Abstract
Objective
Consistent evidence on the effects of specialist services in the primary care setting is lacking. Therefore, this study evaluated the effects of an in-house internist at a GP practice on the number of referrals to specialist care in the hospital setting. Additionally, the involved GPs and internist were asked to share their experiences with the intervention.
Design
A retrospective interrupted times series study.
Setting
Two multidisciplinary general practitioner (GP) practices.
Intervention
An internist provided in-house patient consultations in two GP practices and participated in the multidisciplinary meetings.
Subjects
The referral data extracted from the electronic medical record system of the GP practices, including all referral letters from the GPs to specialist care in the hospital setting.
Main outcome measures
The number of referrals to internal medicine in the hospital setting. This study used an autoregressive integrated moving average model to estimate the effect of the intervention taking account of a time trend and autocorrelation among the observations, comparing the pre-intervention period with the intervention period.
Results
It was found that the referrals to internal medicine did not statistically significant decrease during the intervention period.
Conclusions
This small explorative study did not find any clues to support that an in-house internist at a primary care setting results in a decrease of referrals to internal medicine in the hospital setting.
Key Points
An in-house internist at a primary care setting did not result in a significant decrease of referrals to specialist care in the hospital setting.
The GPs and internist experience a learning-effect, i.e. an increase of knowledge about internal medicine issues.
Keywords: Substitution, general practice, primary care, referral, primary care plus
Introduction
In an attempt to rein in rising healthcare costs, many countries, among which the Netherlands, are reforming policies to stimulate the development of a (financially) sustainable healthcare system [1–4]. Strengthening the primary care system is a common policy goal for many countries [5–7]. Primary care is assumed to alleviate some of the pressure of the rising healthcare costs by improving the population’s health at lower costs [5,8]. In line with these policies numerous regional initiatives have arisen, of which quite a few are focused on substitution of care. Substitution of care can be defined as: ‘the continual regrouping of resources across and within care settings to exploit the best and least costly solutions in face of changing needs and demands’ [9,10]. For example, internationally well-known concepts are specialist outreach clinics and joint consultations [11–15]. Both concepts attempt to shift care from the secondary to the primary care setting by specialists providing services in the general practice setting.
In the Netherlands, a relatively new healthcare delivery model of substitution of care is Primary Care Plus (PC+), which attempts to substitute specialist care from the hospital setting toward the primary care setting [16]. In the Netherlands, the general practitioners (GPs) act as gatekeepers of the healthcare system: hospital care and specialist care are only accessible through GP referral [17,18]. PC+ interventions intend to support GPs in gatekeeping and treating patients by intensifying and strengthening collaboration and communication between GPs and specialists [16]. PC+ is aimed at decreasing the number of (unnecessary) referrals to specialist care in the hospital setting in order to reduce the rising healthcare costs. Moreover, it intends to improve the health of the population and patients’ experience of care.
PC+ is a new concept and, consequently, evidence of its effects is scarce and its support is mostly on conceptual grounds [16,19]. Therefore, evaluations are required to estimate the effects of PC+ initiatives. This study is aimed at a PC+ intervention in which GP practices have an in-house internist. The internist provides consultations with patients and participates in multidisciplinary meetings within the GP practices. This PC+ intervention strengthens collaboration, direct communication and knowledge transfer between the GPs and internist and this has seemed to have a positive influence on the perceived quality of care and health outcomes [12,16]. Besides improving the health of the population and the patients’ experiences of care, the main goal of this PC+ intervention is to decrease the number of (unnecessary) referrals to specialist care in the hospital setting. Effective collaboration between the GPs and internist should enhance the accuracy of referrals, keeping unfitting referred medical complaints out of the hospital. Therefore, this explorative study focused on the referral rates to specialist care in the hospital setting. The research question was: Does an in-house internist reduce the number of referrals to internal medicine in the hospital setting?
Material and methods
Study design and study period
This research was a retrospective interrupted times series (ITS) study. Data regarding the number of referrals to hospital care were extracted from the electronic medical record system of the GP practices. The pre-intervention period was from January 2012 to December 2013, and the intervention period was from January 2014 to December 2015. The original set-up of this study consisted of eight GP practices, including four intervention practices and four control ones. However, during the data collection phase, six were disqualified due to incomplete registration. Hence, only two GP practices, both intervention practices, were included in this study.
Study setting and population
This small-scale study focused on two GP practices. GP practice 1 consisted of two GPs with circa 3000 registered patients, while GP practice 2 consisted of four GPs with circa 7600 registered patients. The GPs of both practices are part of a multidisciplinary team. They work closely together with healthcare professionals, such as nurse practitioners, dieticians, pharmacists and elderly specialists. The multidisciplinary teams meet on a regular basis to discuss cases. The GPs have access to several diagnostic tools, e.g. electrocardiogram, blood test laboratory, blood pressure monitors and spirometers. The size and GP composition of the GP practices did not change within the included time frame of this study.
The GP practices are both located in the same region, namely in the most southern part of the Netherlands. The region is characterized by a relatively old and unhealthy population with a low socio-economic status (SES), as compared to the overall population of the Netherlands [20]. For example 20.6% of the population is above 65 years old, compared to 15.9% of the overall population [20].
Intervention
An independent internist (i.e. not working in and not connected to the hospital) provided in-house patient consultations in the two GP practices and participated in the multidisciplinary meetings. In GP practice 1 the internist was present every other week and in GP practice 2 on a weekly basis. The GPs were able to refer non-acute and low-complexity patients to the in-house internist for a consultation and during the multidisciplinary meetings, the GPs and internist discussed patients with the group of healthcare professionals. The maximum number of consultations with the internist per patient and per medical complaint was three. During the consultations, the internist examined patients and afterwards he provided the GPs with advice on diagnosis, treatment and/or necessity to refer the patient to specialist care in the hospital setting. During the consultation by the in-house internist, the GPs remained clinically responsible for the patient. Besides general internal medicine, the internist focused on the subspecialties gastroenterology, rheumatology, nephrology, endocrinology and geriatric care. All other subspecialties of internal medicine were excluded (e.g. hematology, oncology, pulmonology and immunology). The internist received a fixed salary paid by the healthcare insurers. The salary is independent of the number of enrollees or services rendered.
Data collection
The referral data included all referral letters from the GPs to specialist care in the hospital setting. These were extracted from the electronic medical record system of the GP practices. Thereafter, the referrals to internal medicine were identified by a professional search engine, the program FileLocator Pro. The search strategy used to identify the internal medicine referrals consisted of the following terms (translated from Dutch to English): ‘internist OR internal OR gastroenterologist OR gastroenterology OR rheumatologist OR rheumatology OR nephrologist OR nephrology OR endocrinologist OR endocrinology OR geriatric OR geriatrics OR “all names of the internists working at the local hospital”’. Referrals to the internist in the GP practice, i.e. the PC+ intervention, were not included.
The program accounted for spelling and grammatical errors, as well as differences in the layout of the referrals. Additionally, the researchers ensured the reliability of the search engine. The automatic identification with the professional search engine FileLocator Pro was manually checked for four quarters (i.e. one quarter within each consecutive year). A crosstabs analysis was performed to determine the Cohen’s Kappa. For all four quarters, this resulted in a Cohen’s Kappa of 1. Hence, the inter-rater agreement was perfect and the automatic search with FileLocator Pro was considered as reliable [21].
Data analysis
Data are described using absolute counts and percentages for categorical variables and means and standard deviations for continuous variables. The data of each year was split up into quarters, including eight pre-intervention and eight intervention quarters. The start of the intervention was indicated using different labels for pre-intervention (Phase = 0) and intervention (Phase = 1). The data of both GP practices were taken together (i.e. summed up) to be able to analyze the intervention effect in total.
First, dependent sample t-tests were used to analyze whether there was a difference in the mean number of referrals between the pre-intervention period and the intervention period. Second, the ITS analyses included an autoregressive integrated moving average (ARIMA) model to estimate the effect of the intervention, taking account of a time trend and autocorrelation among the observations [22,23]. ITS analyses, such as the ARIMA model, includes that data is collected at multiple time points before and after an intervention in order to determine whether the intervention produced a discontinuity (change in level or slope) in comparison with the underlying secular trend. The independent variables were (1) time (quarter), (2) phase (pre-intervention and intervention period) and (3) the interaction term (time × phase). The dependent variables were the number of referrals to internal medicine in the hospital setting and a ratio of the number of referrals to internal medicine in the hospital setting divided by the number of total referrals to hospital care. A ratio was measured to correct for an overall trend. Statistical methods were 2-tailed and p values of <.05 were considered significant. Analyses were performed using IBM SPSS Statistics version 24 (IBM SPSS Statistics, Armonk, NY).
Expert meeting
After the statistical analysis of the referral data, an expert meeting was organized. The involved GPs and the internist were asked to give their professional view on the results of the data analysis. The GPs and internist received an overview of the results at the beginning of the meeting. Three main topics, i.e. questions, were discussed during this meeting: (1) What is your view on the results of this study? (2) What is your experience with the intervention? (3) What are the effects of this intervention according to your experiences? The goal of this expert meeting was to clarify and explain the quantitative results.
Results
Table 1 provides an overview of the number of consultations given by the in-house internist during the intervention period.
Table 1.
Number of in-house consultations given by the internist per GP practice in 2014 and 2015.
| GP practice | Year | Number of first consultations given by the in-house internist | Number of follow-up consultations given by the in-house internist |
|---|---|---|---|
| GP practice 1 | 2014 | 83 | 29 |
| 2015 | 101 | 37 | |
| GP practice 2 | 2014 | 106 | 130 |
| 2015 | 130 | 203 |
Table 2 shows the mean numbers of referrals to internal medicine in the hospital setting, the mean numbers of total referrals to hospital care and the ratios. The ratio is calculated as follows: the number of referrals to internal medicine in the hospital setting divided by the number of total referrals to hospital care.
Table 2.
Descriptive characteristics of the study parameters and the results of the t-tests.
| Pre-intervention perioda (mean ± SDd) | Intervention periodb (mean ± SDd) | 95% Confidence Intervalc | p Value | |
|---|---|---|---|---|
| GP practice 1 | ||||
| Number of referrals to internal medicine in the hospital setting per quarter | 18.3 ± 5.8 | 14.4 ± 4.6 | −1.5–9.3 | .133 |
| Number of referrals to hospital care per quarter | 233.1 ± 19.1 | 244.4 ± 22.0 | −30.9–8.4 | .217 |
| Ratio per quarter | 0.078 ± 0.022 | 0.058 ± 0.015 | 0.00–0.04 | .05 |
| GP practice 2 | ||||
| Number of referrals to internal medicine in the hospital setting per quarter | 26.6 ± 5.1 | 34.6 ± 3.8 | −11.2−4.8 | .001* |
| Number of referrals to hospital care per quarter | 558.6 ± 78.2 | 628.5 ± 38.2 | −147.9–8.2 | .072 |
| Ratio per quarter | 0.033 ± 0.008 | 0.023 ± 0.007 | 0.002–0.007 | .016* |
| Sum of both practicese | ||||
| Number of referrals to internal medicine in the hospital setting per quarter | 44.9 ± 6.5 | 49.0 ± 7.1 | −10.2–2.0 | .155 |
| Number of referrals to hospital care per quarter | 791.8 ± 88.9 | 872.9 ± 50.2 | −169.9–7.7 | .068 |
| Ratio per quarter | 0.057 ± 0.009 | 0.056 ± 0.006 | −0.004–0.007 | .648 |
Notes: *Statistically significant, p value <.05.
aThe pre-intervention period is from January 2012, coded as quarter 1 in the data, until December 2013, coded as quarter 8 in the data.
bThe intervention period is from January 2014, coded as quarter 9 in the data, until December 2015, coded as quarter 16 in the data.
cThe 95% confidence interval of the difference between the pre-intervention and the intervention period.
dStandard deviation.
eThe intervention effect.
Regarding GP practice 1, the mean number of referrals to internal medicine in the hospital setting was 18.3 per quarter during the pre-intervention period and 14.4 during the intervention period, this difference was not significant (p = .133). Moreover, with respect to GP practice 2, the mean number of referrals to internal medicine in the hospital was 26.6 during the pre-intervention period and 34.6 during the intervention period, this indicated a significant increase of referrals (p < .05).
The autoregressive integrated moving average model (ARIMA)
Figure 1 visualizes the quarterly trend of referrals to internal medicine in the hospital setting. Regarding the sum of both GP practices (i.e. the intervention effect), the difference in trend was not statistically significant (p = .337). The number of referrals to internal medicine decreased with an average of 2.01 referrals per quarter during the pre-intervention period, while during the intervention period the referral rate decreased with an average of 0.81 referrals per quarter. With respect to the GP practices separately, in GP practice 1, the number of referrals decreased with an average of 2.00 referrals per quarter during the pre-intervention period, while during the intervention period the referral rate decreased with an average of 0.84 referrals per quarter (p = .114). In GP practice 2, the trend changed from a decrease of 0.01 referrals to an increase of 0.04 referrals per quarter (p = .968).
Figure 1.
Number of referrals to internal medicine in the hospital setting (2012–2015).
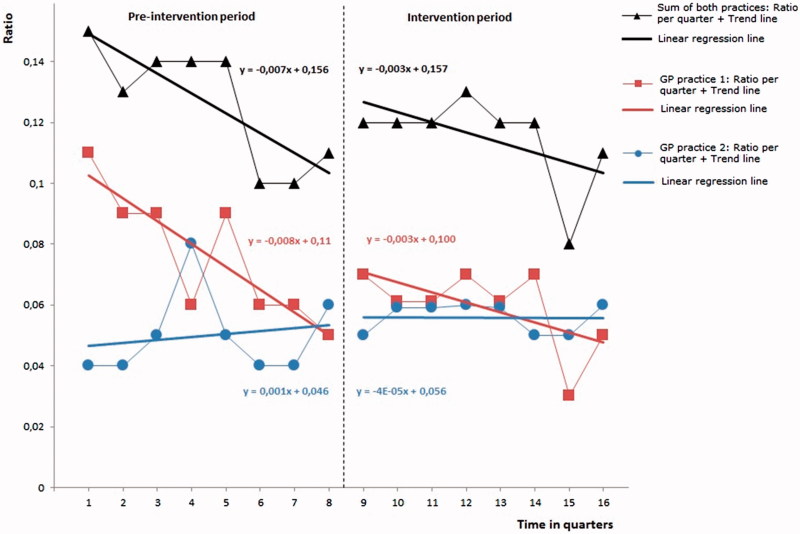
Figure 2 visualizes the quarterly trend of the ratio. The difference in trend of the ratio of the sum of both practices was not statistically significant (p = .940). The difference in trend of the ratio in GP practice 1 was statistically significant (p = .031), however, in GP practice 2 the change in trend of the ratio was not significant (p = .580).
Figure 2.
Ratio: the number of referrals to internal medicine in the hospital setting divided by the number of total referrals to hospital care (2012–2015).
Expert meeting
The results of this study were not in line with the expectations of the involved GPs and internist. The GPs and internist believed that the absence of a decrease in referrals could probably be explained by an increase in knowledge about internal medicine issues. That is, they experienced that close collaboration resulted in a learning-effect for the GPs. For example, GPs became better at recognizing specific symptoms, of which they were not aware or did not recognize before the presence of the in-house internist. This could lead to an increase in referrals to specialist care in the hospital setting but it may also increase the quality of care. Additionally, they mentioned that it is important to note that a proportion of the referrals to hospital care is unavoidable, due to acute and complex conditions, which are unlikely to be influenced by any primary care arrangements like an in-house internist. Above all, the GPs expect that the learning-effect has initially led to an increase of referrals to internal medicine, but in the long run it will lead to a decrease. The start of the in-house internist resulted in a catch-up for the GPs in treating patients with specific internal medicine issues. In the short term, this could have resulted in an increase of referrals to hospital care.
Discussion
This small-scale study investigated the effect of an in-house internist at GP practices on the referral rates to specialist care in the hospital setting. We found that the referrals to internal medicine did not statistically significant decrease during the intervention period. The GPs and internist experienced that close collaboration resulted in a learning-effect for the GPs. They supposed that the absence of a decrease in referrals could probably be explained by an increase in knowledge about internal medicine issues. GPs became better at recognizing specific symptoms which probably led to an increase in referrals to specialist care in the hospital setting.
Strengths and weaknesses
A limitation of this study is the absence of more GP practices and a control group (i.e. general practices with no in-house internist) and the retrospective design of the study. A prospective design would have been better since the researchers could have predefined the registration requirements for the evaluation of the intervention. As described in the methods section, six out of eight GP practices were disqualified for this study due to incomplete and/or untraceable data registration. We advocate for better registration by GPs, not only for research but also for the GPs themselves. In order to be able to measure the effects of interventions and other changes in GP practices, it is important to register the required information in a complete and traceable manner. It is likely that the selection of only two out of eight GP practices probably resulted in a biased sample. These two GP practices may not be a proper representation of the target population. This selection bias is a significant threat to the external validity of this study. Nevertheless, these two eligible practices provided referral data over a period of four years, two years before the start of the intervention and two years during the intervention. The extended time frame strengthens the validity and reliability of the results of this study. Additionally, ITS analyses using ARIMA models were used to analyze the data. This is an appropriate and preferred method when data are collected at multiple time points before and after an intervention in order to detect whether or not the intervention had a significantly greater effect than any underlying secular trend [24]. The analysis estimates the effect of the intervention whilst taking account of time trend and autocorrelation among the observations [22,23].
Findings in relation to other studies
Several studies on specialist services in the primary care setting have shown a decrease in referrals to (outpatient) hospital care; for example specialist outreach services in which specialists hold clinics in general practice settings [13]. Prior research, a review on 73 outreach interventions, showed that specialist outreach services may improve access to care, quality of care, health outcomes and patient satisfaction and result in less use of hospital services [11]. Additionally, joint consultations with specialists and GPs seemed to be an effective method to select the appropriate patients for specialist care in secondary care and to decrease the overall number of referrals to secondary care [14,15,25]. However, Van Hoof and colleagues [16] stated that an in-house medical specialist at a GP practice may lead to overuse of care due to close working relations. They mention that this may result in more referrals because of a relatively low threshold for GPs to refer a patient to the in-house medical specialist. To avoid this threat they are in favor of independent PC+ centers, where medical specialists work in a neutral environment [16]. Another review of interventions at the primary–secondary care interface found little evidence of a beneficial effect of specialist services in primary care on referral rates to secondary care [26]. A study about the effects of joint consultations described substantial educational benefits for GPs where a specialist visited the general practice [27]. This educational benefit for the GPs, i.e. learning-effect, is also considered as a potential effect of the in-house internist. Above all, based on the previous studies it can be concluded that consistent evidence on the effects of specialist services in the primary care setting is lacking [22,24].
Conclusion and implications
This small explorative study did not find any clues to support that an in-house internist at a primary care setting results in a decrease of referrals to internal medicine in the hospital setting. The GPs and internist experience that this intervention contributed to a learning-effect for the GPs. Overall, it can be concluded that more research is needed. It is striking that the results of the GP practices were different, but based on this study it remains unclear why the GP practices differ. Moreover, the results of this study should be compared to care as usual, i.e. GP practices with no in-house internist. We strongly recommend healthcare professionals (e.g. GPs) and managers within the healthcare sector to register all required information in a structured, accurate and traceable manner. Additionally, the results of the expert meeting show that the GPs expect an increase of knowledge regarding internal medicine. Future research focused on interventions with specialist services in the primary care setting, should include knowledge measurements to investigate a possible learning-effect.
Acknowledgments
We gratefully acknowledge the participating general practitioners and internist for providing the data for this study.
Ethical approval
The study was approved by the Medical Research and Ethics Committee of the Maastricht University Medical Centre, Maastricht, The Netherlands in 2015 (METC 15-4-032).
Disclosure statement
The authors declare that they have no competing interests.
Notes on contributors
Tessa C.C. Quanjel, MSc, is a PhD student at the Department of Health Services Research, Care and Public Health Research Institute (CAPHRI), Faculty of Health Medicine and Life Sciences at Maastricht University, Maastricht, The Netherlands.
Anne Winkens, BSc, is a master student Physician ? Clinical Researcher, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands.
Marieke D. Spreeuwenberg, PhD, is an Associate Professor at the Department of Health Services Research, Care and Public Health Research Institute (CAPHRI), Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, and at the Research Centre for Technology in Care, Zuyd University of Applied Sciences, Heerlen, The Netherlands.
Jeroen N. Struijs, PhD, is an Associate Professor at the Department for Quality of Care and Health Economics, Centre for Nutrition, Prevention and Health Services, National Institute for Public Health and the Environment, Bilthoven, and at the Department for Public Health and Primary Care, Leiden University Medical Centre, Leiden, The Netherlands.
Ron A.G. Winkens, MD, PhD, is an Family Physician and an associate professor and medical coordinator at Diagnostic Centre and aMice, Maastricht University Medical Centre (Maastricht UMC+), Maastricht, The Netherlands.
Caroline A. Baan, PhD, is professor of Integrated Health Care at the Scientific Centre for Transformation in Care and Welfare (Tranzo), University of Tilburg, Tilburg and she is head of the Department for Quality of Care and Health Economics, Centre for Nutrition, Prevention and Health Services, National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and, The Netherlands.
Dirk Ruwaard, MD, PhD, is professor of Public Health and Health Care Innovation and head of the Department of Health Services Research, Care and Public Health Research Institute (CAPHRI), Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht,the Netherlands.
References
- 1.Porter ME, Lee TH.. The strategy that will fix healthcare. Harvard Bus Rev. 2013;91:50–70. [Google Scholar]
- 2.Pammolli F, Riccaboni M, Magazzini L.. The sustainability of European health care systems: beyond income and aging. Eur J Health Econ. 2012;13:623–634. [DOI] [PubMed] [Google Scholar]
- 3.Thomson S, Foubister T, Mossialos E.. Financing health care in the European Union: challenges and policy responses. Copenhagen: WHO Regional Office for Europe; 2009. [Google Scholar]
- 4.Ministry of Health Welfare and Sports (MHWS) Naar beter betaalbare zorg. [To better affordable care.] Den Haag: MHWS; 2012. [Google Scholar]
- 5.Starfield B, Shi L, Macinko J.. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macinko J, Starfield B, Shi L.. The contribution of primary care systems to health outcomes within organization for economic cooperation and development (OECD) countries, 1970–1998. Health Serv Res. 2003;38:831–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.OECD/EU Strengthening primary care systems.. In: Health at a glance: Europe 2016: State of health in the EU cycle [Internet]. Paris: OECD/EU; 2016. [Google Scholar]
- 8.Groenewegen PP, Dourgnon P, Gress S, et al. Strengthening weak primary care systems: steps towards stronger primary care in selected Western and Eastern European countries. Health Policy. 2013;113:170–179. [DOI] [PubMed] [Google Scholar]
- 9.Warner M. Re-designing health services. Reducing the zone of delusion. London: The Nuffield Trust; 1997. [Google Scholar]
- 10.Grone O, Gracia-Barbero M.. Integrated care. A position paper of the WHO European office for integrated health care services. Int J Integr Care. 2001;1:1–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Gruen RL, Weeramanthri TS, Knight SS, et al. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2003; 4:CD003798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Powell J. Systematic review of outreach clinics in primary care in the UK. J Health Serv Res Policy. 2002;7:177–183. [DOI] [PubMed] [Google Scholar]
- 13.Bowling A, Bond M.. A national evaluation of specialists’ clinics in primary care settings. Br J Gen Pract. 2001;51:264–269. [PMC free article] [PubMed] [Google Scholar]
- 14.Vlek JF, Vierhout WP, Knottnerus JA, et al. A randomised controlled trial of joint consultations with general practitioners and cardiologists in primary care. Br J Gen Pract. 2003;53:108–112. [PMC free article] [PubMed] [Google Scholar]
- 15.Schulpen GJ, Vierhout WP, van der Heijde DM, et al. Joint consultation of general practitioner and rheumatologist: does it matter? Ann Rheum Dis. 2003;62:159–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Hoof SJM, Kroese MEAL, Spreeuwenberg MD, et al. Substitution of hospital care with primary care: defining the conditions of primary care plus. Int J Integr Care. 2016;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schäfer W, Kroneman M, Boerma W, et al. The Netherlands: health system review. Health Syst Transit. 2010;12:v–229. [PubMed] [Google Scholar]
- 18.Daley C, Gubb J, Clarke E, Bidgood E.. Healthcare systems: the Netherlands Civitas. London: Civitas Health Unit; 2013. [Google Scholar]
- 19.van Hoof SJ, Spreeuwenberg MD, Kroese ME, et al. Substitution of outpatient care with primary care: a feasibility study on the experiences among general practitioners, medical specialists and patients. BMC Fam Pract. 2016;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drewes HW, Heijink R, Struijs JN, et al. . Samen werken aan duurzame zorg; Landelijke monitor proeftuinen. [Working together for sustainable care; National monitor pioneer sites.] Bilthoven: Rijksinstituut voor Volksgezondheid en Milieu; 2015. [Google Scholar]
- 21.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 22.Penfold RB, Zhang F.. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13:38–44. [DOI] [PubMed] [Google Scholar]
- 23.Fretheim A, Soumerai SB, Zhang F, et al. Interrupted time-series analysis yielded an effect estimate concordant with the cluster-randomized controlled trial result. J Clin Epidemiol. 2013;66:883–887. [DOI] [PubMed] [Google Scholar]
- 24.Ramsay CR, Matowe L, Grilli R, et al. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care. 2003;19:613–623. [DOI] [PubMed] [Google Scholar]
- 25.Vierhout WP, Knottnerus JA, van OA, et al. Effectiveness of joint consultation sessions of general practitioners and orthopaedic surgeons for locomotor-system disorders. Lancet. 1995;346:990–994. [DOI] [PubMed] [Google Scholar]
- 26.Winpenny EM, Miani C, Pitchforth E, et al. Improving the effectiveness and efficiency of outpatient services: a scoping review of interventions at the primary-secondary care interface. J Health Serv Res Policy. 2017;22:53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moffatt J, Hossain D, Hansford G.. Physician in practice clinic: educating GPs in endocrinology through specialist-outreach. Rural Remote Health. 2012;12:1–14. [PubMed] [Google Scholar]