Abstract
Objective
In order to improve success rates in psychotherapy, an alliance-focused training (AFT) protocol was developed and evaluated with regard to patient-therapist interpersonal behavior in a 30-session protocol of cognitive-behavioral therapy for outpatients comorbid with Axis I and II conditions conducted in a medical center setting.
Method
Participants included 40 patients treated by 40 therapists in a multiple baseline design in which novice therapists trained to fidelity standards in CBT were introduced to AFT at different time intervals (after either 8 or 16 sessions) during a 30-session CBT protocol. Interpersonal behaviors were assessed with a simplified version of the Structural Analysis of Social Behavior (SASB) on videotaped sessions sampled from the early (between sessions 6–8), mid (14–16), and late (22–24) phases of therapy.
Results
As predicted, several significant interactions were observed between within-subject interpersonal change and between-group differences in exposure to AFT. Specifically, there were decreases in patient dependence and in therapist control (including criticism), plus increases in patient expressiveness and in therapist affirmation and expressiveness, all of which could be attributed to AFT. The predictive relationship of several of these variables to session-level and overall treatment outcome was also demonstrated.
Conclusions
This study demonstrates that novice CBT therapists can be trained to improve their interpersonal process with patients who present with comorbid diagnoses, including a personality disorder.
Public health significance
Demonstrating the efficacy of a protocol designed to develop novice therapists’ alliance-focused abilities has important implications for professional training, as well as for outcome in psychotherapy.
Keywords: therapeutic alliance, psychotherapy outcome, therapist training
Meta-analyses have demonstrated that the therapeutic alliance is a robust predictor of outcome across a range of treatments (see Horvath, Del Re, Flückiger, & Symonds, 2011; Martin, Garske, & Davis, 2000). Generally defined as purposeful collaboration and affective bond between patient and therapist (Bordin, 1979; Hatcher & Barends, 2006), the alliance has received a great deal of attention over the years as a common factor and integrative variable in understanding the change process (e.g., Wampold & Imel, 2015; Wolfe & Goldfried, 1988). The extensive research on its predictive validity set the stage for a “second generation” of alliance research focused on alliance ruptures, which have been defined as breakdowns in collaboration and deteriorations in the bond manifested by negative process or problematic interactions between patient and therapist (Safran & Muran, 2006). In a recent review (Muran, in press), five studies (N=228) found that patients reported ruptures in 19–42% of sessions, therapists reported ruptures in 43–56% of sessions, and observers reported ruptures in 26–100% of sessions; another nine studies (N=1230) found patients reported ruptures in 25–68% of cases. In sum, these studies included both cognitive-behavioral and psychodynamic treatments and not only demonstrated the prevalence of rupture, but many of them also demonstrated predictive validity (8/14): medium, statistically significant, negative relationships of ruptures to treatment retention or outcome.
While problems in the alliance are common, research suggests that recognizing and resolving ruptures in the therapeutic alliance can be quite daunting for therapists (see Hill, 2010 for a review). The importance of therapists’ abilities to resolve or repair alliance ruptures is underscored by evidence that resolution of alliance ruptures is associated with better retention in treatment (Muran et al., 2009). Furthermore, alliance rupture resolution has been found to predict outcome in a meta-analysis of 11 studies (N=1318: Eubanks, Muran & Safran, in press): The majority of these included cognitive-behavioral therapies. In their recent qualitative review of the treatment failure literature, Roos and Werbart (2013) concluded that “therapists need enhanced skills in building and repairing” the therapeutic alliance in order to reduce the incidence of poor outcome in therapy (p. 394). Based on their naturalistic program of research to redress treatment nonresponse and deterioration, Lambert and colleagues (2010; Shimokawa, Lambert & Smart, 2010) have similarly recognized the importance of developing alliance-focused skills.
Several studies have evaluated the effectiveness of treatment interventions and training procedures designed to improve therapists’ abilities to maintain an alliance and to work constructively with weakened alliances and negative interpersonal process with their patients (Eubanks-Carter, Muran, & Safran, 2010). A meta-analysis of six studies (N=373) found a small, nonsignificant significant effect for training conditions compared to control conditions (Eubanks et al., in press). One reason for this small effect is the failure of these between-group studies to adequately control for both patient and therapist variables (i.e., for the variability in the challenging nature of the patients and in the effective abilities of the therapists) –and maybe more importantly to take into account the patient-therapist interaction variable (i.e., factors unique to the specific dyad). Another way of framing this latter issue is in terms of the notion of therapeutic responsiveness (Stiles, Honos-Webb, & Surko, 1998), according to which therapists and patients are always influencing and responding to one another on an ongoing basis. Thus, every therapeutic dyad is unique, and the style of mutual responsiveness varies across time.
In this article, we present findings from a study funded by the National Institute of Mental Health (NIMH) and designed to investigate the effectiveness of a training protocol to enhance therapists’ abilities to recognize and resolve alliance ruptures. This training protocol, which we refer to as Alliance-Focused Training (AFT: Eubanks-Carter, Muran, & Safran, 2015; Muran, Safran & Eubanks-Carter, 2010; Safran et al., 2008), is based on an intervention model that integrates principles from recent research on emotion and communication and contemporary perspectives on interpersonal practice, which has been described elsewhere (e.g., Muran et al, 2005; Safran & Muran, 2000; Safran et al, 2005). The training protocol and intervention model were founded in large part on previous research on the rupture resolution process (see Muran, 2002; Safran & Muran, 1996; Safran, Muran & Samstag, 1994), specifically on a task analytic study that involved an intensive analysis of 16 matched sessions (identified by patient report as resolution or nonresolution) from eight cases of a time-limited cognitive therapy protocol that integrated interpersonal principles (Safran & Segal, 1990).
The task analysis yielded a stage-process model that described the process of rupture resolution as follows: The patient and therapist first acknowledge the rupture event, and then they collaborate to explore the rupture by progressing through greater expressiveness by the patient (e.g., patient expresses negative feelings about the therapy or therapist), as well as affirmation and expressiveness by the therapist (e.g., therapist facilitates and validates the patient’s assertiveness or vulnerable expression). The critical technical principal is metacommunication (Kiesler, 1996), which involves establishing a collaborative exploration of the communication process as it unfolds (see Safran & Muran, 2000). The task analysis included the use of the Structural Analysis of Social Behavior (SASB: Benjamin, 1974) to define and demonstrate the progression away from the rupture (operationalized with the SASB as patient behaviors of appeasing, avoiding and blaming) and toward a more expressive position and resolution (operationalized as patient expressing and therapist affirming, as well as therapist expressing). The analysis also included the Experiencing Scales (EXP: Klein, Mathieu-Coughlan, & Kiesler, 1986), which underscored this movement towards greater patient expressiveness and therapist affirmation in the form of greater emotional involvement.
The SASB has been recognized as a useful tool to operationally define patient and therapist behaviors in the therapeutic alliance (Benjamin & Critchfield, 2010; Goldfried & Wolfe, 1996; Henry & Strupp, 1994). We defined patient appeasing, avoiding, and blaming behaviors (as well as therapist control and blaming behaviors) as markers of rupture or negative process, and patient expressing and therapist affirming as markers of rupture resolution or positive process, which is consistent with several studies that have used the SASB to link these behaviors to alliance (e.g., Coady & Marziali, 1994) or to outcome (e.g., Coady, 1991; Critchfield, et al., 2007; Henry, Schacht, & Strupp, 1986, 1990; Jorgensen, Hougaard, Rosenbaum, Valbak, & Rehfeld, 2000). We also defined therapist expressing as facilitative of patient expressiveness (see Safran & Muran, 2000). The stage-process model demonstrating the relationship among these patient and therapist interpersonal behaviors in rupture resolution was confirmed by sequential analyses (Safran & Muran, 1996).
Our principal aim in this study was to assess the additive effect of AFT on a cognitive-behavioral therapy (CBT) for personality disorders. We selected CBT as the baseline treatment condition because of its widespread application, well-documented success and failure rates, and its relatively more limited focus on the therapeutic alliance, as indicated in several studies (e.g., Castonguay, Hayes, Goldfried, & DeRubeis, 1995; Goldfried, Castonguay, Hayes, Drozd, & Shapiro, 1997; Goldfried, Raue, & Castonguay, 1998). Because patients with personality disorders are widely recognized as having difficulties in interpersonal functioning (e.g., Benjamin & Karpiak, 2001; Clarkin & Levy, 2004), we established a personality disorder as the principal inclusion criterion in order to increase the likelihood that alliance ruptures would arise in the course of treatment. (We focused on Cluster C personality disorders rather than Cluster A or B due to a concern that patients meeting criteria for Cluster A or B diagnoses would likely need a longer term therapy approach.) We selected novice therapists because of the evidence indicating that novices are more receptive to training (e.g., Henry, Schacht, Strupp, Butler, and Binder, 1993; Weissman, Rounsaville, and Chevron, 1982) and the potential public health significance of demonstrating the impact of early training on professional development.
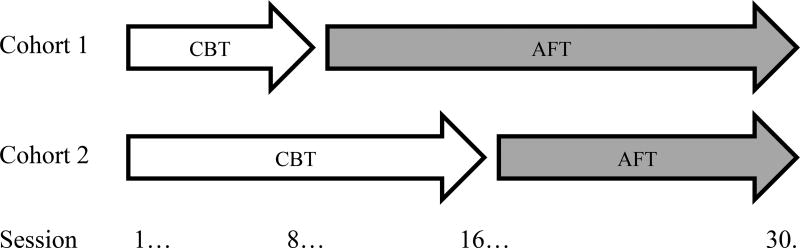
There is evidence that therapists vary in their abilities to build and maintain strong alliances: Therapist individual differences strongly predict alliance quality and treatment success (see Wampold & Imel, 2015). In order to control for therapist individual differences and to evaluate whether changes taking place after the implementation of AFT were attributable to AFT (and not to other factors such as an improvement in therapist skill due to increased experience or greater familiarity with a specific patient), we implemented a multiple baseline design (see Kazdin, 1992). By this design, we controlled for variance attributable to patient, therapist, and patient-therapist interactional sources, and we assessed for the emergence of predicted differences in interpersonal process in each dyad consequent to the introduction of AFT at different time intervals in the protocol. This study consisted of two phases: In the initial phase, therapists received one year of CBT training, consisting of attending a 16-week didactic seminar and then conducting a 30-session CBT protocol with weekly supervision. Therapists were required to demonstrate fidelity to the CBT protocol in order to enter the second phase of the study: the multiple baseline phase. In this phase, the therapists began conducting a second case in CBT, while continuing to attend CBT supervision. After either 8 or 16 sessions of CBT (determined by random assignment), the therapists were transferred from CBT supervision to AFT, where they learned how to augment CBT with AFT principles while continuing to work with the same patient (see Figure 1).
Figure 1.
Multiple baseline design of training conditions
Note. CBT=Cognitive-Behavioral Therapy; AFT=Alliance-Focused Therapy
Consistent with our stage-process model of the rupture resolution as described above, our principal hypotheses concerned changes in interpersonal processes as measured by the SASB. Specifically, we predicted AFT would facilitate the following changes: (1) decreases in patient behaviors of avoidance, appeasement, blaming, and following, and (2) an increase in patient expressiveness. We also predicted AFT would facilitate (3) decreases in therapist behaviors of blaming and directing and (4) increases in therapist affirmation and expressiveness. Because all therapists received significant exposure to AFT, we did not expect to find significant differences between the training conditions in treatment outcome. However, in order to assess whether the changes in behavior were related to outcome, we also examined the relationship between early interpersonal process (before the introduction of AFT) and outcome at the session level (session impact), as well as overall outcome.
Method
Training Conditions
Cognitive-Behavioral Therapy (CBT: Turner, Muran, & Ochoa, 1992/2004)
The cognitive-behavioral therapy condition was designed to treat patients presenting with Cluster C personality disorders and with personality disorders “not otherwise specified” according to DSM-IV (American Psychiatric Association, 1994) in a 30-session, in one 45-minute session/week protocol. It was largely based on Beck and colleagues’ (1990) adaptation of cognitive therapy and incorporates Persons’ (1989) case formulation approach. The CBT protocol began with establishing a case formulation, which included creating a problem list and clarifying core belief systems, and then involved two phases: (1) Symptom relief or reduction, which is focused on the Axis I condition, and (2) Schema change, which is focused on the Axis II condition. Both phases involved the application of various cognitive and behavioral strategies, including in-session tasks (e.g., applied relaxation, role-playing, exposure exercises, cognitive decentering and restructuring) and extra-session tasks in the form of homework assignments (e.g., thought records, scheduling activities, exposure exercises, and behavioral experiments). Training began with a 16-week (75-minutes per week) didactic seminar on CBT focused on developing therapist basic skills with regard to session structure and treatment protocol. On case assignment, training continued with weekly 75-minute group supervision (≤ 6 trainees per group) that concentrated on case-specific formulation, treatment planning, and role-playing, as well as feedback on videotapes of therapists’ work. All psychotherapy sessions were videotaped.
The CBT condition focused on the therapeutic relationship in a fashion consistent with standard approaches to CBT (see Beck, 1995; Persons, 1989). The therapist’s task was to establish a supportive relationship as a necessary condition for the technical work to take place. Dealing directly with problems in the therapeutic relationship and eliciting feedback at the end of each session regarding problems in communication was standard practice. In addition, negative patient reactions that became apparent during a session were treated either (a) as misunderstandings that could be corrected by clarifying a communication or by explaining the cognitive-behavioral rationale, or (b) as opportunities to identify and challenge patient cognitive distortions, as well as maladaptive schemas. There was also an attempt to anticipate problems in the therapeutic relationship by using the case formulation model. Finally, problems that could be attributed to negative therapist reactions, such as anxiety or anger, were considered impediments to the therapeutic process, and therapists were directed to assess and correct their own thoughts or attitudes that might be contributing to a rupture (Newman, 2013).
Alliance-Focused Training (AFT: Eubanks-Carter, Muran & Safran, 2015a; Muran, Safran & Eubanks-Carter, 2010; Safran & Muran, 2000; Safran et al., 2008)
The principles of AFT were based on Safran and Muran’s (2000) Negotiating the Therapeutic Alliance: A Relational Treatment Guide, which served as the training manual. Some key principles were: (a) Alliance ruptures are seen as the result of patients and therapists unwittingly co-participating in a negative process; (b) there is an intensive focus on the here-and-now of the therapeutic relationship; and (c) there is an ongoing collaborative exploration of both patients’ and therapists’ contributions to the interaction (that is, metacommunication). Training was conducted in a weekly 75-minute group supervision (≤ 6 trainees per group), consisting of a didactic component, regarding the definition of rupture events and resolution strategies, and an experiential component, involving awareness exercises as opportunities for deliberate practice (Ericsson et al., 1993).
AFT emphasized experiential learning and self-exploration. Therapists were trained to attend to and explore their own feelings as important sources of information about what is going on in the therapeutic relationship. Like CBT training, AFT made use of role-playing. In AFT, however, these exercises, referred to as “awareness exercises,” provided therapists with the opportunity to simulate working with difficult process and experimenting with metacommunication: an important difference being that the purpose of these exercises was not just to provide therapists with the opportunity to practice technical skills, but also to develop the skill of exploring their own feelings as they emerge during alliance ruptures. In addition, supervision sessions employed mindfulness training for purposes of helping therapists refine their capacity to observe their own internal experience, as well as the nature of their own contributions to interpersonal process. An important byproduct of mindfulness and metacommunication practice is the development of emotion regulation abilities (Gross, 2015), which enable therapists to make therapeutic use of their negative affect associated with a rupture.
Enhancing CBT with AFT
Once therapists transitioned from CBT supervision to AFT, they were instructed to begin incorporating principles of AFT into their work with their patients in a fashion that felt appropriate for their particular case. The precise pace and extent to which they used specific AFT interventions (e.g., in-depth exploration of therapists’ own contributions to ruptures and patients’ emerging feelings in the context of the therapeutic relationship) was worked out collaboratively in supervision. In some cases, where it became apparent that there were well-defined ruptures in the alliance, therapists were encouraged to begin collaboratively exploring these ruptures with their patients soon after transitioning to AFT. If the use of CBT interventions appeared to be problematic, therapists were encouraged to forgo these interventions in order to focus more intensively on metacommunication. In other cases, where ruptures were more subtle or not apparent, therapists were encouraged to continue using CBT interventions while simply paying closer attention to their own experience and subtle patterns possibly playing out in the therapeutic relationship.
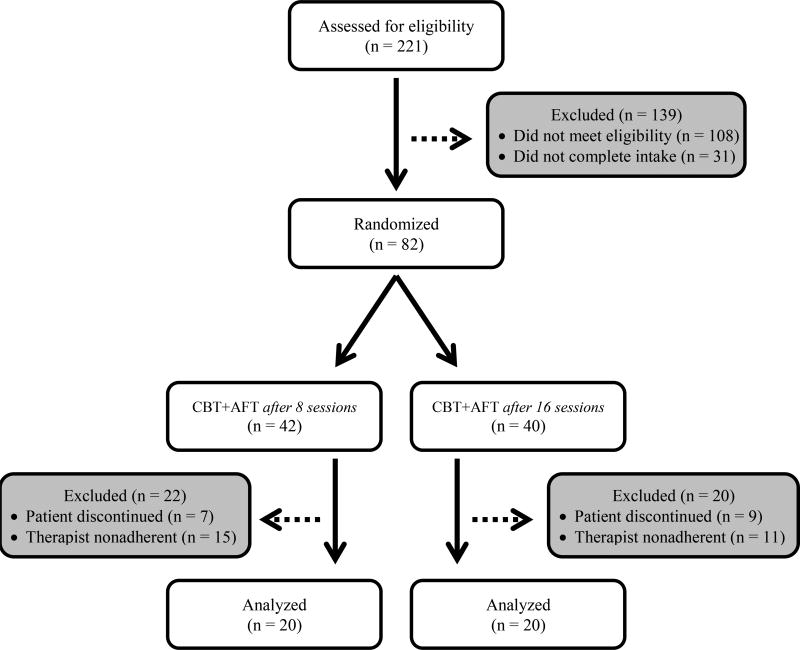
Participants
For this study, 221 adults were assessed for eligibility, and 82 were admitted (based on inclusion/exclusion criteria described below) and randomly assigned to one of the two training conditions (following our multiple baseline design): Forty psychotherapy cases were submitted to analyses, based on patient completion and therapist adherence to protocol (see CONSORT diagram in Figure 2). A subset of these cases (n = 20) were previously presented as part of a preliminary analysis that also explored the impact of AFT on other variables (Safran et al., 2014): This previous study demonstrated main effects for training condition, but did not have sufficient power to test for interaction effects that would adequately assess the impact of AFT.
Figure 2.
CONSORT diagram
Note. CBT=Cognitive-Behavioral Therapy; AFT=Alliance-Focused Therapy
Patients
Patients included 22 women and 18 men (N = 40) admitted to the research program, ranging in age from 23 to 69 (M = 41.93, SD = 13.07): 72.5% single, never married, 15% married or remarried, and 12.5% divorced or separated; 20% high school graduates, 55% college graduates, and 25% post-baccalaureate graduates; 82.5% were employed; 80% White, 7.5% Black, 5% Asian, 5% other, and 7.5% Hispanic. The patients presented with difficulties related to depression, anxiety, and interpersonal functioning: 55% met criteria for a current primary diagnosis of Mood Disorder, 32.5% Anxiety Disorder, 12.5% V-Code on Axis I of DSM–IV (APA, 1994); and 65% met for multiple Axis I diagnoses. The principal inclusion criterion was that they met for a diagnosis of Personality Disorder (PD) Cluster C or Not Otherwise Specified (NOS) on Axis II: 47.5% met criteria for a diagnosis of PD NOS, 30% Obsessive–Compulsive PD, 22.5% Avoidant PD; and 45% met for multiple Axis II diagnoses. Ten patients (25%) stabilized on an antidepressant or anxiolytic for three months prior to intake (that is, no evidence of dosage adjustment during that time) were permitted to participate in this study: We included medicated patients to increase the generalizability of our findings; we required stabilization to control for a confounding effect of psychiatric medication on patient interpersonal behavior and thus on our dependent variable (see Kapfhammer & Hippius, 1998, for a review of the research on pharmacotherapy in personality disorders). Exclusion criteria included evidence of organicity, psychosis, mania or severe major depression, impulse control and compulsive disorder, and any active substance use disorder. We also excluded patients in another psychosocial treatment so as to not confound the results of our study on the effect of our psychosocial protocol. Patients provided informed consent with respect to the parameters of the research protocol. They also paid a nominal fee per therapy session based on an income sensitive sliding scale in order to approximate a naturalistic treatment setting.
Therapists
Therapists included 40 trainees (31 women and 9 men), ranging in age from 24 to 36 (M = 28.87, SD = 3.50), who were psychology externs (third- and fourth-year Ph.D. students) affiliated with an accredited doctoral program in clinical psychology and who committed to a two-year training protocol in the research program: 82.5% of the therapists were White, 5% Asian, and 12.5% Hispanic; 45% were single, never married, 40% married or remarried, and 15% divorced or separated. All completed two cases in the program: one with exclusively CBT supervision and another in which they were introduced to AFT after 8 sessions (n = 20) or 16 sessions (n = 20) of CBT supervision. All therapists provided informed consent with respect to the research parameters, including videotaping of their psychotherapy sessions.
Supervisors
Supervision in CBT was provided by a psychologist who was a Fellow of the Academy of Cognitive Therapy and had an extensive background as a CBT therapist, including a postdoctoral fellowship at the Center for Cognitive Therapy, University of Pennsylvania, and over 10 years of postdoctoral clinical experience at the start of the study. Another CBT expert, a Founding Fellow of the Academy of Cognitive Therapy, also with extensive CBT background and experience (over 15 postdoctoral years), including postdoctoral training also at the Center for Cognitive Therapy, University of Pennsylvania, served as a consultant on the study and provided input on the CBT training protocol. Supervision in AFT was led by the first two authors, who developed the training protocol, presented and published extensively on its development and related research, and had 15–25 years respectively of postdoctoral experience at the start of the study. Two junior faculty with at least one-year of AFT served as co-leaders, including the third author.
Interviewers/raters
Twenty MA-level graduate students from various clinical psychology programs in a metropolitan area served as research assistants and underwent training to conduct semi-structured diagnostic interviews and treatment fidelity assessments, as well as to rate on a measure of interpersonal process (see assessment descriptions, training protocols and rater reliability data below).
Assessment Measures & Procedure
Diagnostic Status
Patients underwent an intake process conducted by research assistants trained to reliable standards that included the administration of the Structured Interview for DSM-IV-Axis I & II (SCID I & II: First, Gibbon, Spitzer, & Benjamin, 1997; First, Spitzer, Gibbon, & Williams, 1997). The SCID is a semi-structured interview used to determine diagnoses on Axis I and Axis II of DSM-IV (APA, 1994). (See Muran et al., 2005, for training and reliability protocol.)
Therapist Fidelity
Beth Israel Fidelity Scale (BIFS: see Patton, Muran, Safran, Wachtel & Winston, 1998, for psychometric development) is a 44-item scale comprised of four subscales: (1) 12 items were developed to assess interventions associated with AFT, (2) 12 items to assess CBT interventions, (3) 12 items to assess short-term dynamic interventions (DYN), and (4) eight items to assess common or nonspecific factors. Each item is rated on a six-point Likert-type format for frequency. (See Muran et al., 2005 for training and reliability protocol.) In the first year of training in this study, one session from each third of each treatment protocol was randomly sampled and rated for fidelity, the results of which were given to the CBT supervisor. The minimally acceptable standard for treatment fidelity was defined as follows: Only the mean score on the CBT subscale should be ≥ 2, among the specific intervention subscales. This was a standard derived from previous research (Muran et al., 2005). In the case of unacceptable fidelity, after feedback was provided to the CBT supervisor, another session among the subsequent three was randomly sampled and rated. We required that therapists demonstrate fidelity to CBT in order to be included in the multiple baseline analysis, and we used an early session (between sessions 4–8) in their second case as a fidelity test in the present study. All 40 therapists included in the present study met the standard of ≥ 2 on the CBT subscale. Mean subscale scores on the BIFS for these therapists were: CBT = 2.70 (SD = .55), AFT = 1.62 (SD = .31), DYN = 1.39 (SD = .27); a within-subject analysis with three levels yielded an effect size (eta2) = .76 (DF = 2), p < .001, with Sidak pairwise comparison indicating significant differences between CBT and AFT (p < .001), and between CBT and DYN (p < .001).
Session Impact
Session impact was assessed on the depth (or value) subscale of the Session Evaluation Questionnaire (SEQ: Stiles, 1980). The SEQ is scaled on a seven-point semantic differential with the depth subscale consisting of the following six adjective anchors: powerful/weak, valuable/worthless, deep/shallow, full/empty, bad/good, and special/ordinary. The SEQ was completed by patients after every session. It was developed to measure session-level outcome and shown to have adequate psychometric properties, including internal consistency and predictive validity (e.g., Muran et al., 2009; Stiles, Shapiro, & Firth-Cozens, 1990). In this study, slope coefficients were calculated on the repeated measurement of the SEQ depth subscale. Through the use of lmer procedure in the R (Team R.C., 2017) multilevel analysis package, Linear Mixed-Effects Models: lme4 (Bates, 2005; Bates, Maechler, Bolker, & Walker, 2015), a simple multilevel change model with both fixed and random effects was constructed: The fixed effects part of the model predicted SEQ from sessions, and the random effects model assessed slopes for each case. The slope coefficients were used to provide further support for the relationship of interpersonal process to treatment outcome.
Treatment Outcome
Treatment outcome of the 30-session protocol was assessed on multiple dimensions, including measures of symptomatology, level of adaptive functioning, and interpersonal behavior, which is consistent with recommendations regarding the assessment of change in personality disorders (Shea, 1997). Patients completed a battery of questionnaires before beginning therapy and after the 30th session; therapists completed a battery after the 3rd session and then again after the 30th. The measures have been widely used with adequate psychometric properties demonstrated. They included: the Symptom Checklist-90-Revised (Derogatis, 1983), a 90-item self-report inventory developed to assess general psychiatric symptomatology, from which an overall mean score (Global Symptom Index) was used in this study; Global Assessment Scale (Endicott, Spitzer, Fleiss, & Cohen, 1976), a clinician-rated scale for evaluating overall mental health, which consists of a single rating on a continuum ranging from 1 (sickest) to 100 (healthiest): All therapists were trained following the authors’ protocol to reliable standards (i.e., intraclass correlation ≥ .90); Target Complaints (Battle et al., 1966), an idiographic self-report instrument developed to assess the presenting problems of the patients: Both patients and therapists independently rate the severity of the problems, from which an average was calculated by reporter for this study; Inventory of Interpersonal Problems-32 (Soldz, Budman, Demby & Merry, 1995), a 32-item self-report inventory developed to assess patient social adjustment and interpersonal difficulties: In this study, it was completed by patients and therapist, and the overall mean score was calculated by reporter. (See Supplemental Materials online for table presenting descriptive data and univariate repeated measures analyses of these measures at intake and termination.) Results from a multivariate repeated measures analysis indicated that the treatment provided was efficacious: Effect size (eta2)= .81 (DF = 6, 33), p < 001. For this study, a composite measure of outcome was also calculated by performing a principal components analysis on residualized gain scores1 of the measures mentioned above: A single component, with an eigenvalue of 3.35 (accounting for 56% of the variance among the outcome scores) and with a Cronbach’s alpha of .83, was obtained, and the standardized component scores were used as the composite outcome measure. This composite was used in this study to examine the predictive relationship of interpersonal process to treatment outcome.
Interpersonal Process
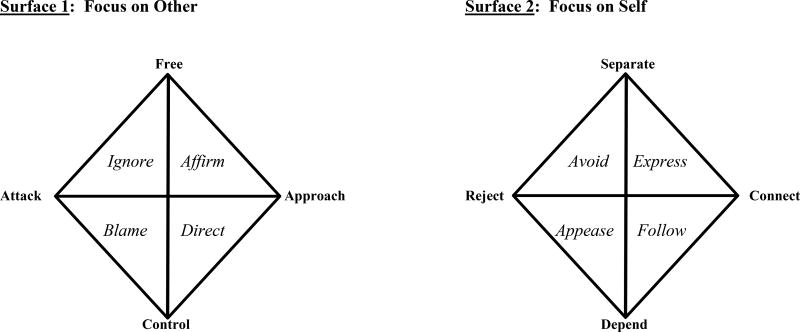
To assess the additive effect of AFT on interpersonal process in CBT, we applied a simplified version of the Structural Analysis of Social Behavior (SASB: Benjamin, 1974, 1996), an observer-based measure that defines interpersonal process, based on a circumplex model, and that has been applied as a measure of the therapeutic alliance (Benjamin & Critchfield, 2010; Henry & Strupp, 1994). The SASB organizes all interpersonal behaviors on two surfaces (“Focus on Other” and “Focus on Self”) and in terms of two orthogonal dimensions: interdependence (from autonomy to involvement) and affiliation (from hostile to friendly). More specifically, on the respective surfaces, the interdependence dimensions are freeing to controlling and separating to depending, and the affiliations dimensions are attacking to approaching and rejecting to connecting (see Figure 2). The SASB has demonstrated inter-rater reliability and predictive validity (see Constantino, 2000, for a review).
For the present study, we required raters to code in terms of the octant items of Surface 1 (Focus on Other) and Surface 2 (Focus on Self). This resulted in 16 possible dimensions that raters were instructed to rate on a 5-point scale (with 1 meaning not present and 5 meaning very present). Both patients and therapists were rated on each of these 16 dimensions. For ease of coding, psychotherapy sessions were broken into 5-minute intervals, which served as the units of coding. Ratings for each of the 5-minute intervals were then averaged to provide a total of 32 SASB dimension ratings for each session coded (16 for patients and 16 for therapists). Reliability was calculated at the session level. After 15 weeks of training, reliability on therapy sessions that were not included in this study was assessed using intraclass correlation coefficients (ICCs; two-way random effects model with absolute agreement on single measures). Individuals were considered reliable after attaining ICC scores ≥ .60 for three consecutive sessions. Subsequently, pairs of raters (selected from a pool) independently coded the sessions included in this study, and their ratings were averaged. All raters were blind to the study hypotheses.
In order to limit the number of tests conducted and experiment-wise error rate, we reduced the number of SASB variables further and applied variables based on the quadrant version. Specifically, we calculated the variables Affirm, Direct, Blame, and Ignore on Surface 1 (Focus on Other), and Express, Follow, Appease, and Avoid on Surface 2 (Focus on Self) for both patient and therapist behaviors. We summed three of the octant items for each quadrant with the middle item (along the circumplex surface) weighted by 1.00 and the two adjacent items weighted by .50. Table 1 provides definitions for each of the quadrant variables derived from the language in the complete SASB model (Benjamin, 1974, 1996). To further reduce the number of tests, we made the following predictions for changes on five patient and four therapist variables that could be attributed to the impact of AFT:
Table 1.
Definitions for surface quadrants on the simplified SASB derived from the complete SASB model (Benjamin, 1974).
| Surface 1 | Surface 2 | ||
|---|---|---|---|
| Focus on Other: Actions of Self on Other | Focus on Self: Reactions of Self to Other | ||
| Affirm | Self understands Other, provides emotional support, and encourages autonomy. | Express | Self discloses and expresses innermost self to Other, straightforward about own position. |
|
| |||
| Direct | Self teaches and directs Other how to understand and behave. | Follow | Self follows, accepts and relies on the direction of Other. |
|
| |||
| Blame | Self criticizes Other to see and behave according to Self. | Appease | Self bottles up emotion and complies with Other to avoid disapproval. |
|
| |||
| Ignore | Self ignores and neglects needs & interests of Other. | Avoid | Self avoids and disconnects from Other to separate. |
Note. SASB=Social Analysis of Social Behavior
Patient interpersonal behavior:
-
1
We predicted decreases in Follow, Appease, and Avoid (Surface 2), as well as in Blame (Surface 1);
-
2
We predicted an increase in Express (Surface 2);
Therapist interpersonal behavior:
-
3
We predicted decreases in Direct and Blame (Surface 1);
-
4
We predicted increases in Affirm (Surface 1) and Express (Surface 2).
To test these predictions, three sessions were rated for each dyad. One session was selected from each of the following phases of treatment: the early phase (defined as sessions 6–8), mid-phase (defined as sessions 14–16), and late phase (defined as sessions 22–24). The session for each phase was selected within a range of three sessions to accommodate missing data (e.g., no video or sound). In cases where three sessions were available, one was randomly selected. To demonstrate the additive effect of AFT on these interpersonal behaviors in CBT, we hypothesized interactions between within-subject differences in interpersonal behavior and between-group differences in exposure to AFT, as dictated by the multiple baseline design.
Results
Preliminary Analyses
Interrater reliability: SASB variables
We calculated intraclass correlation coefficients (ICCs; two-way random effects model with absolute agreement on single measures) on ratings at the session level for patient and therapist interpersonal behaviors on the SASB. Three sessions were rated by two raters (from a pool) for 40 cases, 120 sessions altogether. Mean scores of pairs were retained if the two raters were reliable with each other (ICC ≥ .60). If a pair failed to meet this standard, a third rater was enlisted and had his/her ratings combined with the ratings of one of the original raters to meet this standard: Fifteen sessions (12.5%) required a third rater. The mean ICC scores for patient behavior by treatment phases included in this study were: early .96 (SD = .07), mid .95 (SD = .07), and late .96 (SD = .08). The mean ICC scores for therapist behavior by treatment phases were: early .94 (SD = .08), mid .95 (SD = .08), and late .94 (SD = .09). These results demonstrate excellent inter-rater reliability.
Intercorrelations: SASB variables
We tested relationships among the quadrants on the SASB at the first phase of treatment (before the introduction of AFT) to see if they were consistent with previous research and the circumplex conception. Results are presented in Table 3. Among the patient variables, we found large positive relationships between dependent patient behaviors of Follow and Appease and between hostile patient behaviors of Avoid and Blame. We also found large negative relationships between the autonomous behavior of Patient Express and the dependent patient behaviors of Follow and Appease. Among the therapist variables, we found a large positive relationship between the controlling behaviors of Therapist Direct and Blame and a negative relationship between Therapist Direct and Therapist Affirm. Finally, between patient and therapist variables, we found that both hostile and friendly controlling behaviors by the therapist were significantly correlated with both hostile and friendly dependent behaviors by the patient, with medium to large effect sizes: Both friendly Therapist Direct and hostile Therapist Blame were correlated with friendly Patient Follow and hostile Patient Appease. By contrast, less controlling behavior by the therapist was related to more autonomous behavior by the patient: The friendly autonomous behavior of Patient Express was negatively related to Therapist Direct and was positively related to the friendly autonomy-promoting behavior of Therapist Affirm. For the most part, the findings were consistent with the literature, but they also indicated that any form of control (hostile or friendly) by the therapist and any form of dependence (hostile or friendly) by the patient were correlated.
Table 3.
Patient interpersonal behavior (SASB) in treatment phase by switch in training condition
| Main Effect | Main Effect | Interaction Effect | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | Phase 2 | Phase 3 | Phase (Within-Subject) | Condition (Between-Group) | Phase × Condition | ||||||||
| Focus on Other | M (SD) | M (SD) | M (SD) | F (2, 37) | p-value | eta2 | F (1,38) | p-value | eta2 | F (2, 37) | p-value | eta2 | |
| Blame | |||||||||||||
| Switch at 08 | 2.06 (.24) | 2.00 (.02) | 2.02 (.06) | 2.009 | .149 | .098 | .006 | .938 | .000 | .231 | .795 | .012 | |
| Switch at 16 | 2.04 (.13) | 2.00 (.00) | 2.04 (.17) | ||||||||||
| Focus on Self | |||||||||||||
| Express | |||||||||||||
| Switch at 08 | 3.54 (.51) | 4.50 (.51) | 4.56 (.64) | 23.542 | .000 | .560 | 12.187 | .001 | .243 | 12.964 | .000 | .412 | |
| Switch at 16 | 3.56 (.41) | 3.62 (.48) | 4.41 (.67) | ||||||||||
| Follow | |||||||||||||
| Switch at 08 | 2.89 (.68) | 2.42 (.36) | 2.34 (.48) | 9.534 | .000 | .340 | .075 | .786 | .002 | 4.340 | .020 | .190 | |
| Switch at 16 | 2.80 (.79) | 2.84 (.94) | 2.12 (.13) | ||||||||||
| Appease | |||||||||||||
| Switch at 08 | 2.26 (.36) | 2.06 (.13) | 2.06 (.16) | 5.321 | .011 | .217 | .279 | .600 | .007 | 2.618 | .086 | .124 | |
| Switch at 16 | 2.24 (.35) | 2.18 (.24) | 2.03 (.11) | ||||||||||
| Avoid | |||||||||||||
| Switch at 08 | 2.50 (.81) | 2.24 (.24) | 2.32 (.32) | 2.690 | .081 | .127 | 4.138 | .049 | .098 | .527 | .595 | .028 | |
| Switch at 16 | 2.22 (.26) | 2.11 (.14) | 2.26 (.28) | ||||||||||
Note. SASB=Social Analysis of Social Behavior
Predictive correlations: SASB variables by session impact and treatment outcome
Table 2 also provides results regarding the relationship of patient and therapist interpersonal behaviors assessed early in treatment to session impact and treatment outcome. Specifically, we examined the predictive relationship of the SASB variables at Treatment Phase 1 in the multiple baseline design (before introduction of AFT) to two criterion measures of treatment effect: one based on session-level (i.e., slope on the SEQ depth subscale) and the other based on a composite of patient- and therapist-rated measures (i.e., residualized gain scores derived from intake and termination assessment). As an initial step, we tested for differences between training conditions on session impact and treatment outcome and did not find any statistically significant difference; consequently, our correlational analyses did not require accounting for this independent variable. From these analyses, we found a significant, medium to large relationship of Patient Express to session impact and treatment outcome. We also found significant medium negative relationships of Patient Follow to session impact and of Patient Appease and Patient Blame to treatment outcome. Finally, we found a significant medium negative relationship of Therapist Direct to session impact. In sum, patient expressiveness, as well as therapist control and patient dependence (in the negative direction), were shown to have predictive validity.
Table 2.
Correlations of SASB variables (at Phase 1), session impact (slope on SEQ-depth) and treatment outcome (composite of residualized gain factor scores)
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Patient Express | −.52*** | −.53*** | −.18 | −.20 | |||||||
| 2. Patient Follow | .60*** | −.29 | −.07 | ||||||||
| 3. Patient Appease | .10 | .13 | |||||||||
| 4. Patient Avoid | .74*** | ||||||||||
| 5. Patient Blame | |||||||||||
| 6. Therapist Affirm | .46** | −.22 | −.15 | −.10 | −.11 | −.32* | −.07 | .14 | |||
| 7. Therapist Direct | −.48** | .76*** | .55*** | −.03 | .17 | .51*** | .22 | ||||
| 8. Therapist Blame | −.17 | .35* | .44** | .28 | .27 | .24 | |||||
| 9. Therapist Express | −.08 | .10 | .22 | −.18 | −.20 | ||||||
| 10. Session Impact | .49*** | −.38* | −.15 | .02 | −.10 | .15 | −.37* | .13 | −.01 | ||
| 11. Treatment Outcome | .40** | −.26 | −.34* | −.15 | −.34* | .12 | −.19 | .11 | .22 | .38* |
p < .05,
p < .01,
p < .001
Note. Direction of change on treatment outcome (residualized gain component scores) was reversed to make interpretation more intuitive; thus increase on this index is better. SASB=Social Analysis of Social Behavior.
Principal Analyses
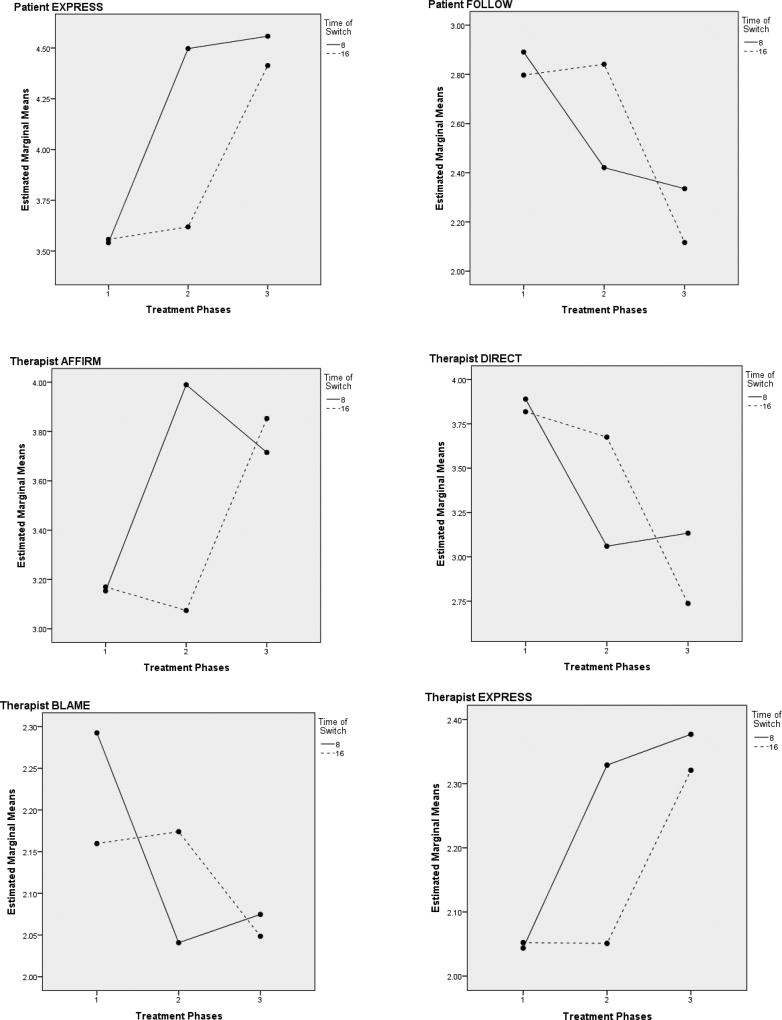
Table 3 presents means and standard deviations for patient interpersonal behavior in each treatment phase (1–3) and by switch in training condition (at session 8 and 16). In addition, it presents results from repeated measures analyses of variance, including main effects for changes in level by phase (within-subject) and for differences in level by condition (between-group), plus interaction effects for phase by condition. The analyses of interaction effects were the principal objective of our study as they examined differences in slope on the various interpersonal variables that could be attributed to AFT, based on the multiple baseline design. The results regarding patient interpersonal behavior indicated statistically significant (medium to large) main effects of phase (within-subject) for Patient Express, Follow, and Appease: an increase for patient expressiveness across time and a decrease for the other patient dependency (both hostile and friendly). In addition, there was a medium within-subject effect for Patient Avoid that approached significance (p = .081) and suggested a decrease in this behavior over time. There was also a statistically significant (medium to large) main effect for condition (between-group) with regard to Patient Express and Avoid, indicating a higher level of expressiveness and a lower level of avoidance in patients in the condition with more AFT. Most importantly, there were statistically significant (medium to large) interactions for phase by condition with regard to Patient Express and Patient Follow with more expressiveness and less dependence by the patient that could be attributed to AFT. There was also a medium interaction effect for Patient Appease that approached significance (p = .086) and suggested AFT accelerated the decrease in patient hostile compliance over time. Figure 4 depicts the significant interaction effects and the effect of AFT on these patient variables. In order to further probe the interaction effects, post-hoc tests of simple main effects were conducted and indicated a significant large difference on Patient Express (F = 31.660, p < .001, eta2 = .454) at only Phase 2 (not at Phases 1 and 3) between the two training conditions; there was also a medium difference that approached significance on Patient Avoid (F = 3.600, p < .065, eta2 = .087) at Phase 2.
Figure 4.
Interactions of change in patient and therapist behavior (on the SASB) by switch in training condition
Note. SASB=Social Analysis of Social Behavior
Table 4 presents means and standard deviations for therapist interpersonal behavior in each treatment phases (1–3) and by switch in training condition (at session 8 and 16). It also presents results from repeated measures analyses of variance, including main effects for changes in level by phase (within-subject) and for differences in level by condition (between-group), plus interaction effects for phase by condition. The results regarding therapist interpersonal behavior indicated statistically significant (medium to large) main effects of phase for Therapist Affirm, Express, Direct, and Blame, indicating an increase for therapist understanding and expressiveness across time and a decrease for controlling behaviors, such as direction and criticism. There was also a significant (medium to large) main effect for condition with regard to Therapist Affirm, indicating a greater level of therapist understanding with more exposure to AFT. Most importantly, there were significant (medium to large) interactions for phase by condition with regard to Therapist Affirm, Express, Direct and Blame, indicating that changes in these behaviors could be attributed to AFT: that is, increases in encouraging and experiencing friendly autonomy (both in terms of affirmation and expressiveness) and decreases in exerting control (both hostile and friendly). Figure 4 also depicts these significant interaction effects and the effect of AFT on these therapist variables. Post-hoc tests of simple main effects indicated large, significant differences on Therapist Affirm (F = 22.612, p < .001, eta2 = .373), Therapist Direct (F = 6.782, p < .05, eta2 = .151), and Therapist Express (F = 12.519, p < .001, eta2 = .092) at only Phase 2 between the two training conditions; there was also a medium difference that approached significance on Therapist Blame (F = 3.865, p < .057, eta2 = .248) at Phase 2.2
Table 4.
Therapist interpersonal behavior (SASB) in treatment phase by switch in training condition
| Main Effect | Main Effect | Interaction Effect | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | Phase 2 | Phase 3 | Phase (Within-Subject) | Condition (Between-Group) | Phase × Condition | ||||||||
| Focus on Other | M (SD) | M (SD) | M (SD) | F (2, 37) | p-value | eta2 | F (1,38) | p-value | eta2 | F (2, 37) | p-value | eta2 | |
| Affirm | |||||||||||||
| Switch at 08 | 3.15 (.33) | 3.99 (.67) | 3.72 (.74) | 12.618 | .000 | .405 | 4.722 | .036 | .111 | 10.495 | .000 | .362 | |
| Switch at 16 | 3.17 (.40) | 3.07 (.55) | 3.85 (.73) | ||||||||||
| Direct | |||||||||||||
| Switch at 08 | 3.89 (.73) | 3.06 (.61) | 3.13 (.87) | 11.123 | .000 | .375 | .126 | .724 | .003 | 7.303 | .002 | .283 | |
| Switch at 16 | 3.82 (.81) | 3.68 (.86) | 2.74 (.48) | ||||||||||
| Blame | |||||||||||||
| Switch at 08 | 2.29 (.35) | 2.04 (.13) | 2.07 (.16) | 7.737 | .002 | .295 | .033 | .856 | .001 | 4.355 | .020 | .191 | |
| Switch at 16 | 2.16 (.13) | 2.17 (.28) | 2.05 (.13) | ||||||||||
| Focus on Self | |||||||||||||
| Express | |||||||||||||
| Switch at 08 | 2.04 (.09) | 2.33 (.33) | 2.38 (.48) | 11.259 | .000 | .378 | 2.851 | .100 | .070 | 5.856 | .006 | .240 | |
| Switch at 16 | 2.05 (.09) | 2.05 (.11) | 2.32 (.42) | ||||||||||
Note. SASB=Social Analysis of Social Behavior
Discussion
The present study demonstrates the additive effect of an alliance-focused training (AFT) on the interpersonal process of a cognitive-behavioral therapy (CBT) for personality disorders. The SASB was used to operationally define patient and therapist interpersonal behaviors in the therapeutic alliance and to track changes in process following the introduction of AFT. Consistent with our predictions, we found AFT facilitated a decrease in patient following (less dependency on the therapist) and an increase in patient expressiveness (more self-disclosure). We also found AFT facilitated a decrease in therapist blaming and directing (less controlling of the patient), and an increase in therapist affirmation and expressiveness (more understanding of the patient and more self-disclosure). We found partial support for our predictions regarding a decrease in patient hostile behaviors of avoidance and appeasement subsequent to AFT. Specifically, while the interaction for phase by training condition with regard to patient avoidance was not significant, the main effect for condition was significant, indicating that patients of therapists who received more AFT had a lower level of avoidance. The interaction for phase by condition with regard to patient appeasing approached significance. However, we did not find support for our prediction regarding a decrease in patient blaming behaviors.
Our findings regarding relationships between process variables and session-level or overall outcome provide some support for the value of these changes in interpersonal process. We found that patient expressing was positively related to session impact and treatment outcome, and patient appeasing and blaming were negatively related to treatment outcome, which is consistent with prior research using the SASB (e.g., Henry, Schacht, & Strupp, 1986, 1990). We also found that patient following and therapist directing were negatively correlated with session impact. Some studies using the SASB have linked the complementary behaviors of following and directing to good outcome (e.g., Coady, 1991; Jorgensen et al., 2000); however, our research on rupture resolution has identified withdrawal ruptures that may manifest as deferential patient behaviors and managing therapy behaviors that mask underlying tensions and thereby constitute a “pseudoalliance” (see Safran & Muran, 2000). We would argue that patient following, including behaviors of trusting and relying, could be aspects of a rupture, and that a therapist movement away from directing could facilitate patient self-assertion in service of resolving a rupture. Movement from patient following to patient expressing could be particularly important for patients with difficulties with assertiveness, such as patients with Cluster C personality disorders. The finding of this study that patient following and therapist directing were negatively correlated with session impact provides some support for our view.
Our findings are also consistent with the Castonguay, Goldfried, Wiser, Raue, and Hayes (1996) finding that better outcome in CBT was linked to greater patient emotional expression and exploration (as measured by the Experiencing Scales). Castonguay et al. also found in a post hoc descriptive analysis that in poor outcome cases, CBT therapists seemed to double down on their efforts to explain and challenge cognitive distortions in response to patients’ negative reactions to the treatment process—in other words, to become more directive and adherent to CBT techniques in the context of a rupture. Our results parallel those findings: We found that therapists directiveness to be negatively related to change in session impact and AFT to be faciltative in decreasing this behavior.
Although we found AFT facilitated greater therapist expressiveness, which (along with therapist affirmation of patient experience) was defined as central to the rupture resolution process according to Safran and Muran (1996), we did not demonstrate any relationship of this variable to session impact or treatment outcome. An increase in this variable as a result of AFT is understandable, given AFT is primarily informed by principles derived from the Safran and Muran model. There is a great emphasis in AFT on expanding therapist awareness of their internal experience and developing skill in therapeutic metacommunication. This emphasis should result in greater emotional awareness and disclosure. There is a growing number of case studies on “therapeutic immediacy,” which involves therapist self-disclosure in relation to the patient, demonstrating its impact on the therapeutic alliance and patient processing of emotional experience (Clemence et al., 2012; Hill et al., 2014). More research with regard to therapist expressiveness and its relevance to change is certainly needed.
In this study, AFT impacted positive interpersonal process more than negative, particularly with regard to the increase in patient expressiveness, but no significant decrease in patient blaming, and only partial evidence of a decrease in patient avoiding and appeasing. It is important to consider a number of points: There is a well-demonstrated inverse relationship between positive and negative interpersonal behavior, as captured by the circumplex conception (e.g., Kiesler, 1996) and also suggested by our preliminary analyses. There is also limited evidence of negative behavior in our study, consistent with other SASB-based psychotherapy process studies (Critchfield et al., 2007; Coady & Marziali, 1994; Henry et al, 1986, 1990; Jorgenson et al., 2000). This is particularly understandable given that many of the patients in this study were diagnosed with a personality disorder of a more anxious and avoidant nature, with interpersonal problems oriented towards deference and dependence (e.g., Benjamin, 1996; Pincus & Wiggins, 1990). Our findings demonstrate that the negotiation of the therapeutic alliance does not simply involve hostility and friendliness, but also autonomy and dependence. Movement toward autonomy (or expressiveness) may be as or even more important than the movement away from hostility, especially for patients with difficulties with self-assertion.
As highlighted, many have argued that the SASB provides an operational definition of patient and therapist interpersonal behavior in the therapeutic alliance (Benjamin & Critchfield, 2010; Henry & Strupp, 1994) that is more precise than measures that are more global in definition, such as the Working Alliance Inventory (WAI: Horvath & Greenberg, 1989), which combines patient and therapist respective contributions. Elsewhere, we have argued for a definition of the alliance construct that includes the continuous negotiation of patient and therapist respective needs for autonomy and relatedness (Safran & Muran, 2000; 2006): The SASB captures this conceptualization well with its circumplex dimensions. Nevertheless, a limitation of this study is our use of a simplified version of the SASB to facilitate coding of a large number of sessions (120). This precluded an even more detailed and nuanced analysis of patient-therapist interactions that the complete version of the SASB can provide. Future efforts could try to replicate our findings with a more intensive analysis. In addition, future studies could apply observer-based measures that are more phenomenon-specific: measures designed to specifically assess ruptures events and resolution processes, such as the Collaborative Interaction Scale (CIS: Colli & Lingiardi, 2009) and the Rupture Resolution Rating System (3RS: Eubanks, Muran, & Safran, 2015b).
Other important considerations with regard to our findings and future directions involve our sample. Its size raises questions regarding reliability and generalizability of our findings. Further, the majority of our patients (87.5%) presented with comorbid Axis I and Axis II disorders, which is consistent with the complexity often encountered in real-world settings, such as clinics and private practices (Dolan-Sewell, Krueger, & Shea, 2001; Kessler et al., 1994; Zimmerman, McDermut, & Mattia, 2000). Nevertheless, active eating, obsessive-compulsive, substance use disorders, and Cluster A and B personality disorders were excluded, which limits the generalizability of our findings, as do other demographics of our participants (e.g., predominantly White, majority with college degrees). Our study demonstrates the effect of AFT on novice therapists, which supports the evidence that therapists at this stage are trainable (e.g., Henry et al., 1993; Weissman, Rounsaville, & Chevron, 1982). This suggests the potential value of an AFT component for psychotherapy training programs. Of course, the extent to which AFT can have an impact on more experienced therapists is left for future investigations.
AFT involves developing therapist skills with regard to interpersonal sensitivity and affect regulation. It includes a didactic component (e.g., readings and discussions of conceptualizations of interpersonal process in psychotherapy), but concentrates on the experiential –the use of mindfulness meditation and awareness exercises to cultivate these skills. Our findings provide some support for its effect on interpersonal process in a CBT with the sample discussed above. Our multiple baseline design determined time of exposure to AFT (22 versus 14 sessions): It remains to be determined if a briefer training (e.g., a one-day workshop) would still be impactful, or if a longer training would yield even greater benefit (e.g., more sophistication in applying AFT principles). Other questions that should be addressed are: What elements of AFT are essential? For example, if we were to dismantle AFT, could the didactic component suffice, or could mindfulness alone be impactful? And of course are there other strategies? Our application of AFT in a group format (which differs from our previous research where individual and group supervisions were combined) was done to promote dissemination. The importance of dissemination should remain an important objective. Some other questions for future consideration are if other trainers can apply AFT with comparable impact, and whether AFT can benefit other treatment models and other patient populations.
In conclusion, with an innovative application of a multiple baseline design, we were able to demonstrate that an alliance-focused training model facilitated changes in interpersonal process in a CBT that was applied by novice therapists in a medical outpatient clinic setting to a sample of patients comorbid on Axis I and II conditions and that some of these improvements were directly linked to outcome in this study. As a result of the training, there were significant improvements with regard to increasing patient expressiveness and therapist understanding and decreasing therapist criticism. Given the importance of the therapeutic alliance for treatment retention and outcome, this study has great public health significance: it provides support for a training intervention provided in an early stage of professional development that could provide a longstanding and widespread beneficial effect on the delivery of psychotherapy services.
Supplementary Material
Figure 3.
Quadrant version of the simplified Structural Analysis of Social Behavior (SASB)
Acknowledgments
The research was supported by Grant MH071768 from the National Institute of Mental Health.
Footnotes
All authors also affiliated with the Brief Psychotherapy Research Program, Mount Sinai Beth Israel, where the research was conducted.
Although there has been some debate around the use of residualized gain scores versus raw difference scores (e.g., Larzelere, Kuhn, & Danelia, 2010), we chose to apply the former, based on the longstanding argument (see Cronbach & Furby, 1970) that it potentially provides more precision than raw difference scores, which assume that the regression weight of prior measures to predict post-scores is 1.0. Instead, the residualized gain score provides an empirically-derived regression weight from the actual regression of pre-scores predicted from post-scores. It is also arguably more appropriate given our experimental design and sample size (see Gollwitzer, M., Christ, O., & Gunnar, L., 2014).
We also examined the impact of AFT on change in therapist fidelity as measured by the BIFS across across the three phases of treatment. The results are presented as supplemental materials online.
Contributor Information
J. Christopher Muran, Derner Institute of Advanced Psychological Studies, Adelphi University.
Jeremy D. Safran, Department of Psychology, New School for Social Research
Catherine F. Eubanks, Ferkauf Graduate School of Psychology, Yeshiva University
Bernard S. Gorman, Derner Institute of Advanced Psychological Studies, Adelphi University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Bates D. Fitting linear mixed models in R. R News. 2005;5:27–30. [Google Scholar]
- Bates D, Maechler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software. 2015;67(1):1–48. [Google Scholar]
- Battle CC, Imber SD, Hoehn-Saric R, Stone AR, Nash ER, Frank JD. Target complaints as criteria of improvement. American Journal of Psychotherapy. 1966;20:184–192. doi: 10.1176/appi.psychotherapy.1966.20.1.184. [DOI] [PubMed] [Google Scholar]
- Beck AT, Freeman A Associates. Cognitive therapy of personality disorders. New York: Guilford Press; 1990. [Google Scholar]
- Beck JS. Cognitive therapy: Basics & beyond. New York: Guilford Press; 1995. [Google Scholar]
- Benjamin LS. Structural analysis of social behavior. Psychological Review. 1974;81:392–425. [Google Scholar]
- Benjamin LS, Critchfield KL. An interpersonal perspective on therapy alliances and techniques. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 97–122. [Google Scholar]
- Benjamin LS, Karpiak CP. Personality disorders. Psychotherapy. 2001;38:487–491. [Google Scholar]
- Bordin E. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy. 1979;16:252–260. [Google Scholar]
- Castonguay LG, Goldfried MR, Wiser S, Raue PJ, Hayes AM. Predicting the effect of cognitive therapy for depression: A study of unique and common factors. Journal of Consulting & Clinical Psychology. 1996;64:497–504. [PubMed] [Google Scholar]
- Castonguay LG, Hayes AM, Goldfried MR, DeRubeis RJ. The focus of therapist interventions in cognitive therapy for depression. Cognitive Therapy & Research. 1995;19:485–503. [Google Scholar]
- Clarkin JF, Levy KN. The influence of client variables in psychotherapy. In: Lambert MJ, editor. Bergin & Garfield’s Handbook of Psychotherapy & Behavior Change. 5. New York, NY: John Wiley & Sons; 2004. pp. 194–226. [Google Scholar]
- Clemence AJ, Fowler JC, Gottdiener WH, Krikorian S, Charles M, Damsky L, Johnson B. Microprocess examination of therapeutic immediacy during a dynamic research interview. Psychotherapy. 2012;49:317. doi: 10.1037/a0026090. [DOI] [PubMed] [Google Scholar]
- Coady NF. The association between client and therapist interpersonal processes and outcomes in psychodynamic psychotherapy. Research on Social Work Practice. 1991;1:122–138. [Google Scholar]
- Coady NF, Marziali E. The association between global and specific measures of the therapeutic relationship. Psychotherapy. 1994;31:17–27. [Google Scholar]
- Colli A, Lingiardi V. The Collaborative Interactions Scale: A new transcript-based method for the assessment of therapeutic alliance ruptures and resolutions in psychotherapy. Psychotherapy Research. 2009;19:718–734. doi: 10.1080/10503300903121098. [DOI] [PubMed] [Google Scholar]
- Constantino MJ. Interpersonal process in psychotherapy through the lens of the Structural Analysis of Social Behavior. Applied & Preventive Psychology. 2000;9:153–172. [Google Scholar]
- Critchfield KL, Henry WP, Castonguay LG, Borkovec TD. Interpersonal process and outcome in variants of cognitive–behavioral psychotherapy. Journal of Clinical Psychology. 2007;63:31–51. doi: 10.1002/jclp.20329. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ, Furby L. How we should measure "change": Or should we? Psychological Bulletin. 1970;74:68–80. [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring, & procedures manual II. Towson, MD: Clinical Psychiatric Research; 1983. [Google Scholar]
- Dolan-Sewell RT, Krueger RF, Shea MT. Co-occurrence with syndrome disorders. In: Livesley WJ, editor. Handbook of personality disorders: Theory, research, & treatment. New York: Guilford Press; 2001. pp. 84–104. [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychological review. 1993;100(3):363. [Google Scholar]
- Eubanks CF, Lubitz J, Muran JC, Safran JD. Rupture Resolution Rating System (3RS): Reliability & Validity. 2017 doi: 10.1080/10503307.2018.1552034. Manuscript submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eubanks CF, Muran JC, Safran JD. Repairing alliance ruptures. In: Norcross JC, Wampold BE, editors. Psychotherapy relationships that work. 3. New York, NY: John Wiley & Sons; (in press) [Google Scholar]
- Eubanks-Carter C, Muran JC, Safran JD. Alliance ruptures and resolution. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 74–94. [Google Scholar]
- Eubanks-Carter C, Muran JC, Safran JD. Alliance-focused training. Psychotherapy. 2015a;52:169–173. doi: 10.1037/a0037596. [DOI] [PubMed] [Google Scholar]
- Eubanks-Carter C, Muran JC, Safran JD. The Rupture Resolution Rating Scale (3RS) Mount Sinai Beth Israel; New York, NY: 2015b. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Benjamin LS. User's guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II. American Psychiatric Press; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. User's guide for the Structured clinical interview for DSM-IV axis I disorders: SCID-I. American Psychiatric Press; 1997. [Google Scholar]
- Goldfried MR, Castonguay LG, Hayes AM, Drozd JF, Shapiro DA. A comparative analysis of the therapeutic focus in cognitive-behavioral and psychodynamic-interpersonal sessions. Journal of Consulting & Clinical Psychology. 1997;65:740–748. doi: 10.1037//0022-006x.65.5.740. [DOI] [PubMed] [Google Scholar]
- Goldfried MR, Raue PJ, Castonguay LG. The therapeutic focus in significant sessions of master therapists: A comparison of cognitive-behavioral and psychodynamic-interpersonal interventions. Journal of Consulting & Clinical Psychology. 1998;66:803–810. doi: 10.1037//0022-006x.66.5.803. [DOI] [PubMed] [Google Scholar]
- Goldfried MR, Wolfe BE. Psychotherapy practice and research: Repairing a strained relationship. American Psychologist. 1996;51:1007–1016. doi: 10.1037//0003-066x.51.10.1007. [DOI] [PubMed] [Google Scholar]
- Gollwitzer M, Christ O, Gunnar L. Individual differences make a difference: On the use and the psychometric properties of difference scores in social psychology. European Journal of Social Psychology. 2014;44:673–682. [Google Scholar]
- Gross JJ. Emotion regulation: Current status and future prospects. Psychological Inquiry. 2015;26:1–26. [Google Scholar]
- Hatcher RL, Barends AW. How a return to theory could help alliance research. Psychotherapy. 2006;43:292–299. doi: 10.1037/0033-3204.43.3.292. [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, Strupp HH. Structural analysis of social behavior: Application to a study of interpersonal process in differential psychotherapeutic outcome. Journal of Consulting & Clinical Psychology. 1986;54:27–31. doi: 10.1037//0022-006x.54.1.27. [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, Strupp HH. Patient and therapist introject, interpersonal process, and differential psychotherapy outcome. Journal of Consulting & Clinical Psychology. 1990;58:768–774. doi: 10.1037//0022-006x.58.6.768. [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, Strupp HH, Butler SF, Binder JL. Effects of training in time-limited dynamic psychotherapy: Mediators of therapists’ responses to training. Journal of Consulting & Clinical Psychology. 1993;61:441–447. doi: 10.1037//0022-006x.61.3.441. [DOI] [PubMed] [Google Scholar]
- Henry WP, Strupp HH. The therapeutic alliance as interpersonal process. In: Horvath AO, Greenberg LS, editors. The working alliance: Theory, research, & practice. New York: John Wiley & Sons; 1994. pp. 51–84. [Google Scholar]
- Hill CE. Qualitative studies of negative experiences in psychotherapy. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidenced-based guide to practice. New York, NY: Guilford Press; 2010. pp. 63–73. [Google Scholar]
- Hill CE, Gelso C, Chui H, Miles JR. To be or not to be immediate with clients: The use and perceived effects of immediacy in psychodynamic/interpersonal psychotherapy. Psychotherapy Research. 2014;3:299–315. doi: 10.1080/10503307.2013.812262. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Jorgensen C, Hougaard E, Rosenbaum B, Valbak K, Rehfeld E. The Dynamic Assessment Interview (DAI), interpersonal process measured by Structured Analysis of Social Behavior (SASB) and therapeutic outcome. Psychotherapy Research. 2000;10:181–195. doi: 10.1093/ptr/10.2.181. [DOI] [PubMed] [Google Scholar]
- Kapfhammer HP, Hippius H. Psychopharmacological approaches in the treatment of personality disorders. Journal of Personality Disorders. 1998;12:277–288. doi: 10.1521/pedi.1998.12.3.277. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 2. Boston: Allyn & Bacon; 1992. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Study. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kiesler DJ. Contemporary interpersonal theory & research: Personality, psychopathology, & psychotherapy. New York: John Wiley & Sons; 1996. [Google Scholar]
- Klein MH, Mathieu-Coughlan P, Kiesler DJ. The Experiencing Scales. In: Greenberg LS, Pinsof WM, editors. The psychotherapeutic process: A research handbook. New York: Guilford Press; 1986. pp. 21–72. [Google Scholar]
- Lambert MJ. Prevention of treatment failure: The use of measuring, monitoring, & feedback in clinical practice. Washington, DC: APA Books; 2010. [Google Scholar]
- Larzelere RE, Ferrer E, Kuhn BR, Danelia K. Differences in causal estimates from longitudinal analyses of residualized versus simple gain scores: Contrasting controls for selection and regression artifacts. International Journal of Behavioral Development. 2010;34:180–189. [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting & Clinical Psychology. 2000;68:438–450. [PubMed] [Google Scholar]
- Muran JC. A relational approach to understanding change: Plurality and contextualism in a psychotherapy research program. Psychotherapy Research. 2002;12:113–138. [Google Scholar]
- Muran JC. Confessions of a New York rupture researcher: An insider’s guide and critique. Psychotherapy Research. doi: 10.1080/10503307.2017.1413261. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Eubanks-Carter C. Developing therapist abilities to negotiate alliance ruptures. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 320–340. [Google Scholar]
- Muran JC, Safran JD, Samstag LW, Winston A. Evaluating an alliance-focused treatment for personality disorders. Psychotherapy. 2005;42:532–345. [Google Scholar]
- Muran JC, Safran JD, Gorman BS, Samstag LW, Eubanks-Carter C, Winston A. The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy. 2009;46:233–248. doi: 10.1037/a0016085. [DOI] [PubMed] [Google Scholar]
- Newman CF. Core competencies in cognitive-behavioral therapy. New York, NY: Routledge; 2013. [Google Scholar]
- Patton J, Muran JC, Safran JD, Wachtel PL, Winston A. Treatment adherence measure for three brief psychotherapies. Beth Israel Medical Center; New York, NY: 1998. [Google Scholar]
- Persons JB. Cognitive therapy in practice: A case formulation approach. New York: W.W. Norton; 1989. [Google Scholar]
- Persons JB, Burns DD, Perloff JM. Predictors of dropout and outcome in cognitive therapy for depression in a private practice setting. Cognitive Therapy & Research. 1988;9:539–557. [Google Scholar]
- Pincus AL, Wiggins JS. Interpersonal problems and conceptions of personality disorders. Journal of Personality Disorders. 1990;4:342–352. [Google Scholar]
- Roos J, Werbart A. Therapist and relationship factors influencing dropout from individual psychotherapy: A literature review. Psychotherapy Research. 2013;23:394–418. doi: 10.1080/10503307.2013.775528. [DOI] [PubMed] [Google Scholar]
- Safran JD, Muran JC. The resolution of ruptures in the therapeutic alliance. Journal of Consulting & Clinical Psychology. 1996;64:447–458. doi: 10.1037//0022-006x.64.3.447. [DOI] [PubMed] [Google Scholar]
- Safran JD, Muran JC. Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford Press; 2000. [Google Scholar]
- Safran JD, Muran JC. Has the concept of the therapeutic alliance outlived its usefulness? Psychotherapy. 2006;43:286–291. doi: 10.1037/0033-3204.43.3.286. [DOI] [PubMed] [Google Scholar]
- Safran JD, Segal ZV. An interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]
- Safran JD, Muran JC, Samstag LW. Resolving alliance ruptures: A task analytic investigation. The working alliance: Theory, research, and practice. 1994:225–255. [Google Scholar]
- Safran JD, Muran JC, Stevens C, Rothman M. A relational approach to supervision: Addressing ruptures in the alliance. In: Falender CA, Shafranske EP, editors. Casebook for clinical supervision: A competency-based approach. Washington, DC: APA Books; 2008. pp. 137–157. [Google Scholar]
- Safran JD, Muran JC, Samstag LW, Winston A. Evaluating alliance-focused intervention for potential treatment failures: A feasibility study and descriptive analysis. Psychotherapy. 2005;42:512. [Google Scholar]
- Safran JD, Muran JC, Demaria A, Boutwell C, Eubanks-Carter C, Winston A. Investigating the impact of alliance-focused training on interpersonal process and therapists' capacity for experiential reflection. Psychotherapy Research. 2014;24:269–285. doi: 10.1080/10503307.2013.874054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharf J, Primavera LH, Diener MJ. Dropout and therapeutic alliance: A meta-analysis of adult individual psychotherapy. Psychotherapy. 2010;47:637–645. doi: 10.1037/a0021175. [DOI] [PubMed] [Google Scholar]
- Shea MT. Core battery conference: Assessment of change in personality disorders. In: Strupp HH, Horowitz LM, Lambert MJ, editors. Measuring patient changes in mood, anxiety, & personality disorders. Washington, DC: APA Books; 1997. pp. 89–400. [Google Scholar]
- Shimokawa K, Lambert MJ, Smart DW. Enhancing treatment outcome of patients at risk of treatment failure: A meta-analytic and mega-analytic review of a psychotherapy quality assurance system. Journal of Consulting & Clinical Psychology. 2010;78:298–311. doi: 10.1037/a0019247. [DOI] [PubMed] [Google Scholar]
- Soldz S, Budman S, Demby A, Merry J. A short form of the inventory of interpersonal problems circumplex scales. Assessment. 1995;2:53–63. [Google Scholar]
- Stiles WB. Measurement of the impact of psychotherapy sessions. Journal of Consulting & Clinical Psychology. 1980;48:176–185. doi: 10.1037//0022-006x.48.2.176. [DOI] [PubMed] [Google Scholar]
- Stiles WB, Shapiro DA, Firth-Cozens JA. Correlations of session evaluations with treatment outcomes. British Journal of Clinical Psychology. 1990;29:13–21. doi: 10.1111/j.2044-8260.1990.tb00844.x. [DOI] [PubMed] [Google Scholar]
- Stiles WB, Honos-Webb, Surko M. Responsiveness in psychotherapy. Clinical Psychology: Science & Practice. 1998;5:439–458. [Google Scholar]
- Team, R.C. R: A language and environment for statistical computing. Vienna, Austria: 2017. [Google Scholar]
- Turner AE, Muran JC, Ochoa E. Cognitive-behavioral therapy for personality disorders: A treatment manual. San Diego, CA: Social & Behavioral Documents; 1992/2004. [Google Scholar]
- Wampold BE, Imel ZE. The great psychotherapy debate: Models, methods, & findings. 2. New York, NY: Routledge; 2015. [Google Scholar]
- Weissman MM, Rounsaville BJ, Chevron E. Training psychotherapists to participate in psychotherapy outcome studies. American Journal of Psychiatry. 1982;139:1442–1446. doi: 10.1176/ajp.139.11.1442. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, McDermut W, Mattia JI. Frequency of anxiety disorders in psychiatric outpatients with major depressive disorder. American Journal of Psychiatry. 2000;157:1337–1340. doi: 10.1176/appi.ajp.157.8.1337. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.