Abstract
Background and purpose
Alternative bearing surfaces such as ceramics and highly crosslinked polyethylene (HXLPE) were developed in order to further improve implant performance of total hip arthroplasties (THAs). Whether these alternative bearing surfaces result in increased longevity is subject to debate.
Patients and methods
Using the Dutch Arthroplasty Register (LROI), we identified all patients with a primary, non-metal-on-metal THA implanted in the Netherlands in the period 2007–2016 (n = 209,912). Cumulative incidence of revision was calculated to determine differences in survivorship of THAs according to bearing type: metal-on-polyethylene (MoPE), metal-on-HXLPE (MoHXLPE), ceramic-on-polyethylene (CoPE), ceramic-on-HXLPE (CoHXLPE), ceramic-on-ceramic (CoC), and oxidized-zirconium-on-(HXL)polyethylene (Ox(HXL)PE). Multivariable Cox proportional hazard regression ratios (HRs) were used for comparisons.
Results
After adjustment for confounders, CoHXLPE, CoC, and Ox(HXL)PE resulted in a statistically significantly lower risk of revision compared with MoPE after 9 years follow-up (HR =0.8–0.9 respectively, compared with HR =1.0). For small (22–28 mm) femoral head THAs, lower revision rates were found for CoPE and CoHXLPE (HR =0.9). In the 36 mm femoral head subgroup, CoC-bearing THAs had a lower HR compared with MoHXLPE (HR =0.7 versus 1.0). Crude revision rates in young patients (< 60 years) for CoHXLPE, CoC, and Ox(HXL)PE (HR =0.7) were lower than MoPE (HR =1.0). However, after adjustment for case mix and confounders these differences were not statistically significant.
Interpretation
We found a mid-term lower risk of revision for CoHXLPE, CoC, and Ox(HXL)PE bearings compared with traditional MoPE-bearing surfaces.
Increased activity of patients and a younger age at the time of the primary procedure have sparked the development of alternative bearing surfaces in total hip arthroplasty (THA) such as ceramics, highly-crosslinked-polyethylene (HXLPE), and metal-on-metal articulations (MoM), in order to further improve survival and implant performance (Mihalko et al. 2014, Varnum et al. 2015). Currently, aseptic loosening of the acetabular component is the most frequent cause of revision after THA with a metal-on-polyethylene (MoPE) counterface (LROI annual report 2015, Norwegian Arthroplasty Register 2016). Osteolysis with subsequent loosening of components can be generated by polyethylene (PE) particles as a result of PE wear (Varnum et al. 2015). Therefore, the use of alternative bearing surfaces has become more common over the last 2 decades. It is unknown whether the survivorship of these implants is better compared with the traditional MoPE bearings they sought to replace.
Studies which compared the survival of different bearing surfaces attained variant conclusions. The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) demonstrated superior results of HXLPE, ceramics, and ceramicized metal (or oxidized zirconium) in terms of increased longevity of the THA compared with standard PE (Annual Report AOANJRR 2016). A systematic review and network meta-analysis of randomized controlled trails demonstrated similar survivorship among ceramic-on-ceramic (CoC), ceramic-on-polyethylene (CoPE), ceramic-on-highly-crosslinked-polyethylene (CoHXLPE) and metal-on-highly-crosslinked-polyethylene (MoHXLPE) bearings, and inferior results for MoM and MoPE bearing implants (Yin et al. 2015).
Whether these alternative bearing materials, in combination with larger heads, have indeed resulted in increased survival rates, however, remains to be proven. Using nationwide data from the LROI, we assessed survivorship of CoC, CoHXLPE, MoHXLPE, CoPE, and oxidized-zirconium-on-(highly crosslinked)-polyethylene (Ox(HXL)PE) bearings in THA in the Netherlands, compared with MoPE.
Patients and methods
Data sources
The LROI, initiated by the Dutch Orthopaedic Association in 2007, is a nationwide population-based registry covering all hospitals in the Netherlands. This inter-institutional database has a completeness of 98% for primary THA and 88% for hip revision arthroplasty (van Steenbergen et al. 2015). The LROI contains prospectively collected data on primary and revision arthroplasty. Patient characteristics are recorded at the time of the primary procedure. In addition, surgical variables such as procedure and implant information are registered in the LROI. Implant information is supplied by all manufacturers, and is collected at the time of the procedure using stickers that could be attached to a registration form. Thereafter, prosthesis characteristics are derived from an implant library within the LROI, which contains several core characteristics of all prostheses used in the Netherlands, including name and type of the prosthesis, manufacturer, material, and femoral head size (van Steenbergen et al. 2015). Data from the LROI are matched with the national insurance database on healthcare (Vektis 2017), in order to obtain information on the vital status and date of death of registered patients.
Data collection
Eligible patients were registered in the LROI as having received a primary THA in a Dutch hospital, from the start of the registry in 2007 until the end of the follow-up period on December 31, 2016 (n = 227,107). A patient can be registered twice, having undergone a bilateral hip replacement. A primary THA is defined as the first implantation of a prosthesis, to replace a hip joint (van Steenbergen et al. 2015). Given their now known higher failure rates, THAs with a MoM bearing surface were excluded (n = 5,359) (Drummond et al. 2015, Nederlandse Orthopaedische Vereniging 2015, Rieker 2017). Patients with unknown prosthesis components or patients for whom 1 of the components was not registered were excluded (n = 11,836). The final cohort contained 209,912 THAs.
The mean length of follow-up was 3.9 years, with a maximum of 9.9 years.
Types of bearing surface
Hip arthroplasty articulation was differentiated based on the bearing surface of the femoral head and the inlay or monoblock cup. Metal-on-standard-polyethylene was used as reference bearing type. All other bearing surfaces, except for ceramic-on-polyethylene, were considered as an alternative bearing type. The following groups were discerned: metal-on-polyethylene (MoPE), metal-on-highly-crosslinked-polyethylene (MoHXLPE), ceramic-on-polyethylene (CoPE), ceramic-on-highly-crosslinked-polyethylene (CoHXLPE), ceramic-on-ceramic (CoC), and oxidized-zirconium-on-(highly-crosslinked)-polyethylene (Ox(HXL)PE). Due to small group sizes, prostheses with an oxidized-zirconium-on-standard-PE (OxPE) and oxidized-zirconium-on-highly-crosslinked-polyethylene (OxHXLPE) were analyzed together.
For demographics on all registered patients see Table 5, supplementary data. Categories for these explanatory variables were, similar to previous studies, classified using data from the LROI (Peters et al. 2016, Zijlstra et al. 2017). Procedure and implant information (surgical variables) were retrieved, e.g., fixation technique, surgical approach, and reason for revision.
Statistics
Group comparisons were made using a chi-square test to test for differences in patient and prosthesis characteristics. Survival time (with 95% confidence interval (CI)) was calculated as the time from primary THA to first revision arthroplasty for any reason, death of the patient, or the end of follow-up. Cumulative crude incidence of revision was calculated using competing risk analysis, where death was considered to be a competing risk (Lacny et al. 2015, Wongworawat et al. 2015). The consequence of using Kaplan–Meier is that the probability of revision will be overestimated (Putter et al. 2007, Keurentjes et al. 2012). Crude cumulative revision percentages within 5 and 9 years were calculated. In addition, revision rates within 9 years according to the reason for revision were estimated for different bearing types. Differences were compared using a chi-square test. In order to test for differences in revision rates between subgroups, hazard ratios were calculated using multivariable Cox proportional hazards regression analyses adjusting for possible confounding variables. The following confounders were entered into our analysis: age, sex, ASA score, diagnosis, previous operation to the affected hip joint, fixation technique, femoral head diameter, surgical approach, and period of surgery. For all covariates added, the proportional hazards assumption was checked by inspecting log-minus-log curves (Jämsen et al. 2014). Differences in revision rate for the different bearing types in patients younger than 60 or with different sizes of femoral head were assessed using multivariable Cox proportional hazards regression analyses. Due to small numbers (1,451 cases, 38 revision procedures) for the subgroup of 38 mm femoral head components, multivariable regression analysis of this subgroup was not feasible. P-values <0.05 were considered statistically significant. All analyses were performed using SPSS for Windows version 23.0 (IBM Corp, Armonk, NY, USA).
Results
The most frequently employed bearing surface between 2007 and 2016 was CoHXLPE (n = 70,175), followed by CoPE (n = 40,109), MoPE (n = 37,351), MoHXLPE (n = 32,867), CoC (n = 17,625), and Ox(HXL)PE (n = 11,785) (Table 5, Supplementary data).
Reasons for revision
The most common reason for revision was dislocation (31%), followed by femoral loosening (21%), and infection (17%) (Table 1). Revision due to dislocation was more frequently registered in THAs with a MoPE bearing surface (38%) compared with other bearing types, but less frequent in CoC and Ox(HXL)PE. Revision due to femoral loosening was more frequently registered in CoC (25%), and Ox(HXL)PE (26%). Periprosthetic fractures which necessitated revision were less frequently registered in MoPE (10%), CoPE (10%), and CoC (9%) THAs compared with other bearings (Table 1).
Table 1.
Reasons for revision or reoperation in revised THAs performed in 2007–2016 in the Netherlands (n = 6,515)
| Revision within follow-up period | MoPE (n = 1,023) |
MoHXLPE (n = 890) |
CoPE (n = 1,186) |
CoHXLPE (n = 1,649) |
CoC (n = 454) |
Ox(HXL)PE (n = 262) |
Totalc (n = 5,464) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Dislocation | 391 | 38 | 248 | 28 | 393 | 33 | 498 | 30 | 91 | 20 | 60 | 23 | 1681 | 31a |
| Loosening of acetabulum | 190 | 19 | 97 | 11 | 171 | 14 | 162 | 9.8 | 46 | 10 | 39 | 15 | 705 | 13a |
| Infection | 163 | 16 | 165 | 19 | 180 | 15 | 330 | 20 | 51 | 11 | 35 | 13 | 924 | 17a |
| Loosening of femur | 145 | 14 | 213 | 24 | 262 | 22 | 323 | 20 | 112 | 25 | 69 | 26 | 1124 | 21a |
| Periprosthetic fracture | 106 | 10 | 166 | 19 | 118 | 9.9 | 283 | 17 | 42 | 9.3 | 59 | 23 | 774 | 14a |
| Cup/liner wear | 27 | 2.6 | 17 | 1.9 | 30 | 2.5 | 29 | 1.8 | 15 | 3.3 | 9 | 3.4 | 127 | 2.3 |
| Girdlestone | 35 | 3.4 | 32 | 3.6 | 44 | 3.7 | 52 | 3.2 | 14 | 3.1 | 9 | 3.4 | 186 | 3.4 |
| Periarticular ossification | 12 | 1.2 | 19 | 2.1 | 36 | 3.0 | 23 | 1.4 | 8 | 1.8 | 2 | 0.8 | 100 | 1.8 |
| Other | 158 | 15 | 133 | 15 | 182 | 15 | 249 | 15 | 133 | 29 | 39 | 15 | 894 | 16a |
C – ceramic, HXL – highly crosslinked, M – metal, Ox – oxidized zirconium, PE – polyethylene.
p < 0.001 between different bearing types.
A patient may have more than 1 reason for revision or reoperation. As such, the total is over 100%.
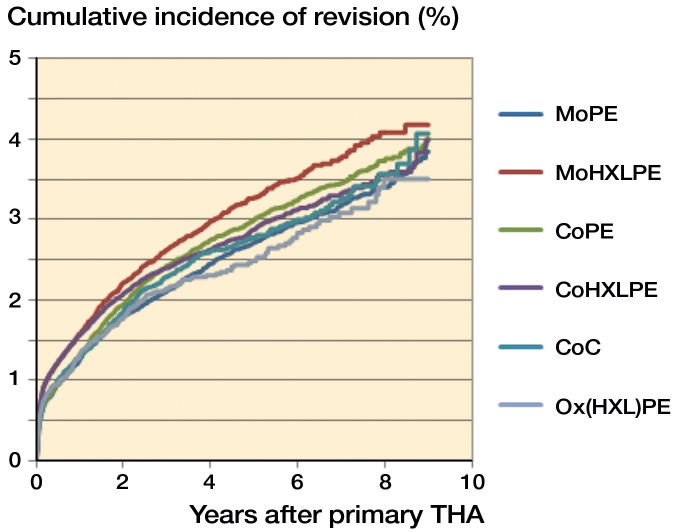
Overall crude cumulative incidence of revision
In total, 5,464 THAs were revised within the follow-up period. The overall, unadjusted 5- and 9-year cumulative incidence of revision for traditional MoPE THAs were respectively 2.7% (CI 2.5–2.9) and 3.9% (3.6–4.2) (Table 2, Figure 1). After 5 years, MoHXLPE showed a higher cumulative incidence of revision compared with MoPE. At 9 years, there were no differences in crude revision rate between the various bearings (Table 2). For MoHXLPE, crude hazard ratio (HR) for revision was higher than for MoPE (HR =1.18; CI 1.08–1.29) (Table 3). Other bearing couples did not display improved crude revision rates over MoPE.
Table 2.
Crude cumulative incidence of revision in THAs performed in 2007–2016 in the Netherlands
| Revision for any reason | MoPE (n = 37,351) % (CI) | MoHXLPE (n = 32,867) % (CI) | CoPE (n = 40,109) % (CI) | CoHXLPE (n = 70,175) % (CI) | CoC (n = 17,625) % (CI) | Ox(HXL)PE (n = 11,785) % (CI) |
|---|---|---|---|---|---|---|
| 5 year | 2.7 (2.5–2.9) | 3.3 (3.1–3.5) | 3.0 (2.8–3.2) | 2.9 (2.7–3.0) | 2.8 (2.5–3.0) | 2.5 (2.2–2.8) |
| 9 year | 3.9 (3.6–4.2) | 4.2 (3.8–4.6) | 4.0 (3.7–4.3) | 4.0 (3.6–4.4) | 4.1 (3.4–4.9) | 3.5 (3.0–4.1) |
For abbreviations, see Table 1.
Figure 1.
Cumulative incidence of revision according to bearing type of THA in the Netherlands in the period 2007–2016.
Table 3.
Multivariable survival analyses of patients with a THA in the period 2007–2016 in the Netherlands (n = 209,912)
| Articulationa | Crude hazard ratio for revision (CI) | Adjusted hazard ratio for revisionb (CI) |
|---|---|---|
| MoPE | 1.0 | 1.0 |
| MoHXLPE | 1.18 (1.08–1.29)d | 0.98 (0.88–1.09) |
| CoPE | 1.08 (0.99–1.17) | 0.99 (0.90–1.08) |
| CoHXLPE | 1.08 (1.00–1.17) | 0.87 (0.79–0.96)c |
| CoC | 1.01 (0.91–1.13) | 0.82 (0.71–0.94)c |
| Ox(HXL)PE | 0.94 (0.82–1.08) | 0.81 (0.70–0.94)c |
For abbreviations, see Table 1.
Adjusted for age at surgery, sex, ASA score, diagnosis, previous operation, fixation, head diameter, surgical approach, and period.
p < 0.05.
p < 0.001.
Overall multivariable (case-mix adjusted) revision rates
Since the risk of revision can be influenced by case-mix, prosthesis, and operation characteristics, we performed multivariable survival analyses, adjusted for age, sex, ASA, diagnosis, previous operation, fixation, head diameter, surgical approach, and period of surgery. These analyses showed that CoHXLPE, CoC, and Ox(HXL)PE had a 13–19% lower risk of revision compared with MoPE (respectively HR =0.87; CI 0.8–1.0, HR =0.82; CI 0.7–0.9, and HR =0.81; CI 0.7–0.9) (Table 3).
Revision rate in young patients (< 60 years)
In patients under 60 years, THAs with a CoHXLPE, CoC, and Ox(HXL)PE bearing surface were less frequently revised compared with traditional MoPE THAs (respectively HR =0.73; CI 0.60–0.88, HR =0.68; CI 0.55–0.85, and HR =0.74; CI 0.56– 0.98 versus HR =1.0) (Figure 2). However, after adjustment for case mix and confounders, revision rates were similar.
Figure 2.
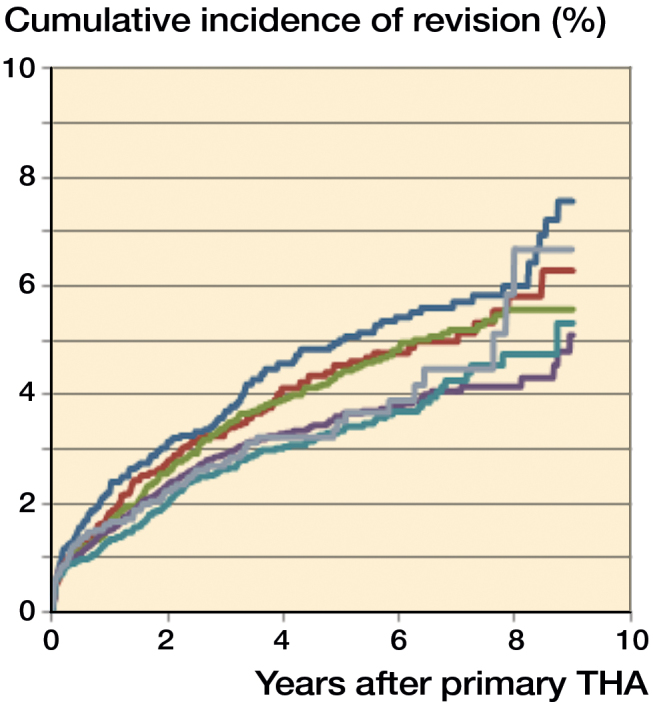
Cumulative incidence of revision according to bearing type for patients aged younger than 60.
Revision rates and femoral head size
Subgroup analyses for different femoral head sizes were performed. For small femoral head components (22–28 mm), the adjusted analyses demonstrated statistically significant lower revision rates for CoPE and CoHXLPE compared with MoPE (HR =0.9 vs. 1.0) (Table 4). Furthermore, CoC and Ox(HXL)PE demonstrated numerically lower revision rates, which, however, were not statistically significant. For 32 mm femoral heads the adjusted analyses showed a higher risk for revision for patients with CoPE bearing surface (HR =1.3, CI 1.1–1.6) (Table 4). In the 36 mm femoral head subgroup, CoC bearing THAs had a significantly lower hazard ratio compared with MoHXLPE (HR =0.7 vs. 1.0) (Table 4). The hazard ratios and associated CI for the MoPE and CoPE articulation were not applicable due to small numbers (number of revisions: MoPE 0, CoPE 1). The overall risk of revision with 22–28 mm heads was 18% higher than 32 mm heads (HR =1.2; CI 1.1–1.3), and 36 mm heads yielded a 11% higher risk over a 32 mm head (HR =1.1; CI 1.0–1.2) (data not shown in Table).
Table 4.
Multivariable survival analysis of patients with different femoral head components
| Femoral head Articulation | n (revisions) | Crude hazard ratio for revision (CI) | Adjusted hazard ratioa (CI) |
|---|---|---|---|
| 22–28 mm (n = 73,114) | |||
| MoPE | 27,423 (843) | 1.0 | 1.0 |
| MoHXLPE | 7,236 (256) | 1.3 (1.2–1.5)c | 1.1 (1.0–1.3) |
| CoPE | 22,165 (660) | 1.0 (0.9–1.1) | 0.9 (0.8–1.0)b |
| CoHXLPE | 14,188 (367) | 1.1 (1.0–1.2) | 0.9 (0.7–1.0)b |
| CoC | 1,406 (42) | 1.0 (0.7–1.4) | 0.8 (0.6–1.1) |
| Ox(HXL)PE | 696 (17) | 0.8 (0.5–1.4) | 0.7 (0.5–1.2) |
| 32 mm (n = 96,330) | |||
| MoPE | 9,908 (179) | 1.0 | 1.0 |
| MoHXLPE | 17,248 (377) | 1.4 (1.1–1.6)b | 1.1 (0.9–1.3) |
| CoPE | 17,888 (525) | 1.5 (1.3–1.8) c | 1.3 (1.1–1.6)b |
| CoHXLPE | 40,496 (877) | 1.3 (1.1–1.6)b | 1.0 (0.9–1.2) |
| CoC | 3,279 (99) | 1.5 (1.2–1.9)b | |
| Ox(HXL)PE | 7,511 (158) | 1.1 (0.9–1.4) | 0.9 (0.8–1.2) |
| 36 mm (n = 39,017) | |||
| MoPE | 13 (0) | n.a.d | n.a.d |
| MoHXLPE | 8,124 (253) | 1.0 | 1.0 |
| CoPE | 56 (1) | n.a.d | n.a.d |
| CoHXLPE | 15,490 (405) | 1.0 (0.8–1.1) | 0. 9 (0.8–1.1) |
| CoC | 11,756 (280) | 0.8 (0.6–0.9)b | 0.7 (0.6–0.9)b |
| Ox(HXL)PE | 3,578 (87) | 0.9 (0.7–1.2) | 0.9 (0.7–1.1) |
Adjusted for sex, ASA score, diagnosis, previous operation, fixation, surgical approach, and period.
p < 0.05.
p < 0.001.
n.a. = not applicable; hazard ratios and confidence intervals for the MoPE and CoPE articulation were not applicable due to small number of revisions.
Conventional versus highly-crosslinked-polyethylene
Adjusted overall hazard ratios were similar between THAs with highly-crosslinked-polyethylene acetabular components compared with standard PE (Table 8, Supplementary data). However, revisions due to loosening of the acetabular component or liner wear were less frequently observed with HXLPE THAs compared with traditional PE (respectively 10% and 1.8% vs. 17% and 2.7%). Revision due to recurrent dislocation was performed more frequently in THAs with conventional PE (35%) versus HXLPE (29%) (Table 9, Supplementary data).
Discussion
There is an ongoing interest in alternative bearing surfaces in THA in order to further improve survivorship and reduce the risk of revision surgery. We found a statistically significant benefit in mid-term revision rates for CoHXLPE, CoC, and Ox(HXL)PE bearings compared with a traditional MoPE bearing surface. Furthermore, stratified analyses for small femoral heads (22–28 mm) demonstrated lower revision rates for CoPE and CoHXLPE bearings. For THAs with a 36 mm femoral head, CoC resulted in a lower risk for revision.
It has been hypothesized that modern bearing surfaces such as ceramics, oxidized-zirconium, and HXLPE articulations can decrease revision rates compared with traditional MoPE THAs. Historically, aseptic loosening is the most frequent cause of revision in THA (LROI annual report 2015, Norwegian Arthroplasty Register 2016). Over time, wear of the polyethylene liner in a traditional MoPE counterface can generate an adverse local host response, which can result in periprosthetic osteolysis and subsequent aseptic loosening of components (Hu et al. 2015, Varnum et al. 2015). This process is even more relevant in young patients with increased activity demands. Alternative bearing surfaces were introduced in order to reduce PE wear. Ceramic is harder and offers more scratch resistance than cobalt-chrome, which improves lubrication through a low friction coefficient, resulting in excellent wear resistance and low osteolysis rate (Wang et al. 2013, Hu et al. 2015). A meta-analysis of RCTs reporting on the comparison between CoC and MoPE bearing surfaces concluded that CoC resulted in lower revision rates, osteolysis, loosening of components and dislocation, despite more squeaking (Hu et al. 2015). Well-documented drawbacks for ceramic components include high cost and adverse events, such as intra- or postoperative ceramic fractures, and audible squeaking (Hu et al. 2015, Wyles et al. 2015). In the Danish Arthroplasty Registry incidences of ceramic head and liner fractures of respectively 0.28% and 0.17% have been reported (Varnum et al. 2015).
Ceramicized metal or oxidized zirconium (Oxinium, Smith & Nephew, Memphis, TN, USA) for femoral heads was developed during the 1980s in an attempt to reduce PE wear. Oxidized-zirconium femoral head components consist of a 5 µm-thick ceramic layer on the metal alloy core, which makes it more resistant to fractures compared with alumina ceramic heads (Jassim et al. 2015). Data from the AOANJRR demonstrated the lowest revision rates for ceramicized-metal-on-HXLPE with a 10-year follow-up. The cumulative incidence of revision was 3.2% (2.9–3.7) compared with 6.3% (6.1–6.6) for traditional MoPE bearing after 10 years. However, these results need to be interpreted with caution since the ceramicized-metal-HXLPE bearing is a single-company product with a small number of femoral stem and acetabular component combinations, which may have a confounding effect on the outcome (Annual Report AOANJRR 2016).
HXLPE was developed to decrease wear in traditional PE liners and subsequently decrease the incidence and severity of osteolysis. Mall et al. (2011) compared the incidence of osteolysis in conventional PE versus HXLPE in young patients (under 50 years of age) undergoing primary THA using radiographs and computed tomography: HXLPE diminished the incidence of osteolysis by 92% compared with conventional PE. The AOANJRR demonstrated that HXLPE had a lower rate of revision compared with non-HXLPE. The difference increased with time and at 15 years the cumulative percentage of revision is 5.6% for HXLPE and 11% for non-HXLPE THAs. Fewer revisions for loosening and dislocation were observed. Other registries, e.g., Kaiser Permanente and NJR, did not report on differences in survival between THAs with conventional and highly-crosslinked PE components, but did also show advantages of ceramics. In the Netherlands, we found a similar overall risk for revision for HXLPE and conventional PE THAs with a short-term follow-up. A similar shift in reasons for revision was observed in the Netherlands. Revisions due to loosening of the acetabular component or liner wear were less frequently observed in HXLPE THAs compared with traditional PE. Revision due to recurrent dislocations was performed more frequently in THAs with conventional PE compared with HXLPE. This can be explained by a preferential use of larger femoral head components in THAs with HXLPE (data not shown). In addition, Jassim et al. (2015) found that the effect of using an HXLPE liner was more important in reducing component wear than the choice of the femoral head bearing (either ceramic or cobalt-chromium).
In the Netherlands, revision due to dislocation was more frequently encountered in MoPE THAs (38%) compared with other bearing types, which could be related to a high proportion of small femoral head components (22–28mm) in this group (73%) (Table 5, Supplementary data). Femoral loosening as reason for revision was more frequently registered in CoC (25%) and Ox(HXL)PE (26%) THAs. Theoretically, this could be associated with the large proportion of uncemented THAs in these bearing type groups (respectively 89% and 55%). Periprosthetic fractures which necessitate revision were less common in MoPE (10%), CoPE (10%), and CoC (9%) THAs compared with other bearings. Theoretically, this could be explained by a large proportion of cemented fixations in THAs with MoPE and CoPE bearings.
In our dataset, metal-on-metal THAs were excluded. National Arthroplasty Registry data have demonstrated inferior results for large-diameter MoM THAs. The use of these articulations has been associated with wear-related adverse events, e.g., soft tissue inflammatory reactions to metal debris, including inflammatory pseudotumors and aseptic lymphocytic vasculitis-associated lesions (Drummond et al. 2015, Nederlandse Orthopaedische Vereniging 2015, Rieker 2017).
We performed a detailed analysis in order to assess the influence of bearing surface on survival of the THAs in young (< 60 years), generally more active patients (n = 34,204). We found a statistically significantly lower crude cumulative incidence of revision for advanced bearing surfaces such as CoHXLPE, CoC, and Ox(HXL)PE, over MoPE. However, after adjustment for confounding variables, no statistically significant differences at mid-term follow-up were found. This trend favoring the use of ceramics, HXLPE, and oxidized-zirconium components was consistent with results in patients aged under 55 years in the AOANJRR (Annual Report AOANJRR 2016).
We performed further subgroup analyses to assess the influence of bearing type in THAs with different femoral head components. Our results from patients with a small femoral head component demonstrate a reduced risk of revision for CoPE, CoHXLPE, CoC, and Ox(HXL)PE, compared with MoPE after correction for confounding variables. Although this phenomenon was visible for all alternative bearing surfaces, only CoPE and CoHXLPE demonstrated statistically significant differences.
In the large femoral head component (36 mm) subgroup, significantly lower revision rates for CoC THAs were determined compared with the MoHXLPE reference bearing surface. Theoretically, the benefits of advanced bearing surfaces with more wear-resistant characteristics would increase with increasing size of the femoral head components since large femoral heads might cause more PE wear and taper corrosion. Respectively, the use of HXLPE and ceramic or oxidized-zirconium heads may presumably lead to less wear and taper corrosion (Ries and Pruitt 2005, Zijlstra et al. 2017).
Our study should be interpreted with its limitations in mind. Possible differences in survival are expected to be found in the long term. Our study has limited follow-up with a mean follow-up of 3.9 years and a maximum of 9.9 years. We acknowledge that variation in bearing type may result in possible differences in survival due to wear or loosening of components that will not be detected within our follow-up. Second, national registry studies are based on observational data and therefore cannot infer causality. Furthermore, our data limit the ability to comment on the effect of individual components, which may be an unknown confounder. However, a prosthesis-specific analysis of frequently registered stem components did demonstrate a similar trend of superior results for THA with advanced bearing surfaces. Lastly, comparing different bearing surfaces inherently results in a confounding by indication bias, which cannot be discounted. This phenomenon was also present in our data, but was statistically corrected for by multivariable Cox proportional regression analysis.
In summary, based on nationwide arthroplasty registry data, the use of a ceramic-on-highly-crosslinked-polyethylene (CoHXLPE), ceramic-on-ceramic (CoC), and oxidized- zirconium-on-(highly-crosslinked)-polyethylene (Ox(HXL)PE) bearing surfaces resulted in significantly better mid-term survival rates compared with traditional MoPE in the Netherlands.
Supplementary data
Tables 5–9 are available as supplementary data in the online version of this article, http://dx.doi.org/10.1080/17453674.2017.1405669
The authors contributed to: (1) study design and study protocol, (2) gathered data, (3) analyzed data, (4) initial draft, and (5) final draft. RMP and WPZ. contributed to: (1), (2), (3), (4), (5); LNS contributed to: (2), (3), (4), (5); MS contributed to: (1), (2), (3), (4), (5); PCR contributed to: (1), (4), (5); SKB contributed to: (1), (4), (5).
Acta thanks Richard de Steiger and other anonymous reviewers for help with peer review of this study.
Supplementary Material
References
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Annual report 2016. [Google Scholar]
- Dutch Arthroplasty Register (LROI). Annual report. LROI report, 2015. [Google Scholar]
- Drummond J, Tran P, Fary C.. Metal-on-metal hip arthroplasty: A review of adverse reactions and patient management. J Funct Biomater 2015; 6 (3): 486–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu D, Tie K, Yang X, Tan Y, Alaidaros M, Chen L.. Comparison of ceramic-on-ceramic to metal-on-polyethylene bearing surfaces in total hip arthroplasty: A meta-analysis of randomized controlled trials. J Orthop Surg Res 2015; 10: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jämsen E, Eskelinen A, Peltola M, Mäkelä K.. High early failure rate after cementless hip replacement in the octogenarian. Clin Orthop Rel Res 2014; 472 (9): 2779–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jassim S S, Patel S, Wardle N, Tahmassebi J, Middleton R, Shardlow D L, Stephen A, Hutchinson J, Haddad F S.. Five-year comparison of wear using oxidised zirconium and cobalt-chrome femoral heads in total hip arthroplasty: A multicentre randomised controlled trial. Bone Joint J 2015; 97-B (7): 883–9. [DOI] [PubMed] [Google Scholar]
- Keurentjes J C, Fiocco M, Schreurs B W, Pijls B G, Nouta K A, Nelissen R G H H.. Revision surgery is overestimated in hip replacement. Bone Joint Res 2012; 1 (10): 258–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacny S, Wilson T, Clement F. Roberts D J, Faris P D, Ghali W A, Marshall D A.. Kaplan–Meier survival analysis overestimates the risk of revision arthroplasty: A meta-analysis. Clin Orthop Relat Res 2015; 473 (11): 3431–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mall N A, Nunley R M, Zhu J J, Maloney W J, Barrack R L, Clohisy J C.. The incidence of acetabular osteolysis in young patients with conventional versus highly crosslinked polyethylene. Clin Orthop Relat Res 2011; 469 (2): 372–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihalko W M, Wimmer M A, Pacione C A, Laurent M P, Murphy R F, Rider C.. How have alternative bearings and modularity affected revision rates in total hip arthroplasty? Clin Orthop Relat Res 2014; 472 (12): 3747–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nederlandse Orthopaedisch Vereniging. Advies Metaal-op-Metaal Heupprothesen per 1 augustus 2015. [Google Scholar]
- Norwegian Arthroplasty Register. Norwegian National Advisory Unit on Arthroplasty and Hip Fractures (NNAUoAaHF). Annual Report, 2016. [Google Scholar]
- Peters R M, van Steenbergen L N, Bulstra S K, Zeegers A V C M, Stewart R E, Poolman R W, Hosman A H.. Nationwide review of mixed and non-mixed components from different manufacturers in total hip arthroplasty. Acta Orthop 2016; 87 (4): 356–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putter H, Fiocco M, Geskus R B.. Tutorial in biostatistics: Competing risks and multi-state models. Stat Med 2007; 26 (11): 2389–430. [DOI] [PubMed] [Google Scholar]
- Rieker C B. Tribology of total hip arthroplasty prostheses: What an orthopaedic surgeon should know. EFORT Open Rev 2017; 1 (2): 52–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ries M D, Pruitt I.. Effect of cross-linking on the microstructure and mechanical properties of ultra-high molecular weight polyethylene. Clin Orthop Relat Res 2005; 440: 149–56. [DOI] [PubMed] [Google Scholar]
- Varnum C, Pedersen A B, Kjaersgaard-Andersen P, Overgaard S.. Comparison of the risk of revision in cementless total hip arthroplasty with ceramic-on-ceramic and metal-on-polyethylene bearings. Acta Orthop 2015; 86 (4): 477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Steenbergen L N, Denissen G A, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, Nelissen R G.. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86 (4): 498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vektis http://www.vektis.nl; 2017. [Google Scholar]
- Wang S, Zhang S, Zhao Y.. A comparison of polyethylene wear between cobalt-chrome ball heads and alumina ball heads after total hip arthroplasty: A 10-year follow-up. J Orthop Surg Res 2013; 8:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongworawat M D, Dobbs M B, Gebhardt M C, Gioe T J, Leopold S S, Manner P A, Rimnac C M, Porcher R.. Editorial: Estimating survivorship in the face of competing risks. Clin Orthop Relat Res 2015; 473 (4): 1173–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyles C C, Jimenez-Almonte J H, Murad M H, Murad M H, Norambuena-Morales G A, Cabanela M E, Sierra R J, Trousdale R T.. There are no differences in short- to mid-term survivorship among total hip-bearing surface options: A network meta-analysis. Clin Orthop Relat Res 2015;473 (6): 2031–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin S, Zhang D, Du H, Du H, Yin Z, Qiu Y.. Is there any difference in survivorship of total hip arthroplasty with different bearing surfaces? A systematic review and network meta-analysis. Int J Clin Exp Med 2015; 8 (11): 21871–85. [PMC free article] [PubMed] [Google Scholar]
- Zijlstra W P, De Hartog B, Van Steenbergen L N, Scheurs B W, Nelissen R G H H.. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty, Acta Orthop 2017; 88 (4): 392–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.