Abstract
Objectives
Individuals with neck pain experience disrupted grip force control when performing manipulative tasks. Manipulative physical therapy might decrease pain and change the activity of surrounding muscles; however, its effect on upper limb motor control remains undetermined. This study aims to analyze the effects of cervical manipulation on pressure pain threshold (PPT), upper extremity muscle activity along with grip force control in individuals with neck pain.
Methods
Thirty subjects with neck pain were instructed to grasp and lift an object before and after cervical (n = 15) or sham (n = 15) manipulation. The patients’ PPT, electromyographic (EMG) activity of the upper extremity/scapular muscles, and grip force control were analyzed before and after one session of manipulation.
Results
No significant differences were found in the grip force control, PPT and EMG activity variables between groups.
Discussion
These results suggest that a single session of cervical manipulation may not modify upper limb motor control, more specifically grip force control and EMG activity, in patients with cervical pain. Future studies should investigate potential changes in grip force control in patients with different features of neck pain and/or by applying long-term treatment.
Level of Evidence
1b.
Keywords: Grasping, lifting, neck pain, thrust, grip force control, EMG
Introduction
It is known that approximately 70% of individuals will have cervical pain at some point in their lives [1], and a large part of these patients will develop chronic symptoms [2] and functional disability [3]. Even though the cause of cervical pain can be associated with degenerative processes such as osteoarthritis or diseases identified in imaging examinations [4], the main cause is usually unknown and cannot be clearly established [4,5]. There is evidence that neck pain causes alterations in motor activity [6], leading to changes of motor control strategies during static and dynamic activities [7]. Regardless of the main cause, functional disability can be the result of motor changes affecting the ability to manipulate objects properly.
Grip force control consists of applying adequate force to neither deform the object nor allow it to slip from the grasping fingers. This applied force depends on the object’s characteristics (weight, shape, and weight distribution), speed of movement, and the friction coefficient that exists between the object’s contact surface and the person’s fingertips [8–10]. Studies involving grip force control usually evaluate grip force at lift-off (GFLO) and grip force peak (GFP), which represent anticipatory (planned force) and feedback-based grip force control, respectively [11,12]. It has been suggested that the increased GFP observed in patients with cervical pain may be due to pain, disrupted sensorial information or both [13]. For example, patients with neck and upper extremity pain showed unnecessary high levels of grip force compared to healthy individuals, while repeatedly elevating and holding an object [13,14]. Therefore, an intervention technique that improves these symptoms, especially decreasing pain, might change grip force control in these patients.
Vertebral manipulation is defined as the passive application of a high-velocity, low-amplitude (HVLA) thrust at the limit of the available joint movement [15,16]. This technique has been proposed for improving neck pain, function, and satisfaction of patients with cervical pain [5,17]. In addition, studies have shown that this technique modifies the activity of upper extremity muscles [18–20], which may lead to changes in grip force control. Studying the effects of cervical manipulation on both activities of upper extremity muscles and grip force control may benefit the rehabilitation process in patients with cervical pain.
Therefore, the purpose of this study was to determine the effects of cervical manipulation on pressure pain threshold (PPT), the activity of upper extremity muscles and on grip force control in patients with neck pain during a functional task of grasping and lifting an object. Particularly, PPT, EMG activity of the muscles, and different variables of grip force control were evaluated before and after cervical manipulation in thirty patients with neck pain. Based on the aforementioned studies, we hypothesized that cervical manipulation will improve PPT and decrease the magnitude of EMG activity and grip force control.
Methods
Subjects
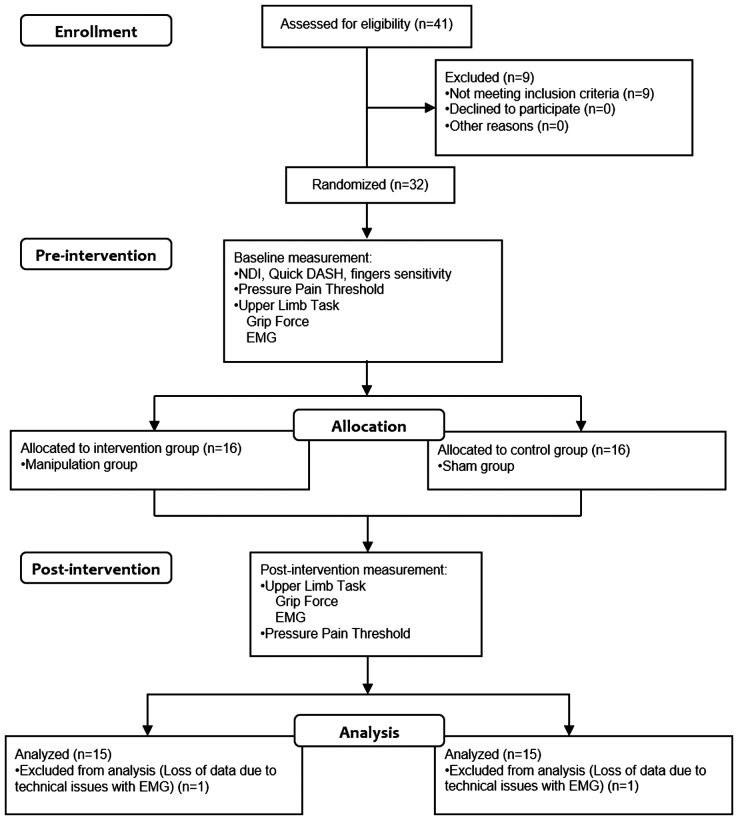
The sample included 30 individuals between 18 and 50 years old (27 females and three males, mean age 27.90 ± 4.87 years). The sample size was calculated based on previous studies using a G*Power 3 software [21]. Only nine subjects in each group were enough to detect statistically significant differences between conditions in grip force peak [13], with 80% of power and 95% of confidence. We included 15 subjects in each group (see details below) to account for the potential differences in the subjects’ characteristics and experimental tasks between the previous study [13] and the present investigation (Figure 1). The definitions of neck pain and chronic pain followed International Association for the Study of Pain (IASP) criteria [22]. The sample included individuals who fulfilled the following criteria: a history of three or more episodes of cervical pain in the last three months, with or without pain radiating to the upper extremities. The exclusion criteria included: (1) a previous history of rheumatic disease, cervical myelopathy, tumors, central or peripheral neurological disorders, (2) a history of major trauma, fracture or surgery in the cervical region, shoulder and/or upper extremities, (3) signs of nerve root compression such as major muscle weakness affecting upper extremity, decrease in biceps and triceps reflexes, decreased sensitivity in upper extremity dermatomes, and (4) ‘red flags’ against cervical manipulation such as vertebrobasilar insufficiency, vertigo and diplopia [23]. All participants were informed about the study’s objectives and procedures and signed the informed consent form approved by the local Ethics Committee (protocol 206/2011). This study was registered in a recognized Registry of Clinical Trials.
Figure 1.
Participant flow chart.
Clinical examination
An initial interview, clinical evaluation before and after treatment, and data processing of all participants was conducted by an experimenter who was blinded to the treatment allocation. A physical therapist who performed the treatments (placebo and manipulation, see below) had no knowledge of the above-mentioned data contents. Tactile sensitivity was evaluated with Semmes-Weinstein monofilaments (Touch-Test™ 5-Piece Hand Kit Sensory Evaluators, North Coast Medical Inc.; Gilroy, California, USA) [24], since reduction or loss of fingertip tactile sensitivity negatively affects grip force control [25,26]. The monofilaments were applied three times bilaterally to the tips of the index fingers and thumbs. Detecting the filament’s touch in two of the three trials was considered the sensorial threshold and the average scores of all sites were used for analysis [27]. For this evaluation, the following monofilaments were used: 2.83, 3.61, 4.31, 4.56, and 6.65, where 2.83–3.61 correspond to a normal sensory threshold for hand function use and 6.65 to an abnormally high-threshold hindering the ability to recognize objects [28].
In order to characterize the sample, the individuals responded to the Neck Disability Index (NDI) and the Disabilities of Arm, Shoulder and Hand questionnaire (Quick DASH). The NDI questionnaire score ranged from 0, no activity limitations, to 50, complete activity limitation. The Quick DASH questionnaire score ranged from 0, no disability, to 100, greatest disability. If the subject reported bilateral cervical pain, then, the most affected side, i.e. the side with greater pain sensation, was considered for EMG electrode placement and for grip force control data derived from the lifting task.
Instrumentation
Pressure pain threshold
The PPT, defined as the minimum pressure (force) necessary to cause pain [29], was measured using a digital pressure algometer (JTECH Commander, Salt Lake City, UT, USA) with a 1-cm wide tip. A digital readout of the pressure applied to the subject’s skin was shown in Newton (N) and the peak pressure was registered automatically (see details below).
EMG
We evaluated the EMG activity of the muscles via electromyography (EMG System of Brazil®, model 811C, SP, Brazil) with an analog output, gain of 2000, band-pass filter from 23 to 500 Hz, Common Mode Rejection Ratio (CMRR) greater than 80 dB, and differential amplifier. All signals reached a computer via a digital/analog acquisition system (model PCI 6259, National Instruments, USA) with a frequency of 1000 Hz and resolution of 16 bits, acquired in a LabView environment (SignalExpress® 2010, Version 4.0. 0 for Windows®, National Instruments, USA). Disposable surface electrodes (3 M®, 223BRQ, Sumaré, SP, Brazil) were placed on the skin of individuals with an inter-electrode distance of 20 mm, after cleansing with 70% alcohol and, when necessary, the area was shaved. In order to evaluate the EMG activity in the ipsilateral upper extremity of the neck pain, surface electrodes were fixed over the following muscles: lower trapezius (LT), upper trapezius (UT), anterior deltoid (AD), biceps brachii (BB), triceps brachii (TB), wrist extensors (WE), wrist flexors (WF), and adductor pollicis (AP). A reference electrode was fixed over the spinous process of the seventh cervical vertebra. All the procedures described above were performed by the same experimenter and followed Surface ElectroMyoGraphy for the Non-Invasive Assessment of Muscles (SENIAM) standards [30].
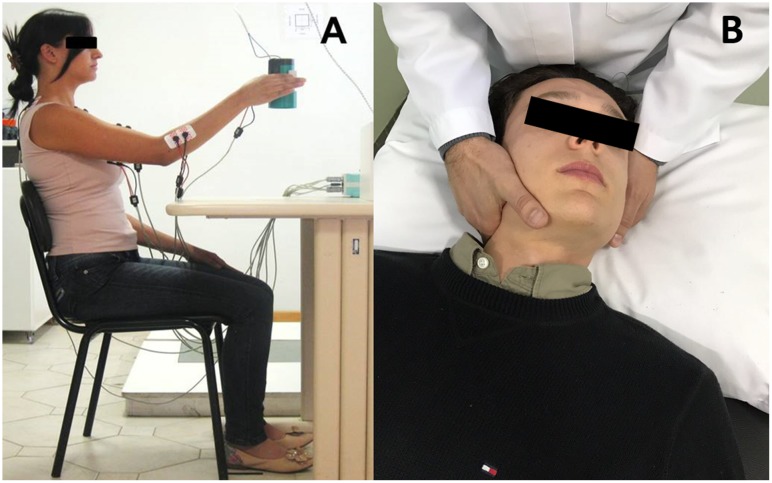
The experimental cup
A cylindrical, plastic object (6 cm in diameter, 13 cm in height, and 305 g in weight) was used to evaluate thumb-index pinch force control (Figure 2). The object, designed in the shape of a cup, was equipped with a piezoelectric force sensor (model 208CO3, PCB Piezotronics Inc.; Depew, New York, USA) installed at its center. Two aluminum pads (2.5 cm wide and 3.8 cm long) connected to the force sensor with two metallic projections were used as grasping surfaces. A triaxial piezoelectric accelerometer (model 333B32, PCB Piezotronics Inc.; Depew, New York, USA) was affixed to the cup to register acceleration in the x-, y-, and z-planes. Accelerometer and force sensor data were powered with two signal conditioners (ICP R Sensor Signal Conditioner, model Y482A22, and Line-Powered ICP R Signal Conditioner, model 484B06, PCB Piezotronics Inc.; Depew, New York, USA). The force and accelerometer signals were sampled at 100 Hz with a 16-bit analog-digital converter (National Instruments; Austin, Texas, USA) and stored for further analysis. Data collection were performed in LabView Signal Express (Version 2.5.1 for Windows, National Instruments; Austin, Texas, USA).
Figure 2.
(A) Gripping and lifting task. (B) High-velocity, low-amplitude cervical manipulation.
Experimental procedure
The PPT was evaluated bilaterally by first marking the specific points on the skin with a demographic pencil. These points were marked on the middle third of the upper trapezius (UT) muscle and the medial third of the middle deltoid (MD) muscle, and over the lateral epicondyle (LE) as described elsewhere [29,31]. The patients were in supine position with their arms at their sides. The evaluator applied gradual force perpendicularly through the algometer to the skin’s surface. The subjects were instructed to indicate the moment when the pressure sensation became painful by saying the word ‘pain’. Hence, the experimenter stopped to apply pressure and the maximum force applied to that point was automatically registered by the algometer. Three measurements were made with 30-s intervals. This evaluation was performed before and 15 min after the intervention. This 15-min lag between the manipulation and the PPT post-test corresponded approximately the time it takes for the subjects to complete the grip force control task (see below).
The grip force control data from the gripping and lifting task were evaluated in the ipsilateral upper extremity of the most affected side. Prior to the beginning of the object-lifting task, alcohol swaps were used to clean the subjects’ fingertips and the metallic surfaces of the object. The participants sat on an adjustable chair in front of a table, with their trunk straight and their feet resting on the floor. The elbow of the evaluated side was flexed at approximately 30°, with the forearm pronated and the wrist in neutral position while resting on the table. Subjects were required to handle the test object by opposing their thumb and index finger while placed centrally on the grasping surfaces, which had been marked previously. The task consisted of lifting the test object vertically from the table; holding it at a point of 20 cm above the table; and then, after 5 s, returning the object to its initial position. Subjects were instructed to perform the lifting task as naturally as possible, starting with the experimenter’s verbal command ‘go’ and returning the object to its starting position with the command ‘return’. The participants performed five familiarization trials before the beginning of data collection which included six repetitions of grasping and lifting the test object.
After performing the task, the individuals were allocated through block randomization to either the experimental group (manipulation) or the control group (sham manipulation). The randomization arrangement was generated via a web-based program at Randomization.com [32]. A physical therapist with 10 years of experience in orthopedic manipulative physical therapy performed the procedure according to the group in which the subject was allocated. The subjects in the experimental group received high-velocity, low-amplitude (HVLA) cervical manipulation technique, also denominated as thrust or grade V manipulation [16]. With the subject in supine and the cervical spine in a neutral position, the therapist’s index finger of one hand was placed on the level of the fifth cervical vertebra (C5), while the other hand contacted the subject’s chin of the opposite side. The physical therapist performed a lateral bending of the cervical spine along with axial-rotation of it to the contralateral side up to the end of the available movement. From this point, the physical therapist applied further cervical rotation subtly within a small range of movement using both hands. It was expected, then, to hear a small ‘crack’ with the manipulation, which is due to cavitation phenomenon [33]. If this did not occur, the physical therapist performed the procedure once more. If there was still no success on the second attempt, the patient was excluded from the study. The direction of cervical rotation was selected according to the painlessness and of opposite motion rules [34,35], i.e. the cervical rotation movement could not cause painful symptoms. For the control group, the physical therapist simulated a HVLA manipulation technique by positioning his hands on the subjects’ cervical/head as previously described for the manipulation group; however, only the cervical rotation was performed without applying any tissue tension at the end of movement, which did not result in cavitation.
An evaluator blinded to the randomization and the procedures performed the data collection pre- and post-intervention. Prior to removing the electrodes, the experimenter performed the PPT evaluation again at the above-mentioned regions.
Data processing
Descriptive measurements were calculated (means and standard deviations) for the relevant subject characteristics: gender, age, and dominance. The NDI, Quick DASH scores, and the mean PPT values of the pre- and post-intervention as well finger sensitivity measures pre-intervention were entered in Microsoft Excel (2007) and stored for statistical analysis.
EMG
To calculate the integral of EMG ( ), first the raw data were filtered with second-order Butterworth band-pass filter (30–400 Hz) [36]. Then, the EMG data were aligned by the moment of the object lift-off (see details below) and the six trials of EMG activity pre-and post-intervention was averaged separately for each participant. The
), first the raw data were filtered with second-order Butterworth band-pass filter (30–400 Hz) [36]. Then, the EMG data were aligned by the moment of the object lift-off (see details below) and the six trials of EMG activity pre-and post-intervention was averaged separately for each participant. The  during the object lifting task was demarcated within specific time intervals (from x0 to x1) based on the acceleration signals. They were: (1) pre-lifting interval (preL), including the time interval of 300 ms just before the object’s lifting (first, subtle increase in the vertical acceleration). This included the time interval where the patients reached, contacted the object with their fingertips, and developed the force to lift it; (2) the post-lifting interval phase (postL) encompassing the time between the object’s lift-off to the end of movement at which the acceleration returned to approximately zero. The pre- and post- lifting intervals represent the feedforward and feedback control of the movement to accomplish the object’s lifting task, respectively. These two
during the object lifting task was demarcated within specific time intervals (from x0 to x1) based on the acceleration signals. They were: (1) pre-lifting interval (preL), including the time interval of 300 ms just before the object’s lifting (first, subtle increase in the vertical acceleration). This included the time interval where the patients reached, contacted the object with their fingertips, and developed the force to lift it; (2) the post-lifting interval phase (postL) encompassing the time between the object’s lift-off to the end of movement at which the acceleration returned to approximately zero. The pre- and post- lifting intervals represent the feedforward and feedback control of the movement to accomplish the object’s lifting task, respectively. These two  intervals (preL and postL), were corrected by their respective EMG activity at the baseline, which was integrated (
intervals (preL and postL), were corrected by their respective EMG activity at the baseline, which was integrated ( ) at the beginning of data collection with the participants in resting position. The integration intervals (from y0 to y1) of the
) at the beginning of data collection with the participants in resting position. The integration intervals (from y0 to y1) of the  have identical time intervals of their respective pre- and post-lifting
have identical time intervals of their respective pre- and post-lifting  according to the equation:
according to the equation:
The  is the integral of the EMG within the time intervals for pre- and post-lifting minus their respective
is the integral of the EMG within the time intervals for pre- and post-lifting minus their respective  baseline activity.
baseline activity.
In order to compare  between groups, they were normalized as follows: for each participant, the maximal absolute value of a given
between groups, they were normalized as follows: for each participant, the maximal absolute value of a given  for a given muscle across the two-time intervals (pre- and post-lifting) and conditions (pre- and post- manipulation) was determined. All other values of this particular participant and muscle (two time intervals and two conditions = 4) were divided by this maximal value [37,38]. The range values of
for a given muscle across the two-time intervals (pre- and post-lifting) and conditions (pre- and post- manipulation) was determined. All other values of this particular participant and muscle (two time intervals and two conditions = 4) were divided by this maximal value [37,38]. The range values of  intervals were therefore limited from −1 to 1. Negative and positive values were associated with inhibition and activation of muscle activity, respectively.
intervals were therefore limited from −1 to 1. Negative and positive values were associated with inhibition and activation of muscle activity, respectively.
Grip force control
From the collected force and accelerometer, the following variables is identified and measured: (1) GFLO in Newton (N), which is the thumb-index pinch force applied at the instant the object leaves the surface of the table and represents planned grip force control [12]; the moment of object lift-off was indicated by the acceleration signal; (2) load force peak (LFP), defined as the maximum load force achieved during object lifting, calculated as LF = m × (AccZ + g), where load force peak (LF), in N, was calculated by multiplication of the object’s mass (m), in kg, by the sum of the recorded vertical acceleration (AccZ) and gravity (g) [39–41]. Loading components acting in the direction of the applied grip force (X-axis) and sagittally (Y-axis) to it were not included in the calculation since the tasks consisted of vertical liftings; (3) Grip Force Peak (GFP; N), defined as the maximum thumb-index pinch force achieved during object lifting, indicating grip force control which depend on previous sensorial feedback during the dynamic phase (lifting) [11]. All data processing were performed by an experimenter blinded to the randomization and intervention. All signals are processed in Matlab (version 7.10 R2010b, The MathWorks®, USA).
Statistical analysis
Independent t-tests were used to compare the groups regarding, age, NDI, Quick DASH, scores, and fingers sensitivity measures from the initial clinical evaluation as shown in (Table 1).
Table 1.
Clinical features at pre-test.
| Groups | Manipulation |
Sham |
||||
|---|---|---|---|---|---|---|
| Clinical features | SD | SD | ||||
| Age (years) | 28 | ±3.80 | 27 | ±5.74 | ||
| Gender (n) | 2 Male | 13 Female | 1 Male | 14 Female | ||
| Laterality (n) | 1 Left | 14 Right | 2 Left | 13 Right | ||
| Task Side | 10 D | 5 ND | 11 D | 4 ND | ||
| SWMT (threshold) | 3.01 | ±0.28 | 3.14 | ±0.33 | ||
| Pain duration (months) | 35 | ±51.62 | 26 | ±19.45 | ||
| Quick Dash (score) | 32.43 | ±61.58 | 25.01 | ±14.24 | ||
| NDI (score) | 11.93 | ±4.30 | 11.73 | ±3.55 | ||
Notes: SD: Standard Deviation; QuickDASH: Disabilities of Arm, Shoulder e Hand questionnaire; NDI: Neck Disability Index; SWMT: Semmes-Weinstein Monofilament Test; Task Side: refers to Dominant (D) and Non-Dominant (ND) hand used in the grip task; number (n).
Analyses of covariance (ANCOVA) [42], controlling for the baseline result, was performed to evaluate the effect of cervical manipulation on PPT, EMG integrals ( ) in both intervals (pre- and post-lifting) and the grip force control variables (GFLO, LFP, and GFP). The pre-test and post-test means were used as co-variables and dependent variables, respectively. The group was used as fixed factor. To account for the relatively large number of comparisons due to the number of co-primary dependent variables, we lowered the significance level to p < 0.01 for the PPT and EMG integral statistical tests. This significance level was chosen based on the overall experimental error rate of approximately 10% for the PPT variables (6) and 15% for the EMG integrals variables (eight pre- and eight post-lifting). In other words, the chance of at least one of the tests within each pool of dependent variables being false-positive (Type-I error) was 10 and 15% or less, respectively. For the grip force control variables (3), the significance level was set at p = 0.05. The statistical analysis was performed in SPSS 20.0.
) in both intervals (pre- and post-lifting) and the grip force control variables (GFLO, LFP, and GFP). The pre-test and post-test means were used as co-variables and dependent variables, respectively. The group was used as fixed factor. To account for the relatively large number of comparisons due to the number of co-primary dependent variables, we lowered the significance level to p < 0.01 for the PPT and EMG integral statistical tests. This significance level was chosen based on the overall experimental error rate of approximately 10% for the PPT variables (6) and 15% for the EMG integrals variables (eight pre- and eight post-lifting). In other words, the chance of at least one of the tests within each pool of dependent variables being false-positive (Type-I error) was 10 and 15% or less, respectively. For the grip force control variables (3), the significance level was set at p = 0.05. The statistical analysis was performed in SPSS 20.0.
Results
No patient was excluded from the study due to lack of cavitation phenomenon caused by the cervical spine manipulation or because of intolerance to the maneuver. Two patients were excluded (one from each group) from this study due to technical difficulties with the EMG signals (refer to the flow chart, Figure 1). The independent t-test showed no significant intergroup differences for age (t = −1.01, p = 0.32), NDI (t = −0.13, p = 0.89), Quick DASH (t = −0.45, p = 0.65) scores, and fingers sensitivity (t = 1.13, p = 0.26), which demonstrates that the two groups were homogenous (Table 1).
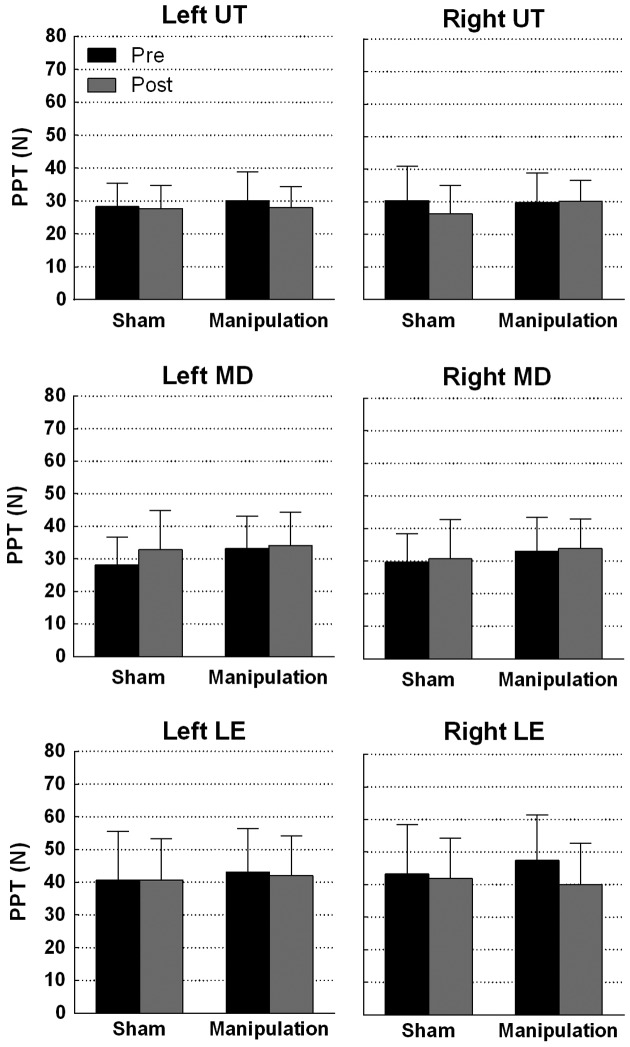
No statistically significant differences were found in PPT between the control and experimental groups: left UT (F = 0.21, p = 0.64); right MD (F = 0.03, p = 0.95); left MD (F = 3.98, p = 0.05); right LE (F = 3.45, p = 0.07) and left LE (F = 0.05, p = 0.81) (Figure 3). The right UT approached significance (F = 7.46, p = 0.01).
Figure 3.
Means and standard deviations of the pressure pain threshold (PPT, N). There were no significant differences between the Sham and Manipulation groups: right upper trapezius (UT) point. Left upper trapezius (UT), the right and left middle deltoid (MD), and the right and left lateral epicondyle (LE) points were not significantly different between groups.
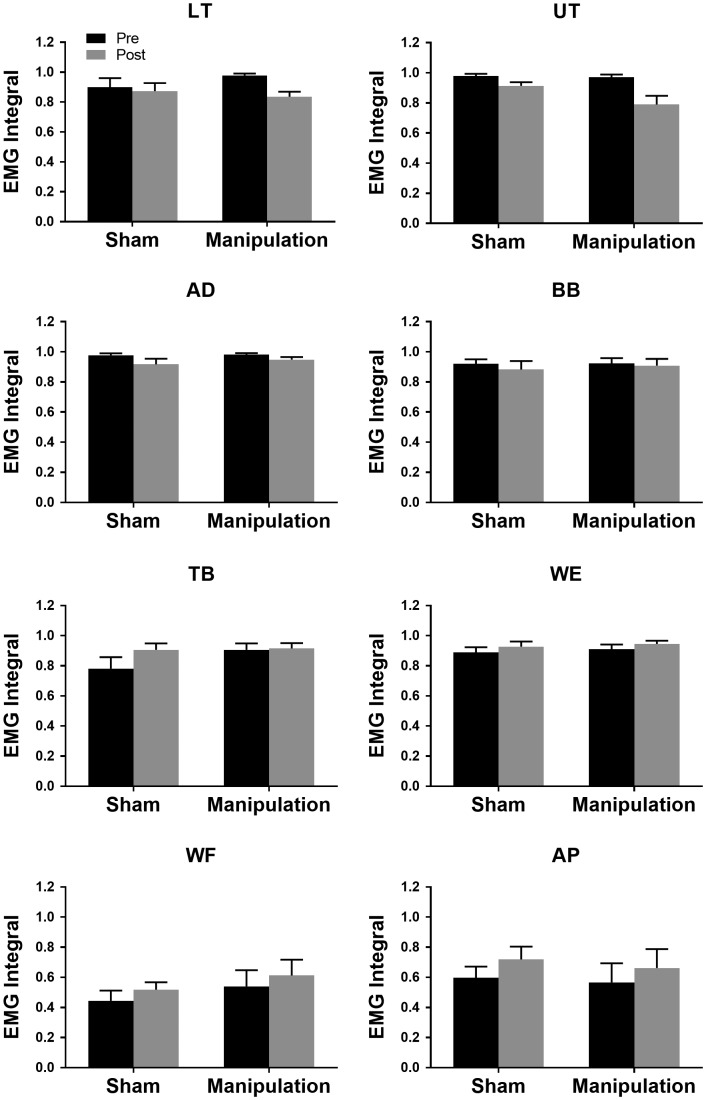
ANCOVA did not detect a statistically significant difference between groups in the  at pre-lifting interval: UT (F = 0.45, p = 0.50); LT (F = 0.84, p = 0.36); AD (F = 0.71, p = 0.40); BB (F = 0.40, p = 0.53); TB (F = 1.02, p = 0.32); WF (F = 0.05, p = 0.82); WE (F = 0.09, p = 0.76); AP (F = 0.18, p = 0.77) and at the post-lifting interval: UT (F = 5.19, p = 0.03); LT (F = 0.04, p = 0.83); AD (F = 0.71, p = 0.40); BB (F = 0.15, p = 0.70); TB (F = 0.66, p = 0.42); WF (F = 0.08, p = 0.77); WE (F = 0.57, p = 0.45); AP (F = 0.09, p = 0.76) (Figure 4).
at pre-lifting interval: UT (F = 0.45, p = 0.50); LT (F = 0.84, p = 0.36); AD (F = 0.71, p = 0.40); BB (F = 0.40, p = 0.53); TB (F = 1.02, p = 0.32); WF (F = 0.05, p = 0.82); WE (F = 0.09, p = 0.76); AP (F = 0.18, p = 0.77) and at the post-lifting interval: UT (F = 5.19, p = 0.03); LT (F = 0.04, p = 0.83); AD (F = 0.71, p = 0.40); BB (F = 0.15, p = 0.70); TB (F = 0.66, p = 0.42); WF (F = 0.08, p = 0.77); WE (F = 0.57, p = 0.45); AP (F = 0.09, p = 0.76) (Figure 4).
Figure 4.
The means and standard errors of the EMG integrals during the post-lifting interval. There was a tendency of decreased activity for proximal muscles (LT and UT) and increased activity for distal muscles (WF and AP) after the intervention. However, no significant differences were found between the groups for any of the muscles: Upper trapezius (UT), lower trapezius (LT), anterior deltoid (AD), biceps brachii (BB), triceps brachii (TB), wrist extensors (WE), wrist flexors (WF), and adductor pollicis (AP).
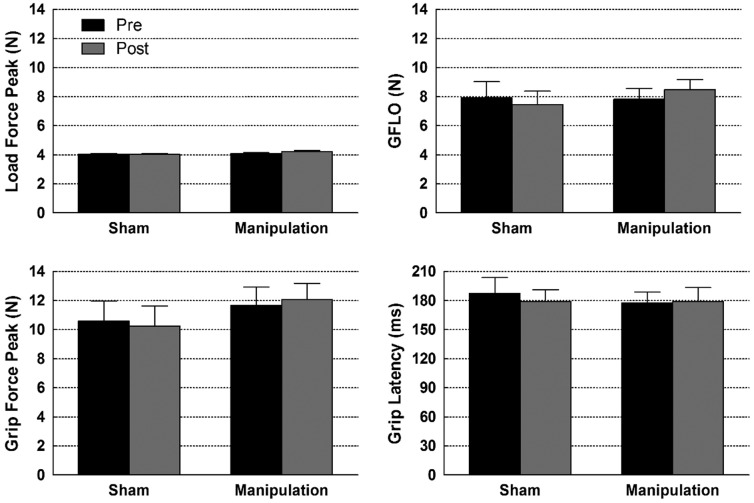
No statistically significant inter-group difference was identified in the grip force control variables: GFLO (F = 4.02, p = 0.05); GFP (F = 1.04, p = 0.31) (Figure 5).
Figure 5.
There were no significant differences in the grip force control variables between groups (Sham and Manipulation) pre- and post-intervention, during grasping and lifting the object. Means and standard deviations are shown. Grip force at lift-off (GFLO).
Discussion
The task paradigm used in this study was intended to replicate a common upper extremity functional task during the daily activities. This would allow us to identify potential motor control-related changes due to the effect of cervical manipulation in people with cervical pain. The findings of our study refute the hypothesis that a single session of cervical manipulation will affect the pain threshold, EMG activity and motor control of the upper extremity after the maneuver.
The PPT approached significance in the right UT point only during the post-lifting activity; however, no apparent change could be noted between pre-and post-manipulation for the experimental group (Figure 3 – left-upper panel). Increased pain threshold would indicate an immediate hypoalgesic effect as the result of the intervention. Our results differ from those by Ruiz-Saez, Fernandez-de-las-Penas [43], who found an increase in the PPT in the upper trapezius region after cervical manipulation as well as from other studies that found effects of the manipulation in distal sites from the maneuver [31,44]. In these studies, the cervical manipulation increased PPT in shoulder and epicondyle regions as well. The discrepancy between this and our study may be related to the type of population involved in the study. In our study, we selected individuals with chronic cervical pain and without signs of radiculopathy whereas in the above-mentioned studies the authors recruited asymptomatic individuals [31] and patients with lateral epicondylalgia [44]. Therefore, the effects of cervical manipulation on pain may depend on the pathophysiological characteristics of the cervical pain, especially, the location of the nociceptive inputs may influence the effects of manipulative therapy.
We found no changes in the EMG activity either pre- or post-lifting task for the group that received the manipulation. Previous studies have shown conflicting results in terms of EMG activity after cervical manipulation. For instance, Camargo and his colleagues showed increased EMG amplitude in the deltoid muscle after C5/C6 cervical manipulation [45]. This change was observed only during long-lasting (30 s) isometric contractions. For short isometric and isotonic contractions, no changes were observed in the deltoid muscle. In our study, the activity of the upper extremity muscles was measured during a common daily task which provoked isotonic contraction and did not require great demand for muscle activity. Thus, it is possible that for tasks that involve greater amount of muscle contraction (activity) some effects of cervical manipulation can emerge for people that suffer from cervical pain. This may be a good topic for future studies since these patients complain about cervical pain during task that requires greater muscular effort.
In the present study, cervical manipulation did not show significant effects on the variables involved in grip force control. These results support those of previous studies, which did not demonstrate modification in motor function in patients with cervical pain after cervical mobilization [46]. Previous studies have demonstrated that patients with cervical and upper extremity pain applied high levels of grip force compared to asymptomatic individuals while lifting an instrumented object [13]. These authors observed that individuals with neck pain applied a mean maximum force of 20 N during the lifting phase (GFP), whereas the values for the asymptomatic group oscillated at approximately 17 N. In the present study, the mean GFP was between approximately 10 and 12 N for both the control and experimental groups. These values are similar to those found for healthy individuals in previous studies using similar experimental methods [47]. In addition, it is known that the reduction or loss of fingertip tactile sensitivity negatively affects grip force control [25,26] and, at the same time, the sample of patients included in this study exhibited their fingertip sensitivity levels close to normality (Table 1). Therefore, the potential alterations in grip force control is more likely to be found in patients who, in addition to neck pain, also experience upper extremity impairment such as pain or paresthesia (radiculopathy). The effects of cervical manipulation in patients with these characteristics should be investigated in future studies. Alternatively, subjects with neck pain may require longer time for a complete recovery in terms of changes in grip force control. Higher grip forces can be a sign of a learned behavior [48,49] in patients with neck pain, which may require a longer time to return to normative after the recovery. For instance, subjects with history of neck pain, but free of symptoms for more than a year did not present with deficits in grip force control as compared to those with neck pain or healthy controls [13]. Nevertheless, we only investigated the short-term effects of cervical manipulation in subjects with frequent episodes of neck pain. Therefore, future studies should investigate the long-term effects of cervical manipulation and whether other alternative treatments are needed to trigger changes in grip force control measures.
Conclusion
The results of the present study indicate that one single session of cervical manipulation in subjects with cervical pain might not immediately change the PPT, muscle activity of upper extremity and grip force control. Thus, the effect of this technique on PPT and upper extremity motor control continue in debate, which encourage more comprehensive studies addressing the effects of cervical manipulation for patients with neck pain. Future studies may address the long-term effect of manipulation, additional and combined treatments as well as other outcome measurements such as pain on the cervical vertebras and range of movement. In addition, they may separate group of patients with neck pain based on specific causes, symptoms and physiopathological phase. Finally, from our perspective and in face of all these experimental challenges, the results of the present study combined with the findings of the previous studies does not invalidate the use of cervical manipulation for patients with neck pain in clinical sites.
Disclosure statement
The authors report no declarations of interest.
Notes on contributors
Marcelo A. Bracht is a physical therapist, clinical specialist in orthopedics and certified manual therapist. He is an adjunct professor in the Department of Physical Therapy at Santa Catarina State University and PhD student in neuroscience at Santa Catarina Federal University. His research interest is orthopedics and manipulative physical therapy.
Ana C. Buogo Coan is a physical therapist specialist in Pilates and acupuncture. She was a student of Physical Therapy at Santa Catarina State University and a clinical specialization student in acupuncture at the CIEPH Institute of Studies. Her research interest is orthopedics and pain processing.
Abdalghani Yahyais a doctor in physical therapy and PhD candidate in the Department of Physical Therapy and Rehabilitation Science at University of Kansas Medical Center. His research interest is in neurological physical therapy. Specifically, areas targeting hand function, proprioception, grip force control, and physical activity in people with diabetes.
Marcio J dos Santos is an assistant professor and director of the Applied Motor Control laboratory in the Department of Physical Therapy and Rehabilitation Science at University of Kansas Medical Center. His research interests are in the areas of physical therapy and motor control, more specifically, gait, postural and grip force control analyses in patients with orthopedic and neurologic conditions.
References
- [1].Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Carroll LJ, Hogg-Johnson S, van der Velde G, et al. . Course and prognostic factors for neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2):S87–S96. [DOI] [PubMed] [Google Scholar]
- [3].Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain. 1998;77(1):1–13. [DOI] [PubMed] [Google Scholar]
- [4].Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin N Am. 2011;22(3):367–382, vii. [DOI] [PubMed] [Google Scholar]
- [5].Childs JD, Cleland JA, Elliott JM, et al. . Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38(9):A1–A34. [DOI] [PubMed] [Google Scholar]
- [6].Bank PJM, Peper CE, Marinus J, et al. . Motor consequences of experimentally induced limb pain: a systematic review. Eur J Pain. 2013;17(2):145–157. [DOI] [PubMed] [Google Scholar]
- [7].Falla D, Farina D. Neuromuscular adaptation in experimental and clinical neck pain. J Electromyogr Kinesiol. 2008;18(2):255–261. [DOI] [PubMed] [Google Scholar]
- [8].Bensmail D, Sarfeld AS, Fink GR, et al. . Intermanual transfer of sensorimotor memory for grip force when lifting objects: the role of wrist angulation. Clin Neurophysiol. 2010;121(3):402–407. [DOI] [PubMed] [Google Scholar]
- [9].Johansson RS. Dynamic use of tactile afferent signals in control of dexterous manipulation. Adv Exp Med Biol. 2002;508:397–410. [DOI] [PubMed] [Google Scholar]
- [10].Cole kJ, Abbs JH. Grip force adjustments evoked by load force perturbations of a grasped object. J Neurophysiol. 1988;60(4):1513–1522. [DOI] [PubMed] [Google Scholar]
- [11].Quaney BM, Perera S, Maletsky R, et al. . Impaired grip force modulation in the ipsilesional hand after unilateral middle cerebral artery stroke. Neurorehabil Neural Repair. 2005;19(4):338–349. [DOI] [PubMed] [Google Scholar]
- [12].Gordon AM, Westling G, Cole KJ, et al. . Memory representations underlying motor commands used during manipulation of common and novel objects. J Neurophysiol. 1993;69(6):1789–1796. [DOI] [PubMed] [Google Scholar]
- [13].Huysmans MA, Hoozemans MJ, Visser B, et al. . Grip force control in patients with neck and upper extremity pain and healthy controls. Clin Neurophysiol. 2008;119(8):1840–1848. [DOI] [PubMed] [Google Scholar]
- [14].Johansson RS, Westling G. Coordinated isometric muscle commands adequately and erroneously programmed for the weight during lifting task with precision grip. Exp Brain Res. 1988;71(1):59–71. [DOI] [PubMed] [Google Scholar]
- [15].IFOMPT, I.F.o.O.M.P.T Glossary of Terminology: Supplement to the Standards document. 2010. Available from: http://www.ifompt.com/Standards/SC+Glossary.html
- [16].Maitland GD. Maitland’s vertebral manipulation. Oxford: Elsevier Butterworth-Heinemann; 2005. [Google Scholar]
- [17].Gross AR, Kay TM, Kennedy C, et al. . Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders. Man Ther. 2002;7(4):193–205. [DOI] [PubMed] [Google Scholar]
- [18].Haavik-Taylor H, Murphy B. Cervical spine manipulation alters sensorimotor integration: a somatosensory evoked potential study. Clin Neurophysiol. 2007;118(2):391–402. [DOI] [PubMed] [Google Scholar]
- [19].Herzog W, Scheele D, Conway PJ. Electromyographic responses of back and limb muscles associated with spinal manipulative therapy. Spine (Phila Pa 1976). 1999;24(2): 146–152, discussion 153. [DOI] [PubMed] [Google Scholar]
- [20].Dunning J, Rushton A. The effects of cervical high-velocity low-amplitude thrust manipulation on resting electromyographic activity of the biceps brachii muscle. Man Ther. 2009;14(5):508–513. [DOI] [PubMed] [Google Scholar]
- [21].Faul F, Erdfelder E, Lang AG, et al. . G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- [22].Merskey H, Bogduk N. Classification of Chronic Pain. Descriptions of Chronic pain Syndromes and Definitions of Pain Terms Seatle (WA): IASP Press; 1994. [Google Scholar]
- [23].Refshauge KM, Parry S, Shirley D, et al. . Professional responsibility in relation to cervical spine manipulation. Aust J Physiother. 2002;48(3):171–179, discussion 180-5 [DOI] [PubMed] [Google Scholar]
- [24].Bell-Krotoski JA, Fess EE, Figarola JH, et al. . Threshold detection and Semmes-Weinstein monofilaments. J Hand Ther. 1995;8(2):155–162. [DOI] [PubMed] [Google Scholar]
- [25].Johansson RS, Westling G. Significance of cutaneous input for precise hand movements. Electroencephalogr Clin Neurophysiol Suppl. 1987;39:53–57. [PubMed] [Google Scholar]
- [26].Nowak DA, Hermsdörfer J, Glasauer S, et al. . The effects of digital anaesthesia on predictive grip force adjustments during vertical movements of a grasped object. Eur J Neurosci. 2001;14(4):756–762. [DOI] [PubMed] [Google Scholar]
- [27].de Oliveira DG, Nunes PM, Aruin AS, et al. . Grip force control in individuals with hand osteoarthritis. J Hand Ther. 2011;24(4):345–54, quiz 355. [DOI] [PubMed] [Google Scholar]
- [28].Radomski MV, Latham CAT. Occupational therapy for physical dysfunction. 6th ed Philadelphia: Lippincott Williams & Wilkins; 2008. xxiii, 1432 p. [Google Scholar]
- [29].Fischer AA. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain. 1987;30(1):115–126. [DOI] [PubMed] [Google Scholar]
- [30].Hermens HJ, Freriks B, Disselhorst-Klug C, et al. . Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361–374. [DOI] [PubMed] [Google Scholar]
- [31].Fernández-De-Las-Peñas C, Pérez-De-Heredia M, Brea-Rivero M, et al. . Immediate effects on pressure pain threshold following a single cervical spine manipulation in healthy subjects. J Orthop Sports Phys Ther. 2007;37(6):325–329. [DOI] [PubMed] [Google Scholar]
- [32].Dallal GE. Randomization.com. 2012. [cited 2012; Randomization Plan generator]. Available from: http://www.randomization.com/
- [33].Dunning J, Mourad F, Barbero M, et al. . Bilateral and multiple cavitation sounds during upper cervical thrust manipulation. BMC Musculoskelet Disord. 2013;14:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Maigne R. The concept of painlessness and opposite motion in spinal manipulations. Am J Phys Med. 1965;44:55–69. [PubMed] [Google Scholar]
- [35].Maigne R, Nieves WL, Sommer HM. Diagnosis and treatment of pain of vertebral origin : a manual medicine approach. 1st ed Baltimore: Williams & Wilkins; 1996, xvii, 550 p. [Google Scholar]
- [36].De Luca CJ, Gilmore LD, Kuznetsov M, et al. . Filtering the surface EMG signal: movement artifact and baseline noise contamination. J Biomechanics. 2010;43(8):1573–1579. [DOI] [PubMed] [Google Scholar]
- [37].Aruin AS, Latash ML. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary arm movements. Exp Brain Res. 1995;103(2):323–332. [DOI] [PubMed] [Google Scholar]
- [38].Kanekar N, Santos MJ, Aruin AS. Anticipatory postural control following fatigue of postural and focal muscles. Clin Neurophysiol. 2008;119(10):2304–2313. [DOI] [PubMed] [Google Scholar]
- [39].Hermsdörfer J, Hagl E, Nowak DA. Deficits of anticipatory grip force control after damage to peripheral and central sensorimotor systems. Hum Mov Sci. 2004;23(5):643–662. [DOI] [PubMed] [Google Scholar]
- [40].Nowak DA, Glasauer S, Meyer L, et al. . The role of cutaneous feedback for anticipatory grip force adjustments during object movements and externally imposed variation of the direction of gravity. Somatosens Mot Res. 2002;19(1):49–60. [DOI] [PubMed] [Google Scholar]
- [41].Raghavan P, Krakauer JW, Gordon AM. Impaired anticipatory control of fingertip forces in patients with a pure motor or sensorimotor lacunar syndrome. Brain. 2006;129(6):1415–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Van Breukelen GJ. ANCOVA versus change from baseline: more power in randomized studies, more bias in nonrandomized studies [corrected]. J Clin Epidemiol. 2006;59(9):920–925. [DOI] [PubMed] [Google Scholar]
- [43].Ruiz-Saez M, Fernández-de-las-Peñas C, Blanco CR, et al. . Changes in pressure pain sensitivity in latent myofascial trigger points in the upper trapezius muscle after a cervical spine manipulation in pain-free subjects. 2007. [cited 30 iy5, 7807107]; 8:[578–583]. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medl&NEWS=N&AN=17996549 [DOI] [PubMed]
- [44].Fernández-Carnero J, Fernández-de-las-Peñas C, Cleland JA. Immediate hypoalgesic and motor effects after a single cervical spine manipulation in subjects with lateral epicondylalgia. J Manipulative Physiol Ther. 2008;31(9):675–681. [DOI] [PubMed] [Google Scholar]
- [45].Maduro de Camargo VM, Alburquerque-Sendín F, Bérzin F, et al. . Immediate effects on electromyographic activity and pressure pain thresholds after a cervical manipulation in mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2011;34(4):211–220. [DOI] [PubMed] [Google Scholar]
- [46].Lluch E, Schomacher J, Gizzi L, et al. . Immediate effects of active cranio-cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio-cervical flexion test. Man Ther. 2014;19(1):25–31. [DOI] [PubMed] [Google Scholar]
- [47].Campos CS Jr, Bracht MA, Santos MJ. The effect of finger joint hypomobility on precision grip force. Journal of Hand Therapy. 2013;26(4):323–329. [DOI] [PubMed] [Google Scholar]
- [48].Nowak DA, Hermsdörfer J. Objective evaluation of manual performance deficits in neurological movement disorders. Brain Res Rev. 2006;51(1):108–124. [DOI] [PubMed] [Google Scholar]
- [49].Nowak DA, Hermsdörfer J. Grip force behavior during object manipulation in neurological disorders: toward an objective evaluation of manual performance deficits. Mov Disord. 2005;20(1):11–25. [DOI] [PubMed] [Google Scholar]