Abstract
Background
The aim of this study was to explore the diagnostic value of sagittal measurement of thoracic inlet parameters for degenerative cervical spondylolisthesis (DCS).
Material/Methods
We initially included 65 patients with DCS and the same number of health people as the control group by using cervical radiograph evaluations. We analyzed the x-ray and computer tomographic (CT) data in prone and standing position at the same time. Measurement of cervical sagittal parameters was carried out in a standardized supine position. Multivariate logistic regression analysis was performed to evaluate these parameters as a diagnostic index for DCS.
Results
There were 60 cases enrolled in the DCS group, and 62 cases included in the control group. The T1 slope and thoracic inlet angle (TIA) were significantly greater for the DCS group compared to the control group (24.33±2.85º versus 19.59±2.04º, p=0.00; 76.11±9.82º versus 72.86±7.31º, p=0.03, respectively). We observed no significant difference for the results of the neck tilt (NT), C2–C7 angle in the control and the DSC group (p>0.05). Logistic regression analysis and receiver operating characteristic (ROC) curve revealed that preoperative T1 slope of more than 22.0º showed significantly diagnostic value for the DCS group (p<0.05).
Conclusions
Patients with preoperative sagittal imbalance of thoracic inlet have a statistically significant increased risk of DCS. T1 slope of more than 22.0º showed significantly diagnostic value for the incidence of DCS.
MeSH Keywords: Cerclage, Cervical; Inpatients; Logistic Models
Background
Degenerative cervical spondylolisthesis (DCS) is one of the most common indications of cervical spine surgery, particularly in patients older than 50 years of age. The published literature reported that prevalence of DCS ranged from 3.9% to 20% [1,2]. Several factors, including patient age, degeneration of the disc, and sagittal change of the facet joint may contribute to the incidence of DCS [3–5].
Current literature regarding the etiology and predisposing factors for DCS remains controversial. Researchers suggested that relative hypermobility in conjunction with degenerative change of facets and laxity of surrounding ligaments may result in the frequent occurs of DCS in the cervical spine mid-region [6]. Liu et al. [7] believed that facet joint and disc degeneration occurred at the same time, and both could be initiating causes in altering spine mechanics, resulting in DCS.
Barrey et al. [8] carried out a measurement to explore the relation between the spinopelvic parameters and DCS; their study results confirmed that patients with DCS were had a greater pelvic incidence (PI) when compared with the normal population; therefore, PI could be used as an indicator for DCS. Another study measured the spinopelvic parameters to analyze adjacent segment disease (ASD) after transforaminal interbody fusion (TLIF) for degenerative lumbar disease by the methods of multivariate logistic regression analysis; the results showed that the risk of ASD incidence was 5.1 times greater in patients with preoperative pelvic tilt (PT) of more than 22.5º [9]. Sagittal balance in the cervical spine is increasingly important in common with the PI and PT. The balanced upright posture and proper horizontal gaze, like the PI in the pelvis, could be obtained by adjusting the sagittal balance of the cervical spine.
Three parameters, including thoracic inlet angle (TIA), neck tilt (NT), and T1 slope, could be used as the result of sagittal measurement of thoracic inlet. These parameters have been confirmed to influence the alignment of the cervical spine and could affect the cervical degeneration, which could be risk factors for the DCS. Physiological sagittal alignment of the cervical spine could also be used to predict by these parameters [10]. Sagittal measurements of thoracic inlet parameters were carried out for the enrolled patients (DCS and control groups) to forecast the diagnostic value of such parameters for the incidence of DCS.
Material and Methods
Ethical considerations
The study protocol was approved by the ethics committee of Hubei University of Medicine. Informed consents from all the enrolled patients were acquired before the research. All the methods carried out in the research were performed in accordance with the relevant guidelines and regulations.
Patients and control participants selected for the study
We identified 65 patients diagnosed with DCS who obtained both cervical radiograph and CT scans from October 2012 to May 2017. Meanwhile, the same number of healthy participants were enrolled as the control group, and all the participants in the control group also had cervical CT scans and cervical radiograph. DCS was defined as being a forward translation of one vertebral body on an adjacent vertebral body, as seen on standard or flexion-extension lateral cervical radiographs (more than 3 mm). All the included participants with previous history of cervical surgery, scoliosis more severe than 15°, malignant tumors, or cervical tuberculosis were excluded from this study.
Radiographic and clinical assessment
All the included participants in the study had radiographic assessments. We obtained lateral radiographs by using standard x-rays, while the tube was located at the center of C3–C4 intervertebral disc. Parameters of C2–C7 Cobb angle, sagittal vertical axis of C2–C7 (C2–C7 SVA) were measured by lateral radiographs. We carried out the sagittal measurement of the thoracic inlet parameters by using cervical CT (Brilliance CT 64-channel scanner; Philips Electronics Amsterdam, Netherlands) at the prone position: the parameters included TIA, NT, and T1 slope.
We described C2–C7 sagittal vertical axis (C2–C7 SVA) as the distance between C2 plumb line and the superior posterior endplate of C7 with positive sagittal alignment, which was defined as an anterior deviation (Figure 1). The C2–C7 angle is formed when the horizontal line of C7 lower endplate and the horizontal line of C2 lower endplate insect (Figure 1). T1 slope is usually formed by drawing a line along the superior endplate of T1 and horizontal reference line at the median sagittal of the cervical vertebra from the CT scans (Figure 2). We defined the TIA as the angle when a line perpendicular to the T1 upper end plate (T1UEP) meet with the line connecting the center of the T1UEP and the upper top of the sternum (Figure 2). Two independent lines, one from the upper sternum and one from the neck tilt angle; one is the vertical line and the other one is the line to the center of the T1UEP (Figure 2).
Figure 1.

C2–C7 angle and C2–C7 SVA at the lateral radiographs; C2–C7 SVA indicates sagittal vertical axis.
Figure 2.
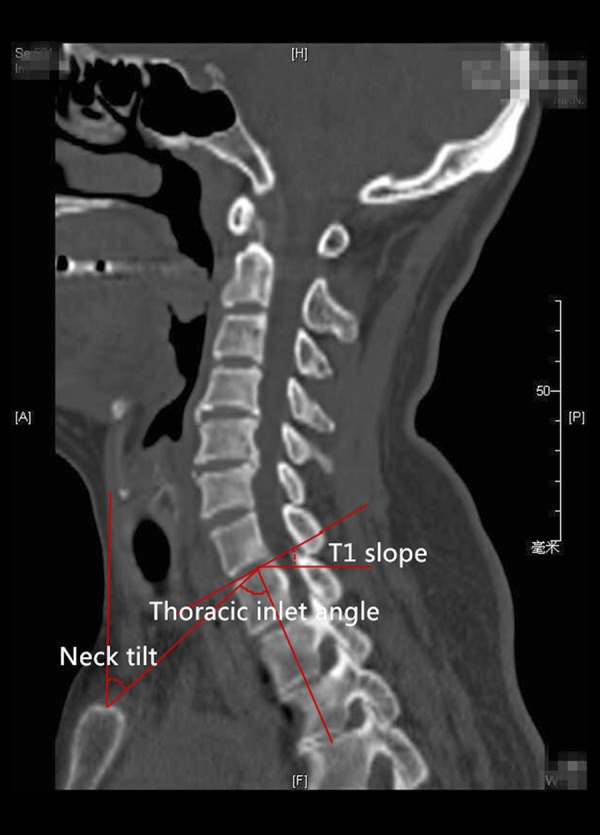
Parameters of the cervical parameters on CT scan (T1 slope, thoracic inlet angle, neck tilt); CT indicates computed tomography.
We also measured clinical indicators such as the body mass index (BMI), age of the patients, gender, and smoking history.
Statistical analysis
All the statistical analyses were performed by using SPSS 21.0 (SPSS, Chicago, IL, USA). Data is presented as mean ± standard deviations. Student’s t-test was employed for the data to compare the DCS group and control group. Tests were two-tailed and p<0.05 was considered significant. Logistic regression was used to evaluate odds ratios (OR) and 95% confidence intervals (CI) for variables with significant associations with DCS based on the results of the t-test. The area under receiver operating characteristic curve (ROC) was the concordant index (c-index), which was used to identify which radiographic measurements could be most effective at predicting DCS.
Results
Patient characteristics
The characteristics of the patients are summarized in Table 1). Sixty of the 65 patients were finally enrolled in the DCS group; five patients had incomplete follow-up due to missing contact information or passing away. Sixty-two participants were included in the control group; three were lost to follow-up due to missing contact information or passing away. The mean age, gender, follow-up period, and BMI were similar between the two groups (p>0.05) (Table 1). DCS was found in specific segments of the cervical vertebra, which are shown in the Table 2.
Table 1.
Characteristics of enrolled pubjects in the DCS and control group.
| Characteristics | DCS group (n=60) | Cotrol group (n=62) | Value of χ2 or t | P |
|---|---|---|---|---|
| Age of the patients (years) | 48.6±7 | 46.1±5.9 | 2.01 | 0.03 |
| Gender | ||||
| Male | 24 (40.0%) | 27 (43.5%) | 0.16 | 0.69 |
| Female | 36 (60.0%) | 35 (56.5%) | ||
| BMI | 25.9±5.6 | 23.8±3.6 | 0.86 | 0.17 |
| Smoking history | 15 (25%) | 12 (22.6%) | 0.12 | 0.73 |
Table 2.
Level of DCS.
| Level | No. of the patients (%) |
|---|---|
| C2–3 | 2 (3.3%) |
| C3–4 | 12 (20.0%) |
| C4–5 | 29 (48.3%) |
| C5–6 | 10 (16.7%) |
| C6–7 | 5 (8.3%) |
| C7–T1 | 2 (3.3%) |
Parameters at the sagittal measurement (univariate analysis)
The mean T1 slope in the DCS group on CT was 24.33±2.85º and the mean T1 slope in the control group on CT was 19.59±2.04º (p=0.00). The TIA in the DCS group was larger than the control group (76.11±5.52º versus 72.86±7.31º, p=0.03). No significant differences were detected between the two groups for the results of C2–C7 angle (10.28±5.63º versus 10.63±6.25º, p=0.59), C2–C7 SVA (17.58±8.09º versus 16.99±8.59º, p=0.49), NT (48.33±8.05º versus 49.16±8.12º, p=0.38) (Table 3).
Table 3.
Parameters at sagittal plane of cervical vertebra.
| Characteristics | DCS group (n=60) | Cotrol group (n=62) | Value of χ2 or t | P |
|---|---|---|---|---|
| C2–C7 angle (°) | 10.28±5.63 | 10.63±6.25 | 0.52 | 0.59 |
| C2–C7 SVA (mm) | 17.58±8.09 | 16.99±8.59 | 0.62 | 0.49 |
| T1 slope (°) | 24.33±2.85 | 19.59±2.04 | 10.60 | 0.00 |
| TIA (°) | 76.11±5.52 | 74.86±7.31 | 2.19 | 0.03 |
| Neck tilt (°) | 48.33±8.05 | 49.16±8.12 | 0.72 | 0.38 |
Results of logistic regression and ROC curve
Multiple logistic regression analysis was carried out to reveal the relative impact of variables on the incidence of DCS. The variables from the univariate analysis which were associated with the incidence of DCS were age of the patients, T1 slope, and TIA. Logistic regression analysis and ROC curve shows that preoperative T1 slope of more than 22.0º show significantly diagnostic value for the incidence of DCS (p<0.05) (Table 4). Good diagnostic value was obtained from T1 slope based on the result of area under curve (AUC, 0.91) (Figure 3).
Table 4.
Logistic regression of risk factors for DCS.
| Risk factors | P | OR 95%CI |
|---|---|---|
| Age | 0.26 | 1.21 (0.67–2.11) |
| T1 slope | 0.01 | 0.33 (0.12–0.62) |
| TIA | 0.08 | 0.56 (0.12–1.19) |
Figure 3.
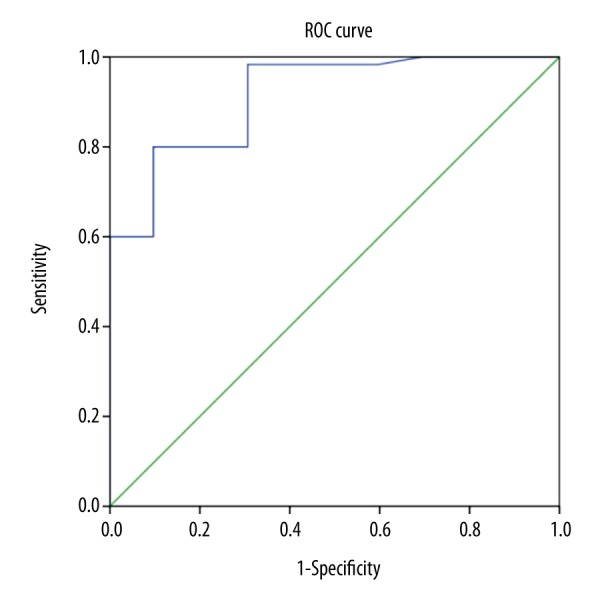
Logistic regression and ROC analysis. Logistic regression and ROC analysis revealed a cut-off value for T1 slope of 22.0°. The area under the curve AUC is 0.91. AUC indicates under receiver operating characteristic, ROC indicates receiver operating characteristic.
Discussion
More attention has been paid to adult spinal deformity. Surgical reconstruction of sagittal spinal alignment has been associated with improvement of functional status for the patients with a severe sagittal plane deformity. The pelvic tilt (PT) is an important parameter indicative of pelvic compensation, and an increase in PT is correlated with increased disability; a study showed that preoperative PT of more than 22.58° was a significant risk factor for the incidence of adjacent segment disease (ASD) after the fusion surgery [13]. Cervical deformity principles have been expanding to include balance throughout the cervical spine, with early data showing promise for similar relationships to be found in the lumbar spine and the related diseases as well. It was not possible to measure the T1 slope, neck tilt (NT), and TIA accurately by collecting data using lower resolution x-rays. We carried out CT scans to measure the parameters, and found that the correlations between parameters on the CT scans were similar to the x-ray data.
Previous studies confirmed that larger T1 slope may be associated with the increasing incidence of DCS; it also could be one of the predisposing factors in the onset of anterolisthesis DCS by increasing TIA, and finally, increasing the C2–C7 angle [14,15]. T1 slope is the most important parameter, which could be used to evaluate the sagittal balance of the cervical spine and has been previously correlated with C2–C7 angle and SVA C2–C7 [13]. Patients with a high T1 slope require more activity from the posterior neck muscles to maintain a horizontal gaze and to minimize energy expenditure in relation to head position. Several studies hypothesized that the posterior neck muscle compensation was one important preventive mechanism from postoperative cervical kyphosis progression, especially in patients with high T1 slope [16,17]. However, some cases could not compensate for high T1 slope with enough cervical lordosis, because of weakness of posterior neck muscles or cervical canal compromise [16]. Such hypothesis was demonstrated by the fact that high T1 slope patients showed more kyphotic alignment after laminoplasty, which they postulated to be because of the posterior neck muscles being severely damaged and atrophied after the operation [18]. Weakness of the posterior neck muscle increased the chance of postoperative kyphosis progression and even influenced head deformity. However, the definite description of such compensation of cervical sagittal balance still remains uncertain.
Our study showed that patients with DCS had a larger T1 slope compared with the normal cases based on results of our univariate analysis. T1 slope of more than 22.0º showed significant diagnostic value for the incidence of DCS based on the results of logistic regression analysis and ROC curve. According to previous experiences and the significant correlations between T1 slope and C2–C7 angle (cervical lordosis), patients with larger T1 slope in the DCS group should have larger C2–C7 angle compared to the control group. However, no significant differences were detected between the two groups for the C2–C7 angle. The sagittal imbalance may explain the phenomena for the cases with DCS. The disc degeneration may result in the slipping and loss of lordosis, which is also the cause of sagittal anterior imbalance [14]. Anterior translation of the axis of gravity may also result in the sliding force observed for the patients with DCS.
The larger T1 slope for patients with DCS could be a possible explanation for the compensatory mechanism of posterior neck muscles. DCS is thought to be the results of cervical structural decompensation [21,22]. For some cases of (DCS) with flexion of the cervical vertebra, posterior neck muscles might be stretched and weaker than in the neutral and extension position, which might lead to an increased risk of developing anterior cervical sagittal imbalance, as decompensated cervical structures might be unable to provide adequate compensatory action to maintain the T1 slope, resulting in larger T1 slope in the patients with DCS [23,24].
Several limitations may exist in the study. The first one is that a retrospective study may bring section bias. Second, all the included patients were from China, which may bring regional bias. Third, the limited number of enrolled patients may limit its power to detect the true differences between the two groups.
Conclusions
Patients with preoperative sagittal imbalance of the thoracic inlet have a statistically significant increased risk of DCS. T1 slope of more than 22.0° showed significant diagnostic value for the incidence of DCS.
Footnotes
Source of support: Departmental sources
References
- 1.Suzuki A, Daubs MD, Inoue H, et al. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine (Phila Pa 1976) 2013;38(17):E1115–20. doi: 10.1097/BRS.0b013e31829b1487. [DOI] [PubMed] [Google Scholar]
- 2.Kopacz KJ, Connolly PJ. The prevalence of cervical spondylolisthesis. Orthopedics. 1999;22(7):677–79. [PubMed] [Google Scholar]
- 3.Park MS, Moon SH, Lee HM, et al. The natural history of degenerative spondylolisthesis of the cervical spine with 2- to 7-year follow-up. Spine (Phila Pa 1976) 2013;38(4):E205–10. doi: 10.1097/BRS.0b013e31827de4fd. [DOI] [PubMed] [Google Scholar]
- 4.Shigematsu H, Ueda Y, Takeshima T, et al. Degenerative spondylolisthesis does not influence surgical results of laminoplasty in elderly cervical spondylotic myelopathy patients. Eur Spine J. 2010;19(5):720–25. doi: 10.1007/s00586-010-1338-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rong X, Liu Z, Wang B, et al. Relationship between facet tropism and facet joint degeneration in the sub-axial cervical spine. BMC Musculoskelet Disord. 2017;18(1):86. doi: 10.1186/s12891-017-1448-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deburge A, Mazda K, Guigui P. Unstable degenerative spondylolisthesis of the cervical spine. J Bone Joint Surg Br. 1995;77(1):122–25. [PubMed] [Google Scholar]
- 7.Liu J, Ebraheim NA, Haman SP, et al. How the increase of the cervical disc space height affects the facet joint: An anatomy study. Spine (Phila Pa 1976) 2006;31(12):E350–54. doi: 10.1097/01.brs.0000219496.42765.8a. [DOI] [PubMed] [Google Scholar]
- 8.Barrey C, Jund J, Perrin G, et al. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61(5):981–86. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 9.Yamasaki K, Hoshino M, Omori K, et al. Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 2017;42(2):E86–92. doi: 10.1097/BRS.0000000000001728. [DOI] [PubMed] [Google Scholar]
- 10.Jun HS, Chang IB, Song JH, et al. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine (Phila Pa 1976) 2014;39(10):E630–36. doi: 10.1097/BRS.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 11.Woiciechowsky C, Thomale UW, Kroppenstedt SN. Degenerative spondylolisthesis of the cervical spine – symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004;13(8):680–84. doi: 10.1007/s00586-004-0673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tani T, Kawasaki M, Taniguchi S, et al. Functional importance of degenerative spondylolisthesis in cervical spondylotic myelopathy in the elderly. Spine (Phila Pa 1976) 2003;28(11):11128–34. doi: 10.1097/01.BRS.0000067263.73474.97. [DOI] [PubMed] [Google Scholar]
- 13.Yamasaki K, Hoshino M, Omori K, et al. Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 2017;42(2):E86–92. doi: 10.1097/BRS.0000000000001728. [DOI] [PubMed] [Google Scholar]
- 14.Jun HS, Kim JH, Ahn JH, et al. T1 slope and degenerative cervical spondylolisthesis. Spine (Phila Pa 1976) 2015;40(4):E220–26. doi: 10.1097/BRS.0000000000000722. [DOI] [PubMed] [Google Scholar]
- 15.Paholpak P, Nazareth A, Hsieh PC, et al. Kinematic evaluation of cervical sagittal balance and thoracic inlet alignment in degenerative cervical spondylolisthesis using kinematic magnetic resonance imaging. Spine J. 2017;17(9):1272–84. doi: 10.1016/j.spinee.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 16.Weng C, Wang J, Tuchman A, et al. Influence of T1 slope on the cervical sagittal balance in degenerative cervical spine: An analysis using kinematic MRI. Spine (Phila Pa 1976) 2016;41(3):185–90. doi: 10.1097/BRS.0000000000001353. [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Cho CB, Song JH, et al. T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc. 2013;53(6):356–59. doi: 10.3340/jkns.2013.53.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg Spine. 2013;19(2):141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 19.Hayashi T, Daubs MD, Suzuki A, et al. The compensatory relationship of upper and subaxial cervical motion in the presence of cervical spondylosis. Clin Spine Surg. 2016l;29(4):E196–200. doi: 10.1097/BSD.0b013e3182aab240. [DOI] [PubMed] [Google Scholar]
- 20.Cho JH, Ha JK, Kim DG, et al. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976) 2014;39(26):E1575–81. doi: 10.1097/BRS.0000000000000614. [DOI] [PubMed] [Google Scholar]
- 21.Kim TH, Lee SY, Kim YC, et al. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 2013;38(16):E992–97. doi: 10.1097/BRS.0b013e3182972e1b. [DOI] [PubMed] [Google Scholar]
- 22.Kim B, Yoon DH, Ha Y, et al. Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J. 2016;16(2):219–25. doi: 10.1016/j.spinee.2015.10.042. [DOI] [PubMed] [Google Scholar]
- 23.Gerling MC, Bohlman HH. Dropped head deformity due to cervical myopathy: Surgical treatment outcomes and complications spanning twenty years. Spine (Phila Pa 1976) 2008;33(20):E739–45. doi: 10.1097/BRS.0b013e31817f1f8b. [DOI] [PubMed] [Google Scholar]
- 24.Xu C, Lin B, Ding Z, et al. Cervical degenerative spondylolisthesis: Analysis of facet orientation and the severity of cervical spondylolisthesis. Spine J. 2016;16(1):10–15. doi: 10.1016/j.spinee.2015.09.035. [DOI] [PubMed] [Google Scholar]


