Abstract
Supplemental Digital Content is Available in the Text.
This article describes the process and evaluation of embedding the IASP Pain Curriculum for Physical Therapy into a 3-year Doctor of Physiotherapy Program in Australia.
Key Points
The IASP Pain Curricula provide a comprehensive framework to expand and redesign education programs, to address major deficiencies in the pre-licensure pain education of health professionals.
The 2012 IASP Pain Curriculum for Physical Therapy has been prospectively embedded into a 3-year pre-licensure Doctor of Physiotherapy Program in Australia.
These physical therapy students improved their knowledge about pain and achieved a high level of clinical competencies in pain management.
1. Introduction
Major deficiencies in pain education for health professionals have been increasingly recognised. In the United States, the National Institutes of Health Pain Consortium identified significant gaps in pain content across 6 interprofessional pre-licensure health science education programs.7 In a landmark report, the U.S. Institute of Medicine (2012) stated that a major impediment to adequate pain relief was patients' limited access to clinicians who are knowledgeable about pain, which was related to the prevalence of outmoded or unscientific knowledge and attitudes about pain.19 In response, several recommendations have been made to better educate health professionals on pain, its causes and treatments. Three key educational recommendations from the U.S. Institute of Medicine were: (1) to expand and redesign education programs to transform the understanding of pain; (2) to improve the curricula and education for health care professionals; and (3) to increase the number of health professionals with advanced expertise in pain care.14 These recommendations align with other national pain strategies, such as Australia's National Pain Strategy, in which the key education-related goal is to increase the skill of health professionals through comprehensive education and training in evidence-based pain management.18 Although these recommendations regarding pain education for health care professionals apply across the spectrum of disciplines, this article focuses on the specific topic of pain education in physical therapy pre-licensure (entry-level) programs.
A 2001 survey of 169 accredited Doctor of Physical Therapy (DPT*) programs in North America found that the modal amount of time spent on pain in their curricula was only 4 hours, with a large proportion of faculty perceiving that this was inadequate.20 Although the situation in some programs has improved significantly since then, with a 2009 survey of designated pain content in Canadian pre-licensure programs reporting a mean of 41 hours (SD: 16; range: 18–69),23 and a 2012 U.S. survey of DPT schools reporting a mean of 31 hours (SD: 1.8; range: 5–115 hours),1 concern about the adequacy of this education remains. Only 63% of DPT schools in the United States believe that their students receive adequate instruction in pain management.1 Furthermore, persisting deficits in curriculum content and competencies have been identified, such as understanding pain mechanisms and the assessment and management of pain across the lifespan.1 To address the disparity in hours of pain education across DPT programs (range: 6–123 hours) and to ensure that pre-licensure physiotherapists have the skills necessary for adequate pain management, it has been recommended that a standardised pain education curriculum be incorporated into DPT programs.1 In 2012, a full review and update of the IASP Pain Curriculum for Physical Therapy was completed.13 This article describes how the 2012 IASP Pain Curriculum for Physical Therapy was prospectively embedded into an Australian pre-licensure DPT program, providing a framework for the redesign of pain education in this context.
2. Methods
2.1. Context: the Doctor of Physiotherapy Program at Macquarie University, Australia
A new 3-year pre-licensure Doctor of Physiotherapy (DPT) program commenced in 2012 at the Department of Health Professions at Macquarie University, in Sydney, Australia. The program was developed to meet international benchmarks, national regulatory, and professional standards. The Department of Health Professions at Macquarie is colocated with a private University hospital (Macquarie University Hospital) and Clinics, which are now integrated to form Australia's first academic health campus.
The Macquarie University DPT program has been designed to produce physiotherapists who are capable of providing innovative and creative solutions to health problems in Australia and globally. Skills training emphasises the provision of high-quality person-centred and evidence-based health care across the lifespan. The quality of the program is reflected by international recognition for its innovation.5 The World Health Organization (WHO)'s, International Classification of Functioning, Disability and Health (ICF) model underpins the Macquarie DPT program to frame students' knowledge and skill development. The 6-semester program blends foundation knowledge with mastery of clinical skills, inquiry-based learning, and reflective practice. The pedagogy of the program is reflected in the development of progressive skills and capabilities in each subsequent semester (Appendix 1, available online as supplemental digital content at http://links.lww.com/PR9/A15). This structure provides a logical, systematic flow throughout the course and ensures progressive development towards attainment of the program goals and professional standards. Embedded in the DPT program is the Health and Wellbeing Collaboration (HAWC) program in which volunteers from the community work with students to develop clinical skills and enhance students' understanding of health systems and health care. The HAWC program is embedded throughout the 3-year program, providing additional clinical opportunities for the students.
2.2. The IASP curriculum outline on pain for physical therapy
The pain curricula established by the IASP were designed for teaching courses on pain at the undergraduate and graduate level (IASP, May 2012), and the principles of the curriculum are based on the Declaration of Montreal (2010). The IASP Pain Curriculum for Physical Therapy13 is structured into 4 domains: (1) Multidimensional Nature of Pain; (2) Pain Assessment and Measurement; (3) Management of Pain; and (4) Clinical Conditions. Within each domain, there are 95 specific curriculum elements that were used to guide the design of content and clinical skills in the DPT program.
2.3. Embedding the IASP pain curriculum into the Macquarie DPT program
2.3.1. Guiding pedagogical frameworks
Two complimentary frameworks were used to guide embedding the IASP pain curriculum in the DPT program: (1) the WHO ICF model24 (see 2.1 above), in which pain is considered an impairment of body structure and function, which in turn limits activity and participation. The influences of environmental and personal factors on these relationships are central to this ICF model. (2) The biopsychosocial model,8 as advocated in the IASP Pain Curriculum (Section II, C). In the foundation semesters of the program, the traditional biopsychosocial model was taught as a fundamental framework for the assessment and management of pain. However, in third year, a reconceptualised model (Fig. 1)12 was introduced to explore the assessment and management of more complex pain presentations, specifically addressing the contributions of neuropathic and nociceptive mechanisms and the underlying neuroplastic processes of adaptation and modulation.
Figure 1.
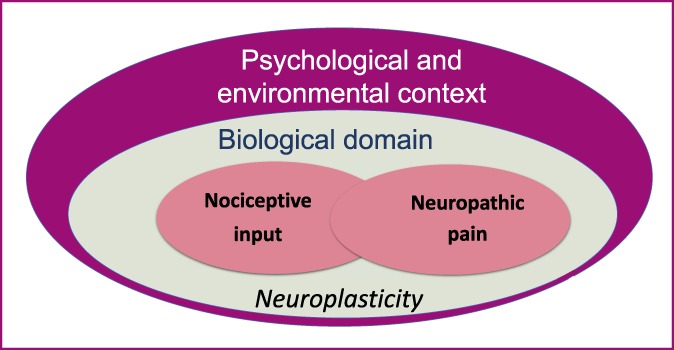
The reconceptualised biopsychosocial model of pain12 introduced in the third year of the Macquarie DPT program.
Because pain assessment and treatment are integral aspects of physical therapy management across disciplines and conditions (Principle 4 of the IASP Pain Curriculum), the pain content was designed to be implemented vertically (in each of the 3 years) and horizontally (in different units in each semester) throughout the program, rather than delivered as a stand-alone subject or module. This was designed to optimise educational outcomes by establishing foundational knowledge at the start of the program, and then extend students' understanding and clinical competencies in the later years of the program.
2.3.2. Educational model
The educational model guiding implementation of the IASP Pain Curriculum into the DPT program is illustrated in Figure 2. Our model was based on the work led by Kathleen Sluka, from which consensus-derived clinical competencies for pre-licensure physical therapy education in pain management were developed.11 Throughout the DPT program, there is a synergistic development of the students' pain-related knowledge and the attainment of clinical competencies. In the first semester of the program, knowledge about pain is addressed as an educational priority. Being a postgraduate degree, students commence with inconsistent levels of previous undergraduate training in pain science, and hence they start the DPT program widely varying beliefs and knowledge about pain. Early evaluation of these factors using validated assessment tools in the first week of the program enables teaching staff to identify inadequate knowledge about pain science. A consistent finding from evaluation of the first 6 student cohorts (2012–2017) on entry into the program is that the majority of students upheld a predominantly biomedical understanding of pain. This emphasised the importance of allocating a significant proportion of the first semester's (semester A) curriculum to facilitate changes in beliefs and knowledge about pain, with the goal of understanding pain as a multidimensional experience that is influenced by both bottom-up (ie, from the periphery) and top-down (ie, from the brain and spinal cord) modulatory influences. Once students attain sufficient foundational understanding of pain that aligns with current pain science, then training can commence to develop clinical skills and competencies in patient assessment, treatment, and clinical reasoning.
Figure 2.
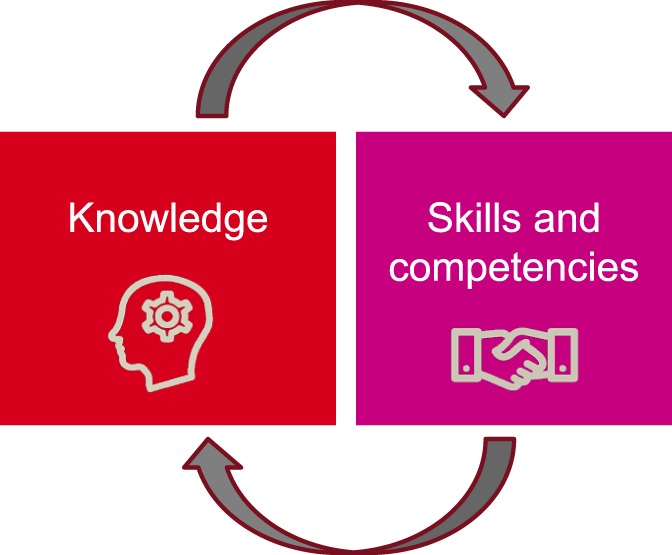
The educational model used to implement the IASP Pain Curriculum into the Macquarie DPT program, illustrating the synergistic relationship between the cyclical attainment of students' pain-related knowledge and clinical competencies.
2.3.3. Clinical education
Clinical education is embedded within 5 of the 6 semesters, encompassing over 1000 hours of traditional block clinical placements—in hospitals, community rehabilitation settings, and private practice. These include the HAWC program, as well as applied clinical education placements that are embedded within academic units covering topics such as workplace safety and sports. Students can observe clinical sessions at 3 high-quality multidisciplinary pain facilities in Sydney, as well as undertake clinical placements in pain management in their final year. This extensive clinical education program enables students to directly apply their new knowledge and develop clinical competencies in pain assessment and management throughout their training, starting with fundamental skills, and building to more advanced competencies by the end of the program.
2.3.4. Pain education tools
Two educational tools were developed to embed core concepts and a clinical model into the students' education, and applied across conditions and throughout the lifespan. These were developed in consultation with leading pain education specialists and clinicians at the Pain Management Research Institute at the Royal North Shore Hospital (Sydney) as well as an experienced Educational Designer and Developer at Macquarie University. The 2 tools are: (1) The Six Core Concepts of Pain (Fig. 3); and (2) The Clinical Model of Pain (Fig. 4). Students are introduced to these early in the DPT program, and they inform future learning at later stages of the curriculum.
Figure 3.
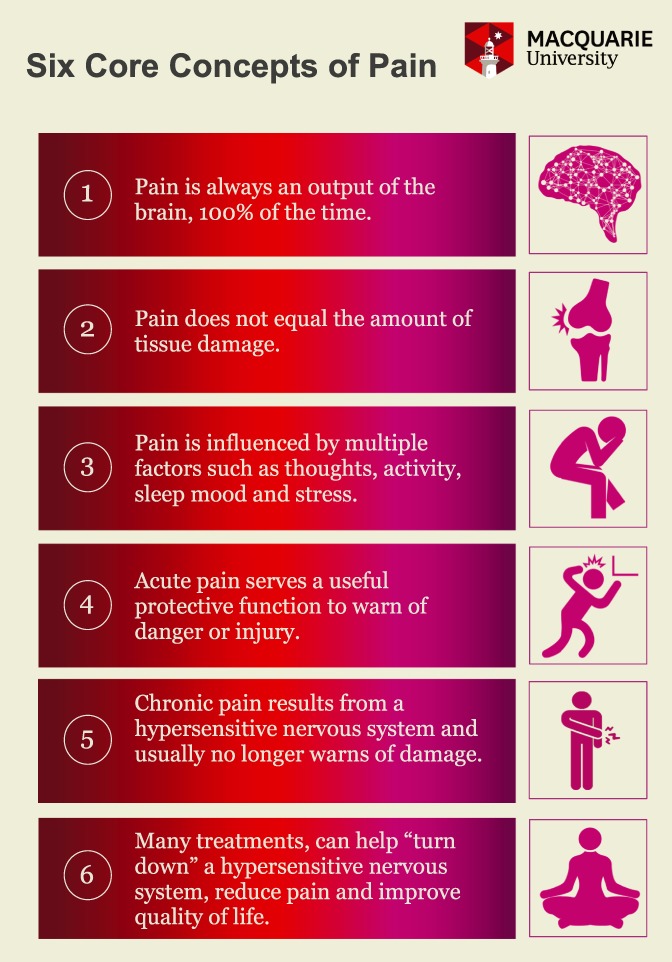
Macquarie University's Six Core Concepts of Pain education tool.
Figure 4.
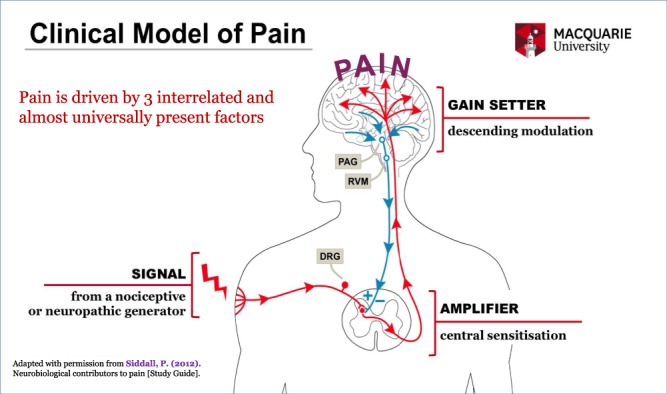
Macquarie University's Clinical Model of Pain education tool. DRG, dorsal root ganglion; PAG, periaqueductal gray; RVM, rostroventral medulla.
Throughout the DPT program, students have access to a variety of educational resources through an online Learning Management System, iLearn. This allows learning activities to be blended with a range of online resources to support their pain education. Resources include clinical simulation videos, research evidence, pain management tools, web sites, and assessment tools, including for people of different cultural backgrounds and across the lifespan. Many video resources (eg, explanation of the relevance of central sensitization to pain assessment or clinical simulation of providing pain education to patient, or assessing a patient with chronic pain) were developed specifically for the program with the assistance of experienced educational designers. In 2017, an additional educational resource was established for both students and staff: a dedicated pain education web site on Macquarie University's iLearn system, which enabled a central point of electronic access for the resources described above.
Resources and training were provided for staff as well, including orientation to the IASP pain curriculum and background information on pain education for health professionals, as well as the latest evidence and knowledge on clinical pain neuroscience. Staff were consulted individually to optimise integration of the IASP curriculum elements in each unit, and to ensure that the Six Core Concepts of Pain and Clinical Model of Pain were applied consistently.
2.3.5. Learning and teaching strategies
A blended learning approach was used to deliver the pain curriculum, including face-to-face lectures and tutorials, case-based learning, on-line activities, patient-simulation activities, clinical education, intensive workshops, and flipped classrooms. The lecture format was used to deliver core content across the 4 IASP curriculum domains. However, these were not purely didactic because the small student cohort size (60–65 students per year) allowed discussions during these face-to-face sessions.
In most units, weekly tutorials provided opportunities for students to apply their knowledge to clinical cases using problem-based learning methods, with an emphasis on the concurrent development of clinical reasoning skills and practical competencies. For example, in semester A, students learn skills in physiotherapy assessment and treatment, and develop basic clinical competencies by practising these skills in case-based activities in tutorials. This is supplemented by clinical application with the HAWC volunteers. In semester B, as the curriculum focuses on discipline-specific learning about musculoskeletal, cardiorespiratory, and neurological conditions, students extend their foundational competencies in the assessment and treatment of pain to specific patient populations or conditions (eg, low back pain, tendinopathies, and stroke). Tutorials involve small groups and experiential activities to consolidate fundamental concepts. For example, an appreciation of the influence of cognitions on pain experiences is gained through students analyzing their experiences from immersing their hands in iced water (as a noxious stimulus), while either attending to the experience or being distracted from it by listening to music.
The case-based learning methods allow students to use a clinical reasoning framework to identify the multidimensional contributors to an individual person's pain presentation, and to develop a person-centered intervention or treatment to address those factors. Critical evaluation of the evidence for pain management interventions is embedded in these activities.
Online activities are used to enhance the students' learning of the pain curriculum. These include: (1) learning to navigate important pain-related web sites (eg, the IASP web site15) to locate information such as the IASP pain taxonomy, classification, and clinical features of different pain conditions; (2) exploring the experiences of patients with pain (eg, receiving a diagnosis, having treatment, and using coping strategies such as pacing, dealing with flare-ups) from web sites such as Health Talk10; and (3) learning how to apply online resources in clinical practice from local pain-related organizations, such as Pain Australia,17 the New South Wales Agency for Clinical Innovation Pain Management Network web site,16 and painHEALTH6 from Western Australia.
Patient-simulation activities are included throughout the DPT pain curriculum. These include peer-based role plays with feedback from the educator and peers in tutorials and workshops, and engaging in online simulated patient cases. An example of the latter is the e-HAWC modules for students in second year to explore more complex chronic health conditions including chronic pain and mental health comorbidities. These online patient-simulation activities enhance the students' pain-related clinical competencies and improve their confidence before their block clinical education placements as well as providing useful reflective practice opportunities during and after their placements.
In the final year of the program, students complete a 1-day Advanced Pain Management workshop, designed to be their capstone pain education experience in the DPT program. Designed and delivered by the Macquarie DPT pain education leader (J.H.), the workshop is conducted in groups of 25 to 30 students, and is highly interactive. The focus is on developing clinical skills in more complex elements of pain management, such as case formulation, explaining pain to patients, and designing effective personalised pain management interventions, using chronic pain case vignettes. Students complete tasks in small groups, for example, to analyse principles and components of effective pain education, and role-play the delivery of tailored pain education with peer feedback. Students also explore novel and emerging pain therapies such as virtual reality, graded motor imagery, and brain stimulation techniques. An additional aim of the workshops is to deepen the students' understanding of complex pain conditions (eg, complex regional pain syndrome and fibromyalgia) and addressing the fourth domain of the IASP pain curriculum. Flipped classroom techniques are applied to address objectives for this domain, in which students research the evidence about chronic pain conditions and then present their clinical summaries to the whole group.
2.4. Evaluation methods
2.4.1. Assessment of students' knowledge
Assessment tasks throughout the DPT program have been designed to align with learning objectives. Pain-related knowledge was evaluated in multiple formats throughout the program. Students' knowledge specifically about pain neurobiology was formally evaluated using a validated questionnaire, the Neurophysiology of Pain Questionnaire (revised 13-item version, NPQ-R).2 The NPQ was devised to assess how an individual conceptualizes the biological mechanisms that underpin the experience of pain. Analysis of the psychometric properties of the instrument has demonstrated that it has acceptable construct validity, internal consistency, and test-retest reliability.2 The NPQ-R was administered at 3 time points: at the start and end of semester A, and in third year (semester E).
Assessments to evaluate the students' ability to apply pain-related knowledge to clinical practice include written assignments and clinical simulation examinations. In addition, written examinations provide assessment of more in-depth knowledge and application to hypothetical clinical cases.
2.4.2. Assessment of students' clinical skills and competencies
Clinical skills and competencies in the assessment and management of patients with painful conditions are primarily assessed during block clinical education placements by the clinical educators using the Assessment of Physiotherapy Practice tool, which has established reliability and validity3,4 and has been implemented across Australia. The validity of the APP tool has been investigated and Rasch analysis supports the interpretation that a student's APP score is an indication of their underlying level of professional competence in workplace practice.3 Furthermore, data collected from a total of 644 APP assessments provide a normative score for the student physiotherapy population of 76% (SD: 15).3
Students' skills are also evaluated informally during face-to-face teaching activities during tutorials and workshops, and formally in clinical simulation examinations. An additional assessment tool used throughout multiple units is the Mastery Checklist, in which peers and educators provide certification that a student has achieved a sufficient level of mastery of key-specific skills. The mastery system allows students to demonstrate evidence of clinical competencies across a range of skills within specific units, alongside skills assessed in a specific clinical context in clinical simulation examinations. These assessment approaches provide both formative and summative feedback to the students.
3. Results
3.1. Curriculum mapping
The 95 elements of the 2012 IASP Curriculum on Pain for Physical Therapy have been successfully embedded into the Macquarie DPT program. Each curriculum element has been explicitly mapped at the level of each unit and learning outcomes within units (Appendix 2: Macquarie DPT Pain Curriculum Mapping Chart, available online as supplemental digital content at http://links.lww.com/PR9/A15). After initial integration of the curriculum into the DPT program (from 2012 to 2014), iterative reviews have been conducted based on formal and informal feedback from teaching staff and students.
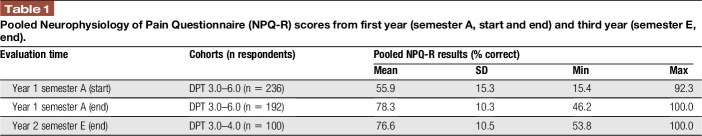
3.2. Pain neurobiology knowledge
The students' knowledge of pain neurobiology on entry into the DPT program was found to be consistently low: pooled data for 4 cohorts (n = 236) revealed a mean NPQ-R score of 56% (95% confidence interval [CI] 54–58). However, by the end of the first semester, the students' pain neurobiology knowledge had improved significantly, with a mean NPQ-R score of 78% (95% CI 76–80) from pooled data for 4 cohorts (n = 192), as shown in Table 1. This improvement in knowledge is maintained throughout the program, which is indicated by reassessment in third year, with mean NPQ-R score of 77% (95% CI 75–79) for the available data of 2 cohorts (n = 100) (Table 1). The change in NPQ-R scores from an individual cohort (DPT 3.0, 2014–2016) is illustrated in Figure 5.
Table 1.
Pooled Neurophysiology of Pain Questionnaire (NPQ-R) scores from first year (semester A, start and end) and third year (semester E, end).
Figure 5.
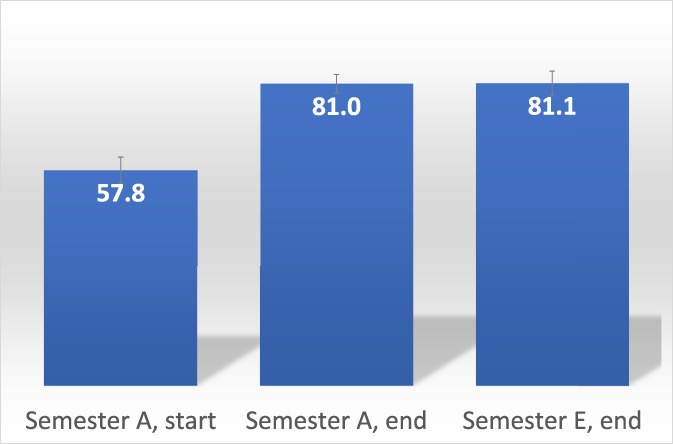
Neurophysiology of Pain Questionnaire (NPQ-R) scores from a single student cohort (DPT 3.0, 2014–2016), from first year (semester A) at the start (week 1) and end (week 12), and in third year (semester E). Scores presented as mean percentage correct with 95% confidence intervals.
3.3. Clinical skills and competencies
Overall, the first 100 DPT graduates demonstrated a high level of clinical skills and competencies, as indicated by the mean Assessment of Physiotherapy Practice tool mark of 78% (SD: 4). The students who completed a 5-week pain management clinical placement (n = 9) had a mean clinical performance score of 86% (SD: 6). This performance was 10% higher (95% CI 3–17) than the mean score of their peers who completed elective placements in nonpain management settings, and higher than normative scores of 76% (SD: 15) of Australian physiotherapy students on clinical placements.3 Moreover, feedback from the Clinical Educators about the students on these placements was very positive, including comments that they had an excellent understanding of the biopsychosocial model of pain, that they were able to build rapport well with patients and tailor their interventions well to each patient.
4. Discussion
It is generally agreed that pain education for future health professionals requires a comprehensive curriculum that is founded on a multidimensional understanding of the nature of pain9 and current scientific evidence, so that graduate clinicians are equipped with appropriate competencies to effectively help patients with pain. The IASP Pain Curricula provide such an educational framework.
In this article, we have described the design and development of a pre-licensure physical therapy program in which each of the 95 elements of the IASP Pain Curriculum for Physical Therapy has been prospectively and explicitly embedded, across a 3-year DPT program, and mapped at the level of specific units and learning outcomes. As far as the authors are aware, this is the first time this has been achieved in any pre-licensure physical therapy program. In other pre-licensure programs the IASP pain curriculum has been integrated at a single time-point (eg over 1 week) in the 2nd or 3rd year.22 However, we designed the content to be delivered throughout the 3-year program. This approach was adopted so that student education could be staged from more foundational to more advanced topics throughout their 3-year training. Advanced content included complex and chronic conditions, pain across the lifespan, and consideration of different cultural experiences of pain, including Australian Indigenous populations. Other pre-licensure programs have applied a similar approach to vertical integration of pain education, for example, in undergraduate medical training in the United States.21
We provide evidence that across the Macquarie DPT program, physical therapy students improve their knowledge about pain and also that they achieve a high level of clinical competencies in pain management. Although we will continue to evaluate the clinical outcomes of students and graduates of this program, it is hoped that the education provided to the first 3 Macquarie DPT graduate cohorts, and future graduands, will help to achieve the key educational goal of Australia's National Pain Strategy, which is “to increase the skill of health professionals through comprehensive education and training in evidence-based pain management.”18 We hope that this account will encourage others to adopt a similar model. We recognise that challenges exist in achieving this, with perhaps the most difficult being the redesign of an existing physical therapy program. In the case described in this article, a unique opportunity to prospectively integrate the curriculum into a new DPT program was used. Curriculum reviews, which occur regularly in educational programs, may provide future opportunities in existing physical therapy programs. Future research opportunities include qualitative studies to explore the experiences of academic staff, clinical educators, and students with pain education curricula. A further challenge is ensuring that faculty and other teaching staff have adequate knowledge and skills to teach the pain curriculum. Provision of training and resources to upskill teachers is critical to address this need. At the time of this publication, all IASP pain curricula have been revised and updated to align with the 2018 IASP Global Year on Excellence in Pain Education.
5. Conclusions
Pain education for health professionals can be integrated into pre-licensure university programs using the IASP Pain Curricula. This approach addresses current educational recommendations from national and international pain authorities and will help to transform the future of our health care workforce to competently manage patients suffering from pain.
Disclosures
The authors have no conflict of interest to declare.
Acknowledgements
The authors acknowledge Professor Phillip Siddall (Sydney Medical School—Northern, University of Sydney, and Department of Pain Management, HammondCare, Greenwich Hospital, Sydney) for generously allowing them to use and adapt his clinical model of pain for teaching purposes in this program. The authors are also grateful to Educational Designer and Developer Ms. Sherrie Love (Macquarie University) for her assistance with the design of the graphics for the Six Core Concepts of Pain and the Clinical Model of Pain.
Appendix A. Supplemental digital content. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A15.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
References
- [1].Bement MKH, Sluka KA. The current state of physical therapy pain curricula in the United States: a faculty survey. J Pain 2015;16:144–52. [DOI] [PubMed] [Google Scholar]
- [2].Catley MJ, O'Connell NE, Moseley GL. How good is the Neurophysiology of Pain Questionnaire? A Rasch analysis of psychometric properties. J Pain 2013;14:818–27. [DOI] [PubMed] [Google Scholar]
- [3].Dalton M, Davidson M, Keating J. The assessment of physiotherapy practice (APP) is a valid measure of professional competence of physiotherapy students: a cross-sectional study with Rasch analysis. J Physiother 2011;57:239–46. [DOI] [PubMed] [Google Scholar]
- [4].Dalton M, Davidson M, Keating JL. The assessment of physiotherapy practice (APP) is a reliable measure of professional competence of physiotherapy students: a reliability study. J Physiother 2012;58:49–56. [DOI] [PubMed] [Google Scholar]
- [5].Dean CM, Duncan PW. Preparing the next generation of physical therapists for transformative practice and population management: an example from Macquarie University Phys Ther 2016;23: 272–4. [DOI] [PubMed] [Google Scholar]
- [6].Department of Health Government of Western Australia. painHEALTH: easing musculoskeletal pain. Available at: https://painhealth.csse.uwa.edu.au/. Accessed December 6, 2017.
- [7].Doorenbos AZ, Gordon DB, Tauben D, Palisoc J, Drangsholt M, Lindhorst T, Danielson J, Spector J, Ballweg R, Vorvick L. A blueprint of pain curriculum across prelicensure health sciences programs: one NIH pain consortium center of excellence in pain education (CoEPE) experience. J Pain 2013;14:1533–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Engel GL. The biopsychosocial model and the education of health professionals. Ann N Y Acad Sci 1978;310:169–81. [DOI] [PubMed] [Google Scholar]
- [9].Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. PAIN 2017;158(suppl 1):S11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Health Talk, Oxford University. Available at: http://www.healthtalk.org/. Accessed December 6, 2017.
- [11].Hoeger Bement MK, St Marie BS, Nordstrom TM, Christensen N, Mongoven JM, Koebner IJ, Fishman SM, Sluka KA. An interprofessional consensus of core competencies for prelicensure education in pain management: curriculum application for physical therapy. Phys Ther 2014;94:451–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hush JM, Stanton TR, Siddall P, Marcuzzi A, Attal N. Untangling nociceptive, neuropathic and neuroplastic mechanisms underlying the biological domain of back pain. Pain Manag 2013;3:1–14. [DOI] [PubMed] [Google Scholar]
- [13].International Association for the Study of Pain: IASP pain curricula. Available at: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2055. Accessed December 6, 2017.
- [14].Institute of Medicine. Relieving pain in America. Washington, DC: The National Academies, 2011. [Google Scholar]
- [15].International Association for the Study of Pain. IASP taxonomy. Available at: https://www.iasp-pain.org/Taxonomy. Accessed December 6, 2017.
- [16].New South Wales Agency for Clinical innovation: ACI pain management Network. Available at: https://www.aci.health.nsw.gov.au/chronic-pain. Accessed December 6, 2017. [DOI] [PubMed]
- [17].PainAustralia. Available at: http://www.painaustralia.org.au/.
- [18].PainAustralia. National pain strategy. Available at: http://www.painaustralia.org.au/improving-policy/national-pain-strategy. Accessed December 6, 2017.
- [19].Pizzo PA, Clark NM. Alleviating suffering 101–pain relief in the United States. N Engl J Med 2012;366:197–9. [DOI] [PubMed] [Google Scholar]
- [20].Scudds RJ, Scudds RA, Simmonds MJ. Pain in the physical therapy (PT) curriculum: a faculty survey. Physiother Theory Pract 2001;17:239–56. [Google Scholar]
- [21].Tauben DJ, Loeser JD. Pain education at the University of Washington School of Medicine. J Pain 2013;14:431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Watt-Watson J, Hunter J, Pennefather P, Librach L, Raman-Wilms L, Schreiber M, Lax L, Stinson J, Dao T, Gordon A. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. PAIN 2004;110:140–8. [DOI] [PubMed] [Google Scholar]
- [23].Watt-Watson J, McGillion M, Hunter J, Choiniere M, Clark A, Dewar A, Johnston C, Lynch M, Morley-Forster P, Moulin D. A survey of prelicensure pain curricula in health science faculties in Canadian universities. Pain Res Manag 2009;14:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].World Health Organisation. International classification of functioning, disability and health: ICF: World Health Organization, 2001. http://www.who.int/classifications/icf/en/. Accessed December 6, 2017. [Google Scholar]