Comment to : Valdez RS, Holden RJ, Novak LL, et al. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc JAMIA Published Online First: 14 August 2014. doi:10.1136/amiajnl-2014-002826
In their paper “Transforming Consumer Health Informatics through a Patient Framework: connecting patients to context,”1 Valdez and colleagues propose a “patient-work” framework based on an holistic view of patient’s socio-environmental context that should streamline Consumer Health Informatics (CHI) application development and deployment. However, the proposed framework does not consider CHI applications as potential actors of the healthcare digital information flow, within the so-called “health-IT ecosystem” envisaged by the Health Information Exchange movement.2 In this letter, we propose a framework for the integration of CHI applications into the “health-IT ecosystem”. This is in line with the American Medical Association’s vision for improving electronic health record (EHR) usability by facilitating “Digital and Mobile Patient Engagement” through “interoperability between patient’s mobile technology and the EHR”.3 We believe that such integration is a fundamental pre-requisite for CHI applications that, together with the holistic “patient-work” design perspective, will lead to full adoption and effectiveness for better patient care. In the healthcare switch to a patient-centered and home-settled paradigm, self-care and self-management add new expanded responsibilities for patients, families, and communities. CHI has the potential to enable this scenario.1
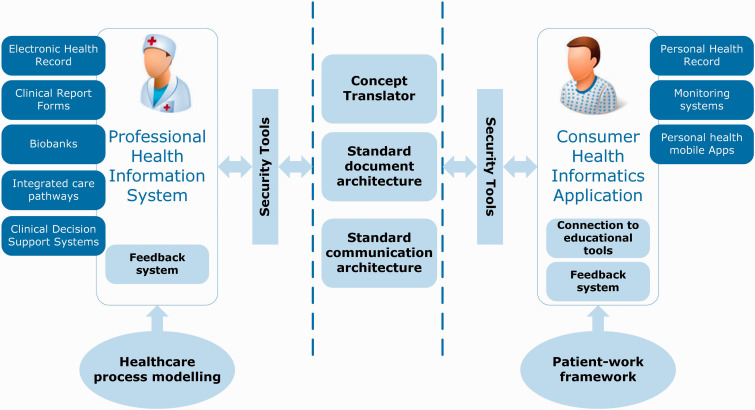
CHI applications produce health information that is potentially relevant for patient’s assessment, physiological monitoring, diagnosis, therapy, and rehabilitation, and that could be beneficially integrated into health information systems, such as the EHR. This would avoid duplication and redundancy, as well as potential errors and misunderstanding. Figure 1 shows the architecture that we propose to ensure the direct exchange between CHI applications and health information systems.
Figure 1:
General architecture for the data exchange among CHI applications and health information systems.
The patient-work framework1 is an essential building block of the architecture, ensuring that the CHI application is designed for and around the patient. However, other building blocks are needed to allow the interaction between CHI applications and health information systems, including the EHRs:
Concept Translator: In the CHI-EHR exchange domain, the technical solution should take into account the “health literacy” issue. The efficacy of patient/doctor communication and the degree of the patient’s engagement in decision-making depends on the patient’s understanding of the healthcare process.4 CHI applications should ensure the proper concept mapping from the healthcare specialist domain to the patient/family domain. This is represented by the “concept translator” that can be implemented relying on experiences like the Consumer Health Vocabulary.
Security Tools: Data protection policies should be transparent and clearly stated as part of a patient’s education and awareness.4
Standard Document and Communication Architectures: Both professional health information systems and CHI applications should follow a model-based development. The patient-work framework1 grounds the development of CHI applications, while healthcare process modelling should be at the basis of healthcare information system development. This will ensure the necessary flexibility to face different clinical settings (EHR-side) or socio-technical environments (patient-side). Communication standards for EHR-Personal Health Record (PHR) data exchange can be adapted for CHI applications. For example, the X-PHR Integrating the Healthcare profile provides the general transaction framework for EHR-PHR information exchange; the HL7 Clinical Document Architecture release 2 “Personal Health Monitoring Record” drafts a standard document architecture for exchanging personal monitoring information.
Connection to Educational Tools. The application should include the connection to qualified information sources, such as MedlinePlus and PubMed.
Feedback System. Appropriate logging systems able to collect user’s experience and feedback on the application should be included.
The implementation of such building blocks ensures, as essential requirements for the interaction process, that (1) the information exchanged is accurate, as described in the ISO 13606 standard regarding healthcare information exchange, thus, preserving the original meaning intended by the author; (2) data are protected, accounting for confidentiality (protection from unwanted access), integrity (transmission and maintenance of accurate data), and availability (data accessibility and usability upon demand by authorized request), as well as accountability (traceability of responsibility on data content) and disaster recovery; (3) flexibility is guaranteed by interoperability, according to the “not-one-fit-all” concept,1,2,4 and considering both technological (eg, standard communication architectures), and semantic (eg, shared terminologies/ontologies) interoperability; (4) patient education is supported to both enhance “health literacy” and to create a “culture of custodianship”4 related to the nature of personal health information; and (5) research and evidence-based practice can be prompted thanks to the availability of information necessary for establishing the benefits and limitations4 of the CHI-EHR two-way exchange.
The strong need of shared decision-making and patient’s contribution to their health records is demonstrated by initiatives, like OpenNotes,5 already allowing a more effective information exchange between patients and healthcare professionals. Complementary to these, the design, development, and deployment of CHI applications able to communicate with health-IT ecosystems through the proposed architecture will be the key for patient engagement in self-management and self-care.
REFERENCES
- 1. Valdez RS, Holden RJ, Novak LL, et al. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc. Published Online First: 14 August 2014. doi:10.1136/amiajnl-2014-002826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. The Office of the National Coordinator for Health Information Technology. Connecting Health and Care for the Nation: A Ten Year Vision to Achieve Interoperable Health IT Infrastructure. Published Online First: 2014. http://healthit.gov/sites/default/files/ONC10yearInteroperabilityConceptPaper.pdf. Accessed August 4, 2014. [Google Scholar]
- 3. American Medical Association. Improving Care: Priorities to Improve Electronic Health Record Usability. 2014. http://www.ama-assn.org/ama/pub/ama-wire/ama-wire/post/8-top-challenges-solutions-making-ehrs-usable. Accessed September 17, 2014. [Google Scholar]
- 4. Wiljer D, Urowitz S, Apatu E, et al. Patient accessible electronic health records: exploring recommendations for successful implementation strategies. J Med Internet Res. 2008; 10: e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walker J, Darer JD, Elmore JG, et al. The road toward fully transparent medical records. N Engl J Med. 2014; 370: 6–8. [DOI] [PubMed] [Google Scholar]