Abstract
Background
The relative importance of different attitudes in predicting vaccination among healthcare personnel (HCP) is unclear. We hypothesized that HCP who feel at risk without vaccination or say they would regret not getting vaccinated would be more likely to get vaccinated than HCP who do not expect these emotional benefits.
Methods
A prospective cohort of 1544 HCP with direct patient care was enrolled from September 18 to December 18, 2010 at Scott & White Healthcare in Texas and Kaiser Permanente Northwest in Oregon and Washington. An Internet-based questionnaire assessed pre-season intention to be vaccinated and included 12 questions on attitudes about vaccination: single-item measures of perceived susceptibility and vaccine effectiveness, 5 items that were summed to form a concerns about vaccine scale, and 5 items summed to form an emotional benefits of vaccination scale. Influenza vaccination status for the 2010–2011 season and for 5 prior seasons was confirmed by medical record extraction.
Results
There were significant differences between vaccinated and unvaccinated HCP on all attitude items; 72% of vaccinated HCP agreed that they “worry less about getting the flu” if vaccinated, compared to only 26% of the unvaccinated (odds ratio = 7.4, 95% confidence interval = 5.8–9.5). In a multivariate model, the emotional benefits scale was the strongest predictor of 2010–2011 seasonal influenza vaccination, after adjusting for other attitude measures, prior vaccination history, and pre-season intention to be vaccinated. The predictive value of the emotional benefits scale was strongest for HCP with low preseason intention to be vaccinated, where HCP vaccine receipt was 15% versus 83% for those with low versus high scores on the emotional benefits scale.
Conclusions
The expected emotional benefits of vaccination strongly affect seasonal influenza vaccination among HCP, even after taking into account other attitudes, pre-season intentions, and prior vaccination history. These attitudes are promising targets for future vaccination campaigns.
Keywords: Health care personnel, Health care workers, Influenza vaccination, Attitudes, Emotion
1. Introduction
With persistently low rates of voluntary vaccination [1–4] and debates over mandatory vaccination policies [5–10], influenza vaccination among healthcare personnel (HCP) has become a national and international health issue [11–15]. Although reviews have identified common barriers [1,3,14], including doubts about vaccine safety and effectiveness, the relative importance of different attitudes in predicting subsequent vaccination among HCP [13,16] and the best attitudes to target in vaccination campaigns remain unclear [17–19].
In a prospective cohort study of 1544 HCP who provide direct patient care in two medical systems, we pursued three objectives. First, following two previous studies of university students and employees that found emotions play a central role in vaccination decisions [20,21], we hypothesized that HCP who feel at risk without vaccination or say they would regret not getting vaccinated would be more likely to get vaccinated than HCP who do not, even after adjusting for other more commonly studied attitudes, such as perceived susceptibility, vaccine effectiveness, and safety.
Our second objective was to examine the extent to which pre-season intentions (or the perceived likelihood of getting vaccinated) predict subsequent vaccination behavior. Although multiple theories agree that intentions are a key determinant of health behavior [22] and previous studies have noted a gap between anticipated acceptance of vaccine and subsequent vaccine uptake [19,23–25], influenza vaccination intentions and actions have not been examined prospectively among HCP.
Given repeated findings that receipt of seasonal influenza vaccine in prior seasons is the best predictor of subsequent vaccination behavior [1,3,13], our third objective was to examine whether expectations about the emotional benefits of vaccination and other attitudes help to predict vaccination after taking into account prior vaccination history. Our goal was to identify attitudes that varied substantially among HCP and predicted subsequent vaccination, even after adjusting for prior vaccination habits and pre-season intentions, since such attitudes would be promising targets for vaccination campaigns and tailored interventions [17,18].
2. Methods
2.1. Participants
A prospective cohort of HCP was enrolled from September 18 to December 18, 2010 at Scott & White Healthcare (SWH) in central Texas and Kaiser Permanente Northwest (KPNW) located in Oregon and Washington. At both sites influenza vaccination is strongly encouraged but not mandatory, supported by month-long information campaigns and system-wide email reminders, and made available for free at clinics or nursing carts at all medical facilities. Eligible enrollees were: (a) aged 18–65 years, (b) working full-time (≥32 h per week), (c) employed by and receiving medical care from the healthcare system for >12 months, and (d) providing direct patient care, defined as “regular, close, face-to-face, handson contact with patients as part of a typical work shift, including regular contact within 3 feet of patients for 5 minutes or more” [26]. Multiple announcements and email invitations regarding a study of “respiratory illness and healthcare workers” were targeted to all employees over a 6-week period and all potentially eligible employees were encouraged to contact study personnel to be screened and if eligible, invited to participate. In cooperation with local employee health representatives, each site estimated the number of eligible HCP (according to the study criteria) by sex, age group, and occupation group prior to the start of the study. Additional announcements and invitations were targeted to male HCP and to physicians, nurse practitioners, and physician assistants at both sites due to lower than expected volunteer response in these categories. Participants were offered small incentives in the form of cash or gift cards ($50 at SWH and $25 at KPNW) upon completion of the enrollment questionnaire.
2.2. Procedures
Study procedures, informed consent documents, and data collection instruments were reviewed and approved by Institutional Review Boards at both sites. Consented participants completed an Internet-based questionnaire at home or on facility computers. Both sites had integrated electronic medical record (EMR) systems and separate electronic vaccination registries maintained by their employee health services. Presence of a chronic medical condition was identified by a medical visit during the prior year in EMR for a medical condition associated with increased risk of influenza complications [4] (codes available from the authors). Influenza vaccination status for the 2010–2011 season and for 5 prior seasons was confirmed by employee health records and EMR, so that vaccinations provided via employee health or their personal HCP would be captured. Prior influenza vaccination history was represented with three ordinal categories: (a) consistent vaccinees had records of annual vaccination for all seasons going back 5 years or since their hiring date; (b) inconsistent vaccinees had at least one vaccination record but not consistent and consecutive vaccinations; (c) the remaining HCP had no records indicating receipt of influenza vaccination prior to the 2010–2011 season.
2.3. Questionnaire
The questionnaire included items on demographic, occupational, and health factors (Table 1), pre-season intention to be vaccinated, and 12 attitudes about influenza vaccination (Table 2). The questionnaire was presented in English with readability Flesch—Kincaid Grade Level of 7.5. Pre-season intention to be vaccinated was measured by asking: “What are the chances that you will get a seasonal flu vaccination this year?” A 7-point verbal description of likelihood was used (Table 2, footnote c), similar to prior studies [21,27,28]. The 12 attitude items (Table 2) included two previously used single-item indicators for perceived susceptibility to influenza without vaccine (item 1) [21,27] and perceived vaccine effectiveness (item 2) [21]. Concerns about the influenza vaccine were assessed with previously studied items on side-effects (items 3–5) [21,29] and available information (item 6) [30], plus a new item on trust in guidelines (item 7). Items on the expected emotional benefits of vaccination were drawn from prior research [20,21] and included feeling at risk without vaccination (items 8 and 9), anticipated regret if not vaccinated (items 10 and 11), and anticipated reduction in worry if vaccinated (item 12). A principal component factor analysis with orthogonal rotation of items 3–12 confirmed a two factor solution (61.0% of variance) suggesting two scales: (a) concerns about vaccine (items 3–7, Eigenvalue = 1.71, Cronbach’s α = 0.73) and (b) emotional benefits of vaccination (items 8–12, Eigenvalue = 4.37, Cronbach’s α = 0.89).
Table 1.
Descriptive statistics for demographic, occupational, medical care setting, health status, and prior influenza vaccination variables for 1544 healthcare personnel.
| N | (%) | |
|---|---|---|
| Demographics | ||
| Female | 1226 | (79.4) |
| Age (years) | ||
| 18–34 | 581 | (37.6) |
| 35–49 | 594 | (38.5) |
| 50–65 | 369 | (23.9) |
| Race (White) | 1198 | (77.6) |
| Married | 959 | (62.1) |
| Education | ||
| High school | 112 | (7.3) |
| Some college | 382 | (24.7) |
| Bachelor degree | 753 | (48.8) |
| Masters | 77 | (5.0) |
| Advanced graduate | 220 | (14.2) |
| Occupation and medical care setting | ||
| Occupation | ||
| Physicians | 204 | (13.2) |
| PA, NP, and RN managersa | 124 | (8.0) |
| Nurses | 552 | (35.8) |
| Allied professional | 664 | (43.0) |
| Patient care for >10 years | 809 | (52.0) |
| Medical care setting | ||
| Outpatient | 1013 | (65.6) |
| Intensive care unit | 556 | (36.0) |
| Hospital | 988 | (64.0) |
| Emergency department | 424 | (27.5) |
| Study site | ||
| Scott & White Healthcare | 1099 | (71.2) |
| Kaiser Permanente | 445 | (28.8) |
| Health status | ||
| Subjective: very good or excellent | 1257 | (81.4) |
| Smoker | 108 | (7.0) |
| BMI >30 | 537 | (34.8) |
| High risk condition | 472 | (30.6) |
| Influenza vaccination history for prior 5 yearsb | ||
| None recorded | 289 | (18.7) |
| Inconsistent | 689 | (44.6) |
| Consistent | 566 | (36.7) |
Physician assistant (PA), nurse practitioner (NP), and nurse (RN) manager.
Consistent vaccinees had confirmed records of annual vaccination for all seasons going back 5 years or since their hiring date; inconsistent vaccinees had at least one vaccination record but no consistent history over consecutive years.
Table 2.
Attitudes toward influenza vaccination including the means and standard deviations (SD) for items and scales, the percentage who agreed with each item, and the crude odds ratio (COR) and confidence interval (CI) of vaccination for those who agreed, among 460 unvaccinated and 1084 vaccinated healthcare personnel during the 2010–2011 influenza season.
| Category | Item number | Item phrasing and response options |
Not vaccinated (n = 460)
|
Vaccinated (n = 1084)a
|
COR | (95% CI)b | ||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | % agree | Mean (SD) | % agree | |||||
| Perceived susceptibility itemc | 1 | Imagine that the flu vaccine for this year is unavailable and you are therefore unable to get the vaccine. If you do not get a flu vaccination, what do you think your chance of getting the flu this year will be? | 3.0 (1.2) | 5.3% | 4.0 (1.2) | 24.7% | 6.0 | (3.9–9.2) |
| Perceived effectiveness of vaccine itemd | 2 | How effective do you think the seasonal flu vaccination is in preventing you from getting the seasonal flu? | 2.8 (0.8) | 69.1% | 3.4 (0.6) | 95.7% | 10.1 | (7.1–14.4) |
| Concerns about vaccine itemse | 3 | The flu vaccine could give me the flu | 2.7 (1.3) | 28.7% | 1.9 (1.1) | 10.2% | 0.3 | (0.2–0.4) |
| 4 | Systemic adverse effects from the flu vaccine are rare (reverse scored) | 3.4 (1.1) | 46.3% | 3.8 (1.0) | 64.4% | 2.1 | (1.7–2.6) | |
| 5 | I am concerned about side effects from the influenza vaccine | 3.0 (1.3) | 40.9% | 2.2 (1.1) | 16.4% | 0.3 | (0.2–0.4) | |
| 6 | I am concerned that there may be something that I do not know about the flu vaccine | 2.6 (1.3) | 26.3% | 2.3 (1.1) | 16.6% | 0.6 | (0.4–0.7) | |
| 7 | I trust guidelines by the CDC and the US Advisory Committee on Immunization Practices that recommend that all health care workers get an annual influenza vaccination (reverse scored) | 3.5 (1.2) | 50.7% | 4.4 (0.9) | 86.0% | 6.0 | (4.6–7.7) | |
| Concerns about vaccine scale | Sum of items 3–7 (range 5–25) | 13.5 (4.1) | 10.1 (3.5) | |||||
| Emotional benefits of vaccination itemse | 8 | With no flu vaccination, I would feel that I am going to get the flu this year | 2.0 (1.1) | 10.5% | 3.0 (1.2) | 35.8% | 4.8 | (3.5–6.6) |
| 9 | With no flu vaccination, I would feel very vulnerable to the flu | 2.2 (1.2) | 14.8% | 3.4(1.2) | 55.4% | 7.1 | (5.3–9.5) | |
| 10 | If I do not get a flu vaccination, I will regret it | 2.0 (1.2) | 13.1% | 3.3 (1.3) | 46.9% | 5.9 | (4.4–7.9) | |
| 11 | If I do not get a flu vaccination and end up getting the flu, I would be mad at myself for not getting the vaccine | 2.3 (1.4) | 24.5% | 3.5 (1.4) | 58.3% | 4.3 | (3.4–5.5) | |
| 12 | I worry less about getting the flu if I get a flu vaccination | 2.6 (1.3) | 26.1% | 3.9 (1.1) | 72.4% | 7.4 | (5.8–9.5) | |
| Emotional benefits scale | Sum of items 8–12 (range 5–25) | 11.1 (5.1) | 17.2 (4.8) | |||||
All student t-tests comparing means of items and scale scores between vaccinated and unvaccinated HCP were statistically significant (p < .001).
Crude odds ratio (COR) compares the odds of vaccination among those who agree with the attitude compared to those who disagree.
Options for susceptibility (item 1): 1 = almost zero chance, 2 = very small chance, 3 = small, 4 = moderate, 5 = large, 6 = very large chance, 7 = almost certain; agree = 5 (large) or greater.
Options for vaccine effectiveness (item 2): 1 = not at all effective, 2 = not too effective, 3 = somewhat effective, 4 = very effective; agree = 3 (somewhat) or 4 (very effective).
Options for items 3–12: 1 = strongly disagree, 2 = mildly disagree, 3 = neutral, 4 = mildly agree, 5 = strongly agree; agree = 4 (mildly) or 5 (strongly agree).
2.4. Analysis
Pearson correlations and linear regression were applied to examine associations among attitude measures (as standardized scores, with one unit equal to one standard deviation), pre-season intention, and vaccination history. Logistic regression was applied to examine the univariate and multivariate associations with 2010–2011 seasonal vaccination status. Attitude measures were categorized into quartiles for analysis to facilitate interpretation, comparison, and consideration of possible non-linear associations with vaccination. Patient characteristics (Table 1) were included as potential confounders in the final multivariate model, starting with significant (p < .1) univariate predictors and removing nonsignificant factors (p > .01) in a stepwise backward fashion [31,32]. Interaction terms were also assessed in a final multivariate model to test whether the magnitude of any significant attitude-vaccination association varied by the level of pre-season intention or by vaccination history [33]. All analyses were conducted using PASW Statistics 18.0 (Armonk, NY).
3. Results
3.1. Characteristics of participants
Across sites, 2393 individuals were screened by study personnel (SWH = 1343; KPNW = 1050). Of these, 314/2393 (13.1%; SWH = 118; KPNW = 196) were ineligible; the most common reasons were not meeting direct patient care criteria (186/314, 59.2%), not working full time (61/314, 19.4%), and not working and receiving health care at the site for >12 months (38/314, 12.1%). An additional 264/2393 (11.0%; SWH = 120; KPNW = 144) refused or failed to complete the consent and enrollment process. In total, 1815/2393 (75.8%) of screened HCP were eligible, consented, and completed enrollment. Based on each site’s estimate of the total number of potentially eligible HCP, KPNW enrolled 710/3550 (20%) and SWH enrolled 1105/2757 (40.1%) of their source populations. Supplemental Table A presents the number of enrolled participants divided by the estimated number of eligible HCP by sex, age group, and occupation group. The estimated proportion of volunteers was high for all categories of females at SWH (850/1917, 40%), but lower among male HCP (225/840, 30%), and especially men over age 50. The proportion of volunteers was lower overall at KPNW, but we observed a similar lower ratio of volunteers among male HCP (116/990, 12%) compared to female HCP (595/2560, 23%) and lower volunteer ratios among the highest occupation category, which included physicians.
Finally, because this study centered on the prediction of vaccination from pre-season attitudes and intentions, of the 1815 enrollees, this study excluded 34 (1.9%) participants with incomplete enrollment questionnaires, 229 (12.6%) who completed the questionnaire after being vaccinated, and 8 (0.4%) who completed the questionnaire after the start of local influenza circulation.
The demographic characteristics for the combined sample of 1544 HCP with direct patient care are presented in Table 1. The mean age of participants was 40.8 years, 79.4% were female, and 77.6% were white. The characteristics of participants at the two study sites were similar, with the exceptions that KPNW participants were more likely to be female and older, and SWH included more non-white and Hispanic participants (data not presented).
Seventy percent of participants (1084/1544) received 2010–2011 seasonal influenza vaccination. Uptake was higher for participants at SWH (794/1099, 72.2%) than KPNW (290/445, 65.2%), which reflected similar differences reported for all employees by employee health services at both sites (SWH = 71%, KPNW = 64%). In a post-season survey completed by 1475/1544 (95.5%) enrollees, only 36/1475 (2.4%) participants self-reported that they received a seasonal vaccination but lacked a corresponding medical record. These were counted as non-vaccinees in our analyses. However, in sensitivity analyses, results did not differ when self-reported vaccination status was used as the outcome.
3.2. Attitudes and vaccination
There were significant differences between vaccinated and unvaccinated HCP on all 12 attitude items (p < .001) (Table 2). Perceived susceptibility to influenza if not vaccinated was rated as large or higher among <25% of HCP, but the odds of vaccination among HCP who described their susceptibility as “large” or higher were 6 times higher than those who described their susceptibility as “moderate” or lower. Similarly, the majority of vaccinated and unvaccinated HCP believed the influenza vaccine was effective, but the odds of vaccination among HCP who described the vaccine as “somewhat” or “very effective” were 10 times higher than those who described the vaccine as “not too” or “not at all effective”. Less than half of the vaccinated and unvaccinated HCP expressed concerns about the vaccine (items 3–6), but those who had concerns were 40–70% less likely to be vaccinated. In contrast, HCP who believed systemic adverse effects are rare and trusted guideline recommendations for annual vaccination had odds of vaccination that were 2 and 6 times higher, respectively. The odds of vaccination among HCP with very low concerns about vaccine scores were 55.8 times higher than HCP with high levels of concern (Table 3).
Table 3.
Factors associated with 1544 healthcare personnel’s receipt of 2010–2011 influenza vaccination, with crude odds ratio (COR) and confidence interval (CI) for each factor and the multivariate logistic regression model with only statistically significant predictors and their adjusted odds ratio (AOR).
| Factors | COR | (95% CI) | AOR | (95% CI)c |
|---|---|---|---|---|
| Demographics/occupation | ||||
| Age (50–65 years) | 1.5 | (1.2–2.0) | – | |
| Race (White) | 1.3 | (1.0–1.7) | – | |
| Married | 1.6 | (1.3–2.0) | 1.4 | (1.0–1.9) |
| Occupation (PA, NP, or RN manager)a | 1.6 | (1.0–2.5) | – | |
| Medical setting (Emergency Department) | 0.6 | (0.5–0.8) | 0.5 | (0.4–0.7) |
| Study site (Scott & White Healthcare) | 1.4 | (1.1–1.8) | – | |
| Influenza vaccination history for prior 5 yearsb | ||||
| None recorded (ref) | 1.0 | 1.0 | ||
| Inconsistent | 8.3 | (6.1–11.4) | 2.6 | (1.7–3.8) |
| Consistent | 23.6 | (16.3–34.3) | 4.3 | (2.7–6.8) |
| Pre-season intention to be vaccinated | ||||
| Almost zero chance (1) | 1.0 | 1.0 | ||
| Very small, small, or moderate (2–4) | 7.1 | (4.6–11.0) | 3.6 | (2.1–6.3) |
| Large or very large (5–6) | 20.0 | (11.9–33.7) | 9.8 | (4.6–21.06) |
| Almost certain (7) | 61.4 | (29.5–95.6) | 24.3 | (10.1–58.1) |
| Attitudes | ||||
| Perceived susceptibility | ||||
| Zero or very small chance (1–2) | 1.0 | 1.0 | ||
| Small (3) | 3.8 | (2.7–5.2) | 1.8 | (1.1–2.8) |
| Moderate (4) | 6.5 | (4.7–8.9) | 1.6 | (1.0–2.4) |
| Large, very large, certain (5–7) | 20.9 | (12.8–34.0) | 2.8 | (1.5–5.5) |
| Perceived vaccine effectiveness | ||||
| Not at all effective | 1.0 | 1.0 | ||
| Not too effective | 2.6 | (0.9–7.8) | 0.8 | (0.2–3.2) |
| Somewhat effective | 15.9 | (5.5–45.8) | 0.9 | (0.3–3.9) |
| Very effective | 53.4 | (18.1–157.6) | 1.2 | (0.3–5.0) |
| Concerns about vaccine scale | ||||
| No concerns (5–9) | 55.8 | (19.5–159.9) | 4.1 | (1.2–13.9) |
| Low (10–14) | 16.6 | (5.9–47.2) | 2.5 | (0.8–8.3) |
| Moderate (15–19) | 6.7 | (2.3–19.5) | 1.8 | (0.5–6.0) |
| High concerns (20–25) (referent) | 1.0 | 1.0 | ||
| Emotional benefits scale | ||||
| No benefit (5–9) (referent) | 1.0 | 1.0 | ||
| Low (10–14) | 4.9 | (3.6–6.7) | 2.0 | (1.0–4.8) |
| Moderate (15–19) | 13.1 | (9.1–18.8) | 6.8 | (2.0–22.3) |
| High benefit (20–25) | 23.3 | (15.5–34.9) | 11.7 | (2.1–63.9) |
| Emotional benefits × pre-season intention | ||||
| No benefit (5–9) × intention referent | 1.0 | |||
| Low (10–14) × intention | 0.89 | (0.74–0.99) | ||
| Moderate (15–19) × intention | 0.76 | (0.60–0.94) | ||
| High benefit (20–25) × intention | 0.70 | (0.51–0.92) |
Physician assistant (PA), nurse practitioner (NP), and nurse (RN) manager.
Consistent vaccinees had confirmed records of annual vaccination for all seasons going back 5 years or since their hiring date; inconsistent vaccinees had at least one vaccination record but no consistent history over consecutive years.
All demographic and occupational variables with significant univariate associations with vaccination were entered in the initial multivariate model, and then non-significant variables were removed as controls through backward stepwise elimination.
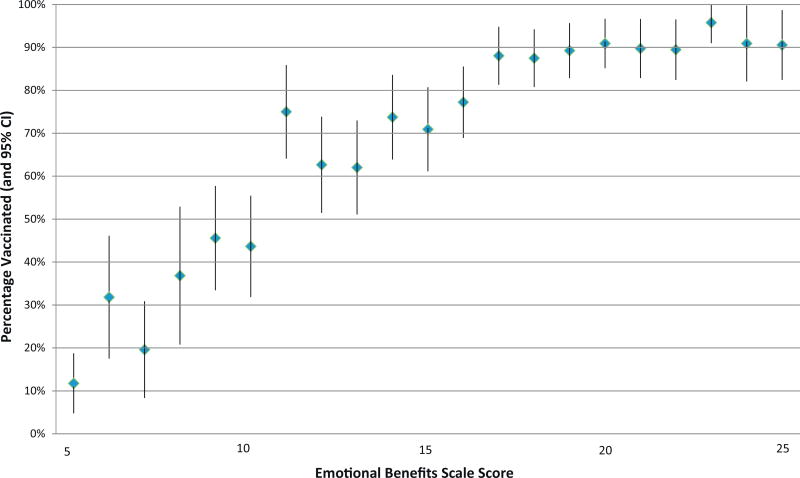
The likelihood of vaccination among HCP who felt at risk without vaccination, expected they would regret or be mad at themselves if they did not get vaccinated, or said they “worry less about getting the flu” if vaccinated were 4.3–7.4 times higher than HCP who did not expect these emotional benefits (Table 2). The most commonly endorsed attitude was the feeling that they would “worry less” if vaccinated; 26% of unvaccinated HCP agreed with this attitude compared to 72% of vaccinated HCP. As illustrated in Fig. 1, the percentage of HCP who were vaccinated climbed steadily from 12% among HCP with the lowest emotional benefits scale score and then plateaued at >88% for scores 15–19 which corresponded to average item ratings of “neutral” to “mildly agree”. Contrasting the extreme groups, the odds of vaccination among HCP with the highest emotional benefits scores were 23.3 times higher than HCP with the lowest scores (Table 3).
Fig. 1.
Percentage of HCP with 2010–2011 seasonal influenza vaccination and 95% confidence interval (CI) by emotional benefits scale score.
3.3. HCP characteristics and vaccination
In crude univariate analyses, of the participant characteristics in Table 1, seven factors were associated with HCP vaccination (Table 3). HCP who were over age 50, white, married, physician extenders, or at the SWH site were 30–60% more likely to be vaccinated, while HCP who worked in emergency departments were 40% less likely to be vaccinated. The likelihood of 2010–2011 seasonal vaccination among HCP with consistent and inconsistent annual vaccination records during the prior 5 seasons were 23.6 and 8.3 times higher, respectively, than HCP with no previous seasonal influenza vaccinations on record. Stated with the opposite referent, HCP without prior vaccination records were 96% less likely (odds ratio = 0.04, CI = 0.03–0.06) to be vaccinated than consistent vaccinees.
3.4. Pre-season intention to be vaccinated and subsequent vaccination
Half (53.6%) of the HCP said they were “almost certain” to get vaccinated, while the other half expressed varying levels of uncertainty regarding their vaccination plans. Mean ratings of intention (on a 7-point scale) were highest for consistent vaccinees (mean = 6.2, standard deviation [SD] = 1.5) and declined significantly stepwise among inconsistent vaccinees (mean = 5.3, SD = 2.1) and HCP without prior vaccination records (mean = 2.7, SD = 2.2) (F-ratio = 322.8, p < .001). The majority of consistent (73.7%) and inconsistent vaccinees (53.6%) said they were “almost certain” to get vaccinated compared to only 14.2% of HCP with no prior vaccination record. Half (51.9%) of these previously unvaccinated HCP rated their pre-season intention as “almost zero chance” compared to only 9.6% of inconsistent and 2.1% of consistent vaccinees.
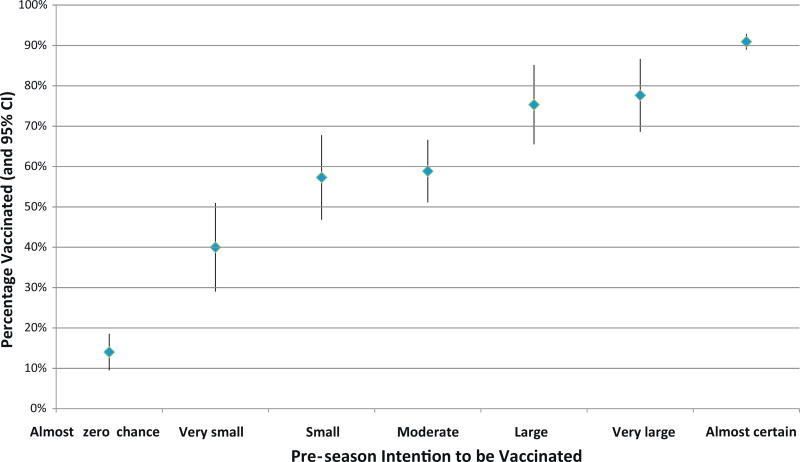
Pre-season intention was strongly associated with subsequent vaccination. The likelihood of vaccination among HCP who said they were “almost certain” to get vaccinated were 61.4 times higher than with HCP who said there was “almost zero chance” (Table 3). Nonetheless, as illustrated in Fig. 2, pre-season intention and subsequent vaccination were not equivalent; 14% of HCP whose pre-season intention was “almost zero chance” subsequently got vaccinated, while 22% of HCP with a “very large chance” subsequently failed to get vaccinated.
Fig. 2.
Percentage of HCP with 2010–2011 seasonal influenza vaccination and 95% confidence interval (CI) by pre-season intention to be vaccinated.
3.5. Associations among attitudes, pre-season intentions, and vaccination history
There were moderately strong correlations among the attitude measures (absolute value of correlation coefficients = 0.23–0.64). In a multivariate linear model with pre-season intention as the dependent variable, all attitude measures were significant independent predictors (F-ratio = 191.9, p < .001) and together explained half (R2 = 0.47) the variance in intention ratings. The emotional benefits scale had the strongest independent association with pre-season intention, with a standardized beta (Beta = 0.41, 95% CI = 0.36–0.47) twice that of the concerns about vaccine scale (Beta = −0.20, 95% CI = −0.16, −0.24), which was the second strongest predictor.
Similarly, in a multivariate linear regression with three levels of vaccination history as the dependent variable, all attitude measures were significant independent predictors of vaccination history. The strongest association was between the emotional benefits scale and vaccination history, with a standardized beta (Beta = 0.29, 95% CI = 0.20–0.31) that was twice the magnitude of the other attitude measures.
3.6. Multivariate predictors of vaccination
In the multivariate logistic regression model (Table 3) that adjusted for the correlations among predictors, the magnitude of effects were reduced for all attitudes; perceived vaccine effectiveness was no longer significantly associated with vaccination, and the associations for perceived susceptibility and concerns about vaccine were greatly diminished. However, the contrasts between all four levels of the emotional benefits scale remained significant, even after adjusting for the other attitude measures, vaccination history, and pre-season intentions. Thus, even with these adjustments, the likelihood of vaccination among HCP who recognized high emotional benefits of vaccination were 11.7 times higher than HCP who saw no benefit.
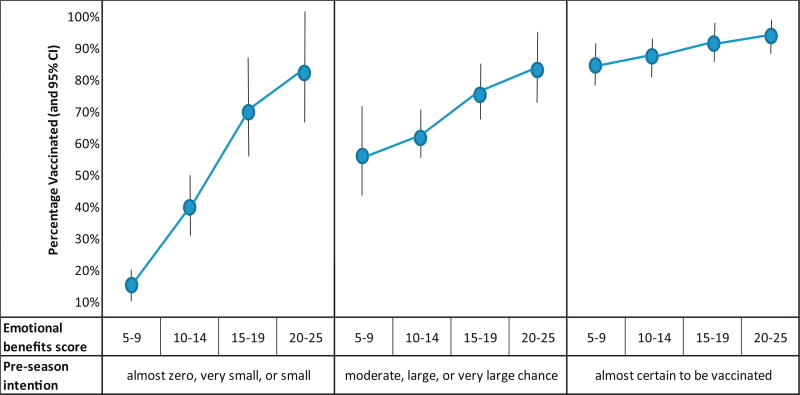
Only one significant interaction term was noted. The negative interaction of emotional benefits times pre-season intention indicates that the magnitude of the association between this attitude scale and subsequent vaccination was strongest for HCP with the lowest pre-season intention to be vaccinated. As illustrated in Fig. 3, only 15% of HCP with low pre-season intention and an emotional benefits scale score (of 5–9) that corresponded to “mildly disagree” with these items subsequently got vaccinated in contrast to 83% vaccinated among HCP with low pre-season intention but at least “mild” agreement (scores 20–25) on average with the emotional benefits items.
Fig. 3.
Percentage of HCP with 2010–2011 seasonal influenza vaccination and 95% confidence interval (CI) by four levels of emotional benefits scale scores and by three levels of pre-season intention to be vaccinated.
4. Discussion
In our prospective cohort of 1544 HCP with direct patient care at two medical systems, we found that the expected emotional benefits of influenza vaccination, including worrying less about getting influenza if vaccinated, were significant predictors of 2010–2011 seasonal influenza vaccination. The predictive value of the emotional benefit attitudes was noted even after adjusting for other attitudes, prior vaccination habits, and pre-season intention to be vaccinated. Indeed, the effect is strongest for HCP ambivalent about getting vaccinated. Among HCP who said there was little or no chance that they would get vaccinated, the difference in subsequent vaccination rates was 83% versus 15% depending on whether they recognized the emotional benefits of vaccination or not.
The emotional benefits scale was the strongest attitudinal predictor of pre-season intention and subsequent vaccination among HCP. The magnitude of the associations between the emotional benefits scale and pre-season intention and prior vaccination history were twice that noted for other attitude measures. The associations between 2010–2011 seasonal vaccination and other more commonly studied attitudes either diminished (susceptibility and vaccine concerns) or disappeared (perceived vaccine effectiveness) once emotional benefits and other factors were taken into account. These findings are similar to those from previous studies of influenza vaccination in college settings [20,21] and consistent with other research suggesting emotional expectations are a primary driver of preventive health behavior [20,21,34–37]. Although the attitudes we examined explained half the variability in preseason intentions, which in turn strongly predicted subsequent vaccination, there were gaps between HCP’s intentions and subsequent actions, and the emotional benefits attitudes continued to predict vaccination even after controlling for intentions. This is consistent with research that shows attitudes can influence behavior directly through plans and intentions or indirectly without conscious awareness [22,38].
Regardless of the role mandates may play in the future of HCP influenza vaccination policy [5–8,39], promoting confidence in and enthusiasm for influenza vaccination among HCP continues to be an important goal, especially since HCP’s personal beliefs and attitudes may influence whether they recommend vaccination to their patients [40–42]. Given the limited success of voluntary HCP vaccination campaigns to date [43–45], new intervention approaches and targets may be needed, especially for previous vaccine refusers who in our study were 96% less likely to be vaccinated than consistent vaccinees.
Our findings suggest emotional benefit attitudes may be a promising intervention target for four reasons. First, our findings suggest that part of what vaccination campaigns provide is peace of mind and reduction in worry. In our study, 72% of vaccinated HCP agreed that they “worry less about getting the flu” if vaccinated, compared to only 26% of the unvaccinated. Second, there is considerable variability in these attitudes and room for attitude change. In our two medical systems, traditional education targets, such as information on vaccine effectiveness and safety, would offer little leverage because doubts and concerns in these areas are not common, even among unvaccinated HCP. In contrast, doubts about the emotional benefits of vaccination were very common; about 8 out of 10 unvaccinated HCP did not anticipate feeling more vulnerable to influenza without vaccination or regretting their decision. Third, extensive attitude change may not be required, since even modest acceptance of these attitudes was associated with high vaccine uptake. Vaccination among HCP whose average response to the emotional benefits items was “mildly agree” was over 88%. Fourth, emotional benefit attitudes appear to be especially influential among HCP least inclined to be vaccinated and thus the most challenging targets of vaccination campaigns.
Among the strengths of this study are its focus on HCP with direct patient care, its prospective design, and the confirmation of vaccination through medical records going back 5 seasons. Most prior studies have relied on self-reported vaccination status, which is subject to consistency, social-desirability, and memory biases [16,46,47].
By combining single or dual-item indicators from previous studies into multi-item scales, this study also benefits from more reliable measures of key constructs, which may have contributed to our ability to explain more variance in outcomes than previous studies [20,21]. It is possible that the standard single item measures of perceived effectiveness and susceptibility applied in this and other studies [21,27] would also benefit from multi-item measurement to increase variance and reduce measurement error. Future studies are needed to improve the measurement of these and other attitude constructs. Although in this study, the five items focused on emotional expectations were highly interrelated and best examined as a single construct, future research is needed to generate and test multiple item options for distinct but overlapping concepts like “feeling at risk” and “anticipated regret”, which could potentially be measured separately and contribute in different ways to explaining vaccination behavior.
Our conclusions are subject to several limitations. Participants were volunteers and may not be representative of all HCP. Although our multivariate models adjusted for significant demographic and occupational covariates, differences in volunteering between sites, men and women, and other groups may have influenced the results in unknown ways. Although our focus on two medical systems in three states and enrollment of sizeable proportions of HCP at both sites is broader than the typical single setting study, we are unsure how these sites generalize to other settings. Both study sites had vaccine uptake (>65%) that was similar to their local estimates for all employees and close to the national average [43], but it is unclear how our findings would apply to settings with higher compliance and/or a vaccination mandate [48] or with low compliance settings, where most prior HCP attitude research has occurred [11,49]. Ideally, this study also would have assessed whether HCP value vaccination as a way to protect their patients. Rather, we focused on self-protection, which most prior studies have found to be the primary motivation for vaccination among HCP [1,3,11,29].
5. Conclusion
The expected emotional benefits of vaccination strongly affect seasonal influenza vaccination among HCP, even after taking into account other attitudes, pre-season intentions, and prior vaccination history. Expected emotional benefits are promising targets for intervention because of the large gap between vaccinated and unvaccinated HCP’s attitudes and because they appear to be especially influential among HCP least inclined to be vaccinated. Nonetheless, future research is needed to establish whether vaccination campaigns can change emotion-focused attitudes and whether these changes will result in increased vaccination.
Supplementary Material
Acknowledgments
The authors thank Samanth Beeram, Meredith Vandermeer, Lydia Clipper, Jennifer Gerber, Eresha Bluth, Jennifer Carlston, Ashley Kossie, and Jacqueline Flores for their assistance in project and data management. They also appreciate the contributions of their research assistants. They thank Jerry Tokars, Joseph Bresee, and Carolyn Bridges for feedback on early versions of this manuscript. Finally, they also thank the healthcare professionals at both study sites for participating in this study.
Funding
Funding for this study was supported by the Centers for Disease Control and Prevention (contract 200-2010-F-33396 to Abt Associates, Inc.). The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention, Abt Associates, Inc., Kaiser Permanente Center for Health Research, or Scott & White Healthcare.
Footnotes
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.vaccine.2012.03.062.
References
- 1.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine. 2009;27(30):3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 2.Pearson ML, Bridges CB, Harper SA. Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55(RR-2):1–16. [PubMed] [Google Scholar]
- 3.Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34(3):142–7. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 4.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1–62. [PubMed] [Google Scholar]
- 5.Poland GA, Tosh P, Jacobson RM. Requiring influenza vaccination for health care workers: seven truths we must accept. Vaccine. 2005;23(17–18):2251–5. doi: 10.1016/j.vaccine.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 6.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis. 2010;50(4):459–64. doi: 10.1086/650752. [DOI] [PubMed] [Google Scholar]
- 7.Rakita RM, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol. 2010;31(9):881–8. doi: 10.1086/656210. [DOI] [PubMed] [Google Scholar]
- 8.Poland GA. Mandating influenza vaccination for health care workers: putting patients and professional ethics over personal preference. Vaccine. 2010;28(36):5757–9. doi: 10.1016/j.vaccine.2010.07.057. [DOI] [PubMed] [Google Scholar]
- 9.Wynia MK. Mandating vaccination: what counts as a mandate in public health and when should they be used? Am J Bioeth. 2007;7(12):2–6. doi: 10.1080/15265160701795809. [DOI] [PubMed] [Google Scholar]
- 10.Lugo NR. Will carrots or sticks raise influenza immunization rates of health care personnel? Am J Infect Control. 2007;35(1):1–6. doi: 10.1016/j.ajic.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Takayanagi IJ, Cardoso MR, Costa SF, Araya ME, Machado CM. Attitudes of health care workers to influenza vaccination: why are they not vaccinated? Am J Infect Control. 2007;35(1):56–61. doi: 10.1016/j.ajic.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Virseda S, Restrepo MA, Arranz E, Magan-Tapia P, Fernandez-Ruiz M, de la Camara AG, et al. Seasonal and pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish University Hospital. Vaccine. 2010;28(30):4751–7. doi: 10.1016/j.vaccine.2010.04.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poland GA. The 2009–2010 influenza pandemic: effects on pandemic and seasonal vaccine uptake and lessons learned for seasonal vaccination campaigns. Vaccine. 2010;28(Suppl. 4):D3–13. doi: 10.1016/j.vaccine.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Burls A, Jordan R, Barton P, Olowokure B, Wake B, Albon E, et al. Vaccinating healthcare workers against influenza to protect the vulnerable—is it a good use of healthcare resources? A systematic review of the evidence and an economic evaluation. Vaccine. 2006;24(19):4212–21. doi: 10.1016/j.vaccine.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 15.Bernstein HH, Starke JR. Policy statement—recommendation for mandatory influenza immunization of all health care personnel. Pediatrics. 2010;126(4):809–15. doi: 10.1542/peds.2010-2376. [DOI] [PubMed] [Google Scholar]
- 16.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–45. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 17.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–93. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 18.Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2010;(3):CD005470. doi: 10.1002/14651858.CD005470.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poland GA. Pandemic 2009–2010 influenza vaccine: six lessons learned and the way forward (Allegro not Adagio) Vaccine. 2011;29(4):613–4. doi: 10.1016/j.vaccine.2010.11.086. [DOI] [PubMed] [Google Scholar]
- 20.Chapman GB, Coups EJ. Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 2006;25(1):82–90. doi: 10.1037/0278-6133.25.1.82. [DOI] [PubMed] [Google Scholar]
- 21.Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. 2007;26(2):146–51. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- 22.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–68. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 23.Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, et al. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009;339:b3391. doi: 10.1136/bmj.b3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thoon KC, Chong CY. Survey of healthcare workers’ attitudes: beliefs and willingness to receive the 2009 pandemic influenza A (H1N1) vaccine and the impact of educational campaigns. Ann Acad Med Singapore. 2010;39(4):307–16. [PubMed] [Google Scholar]
- 25.Pareek M, Clark T, Dillon H, Kumar R, Stephenson I. Willingness of healthcare workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine. 2009;27(8):1242–7. doi: 10.1016/j.vaccine.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 26.Melia M, O’Neill S, Calderon S, Hewitt S, Orlando K, Bithell-Taylor K, et al. Development of a flexible: computerized database to prioritize, record, and report influenza vaccination rates for healthcare personnel. Infect Control Hosp Epidemiol. 2009;30(4):361–9. doi: 10.1086/596043. [DOI] [PubMed] [Google Scholar]
- 27.Diefenbach MA, Weinstein ND, O’Reilly J. Scales for assessing perceptions of health hazard susceptibility. Health Educ Res. 1993;8(2):181–92. doi: 10.1093/her/8.2.181. [DOI] [PubMed] [Google Scholar]
- 28.Liao Q, Cowling BJ, Lam WW, Fielding R. Factors affecting intention to receive and self-reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: a longitudinal study. PLoS One. 2011;6(3):e17713. doi: 10.1371/journal.pone.0017713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark SJ, Cowan AE, Wortley PM. Influenza vaccination attitudes and practices among US registered nurses. Am J Infect Control. 2009;37(7):551–6. doi: 10.1016/j.ajic.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20(1):21–5. doi: 10.1016/s0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 31.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125–37. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Routledge: Academic; 2002. [Google Scholar]
- 33.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 34.Wroe AL, Turner N, Salkovskis PM. Understanding and predicting parental decisions about early childhood immunizations. Health Psychol. 2004;23(1):33–41. doi: 10.1037/0278-6133.23.1.33. [DOI] [PubMed] [Google Scholar]
- 35.Diefenbach MA, Miller SM, Daly MB. Specific worry about breast cancer predicts mammography use in women at risk for breast and ovarian cancer. Health Psychol. 1999;18(5):532–6. doi: 10.1037//0278-6133.18.5.532. [DOI] [PubMed] [Google Scholar]
- 36.Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychol Bull. 2001;127(2):267–86. doi: 10.1037/0033-2909.127.2.267. [DOI] [PubMed] [Google Scholar]
- 37.Connolly T, Reb J. Regret in cancer-related decisions. Health Psychol. 2005;24(4 Suppl):S29–34. doi: 10.1037/0278-6133.24.4.S29. [DOI] [PubMed] [Google Scholar]
- 38.Baumeister RF, Masicampo EJ, Vohs KD. Do conscious thoughts cause behavior? Annu Rev Psychol. 2011;62:331–61. doi: 10.1146/annurev.psych.093008.131126. [DOI] [PubMed] [Google Scholar]
- 39.Rakita RM, Hagar BA, Lammert JK. Vaccination mandates vs opt-out programs and rates of influenza immunization. JAMA. 2010;304(16):1786. doi: 10.1001/jama.2010.1478. [author reply 1786] [DOI] [PubMed] [Google Scholar]
- 40.Schwarzinger M, Verger P, Guerville MA, Aubry C, Rolland S, Obadia Y, et al. Positive attitudes of French general practitioners towards A/H1N1 influenza-pandemic vaccination: a missed opportunity to increase vaccination uptakes in the general public? Vaccine. 2010;28(15):2743–8. doi: 10.1016/j.vaccine.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 41.Frank E, Rothenberg R, Lewis C, Belodoff BF. Correlates of physicians’ prevention-related practices. Findings from the Women Physicians’ Health Study. Arch Fam Med. 2000;9(4):359–67. doi: 10.1001/archfami.9.4.359. [DOI] [PubMed] [Google Scholar]
- 42.Nichol KL, Zimmerman R. Generalist and subspecialist physicians’ knowledge, attitudes, and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients: a nationwide survey. Arch Intern Med. 2001;161(22):2702–8. doi: 10.1001/archinte.161.22.2702. [DOI] [PubMed] [Google Scholar]
- 43.Harris K, Uscher-Piners L, Black CL, Euler GL, Singleton JA, Lindley MC. Influenza vaccination coverage among health-care personnel—United States, 2010–11 influenza season. MMWRMorb Mortal Wkly Rep. 2011;60:1073–7. mm6032a1 [pii] [PubMed] [Google Scholar]
- 44.Caban-Martinez AJ, Lee DJ, Davila EP, LeBlanc WG, Arheart KL, McCollister KE, et al. Sustained low influenza vaccination rates in US healthcare workers. Prev Med. 2010;50(4):210–2. doi: 10.1016/j.ypmed.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohrt CK, McKinney WP. Achieving compliance with influenza immunization of medical house staff and students. A randomized controlled trial. JAMA. 1992;267(10):1377–80. [PubMed] [Google Scholar]
- 46.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 47.Barsky AJ. Forgetting, fabricating, and telescoping: the instability of the medical history. Arch Intern Med. 2002;162(9):981–4. doi: 10.1001/archinte.162.9.981. [DOI] [PubMed] [Google Scholar]
- 48.Hakim H, Gaur AH, McCullers JA. Motivating factors for high rates of influenza vaccination among healthcare workers. Vaccine. 2011;29(35):5963–9. doi: 10.1016/j.vaccine.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 49.Bautista D, Vila B, Uso R, Tellez M, Zanon V. Predisposing: reinforcing, and enabling factors influencing influenza vaccination acceptance among healthcare workers. Infect Control Hosp Epidemiol. 2006;27(1):73–7. doi: 10.1086/499148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.