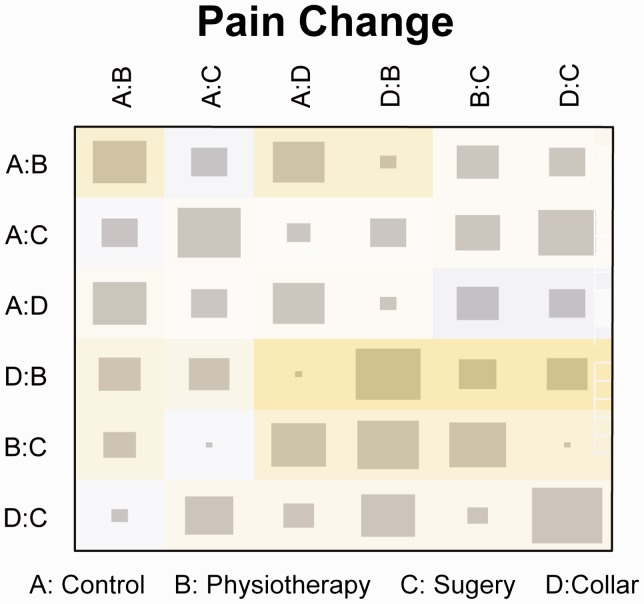
Consistency of direct and indirect comparisons for pain change
Node-splitting method (Table 4) and heat plot (Figure 4) were utilized to assess the inconsistency between direct and indirect comparisons. Based on the direct evidence results shown in Table 4, no significant outcomes were detected concerning pain change. It can also be seen that no inconsistency existed between direct and indirect evidence according to node-splitting results. No high levels of inconsistency were observed in the heat plot for pain change (node splitting and heat plot were only available for pain change). Funnel plot showed no significant publication bias (Figure S1).
Table 4.
Node-splitting results of pain change.
| Treatment |
Comparison |
p | ||
|---|---|---|---|---|
| Direct | Indirect | Network | ||
| Control vs. Collar | 1.20 (−1.10, 3.50) | −0.61 (−3.80, 2.40) | 0.61 (−1.20, 2.30) | 0.286 |
| Surgery vs. Collar | −1.90 (−4.50, 0.52) | −0.40 (−3.70, 2.90) | −1.30 (−3.10, 0.58) | 0.430 |
| Physiotherapy vs. Control | −0.76 (−2.50, 1.10) | −0.39 (−3.90, 3.20) | −0.78 (−2.30, 0.68) | 0.833 |
| Surgery vs. Control | −1.50 (−3.90, 1.00) | −2.40 (−4.80, 0.30) | −1.90 (−3.50, −0.13) | 0.580 |
| Surgery vs. Physiotherapy | −1.10 (−3.40, 1.50) | −0.83 (−4.20, 2.40) | −1.10 (−2.80, 0.59) | 0.864 |
Mean difference with 95% credible intervals and p values were used to determine the difference between direct and indirect evidence.
Figure 4.
Heat plot of pain change. The area of the gray squares displays the contribution of the direct estimate in design (shown in the column) to the network estimate in design (shown in the row). The colors are associated with the change in inconsistency between direct and indirect evidence (shown in the row) after detaching the effect (shown in the column). Cold colors indicate an increase in inconsistency, and warm colors indicate a decrease in inconsistency (the stronger the color is, the stronger the change is).
Discussion
We conducted the first NMA of the different treatment strategies for radiculopathy in order to better understand the relative efficacies of the available treatment options. A total of 16 RCTs were selected according to the standard literature selection criteria and included in this NMA. The response rate or pain score change data were extracted from each study and synthesized. Surgery along with traction and corticosteroids is highly recommended as the first-class treatments for radiculopathy based on the relative effects and SUCRA values. Surgery, in particular, has been highly recommended for being the highest rank treatment in pain score change. As for inconsistencies between indirect and direct evidence, no obvious inconsistencies were detected. Thus, it confirmed the acceptable quality of evidence included in this NMA.
Furthermore, our results showed consistency with other recent published systematic reviews, which strengthened the reliability of this NMA. In a prospective study, cervical radiculopathy patients who underwent surgical procedure exhibited a significant improvement in pain as compared to patients without surgery in the first year after diagnosis.33 Another systematic review, which focused on the effectiveness of treatments for the lumbosacral radicular syndrome, demonstrated that surgery was more efficacious for patients with lumbosacral radicular syndrome regarding overall improvement after a one-year follow-up, compared to physiotherapy.34 Corticosteroid injections showed early and moderate but unsustained improvements versus placebo in certain outcomes.35–37 Corticosteroids demonstrated effectiveness in reducing pain in a substantial proportion of patients with lumbar radicular pain.38 The first report regarding the clinical use of steroid injection was published in 1953;39 since then, it has been increasingly utilized on the strong pathophysiologic basis that its local anti-inflammatory function can inhibit inflammation by eliminating the secretion of cytokines, thereby reducing pain.36 Therefore, corticosteroid injections were considered as an efficient and safe choice. Complications resulting from corticosteroid injection are rare. However, the method involving injection into the patients’ foramen is still worthy of optimization with regard to the detection of arterial injuries.37
Although our study showed consistencies with other recently published analyses, contradictory results can also be observed according to other associated MAs. In an MA carried out by Nikolaidis et al.,14 it was concluded that the trials included in the analysis did not provide reliable evidence of surgery effectiveness on cervical spondylotic radiculopathy or myelopathy. They also stated that low-quality evidence was used to demonstrate that surgery might provide pain relief faster than physiotherapy or hard collar immobilization in patients with cervical radiculopathy, but little or no difference was shown in the long term. With respect to traction, one MA pointed out that traction was no more effective than placebo and collar. However, it should be noted that the study admitted that the evidence was of very low quality.40 This inconsistency with our findings may be due to risks of bias and patient background variations. As the first NMA study to evaluate the efficacy of different treatments for radiculopathy, the conclusion of our study is clear and is supported by reproducible eligibility criteria. However, admittedly, a few limitations still exist. First, the optimal treatments for three kinds of radiculopathy might be different while in our study we put all the relevant studies together due to the lack of correlated researches. Second, when it came to SUCRA rankings of response rate, only 6 out of the 10 treatment groups could be assessed, making the evaluation process lack comprehensiveness. Furthermore, the different administrative approaches and doses of specific treatments were not considered as variables in this analysis. The different approaches in steroid injection, surgery, traction, or different combination and dosage of drugs in medication therapies would also have impacts on efficacy rankings. For instance, among steroid injection, facet injection has been suggested to be more effective and safer than transforaminal injection.41 The combination of bupivacaine and betamethasone has also been shown to achieve better response rates than using bupivacaine alone.42 Autotraction seems to perform better with regard to traction pain relief compared to conventional passive traction methods.43
Besides, several limitations still exist in our NMA although we conducted it as meticulously as possible. First, the sample sizes of included studies were not very satisfying, which is also due to the essential characteristics of NMA. Second, a lack of sufficient data caused the absence of some variables in our analysis, such as administrative methods and dosages of drugs aforementioned. More RCTs with appropriate sample sizes should be conducted in future studies in order to better understand and compare efficacies of the regimens of radiculopathy. Third, various types of treatments used in control groups such as needle placement, physical therapy, and “wait and see” might weaken the credibility of the comparisons among different trials.
In summary, according to this NMA, surgery is recommended as the optimal treatment while traction and corticosteroid can also be considered good interventions. However, the choice of treatment should be based on the clinical situation. Moreover, related RCTs with long-term follow-up data and other outcome measurements such as side effects were needed to further analyze all the treatments.
Author Contributions
Research conception and design: DS; Data collection and screening: XZ and ZZ; Drafting of the manuscript: XZ, JW, and JL; Critical revision of the manuscript: YS and DS; Approval of final manuscript: All authors.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Corey DL andComeau D.. Cervical radiculopathy. The Medical clinics of North America 2014; 98: 791–799, xii. DOI: 10.1016/j.mcna.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 2. DeFroda SF Daniels AH andDeren ME.. Differentiating Radiculopathy from Lower Extremity Arthropathy. The American Journal of Medicine 2016; 129: 1124 e1121–1127. DOI: 10.1016/j.amjmed.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 3. Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P, 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL, Jr., Toton JF. and North American Spine S. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. The Spine Journal : Official Journal of the North American Spine Society 2014; 14: 180–191. DOI: 10.1016/j.spinee.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 4. Cho N Keith J andPirouzmand F.. Lumbar discal cyst as a cause of radiculopathy: case report. British Journal of Neurosurgery 2016; 30: 675–677. DOI: 10.3109/02688697.2015.1100274. [DOI] [PubMed] [Google Scholar]
- 5. Gunduz OH Sencan S andKokar S.. A rare cause of lumbar radiculopathy: perineural cyst. Pain Medicine 2015; 16: 199–200. DOI: 10.1111/pme.12560. [DOI] [PubMed] [Google Scholar]
- 6. Schoenfeld AJ Laughlin M Bader JO andBono CM.. Characerization of the incidence and risk factors for the development of lumbar radiculopathy. Journal of Spinal Disorders & Techniques 2012; 25: 163–167. DOI: 10.1097/BSD.0b013e3182146e55. [DOI] [PubMed] [Google Scholar]
- 7. Schoenfeld AJ George AA Bader JO andCaram PM Jr.. Incidence and epidemiology of cervical radiculopathy in the United States military: 2000 to 2009. Journal of Spinal Disorders & Techniques 2012; 25: 17–22. DOI: 10.1097/BSD.0b013e31820d77ea. [DOI] [PubMed] [Google Scholar]
- 8. Tarulli AW andRaynor EM.. Lumbosacral radiculopathy. Neurologic Clinics 2007; 25: 387–405. DOI: 10.1016/j.ncl.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 9. Radhakrishnan K Litchy WJ O'Fallon WM andKurland LT.. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990 Brain: A Journal of Neurology 1994; 117: 325–335 [DOI] [PubMed] [Google Scholar]
- 10. Iyer S andKim HJ.. Cervical radiculopathy. Current Reviews in Musculoskeletal Medicine 2016; 9: 272–280. DOI: 10.1007/s12178-016-9349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mondelli M Aretini A Arrigucci U Ginanneschi F Greco G andSicurelli F.. Clinical fidings and electrodiagnostic testing in 108 consecutive cases of lumbosacral radiculopathy due to herniated disc. Neurophysiologie Clinique = Clinical Neurophysiology 2013; 43: 205–215. DOI: 10.1016/j.neucli.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 12. Chou R Hashimoto R Friedly J Fu R Dana T Sullivan S Bougatsos C andJarvik J. Pain Management Injection Therapies for Low Back Pain. Rockville (MD) 2015 [PubMed]
- 13. Woods BI andHilibrand AS.. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. Journal of Spinal Disorders & Techniques 2015; 28: E251–259. DOI: 10.1097/BSD.0000000000000284. [DOI] [PubMed] [Google Scholar]
- 14. Nikolaidis I Fouyas IP Sandercock PA andStatham PF. Surgery for cervical radiculopathy or myelopathy. The Cochrane Database of Systematic Reviews 2010; 65: CD001466. DOI: 10.1_/14651858.CD001466.pub3. [DOI] [PMC free article] [PubMed]
- 15. Krahn U Binder H andKonig J. A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol 2013; 13: 35. 2013/03/19. DOI: 10.1186/1471-2288-13-35. [DOI] [PMC free article] [PubMed]
- 16. Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods 2012; 3: 80–97. 2012/06/01. DOI: 10.1002/jrsm.1037. [DOI] [PubMed] [Google Scholar]
- 17. Brewerton DA. Pain in the neck and arm: a multicentre trial of the effects of physiotherapy, arranged by the British Association of Physical Medicine. British medical journal 1966; 1: 253–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Burton AK Tillotson KM andCleary J.. Single-blind randomised controlled trial of chemonucleolysis and manipulation in the treatment of symptomatic lumbar disc herniation. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2000; 9: 202–207. 2000/07/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dilke TF Burry HC andGrahame R.. Extradural corticosteroid injection in management of lumbar nerve root compression. British Medical Journal 1973; 2: 635–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ghahreman A Ferch R andBogduk N.. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Medicine 2010; 11: 1149–1168. DOI: 10.1111/j.1526-4637.2010.00908.x. [DOI] [PubMed] [Google Scholar]
- 21. Hofstee DJ Gijtenbeek JM Hoogland PH van Houwelingen HC Kloet A Lotters F andTans JT.. Westeinde sciatica tial: randomized controlled study of bed rest and physiotherapy for acute sciatica. Journal of Neurosurgery 2002; 96: 45–49. [DOI] [PubMed] [Google Scholar]
- 22. Kanayama M Hashimoto T Shigenobu K Oha F andYamane S.. New treatment of lumbar disc herniation involving 5-hydroxytryptamine2A receptor inhibitor: a randomized controlled trial. Journal of Neurosurgery Spine 2005; 2: 441–446. DOI: 10.3171/spi.2005.2.4.0441. [DOI] [PubMed] [Google Scholar]
- 23. Karppinen J Malmivaara A Kurunlahti M Kyllonen E Pienimaki T Nieminen P Ohinmaa A Tervonen O andVanharanta H.. Peiradicular infiltration for sciatica: a randomized controlled trial. Spine 2001; 26: 1059–1067. [DOI] [PubMed] [Google Scholar]
- 24. Kuijper B Tans JT Beelen A Nollet F andde Visser M.. Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomised trial. Bmj 2009; 339: b3883. DOI: 10.1136/bmj.b3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu J andZhang S.. Treatment of protrusion of lumbar intervertebral disc by pulling and turning manipulations. Journal of traditional Chinese medicine = Chung i tsa chih ying wen pan / sposored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine 2000; 20: 195–197. [PubMed] [Google Scholar]
- 26. Osterman H Seitsalo S Karppinen J andMalmivaara A.. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine 2006; 31: 2409–2414. DOI: 10.1097/01.brs.0000239178.08796.52. [DOI] [PubMed] [Google Scholar]
- 27. Ozturk B Gunduz OH Ozoran K andBostanoglu S.. Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc heriation. Rheumatology International 2006; 26: 622–626. DOI: 10.1007/s00296-005-0035-x. [DOI] [PubMed] [Google Scholar]
- 28. Persson LC Moritz U Brandt L andCarlsson CA.. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with sugery, physiotherapy or cervical collar. A prospective, controlled study. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 1997; 6: 256–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shakoor MA Ahmed MS Kibria G Khan AA Mian MA Hasan SA Nahar S andHossain MA.. Effects of cervical traction and exercise therapy in cervical spondylosis. Bangladesh Medical Research Council bulletin 2002; 28: 61–69. [PubMed] [Google Scholar]
- 30. Shanthanna H Chan P McChesney J Thabane L andPaul J.. Pulsed radiofrequency treatment of the lumbar dorsal root ganglion in patients with chronic lumbar radicular pain: A randomized, placebo-controlled pilot study. Journal of Pain Research 2014; 7: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Snoek W Weber H andJorgensen B.. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta orthopaedica Scandinavica 1977; 48: 635–641. [DOI] [PubMed] [Google Scholar]
- 32. Vad VB Bhat AL Lutz GE andCammisa F.. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine 2002; 27: 11–16. [DOI] [PubMed] [Google Scholar]
- 33. Engquist M Lofgren H Oberg B Holtz A Peolsson A Soderlund A Vavruch L andLind B.. Surgery versus nonsurgical treatment of cervical radiculopathy: a prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine 2013; 38: 1715–1722. DOI: 10.1097/BRS.0b013e31829ff095. [DOI] [PubMed] [Google Scholar]
- 34. Luijsterburg PA Verhagen AP Ostelo RW van Os TA Peul WC andKoes BW.. Effectiveness of consevative treatments for the lumbosacral radicular syndrome: a systematic review. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2007; 16: 881–899. DOI: 10.1007/s00586-007-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chou R Hashimoto R Friedly J Fu R Bougatsos C Dana T Sullivan SD andJarvik J.. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Annals of Internal Medicine 2015; 163: 373–381. DOI: 10.7326/M15-0934. [DOI] [PubMed] [Google Scholar]
- 36. Benoist M Boulu P andHayem G.. Epidural steroid injections in the management of low-back pain with radiculopathy: an update of their efficacy and safety. European spine journal : oficial publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2012; 21: 204–213. DOI: 10.1007/s00586-011-2007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Quraishi NA. Transforaminal injection of cortices eroids for lumbar radiculopathy: systematic review and meta-analysis. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2012; 21: 214–219. DOI: 10.1007/s00586-011-2008-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. MacVicar J King W Landers MH andBogduk N.. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Medicine 2013; 14: 14–28. DOI: 10.1111/j.1526-4637.2012.01508.x. [DOI] [PubMed] [Google Scholar]
- 39. Lievre JA Bloch- Michel H andAttali P.. [Trans-sacral injection; clinical and radiological study]. Bulletins et memoires de la Societe medicale des hopitaux de Paris 1957; 73: 1110–1118 [PubMed] [Google Scholar]
- 40. Thoomes EJ Scholten-Peeters W Koes B Falla D andVerhagen AP.. The effectiveness of conservative treatment for patients with cervical radiculopathy: a systematic review. The Clinical Journal of Pain 2013; 29: 1073–1086. DOI: 10.1097/AJP.0b013e31828441fb. [DOI] [PubMed] [Google Scholar]
- 41. Bureau NJ Moser T Dagher JH Shedid D Li M Brassard P andLeduc BE.. Transforaminal versus intra-articular facet corticosteroid injections for the treatment of cervical radiculopathy: a randomized, double-blind, controlled study. AJNR American Journal of Neuroradiology 2014; 35: 1467–1474. DOI: 10.3174/ajnr.A4026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Riew KD Yin Y Gilula L Bridwell KH Lenke LG Lauryssen C andGoette K.. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, contolled, double-blind study. The Journal of Bone and Joint Surgery American Volume 2000; 82-A: 1589–1593. [DOI] [PubMed] [Google Scholar]
- 43. Tesio L andMerlo A.. Autotraction versus passive traction: an open controlled study in lumbar disc herniation. Archives of Physical Medicine and Rehabilitation 1993; 74: 871–876. [DOI] [PubMed] [Google Scholar]