Abstract
Aim
Trauma, in geriatric patients, increases with age, and is a leading cause of disability and institutionalization, resulting in morbidity and mortality. The aim of our study was to analyse the prevalence of trauma, the related risk factors, mortality and sex differences in the prevalence in a geriatric population.
Patients and method
We observed 4,554 patients (≥65 years) with home injuries or car accidents. Patients were evaluated with ISS (Injury Severity Score) and major trauma with ATLS (Advanced Trauma Life Support). The instrumental investigation was in the first instance, targeted X-Ray or whole-body CT.
Results
In over four years of study we treated 4,554 geriatric: 2,809 females and 1,745 Males. When the type of trauma was analysed the most common was head injury, followed by fractures of lower and upper limbs. In our experience hospitalization mainly involved patients over 80. In all patients mortality during assessment was 0.06%.
Discussion
The geriatric patient is often defined as a “frail elderly”, for the presence of a greater “injury sensitivity”. This is due to the simultaneous presence of comorbidity, progressive loss of full autonomy and exposure to a high risk of traumatic events. Optimal management of the trauma patient can considerable reduce mortality and morbidity.
Conclusions
Falls and injuries in geriatric age are more frequent in women than in men. Among typical elder comorbidities, osteoporosis certainly causes a female preponderance in the prevalence of fractures. Our discharge data demonstrate that disability, which requires transfer to health care institutions, has a greater effect on women than men.
Keywords: Geriatric trauma, Elderly patients, Comorbidity, Mortality, Gender
Introduction
Trauma, in geriatric patients, increases with age, and is a leading cause of disability and institutionalization, also resulting in morbidity and mortality (1–5).
A deficit across the: visual, auditory, musculoskeletal and nervous systems, with reduced visual acuity, lower perception of pure tones, postural instability, deterioration of reflexes and/or slowing of reaction time, are closely related to age.
Also, comorbidities and drug therapies increase risk of trauma in the elderly (6–11).
Environmental risk alone may be enough to cause the traumatic event or may be a facilitating element.
The immediate and/or late consequences, which the elderly incurs in after a traumatic event are numerous: fractures, contusions, bruises, wounds, visceral lesions, head injuries, post-fall syndrome, death (12–14).
The most dangerous are craniofacial traumas which are related to high mortality, the most frequent, however, are hip fractures.
The hip fracture (especially proximal) is often secondary to an altered static and dynamic balance and, for the elderly, is one of the most debilitating traumatic event (15–19).
Disability determines sequelae directly proportional to age, such as prolonged bed rest, post-fall-Syndrome, increased risk of secondary and tertiary related events (pneumonia, bedsores, thromboembolic events etc.), greater recourse to the use of drugs, etc. (11).
All this leads to a significant increase in individual and social costs (hospitalization, home care, institutionalization) and risk of mortality (20–24).
The aim of our study was to analyse, from September 2012 to December 2016, the prevalence of trauma, related risk factors, mortality and sex differences in the prevalence in a geriatric population treated at our Emergency Department (UOC MCAU with OB).
Patients and method
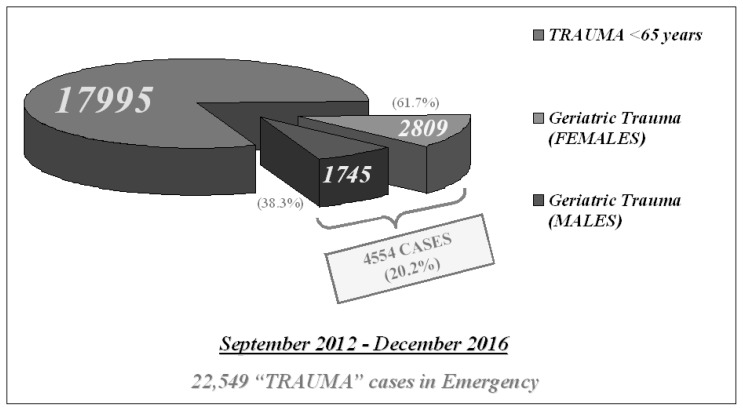
From September 2012 to December 2016, we recorded 22,549 patients with “TRAUMA”, 20.2% (4,554 cases) involved the elderly (≥65 years) with home injuries or car accidents.
Patients were evaluated with ISS (Injury Severity Score) (25, 26).
Major trauma (multiple injuries), was evaluated in the Shock Room by a multidisciplinary team, the approach followed the guidelines of the Advanced Trauma Life Support (ATLS).
The instrumental investigation was in the first instance, targeted X-Ray or whole-body CT.
Data on age, sex, hemodynamic parameters, mechanism of injury, number and location of lesions, medical history (focused on finding any concomitant pathologies) were collected.
According to the World Health Organization classification (WHO), patients were divided into 3 age groups:
- Age 65–74 yrs;
- Age 75–84 yrs;
- Age ≥85 yrs.
Results
In over four years of study (September 2012-December 2016) we treated 4,554 geriatric trauma, 20.2% of overall trauma cases in all ages (22,549 cases).
The patients studied, aged between 65 and 103 years old, were predominantly female: 2,809 females (61.7%) and 1,745 males (38.3%) (Figure 1).
Figure 1.
Complex Trauma Card.
Over 60% of patients, evaluated with the ISS, had score > 15 (class of gravity V-severe injuries), and 40% a score <15 (severity class I to IV).
The prevalence of trauma, in our population, was almost steady for each year of study.
The most affected age group was between 75 and 84 years (859 patients).
The prevalence in females was constant in each year of study, in each age group (65–74, 75–84; >85) and in each type of trauma except for abdominal trauma.
Moreover, despite the age group with larger number of traumas was between 75–84 years, in the comparison between the sexes, whilst women had a higher prevalence of trauma in this age range, men presented more commonly with trauma in the age range 65 and 74 years.
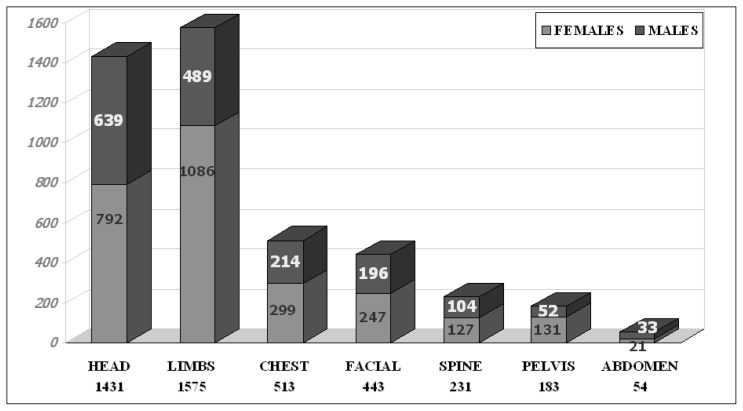
When the type of trauma was analysed the most common was head injury: 1,431 cases (792F/639M), followed by fractures of lower and upper limbs (1,575 cases: 1086F/489M, in 826 lower and 749 upper).
Chest trauma was recorded in 513 cases (299F/214M), facial in 443 cases (247F/196M), spinal 231 cases (127F/104M), pelvic (183 cases: 131F/52M), abdominal in 54 cases (21F/33M) (Figure 2).
Figure 2.
Causes of multiple traumas.
An increased frequency in patients aged over 85 of head trauma due to fall was observed.
The head injury in this age group was N=614 over a total of 1,431 (42.9%), with a female predominance 335F (54.6%)/279M (45.4%).
Head trauma is often associated with facial trauma (lesions of nasal bones, upper and/or lower jaw).
The prevalence of facial trauma in men and women was similar to that seen in head trauma, with a higher prevalence in females and a higher frequency in the aged >85, with 209 cases (47.2%) (out of 443 total), 112 women and 97 men.
In our series, head injury following a fracture of the lower and upper limbs occurred in 1,575 cases: 826 lower limbs and 749 upper limbs.
The lower limb injuries are more frequent in the over 80, with 382 cases, 259 women and 123 men, there is a constant majority of women in all three age groups.
Hip fracture (571 cases) is the most common injury, followed by lateral malleolus and knee fractures.
Hip fractures have a higher prevalence in females than in males (423F/148M) and a larger number of cases were observed in 2013 and in 2015, respectively 147 and 156 cases, compared to the study period.
The most frequent upper limb fracture (749 cases) was humerus (259 cases), with a considerably female majority (202F/57M).
Chest trauma associated with rib fractures, often accompanied by severe complications, such as pneumothorax, hemothorax or pulmonary contusions had a prevalence of 11.3% (513 cases) and more frequently was observed in patients over 80, with 228 cases in females (122F/106M).
Abdominal trauma was only 1.2% of all traumatic events (54 cases) and was the only type higher in males (21F and 33M).
Among minor trauma, the higher frequency was recorded for blunt trauma 26.7% (1,218 cases: 679F/539 M), mainly recorded in the age group 65–74 years (603 cases: 341F/262M).
We report the prevalence of most frequent comorbidities observed in Table 1.
Table 1.
REPORT PREVALENCE COMORBIDITIES.
| PREVALENCE COMORBIDITIES (%/patients) | |||
|---|---|---|---|
|
| |||
| COMORBIDITY (%/patients) | 65–74 years | 75–84 years | ≥ 85 years |
| Diabetes | 9% (409) | 10% (455) | 10% (455) |
| Hypertension | 60% (2732) | 75% (3415) | 76%(3461) |
| Coronary Artery Disease | 23% (1047) | 31% (1411) | 33% (1502) |
| Dementia | 4% (182) | 14% (637) | 26% (1184) |
| Reversibile anticoagulant therapy | 11% (501) | 19% (865) | 19% (865) |
| Antiplatelet therapy | 11% (501) | 13% (592) | 13% (592) |
| Celebral vascular disease | 8% (364) | 12.2% (552) | 12.5% (569) |
In our experience hospitalization mainly involved patients over 80 (N 674 patients, 421 women and 253 men).
Rapid discharge was more frequent in the 65–74 age group, with a total of 879 patients, including 459 women and 420 men.
Among the 4,554 patients admitted to the emergency department for trauma, 18.9% (N 862 patients of which 506 women and 356 men) refused hospitalization.
In all patients mortality during assessment was 0.06% (3 deaths out of 4554 cases).
The 3 patients who died were female and belonged to the age group over 80.
It was not possible to estimate the prevalence of long-term mortality.
Discussion
Given an increased aging population geriatric subjects (> 65 years) represent a significant portion of the population (27).
The frequent service use of emergency facilities amongst the elderly appears mostly related to a higher prevalence of traumatic events due to falls and/or accidental injuries (28–31).
Falls associated with syncopal events are recurrent.
The geriatric patient is often defined as a “frail elderly”, for the presence of a greater “injury sensitivity” (32).
This is due to the simultaneous presence of comorbidity, progressive loss of his full autonomy and exposure to a high risk of traumatic events (6–9).
Optimal management of the trauma patient can considerable reduce mortality and morbidity and results in a shorter hospital stays (33–38).
The early use of CT-scans is a useful method, in hemodynamically unstable elderly patients, for quick diagnosis of site and number of injuries to avoid any delay in treatment.
In our experience the correct application of protocols in the Shock Room was fundamental in reducing mortality and morbility (39–41).
Special care should apply to patients treated with anticoagulants or antiaggregation, in this population morbidity can be observed with a delay following the traumatic event (42).
We showed that, in geriatric age, the most common trauma in the emergency department was head trauma (31.4%), associated or not with other injury and/or fractures.
Often these patients are in pharmacological treatment with anticoagulants and/or antiaggregants and delayed risk of bleeding must be evaluated.
Recent studies underscore the need to re-evaluate patients for an observational period greater than 24 hours, followed by a second CT-scan, also in case of negative initial CT (43).
This protocol, in all probability, can detect cases of delayed intracranial hemorrhage.
Conclusions
Our data are similar to those in the current literature.
Falls and injuries in geriatric age are more frequent in women than in men, and the proportion increases with age.
Among typical old age comorbidities, osteoporosis certainly causes a female preponderance in the prevalence of fractures; the reduction of skeletal mass due to osteoporosis is greater in postmenopausal women than in men of the same age.
Hip fractures in female patients, over 65, are the most frequent, after wrist or proximal humerus ones.
Among all traumas affecting elderly patients, hip fractures are important, in most cases, this type of trauma determines an increase in institutionalization and can lead to clinical and social problems.
Our discharge data demonstrate the same prevalence and degree of disability produced by trauma in both sexes.
But it is once again evident that disability, which requires transfer to health care institutions, has a greater effect on women than men.
References
- 1.Aschkenasy MT, Rothenhaus TC. Trauma and falls in the elderly. Emerg Med Clin North Am. 2006;24:413–32. doi: 10.1016/j.emc.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 2.da Silva HC, Pessoa Rde L, de Menezes RM. Trauma in elderly people: access to the health system through pre-hospital care. Rev Lat Am Enfermagem. 2016;24:e2690. doi: 10.1590/1518-8345.0959.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shankar KN, Liu SW, Ganz DA. Trends and Characteristics of Emergency Department Visits for Fall-Related Injuries in Older Adults, 2003–2010. West J Emerg Med. 2017 Aug;18(5):785–793. doi: 10.5811/westjem.2017.5.33615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: Injury patterns and outcome. J Trauma. 1984;24:565–72. [PubMed] [Google Scholar]
- 5.Osler T, Hales K, Baack B, Bear K, Hsi K, Pathak D, et al. Trauma in the elderly. Am J Surg. 1988;156:537–43. doi: 10.1016/s0002-9610(88)80548-8. [DOI] [PubMed] [Google Scholar]
- 6.Kirshenbom D, Ben-Zaken Z, Albilya N, Niyibizi E, Bala M. Older Age, Comorbid Illnesses, and Injury Severity Affect Immediate Outcome in Elderly Trauma Patients. J Emerg Trauma Shock. 2017 Jul-Sep;10(3):146–150. doi: 10.4103/JETS.JETS_62_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGwin GL, McLennan PA, Fife JB, Davis GG, Rue LW. Pre-existing conditions and mortality in older trauma patients. J Trauma. 2004;56:1291–1296. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 8.Niven DJ, Kirkpatrick AW, Ball CG, Laupland KB. Effect of comorbid illness on the long-term outcome of adults suffering major traumatic injury: A population-based cohort study. Am J Surg. 2012;204:151–6. doi: 10.1016/j.amjsurg.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Hollis S, Lecky F, Yates DW, Woodford M. The effect of pre-existing medical conditions and age on mortality after injury. J Trauma. 2006;61:1255–60. doi: 10.1097/01.ta.0000243889.07090.da. [DOI] [PubMed] [Google Scholar]
- 10.Eschbach D, Kirchbichler T, Wiesmann T, Oberkircher L, Bliemel C, Ruchholtz S, Buecking B. Nutritional intervention in cognitively impaired geriatric trauma patients: a feasibility study. Clin Interv Aging. 2016 Sep 12;11:1239–1246. doi: 10.2147/CIA.S109281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neloska L, Damevska K, Nikolchev A, Pavleska L, Petreska-Zovic B, Kostov M. The Association between Malnutrition and Pressure Ulcers in Elderly in Long-Term Care Facility. Open Access Maced J Med Sci. 2016 Sep 15;4(3):423–427. doi: 10.3889/oamjms.2016.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs DG. Special considerations in geriatric injury. Curr Opin Crit Care. 2003;9:535–9. doi: 10.1097/00075198-200312000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Schoeneberg C, Probst T, Schilling M, Wegner A, Hussmann B, Lendemans S. Mortality in severely injured elderly patients: A retrospective analysis of a German level 1 trauma center (2002–2011) Scand J Trauma Resusc Emerg Med. 2014;22:45. doi: 10.1186/s13049-014-0045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: Geriatric status increases risk of delayed death. J Trauma. 1998;45:805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 15.Flikweert ER, Izaks GJ, Reininga IH, Wendt KW, Stevens M. Evaluation of the effect of a comprehensive multidisciplinary care pathway for hip fractures: design of a controlled study. BMC Musculoskelet Disord. 2013 Oct 12;14:291. doi: 10.1186/1471-2474-14-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalmet PH, Koc BB, Hemmes B, Ten Broeke RH, Dekkers G, Hustinx P, Schotanus MG, Tilman P, Janzing HM, Verkeyn JM, Brink PR, Poeze M. Effectiveness of a Multidisciplinary Clinical Pathway for Elderly Patients With Hip Fracture: A Multicenter Comparative Cohort Study. Geriatr Orthop Surg Rehabil. 2016 Jun;7(2):81–5. doi: 10.1177/2151458516645633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taraldsen K, Thingstad P, Sletvold O, Saltvedt I, Lydersen S, Granat MH, et al. The long-term effect of being treated in a geriatric ward compared to an orthopaedic ward on six measures of free-living physical behavior 4 and 12 months after a hip fracture – A randomised controlled trial. BMC Geriatr. 2015;15:160. doi: 10.1186/s12877-015-0153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aguado-Maestro I, Panteli M, García-Alonso M, Bañuelos-Díaz A, Giannoudis PV. Incidence of bone protection and associated fragility injuries in patients with proximal femur fractures. Injury. 2017 Aug 26; doi: 10.1016/j.injury.2017.08.035. pii: S0020-1383(17)30554-5. [DOI] [PubMed] [Google Scholar]
- 19.Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, et al. Comprehensive geriatric care for patients with hip fractures: A prospective, randomised, controlled trial. Lancet. 2015;385:1623–33. doi: 10.1016/S0140-6736(14)62409-0. [DOI] [PubMed] [Google Scholar]
- 20.Bala M, Willner D, Klauzni D, Bdolah-Abram T, Rivkind AI, Gazala MA, et al. Pre-hospital and admission parameters predict in-hospital mortality among patients 60 years and older following severe trauma. Scand J Trauma Resusc Emerg Med. 2013;21:91. doi: 10.1186/1757-7241-21-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demetriades D, Murray J, Sinz B, Myles D, Chan L. Epidemiology of major trauma and trauma deaths in Los Angeles county. J Am Coll Surg. 1998;187:373–383. doi: 10.1016/s1072-7515(98)00209-9. [DOI] [PubMed] [Google Scholar]
- 22.Morris S, Ridley S, Munro V, Christensen MC. Cost effectiveness of recombinant activated factor seven for the control of bleeding in patients with severe blunt trauma injuries in the United Kingdom. Anaesthesia. 2007;62:43–52. doi: 10.1111/j.1365-2044.2006.04896.x. [DOI] [PubMed] [Google Scholar]
- 23.Pape HC, Neugebauer E, Ridley SA, Chiara O, Nielsen TG, Christensen MC. Cost-drivers in acute treatment of severe trauma in Europe: a systematic review of literature. Eur J Trauma Emerg Surg. 2009;35:61–66. doi: 10.1007/s00068-008-8013-0. [DOI] [PubMed] [Google Scholar]
- 24.Velopulos CG, Enwerem NY, Obirieze A, Hui X, Hashmi ZG, Scott VK, Cornwell EE, 3rd, Schneider EB, Haider AH. National cost of trauma care by payer status. J Surg Res. 2013;184(1):444–9. doi: 10.1016/j.jss.2013.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolorunduro OB, Villegas C, Oyetunji TA, Haut ER, Stevens KA, Chang DC, Cornwell EE, 3rd, Efron DT, Haider AH. Validating the Injury Severity Score (ISS) in different populations: ISS predicts mortality better among Hispanics and females. J Surg Res. 2011 Mar;166(1):40–4. doi: 10.1016/j.jss.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: The TRISS method. Trauma score and the injury severity score. J Trauma. 1987;27:370–8. [PubMed] [Google Scholar]
- 27.Pitidis A, Gallo L, et al. Rapporti ISTISAN, 08/45. Italian National Institute of Health; 2008. The injury database (IDB) in Europe, surveillance of home and leisure accidents: Italy 2005. [Google Scholar]
- 28.Finelli FC, Jonsson J, Champion HR, Morelli S, Fouty WJ. A case control study for major trauma in geriatric patients. J Trauma. 1989;29:541–8. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Seow-Yian T, Sloan EP, Zun L, Zaret P. Comparison of the new injury severity score and the injury severity score. J Trauma. 2004;56:162–164. doi: 10.1097/01.TA.0000058311.67607.07. [DOI] [PubMed] [Google Scholar]
- 30.Osler T, Rutledge R, Deis J, Bedrick E. An international classification of disease –9 based injury severity score. J Trauma. 1996;41:380–388. doi: 10.1097/00005373-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Zeckey C, Kammerlander C. Whats New in Emergencies Trauma and Shock? Age and Trauma: Geriatric Trauma Patients and Geriatric Trauma Ward Services. J Emerg Trauma Shock. 2017 Jul-Sep;10(3):89–90. doi: 10.4103/0974-2700.212495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pape HC, Bischoff-Ferrari HA. How can we influence the incidence of secondary fragility fractures? A review on current approaches. Injury. 2017 Sep 1; doi: 10.1016/j.injury.2017.08.034. pii: S0020-1383(17)30553-3. [DOI] [PubMed] [Google Scholar]
- 33.Demetriades D, Karaiskakis M, Velmahos G, Alo K, Newton E, Murray J, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89:1319–22. doi: 10.1046/j.1365-2168.2002.02210.x. [DOI] [PubMed] [Google Scholar]
- 34.Trunkey DD. Trauma centers and trauma systems. JAMA. 2003 Mar 26;289(12):1566–7. doi: 10.1001/jama.289.12.1566. [DOI] [PubMed] [Google Scholar]
- 35.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma center care on mortality. N Eng J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 36.Chiara O, Cimbanassi S, Pitidis A, Vesconi S. Preventable trauma deaths: from panel review to population-based studies. World J Em Surg. 2006;1:1–7. doi: 10.1186/1749-7922-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gioffre-Florio M, Murabito LM, Visalli C, Villari A, Lauritano F, Bramanti C, Fama F. The relationship between scores and outcomes for polytrauma patients in the emergency department A case study. Ann Ital Chir. 2016 Dec;29:5. [PubMed] [Google Scholar]
- 38.Liem IS, Kammerlander C, Raas C, Gosch M, Blauth M. Is there a difference in timing and cause of death after fractures in the elderly? Clin Orthop Relat Res. 2013;471:2846–51. doi: 10.1007/s11999-013-2881-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gioffrè Florio M, Famà F, Gullo G, Buccheri G, Beccaria A, Caruso A, Cucinotta F, Estollere C, Malara C, Mamo M, Manti L, Placanica P, Versace G. Management of polytrauma: our experience. Chir Ital. 2005;57(4):485. [PubMed] [Google Scholar]
- 40.Gioffrè Florio MA, Famà F, Gullo G, Buccheri G, Mazzei S. Gunshot wounds. Our experience. Chir Ital. 2006;58(6):779–83. [PubMed] [Google Scholar]
- 41.Marcus-Varwijk AE, Koopmans M, Visscher TL, Seidell JC, Slaets JP, Smits CH. Optimizing Tailored Health Promotion for Older Adults: Understanding Their Perspectives on Healthy Living. Gerontol Geriatr Med. 2016 Feb 2;2 doi: 10.1177/2333721415625293. 2333721415625293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mayberry JC, Kroeker AD, Ham LB, Mullins RJ, Trunkey DD. Long-term morbidity, pain, and disability after repair of severe chest wall injuries. Am Surg. 2009;75(5):389–94. [PubMed] [Google Scholar]
- 43.Heffernan DS, Thakkar RK, Monaghan SF, Ravindran R, Adams CA, Jr, Kozloff MS, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69:813–20. doi: 10.1097/TA.0b013e3181f41af8. [DOI] [PubMed] [Google Scholar]