Abstract
We aimed to evaluate HIV prevalence among residents of Liangshan Prefecture through HIV sentinel surveillance (HSS) data over the period from 2010 to 2016, and investigate risk factors for HIV infection in this population and interactions among them.
Two sites (Dechang and Ningnan counties) with majority-Han populations, and 1 site (Butuo) with a majority-Yi population were selected. We used questionnaires to investigate residents’ demographic and behavioral characteristics from 2010 to 2016, and performed HIV testing. Multivariate logistic regression and path analysis were undertaken to investigate the interactions and mediating effects among significant risk factors for HIV infection.
A total of 5403 community residents in the Yi area and 10,897 community residents in the Han areas were enrolled. HIV prevalence in the Yi area was consistently high, ranging from 9.46% (63/666, 2011) to 2.88% (23/798, 2012) over the period from 2010 to 2016. HIV prevalence in the Han areas ranged from 0.15% (2/1333, 2010) to 0.44% (7/1604, 2011) over the same period. Multivariate logistic regression showed that unprotected casual sexual behavior, male gender, illiteracy, drug use, and injection drug use were positively associated with HIV infection risk in the Yi area. Path analysis of the risk factors revealed that casual sexual behavior (0.051) and injection drug use (0.161) were directly associated with HIV infection. However, marital status (0.004), ethnicity (0.017), education level (−0.004), HIV/AIDS-related prevention knowledge (−0.012), and drug use (0.11) had an indirect influence on HIV infection through casual sexual behavior and injection drug use.
The prevalence of HIV is high among residents of majority-Yi areas, and injection drug use and casual sexual behavior are risk factors for infection.
Keywords: community residents, ethnic minority region, HIV, Yi people
1. Introduction
Liangshan Prefecture is home to more people of Yi ethnicity than any other area in China. It is located in southwest China, and approximately 50% of its residents are of Yi ethnicity. The first HIV case in Liangshan Prefecture was reported in 1995, an injecting drug user (IDU). Since then, the local incidence of HIV infection has greatly increased. Until December 2015, the cumulative number of HIV/AIDS cases in this area was reported to be 29,987, and Liangshan Prefecture has the highest HIV prevalence rate in Sichuan Province.[1,2] Previous studies have shown that the high prevalence of HIV is due in part to injected drug use in the last 2 decades.[3] The epidemic trend of HIV has gradually changed, and sex transmission is now the main reason of HIV infection in Liangshan Prefecture, and it has spread from IDUs to the general population.[2]
HIV sentinel surveillance (HSS) is an important method for monitoring HIV prevalence and trends among particular populations, such as men who IDUs, have sex with men (MSM), female sex workers, pregnant women, and community residents. HSS of unmarried youth in rural areas of Liangshan Prefecture was first conducted in 2010. Community residents are a key population to target for HIV prevention, and HSS for this population is critical for developing effective strategies to prevent AIDS epidemic.
Previously we observed that HIV incidence in clinical patients increased between 2011 and 2013 in Liangshan Prefecture, and that Yi people accounted for more than 85% of new HIV infections.[2,4] HSS for community residents has been implemented at 3 HSS sites in Liangshan Prefecture since 2009. In this study, we evaluate HIV prevalence among community residents of Liangshan Prefecture through HSS data over the period from 2010 to 2016, and investigate risk factors for HIV infection in this population and their interactions.
2. Methods
2.1. Ethics
All subjects voluntary participated in our study and signed informed consent forms before enrollment. This study was approved by the ethics committee of the Liangshan Yi Autonomous Prefecture Center for Disease Control and Prevention (CDC), and the study was carried out in accordance with the Helsinki Declaration of 1964.
2.2. HSS site selection
HSS sites in Liangshan Prefecture were selected to be representative of the prefecture's HIV epidemic, based on data analysis by the Chinese CDC and the Sichuan CDC.[5] Multistage stratified random sampling was used to acquire the study sample. First, 3 counties were selected from among Liangshan Prefecture's 17 counties. Two sites (Dechang and Ningnan counties) both have majority-Han populations, and 1 site (Butuo) was selected to be representative of a majority-Yi area in the prefecture. Second, all towns in each of the selected counties were rated as having mild, moderate, or severe HIV/AIDS prevalence. One town each was randomly selected for further analysis from among the towns with mild and severe HIV/AIDS prevalence, and 2 towns were randomly selected from among those with moderate prevalence, for a total of 4 towns in each surveillance county. Two hundred community residents were randomly enrolled within each selected town. A total of 800 people in the 3 supervised counties were enrolled each year.
2.3. Questionnaire
The questionnaire was designed by the STD and AIDS centers for disease control of the Chinese CDC and Sichuan CDC. All HSS data were collected by the Liangshan Yi Autonomous Prefecture CDC which had approval to analyze and publish the HSS data.
The questionnaire was 2 pages long, and included questions about demographic characteristics, HIV-related prevention knowledge, and behavioral characteristics. The demographic characteristics included sex, age, ethnicity, education level, and marital status. HIV-related prevention knowledge was assessed with 8 items, each expressed with a 2-point Likert scale of 0 (no) to 1 (yes). A total score of ≥5 of the 8 items was considered to indicate awareness of HIV-related prevention principles; otherwise, the patient was regarded as unaware. The behavioral characteristics included drug use, injection drug use, casual sexual behavior in the past year, and high-risk casual sexual behavior. High-risk sexual behaviors were defined as casual sexual behaviors without consistent condom use.
The questionnaire was administered along with an introduction to the study's purpose. Study participants remained anonymous, and the questionnaire was administered by trained investigators in face-to-face interviews.
2.4. HIV testing
Before the interview, each participant provided 3 to 5 mL of venous blood for HIV testing. Specimens were tested for HIV antibodies at the Liangshan Prefecture CDC. Enzyme-linked immunosorbent assay (ELISA) was used to screen for HIV antibodies. Negative ELISA results indicated no HIV infection, while those with positive results were re-tested for HIV antibodies by Western blot with either different reagents or reagents from a different manufacturer. If the second test was positive, the serum was confirmed as positive for HIV antibodies. If negative, the serum was regarded as negative for HIV antibodies.[6]
2.5. Statistical analysis
Demographic characteristics, HIV-related prevention knowledge, and behavioral characteristics were expressed as frequencies and percentages. The categorical variables of the investigated groups were compared using the Pearson chi-square (χ2) or Fisher's exact test. Three multivariate logistic regression models were constructed to identify risk factors potentially related to HIV infection, drug use behaviors, and high-risk casual sexual behaviors, in which the independent variables were demographic information, HIV-related prevention knowledge, and behavioral characteristics over the period from 2010 to 2016. The results were reported as odds ratios (ORs) and 95% confidence intervals (CIs).
Second, path analysis using a structural equation modeling (SEM) framework was conducted to investigate the interactions and mediating effects among significant risk factors for HIV infection, based on the results of the logistic regression analyses. The quality of the models was estimated using the normed chi-square (χ2/df), comparative fit index (CFI), Tucker–Lewis index (TLI), and root mean square error of approximation (RSMEA). A model was considered to be a very good fit when CFI>0.95, AGFI>0.95, and RSMEA<0.05. A model was regarded as adequate when CFI>0.95, AGFI>0.95, and RSMEA<0.10. Statistical analyses were performed using SPSS version 21.0 for Windows (SPSS Inc., Chicago, IL) and IBM SPSS Amos 17.0 (SPSS Inc., Chicago, IL). The cutoff for statistical significance was set at P<.05.
3. Results
3.1. Characteristics of the studied population
A total of 5403 community residents in the majority-Yi area and 10,897 community residents in majority-Han areas were enrolled from 2010 to 2016, and all subjects received HIV testing. HIV prevalence in residents of the Han areas was as low as 0.15% (2/1333, 2010) and varied by year, peaking at 0.44% (7/1604) in 2011. The temporal variation was not significant (χ2trend = 0.03, P = .86) (Fig. 1). In the Yi area, HIV prevalence reached a peak of 9.46% (63/666) in 2011, up from 8.72% (67/768) in 2010. It remained relatively high and ranged between 2.88% (23/798, 2012) and 3.77% (30/795, 2013) from 2012 to 2016. The temporal variation in HIV prevalence for this area was significant (Fig. 1).
Figure 1.
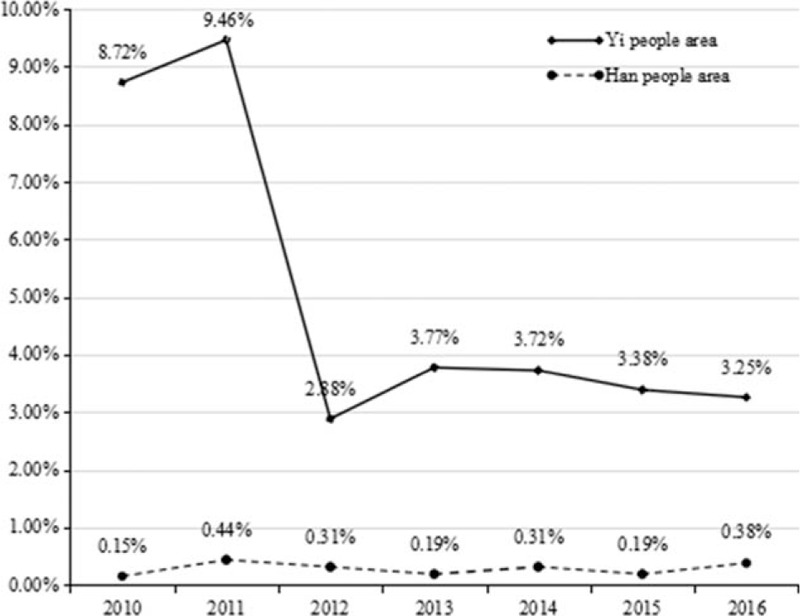
Prevalence of HIV in Yi and Han areas. HIV = human immunodeficiency virus.
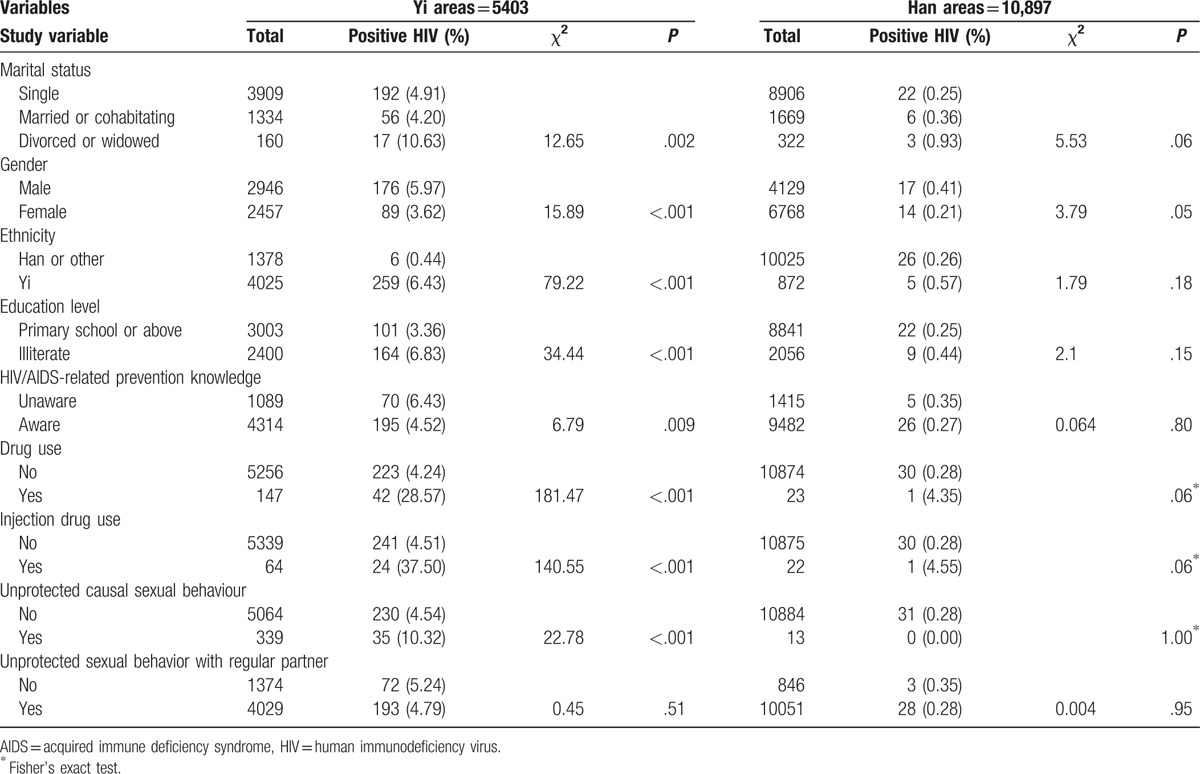
Among the residents of the Yi area, we observed that HIV infection rates varied significantly among subjects of different marital status, gender, ethnicity, education levels, HIV/AIDS-related prevention knowledge, drug use and injection drug use, and unprotected casual sexual behavior (Table 1). However, HIV infection rates did not differ significantly with these factors among residents of the Han areas.
Table 1.
The demographic characteristics and HIV infection rate among community residents.
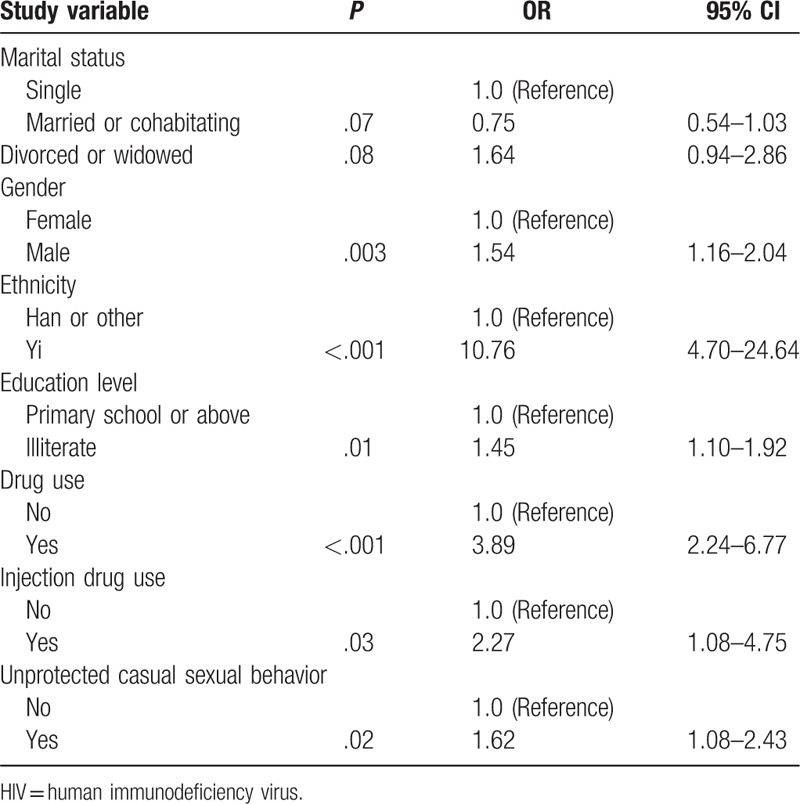
3.2. Risk factor analysis for HIV infection in Yi areas
Based on our comparison of HIV infection rates in Yi and Han areas, we only performed multivariate logistic regression analysis for residents of the Yi area (Table 2). Significantly higher HIV risk was observed in community residents of Yi ethnicity (OR = 10.76, 95% CI = 4.70–24.64), those who reported engaging in unprotected casual sexual behavior (OR = 1.62, 95% CI = 1.08–2.43), males (OR = 1.54, 95% CI = 1.16–2.04), those who were illiterate (OR = 10.76, 95% CI = 4.70–24.64), drug users (OR = 3.89, 95% CI = 2.24–6.77), and injection drug users (OR = 2.27, 95% CI = 1.08–4.75).
Table 2.
Logistic regression analysis of factors associated with HIV infection.
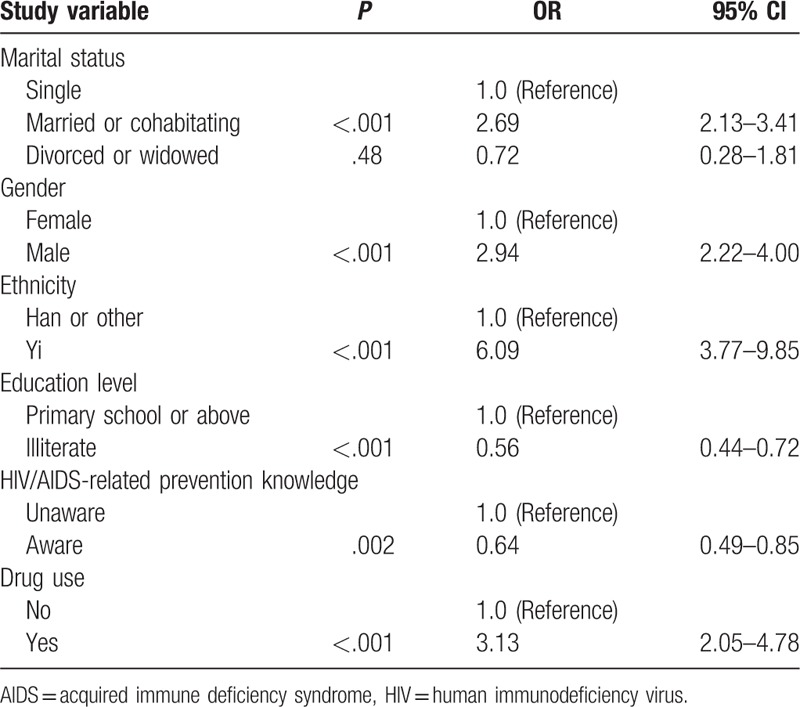
We found that marriage or cohabitation (OR = 2.69, 95% CI = 2.13–3.41), male gender (OR = 2.94, 95% CI = 2.22–4.00), Yi ethnicity (OR = 6.09, 95% CI = 3.77–9.85), and drug use (OR = 3.13, 95%CI = 2.05–4.78) were significantly associated with high likelihood of unprotected casual sexual behavior (Table 3), while illiteracy (OR = 0.56, 95% CI = 0.44–0.72) and awareness of HIV/AIDS-related prevention knowledge (OR = 0.64, 95% CI = 0.49–0.85) were associated with low likelihood of unprotected casual sexual behavior.
Table 3.
Logistic regression analysis of factors associated with unprotected casual sexual behavior.
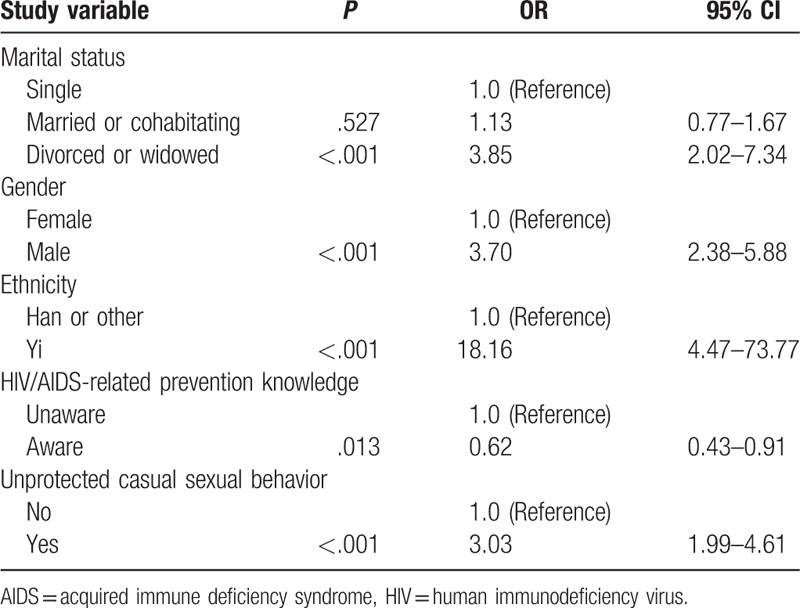
We observed that divorced or widowed status (OR = 3.85, 95% CI = 2.02–7.34), male gender (OR = 3.70, 95% CI = 2.38–5.88), Yi ethnicity (OR = 18.16, 95% CI = 4.47–73.77), and unprotected casual sexual behavior (OR = 3.03, 95% CI = 1.99–4.61) were significantly associated with drug use, while awareness of HIV/AIDS-related prevention principles (OR = 0.62, 95% CI = 0.43–0.91) was significantly negatively correlated with drug use (Table 4).
Table 4.
Logistic regression analysis of factors associated with drug use.
3.3. Final path model
We used path analysis to investigate interactions among risk factors for HIV infection, as identified by multivariate logistic regression: ethnicity, casual sexual behavior, drug use, injection drug use, education, and HIV/AIDS-related prevention knowledge, with these factors considered as covariates in the path model (Fig. 1). All regression weights of these factors were statistically significant (P < .001). The goodness of fit indices for this model were as follows: χ2 = 186.256; df = 14; CFI = 0.966, AGFI = 0.991, and RMSEA = 0.048—meaning that the model was a very good fit.
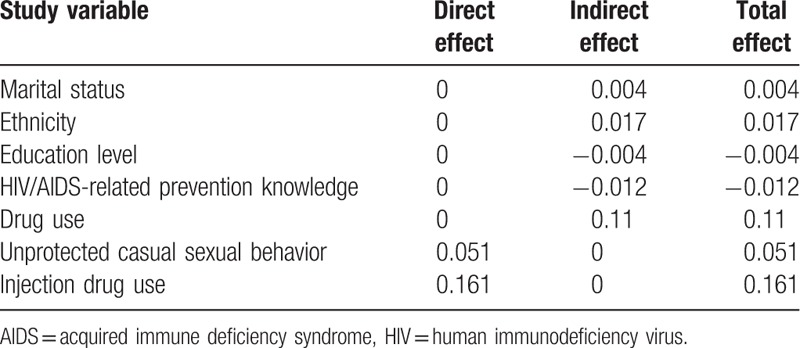
An arrow between 2 dimensions in Figure 2 indicates a direct relationship. Total effects are equal to the sum of direct and indirect effects. Casual sexual behavior (0.051) and injection drug use (0.161) were the only factors directly associated with HIV infection (Table 5). However, marital status (0.004), ethnicity (0.017), education level (−0.004), HIV/AIDS-related prevention knowledge (−0.012), and drug use (0.11) each indirect influenced HIV infection risk through casual sexual behavior and injection drug use.
Figure 2.
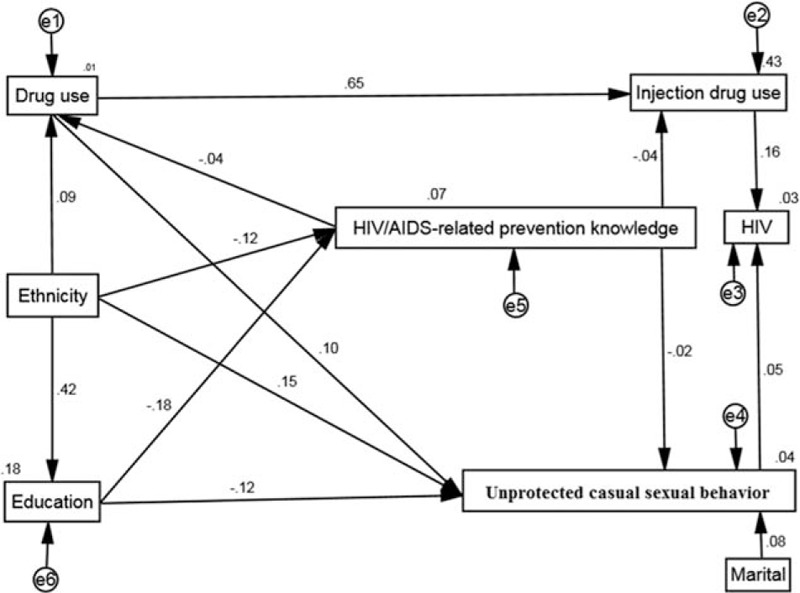
Path model predicting HIV risk factors among a sample of residents of a majority-Yi area (N = 5403). HIV = human immunodeficiency virus.
Table 5.
Factors affecting HIV infection in a Yi-majority area.
4. Discussion
Our study found that the prevalence of HIV in residents of a majority-Yi area (2.88%–9.46%) was much higher than the average rate in China (0.04%, 501,000/1,367,820,000) as of the end of 2014.[7] We found that HIV infection in this area peaked during 2010 and 2011, but sharply decreased after 2012. The main reason may be that the HSS for community residents started in 2010, and many previous infections were detected for the first time in 2010 and 2011, resulting in an apparently high HIV infection rate in those 2 years. Our previous study reported a similar change in the HIV infection rate detected through HSS begun in 2010 for unmarried Yi youth in Liangshan Prefecture.[8]
Our path analysis showed that drug use still plays a prominent role in HIV infection, with a total effect of over 16%—especially through the indirect effect of needle sharing. Liangshan Prefecture has a long history of opium cultivation and opium/heroin trade due to its location.[9] The prevalence of HIV-1 infection in the twentieth century in Liangshan Prefecture is primarily attributed to IDU.[10] Three factors contribute to the relatively high likelihood of Yi people's engaging in high-risk needle sharing: Sharing is an integral part of traditional Yi culture, leading drug users to share both drugs and needles; many Yi people are illiterate, and thus may lack knowledge about the importance of needle exchange[11]; and Yi people are concentrated in remote and impoverished areas where needle sharing may be seen as an effective way to reduce costs.
Another risk factor identified by our analysis was unprotected casual sexual behavior. The sexual mores of Yi people are different from those of Han people,[12] and the attitudes of unmarried and male Yi people toward sexual behaviors are relatively liberal.[13,14] In our previous study, we found that 41.4% of young, unmarried Yi people had engaged in unprotected causal sexual behaviors.[14] Yang et al[13] reported that more than 30% of Yi people hold permissive attitudes toward extramarital sexual behavior and premarital sexual behavior before and after cohabitating, and about 66.7% of Yi study participants had had multiple sexual partners in the last year. Moreover, Yi people traditionally have a negative attitude toward condom use, as condoms are distrusted and regarded as a means of birth control.[15] The traditional Yi concept of “the more babies you raise, the luckier you will be” strengthens this population's negative attitude toward condoms.[15] In addition, the high rate of poverty makes condoms difficult to obtain for some people.[16] Casual sexual behavior is common among Yi people, but the main problem is inconsistent use of condoms rather than the casual sexual behavior itself.[17]
Our study revealed that Yi ethnicity was significantly associated with casual sexual behavior, drug use, and low HIV/AIDS-related prevention knowledge. The high rate of poverty in Yi areas limits residents’ opportunities to change their current situation,[18] with factors such as lack of skills, unemployment, low education level, and social discrimination increasing the likelihood they will engage in high risk behaviors such as drug dealing, selling blood, and commercial sexual services.[19–22] Therefore, remedying poverty and targeting attitudes toward sexual behaviors and condoms might be potential measures for HIV prevention in this area.
Individuals with lower education levels tend to engage in high-risk sexual behaviors, and are at higher risk of being infected with HIV.[20,23] In our previous study, we found the illiteracy rate was as high as 61.3% among newly infected people in Liangshan Prefecture,[2] which is similar to our current results [the illiteracy rate of HIV-infected individuals in Yi areas was 61.9% (164/101)]. The low education level would result in lack of knowledge and misperceptions about the importance of condom use and self-protection, as well as lack of communication skills.[21] Moreover, education is closely correlated with economic status, which influences high-risk behaviors as described above.[24]
In addition, we found that HIV/AIDS-related prevention knowledge was slightly associated with injection drug use and unprotected casual sexual behaviors. Increased HIV/AIDS-related prevention knowledge may be associated with HIV/AIDS prevention attitudes, and thus to potentially safer sexual decision-making and behaviors.[25] Previous studies have reported that lack of HIV/AIDS-related prevention knowledge is associated with greater likelihood of premarital sex, extramarital sex, history of sexually transmitted diseases, and drug use.[26]
Two limitations of our study should be noted. First, this was a cross-sectional study, so the exploratory variables and turnover intention were measured simultaneously, and we could not obtain any information on how these associations changed over time. Second, although the questionnaire used in our study was anonymous, respondents may have concealed the truth about sensitive questions about sexual behaviors and drug use. Therefore, reporting bias could not be ruled out.
Our results suggest that the prevalence of HIV is very serious among residents of majority-Yi areas. Injection drug use was strongly associated with HIV infection, and casual sexual behavior was moderately correlated with HIV infection. In addition, marital status, ethnicity, education level, HIV/AIDS-related prevention knowledge, and drug use each indirectly influenced HIV infection through casual sexual behavior and injection drug use.
Acknowledgment
We thank Shawna Williams to help polish the English of this manuscript.
Author contributions
Data curation: GY, LX, QL, RP, SY.
Formal analysis: SY, WZ.
Funding acquisition: SY.
Investigation: JW, KW, SY.
Methodology: SY.
Project administration: CJ, QL, SY, YG.
Resources: SY.
Software: SY.
Supervision: BG, DL, LN, QW, SY.
Validation: SY.
Writing—original draft: SY.
Writing—review and editing: SY.
Footnotes
Abbreviations: χ2/df = normed chi-square, CDC = disease control and prevention, CFI = comparative fit index, CIs = confidence intervals, ELISA = enzyme-linked immunosorbent assay, HIV/AIDS = human immunodeficiency virus/acquired immune deficiency syndrome, HIV = human immunodeficiency virus, HSS = HIV sentinel surveillance, IDU = injecting drug user, ORs = odds ratios, RSMEA = root mean-square error of approximation, SEM = structural equation modeling, STD = sexually transmitted disease, TLI = Tucker–Lewis index.
SY and WZ contribute equally to this study.
Funding: This research was supported by grant funding from the National Natural Science Foundation of China (81703279); Liangshan AIDS/HIV prevention project (H170614; H161236); the research project of Health and Family Planning Commission of Sichuan Province (16PJ259).
The authors have no conflicts of interest to disclose.
References
- [1].Li L, Wei D, Hsu WL, et al. CRF07_BC strain dominates the HIV-1 epidemic in injection drug users in Liangshan Prefecture of Sichuan, China. AIDS Res Hum Retroviruses 2015;31:479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhao QG, Gong YH, Liao Q, et al. [Estimation on the HIV-1 incidence in Liangshan Yi Autonomous Prefecture, under BED-capture enzyme immunoassay, from 2011 to 2013]. Zhonghua Liu Xing Bing Xue Za Zhi 2016;37:1105–7. [DOI] [PubMed] [Google Scholar]
- [3].Wu Z. Recent trends of injecting drug use and related HIV infection in China. Global Research Network Meeting on HIV Prevention in Drug-Using Populations: Inauguration Meeting Report National Institute on Drug Abuse, Geneva, Switzerland. Geneva, 1999. [Google Scholar]
- [4].Jike CN, Yang SJ, Yu G, et al. Analysis of HIV related high risk behaviors and factors maternal AIDS sentinel surveillance in Liangshan Prefecture between 2009 and 2015. Chin J AIDS STD 2017;23:1019–22. [Google Scholar]
- [5].Wang L, Wang L, Ding ZW, et al. HIV prevalence among populations at risk, using sentinel surveillance data from 1995 to 2009 in China. Chin J Epidemiol 2011;32:20–4. [PubMed] [Google Scholar]
- [6].Zhang SH, Luo M, Yang SJ, et al. HIV-infection related behaivors and preventive measures among unmarried youths from the rural areas in Liangshan Prefecture, 2011–2013. Chin J Epidemiol 2017;38:486–90. [DOI] [PubMed] [Google Scholar]
- [7].National Health and Family Planning Commission of the People's Republic of China. 2015 China AIDS Response Progress Report.UNAIDS, Beijing: 2015. http://www.unaids.org.cn/pics/20160614144959.pdf. [Google Scholar]
- [8].Yu G, Yang SJ, Wang QX, et al. Analysis of HIV sentinel surveillance among unmarried youth from rural areas in Liangshan Prefecture. Mod Prev Med 2017;44:2259–63. [Google Scholar]
- [9].Zhou YiBiao, Liang Song, Wang QiXing, et al. The geographic distribution patterns of HIV-, HCV- and co-infections among drug users in a national methadone maintenance treatment program in Southwest China. BMC Infect Dis 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yang C, Latkin C, Luan R, et al. HIV, syphilis, hepatitis C and risk behaviours among commercial sex male clients in Sichuan province, China. Sex Transm Infect 2010;86:559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Zhang SH, Luo M, Yang SJ, et al. Analysis of HIV infection related behaviors among unmarried youth from rural areas in Liangshan Prefecture and effective factors, 2011–2013. Chin J Epidemiol 2017;38:486–90. [DOI] [PubMed] [Google Scholar]
- [12].Yang SJ, Luo M, Zhang SH, et al. Overview on culture and customs related to AIDS epidemic and prevention among Yi people in Liangshan. Chin J AIDS STD 2017;23:271–2. [Google Scholar]
- [13].Yang Y, Wu CL, Liu P, et al. Analysis of an investigation of casual sexual behaviors among Yi Ethnic villagers in one county in Liangshan of Sichuan Province. Med Soc 2011;24:41–4. [Google Scholar]
- [14].Zhang SH, Luo M, Yang SJ, et al. HIV-infection related behaviors and preventive measures among unmarried youths from the rural areas in Liangshan Prefecture, 2011–2013. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:486–90. [DOI] [PubMed] [Google Scholar]
- [15].Zhou RN. Transmission, control and prevention of AIDS in ethnic regions—Taking HIV/AIDS and local cultural survey in Liangshan Yi area as an example. 2012. Journal of Nanjing Medical University (Social Science) 2012;12:11–7. [Google Scholar]
- [16].Wang S, DK Developing an innovative cross-cultural strategy to promote HIV/AIDS prevention in different ethnic cultural groups of China. AIDS Care 2005;17:874–91. [DOI] [PubMed] [Google Scholar]
- [17].Yang Yi, Luan RongSheng, Liu Peng, et al. Casual sex and concurrent sexual partnerships among young people from an Yi community with a high prevalence of HIV in China. Asian Journal of Andrology 2012;14:758–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bureau of Statistics of Liangshan prefecture; the National Bureau of Investigation Team in Liangshan prefecture. Statistical Report on National Economy and Social Development in 2015 of Liangshan Prefecture. 2016. Available at: http://tjj.lsz.gov.cn/index.php/Article/View/cid/39/id/285.html [Accessed March 22, 2018] [Google Scholar]
- [19].Piot P, Greener R, Russell S. Squaring the circle: AIDS, poverty, and human development. PLoS Med Oct 2007;4:1571–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Allen CF, Simon Y, Edwards J, et al. Factors associated with condom use: economic security and positive prevention among people living with HIV/AIDS in the Caribbean. AIDS Care 2010;22:1386–94. [DOI] [PubMed] [Google Scholar]
- [21].Davidoff-Gore A, Luke N, Wawire S. Dimensions of poverty and inconsistent condom use among youth in urban Kenya. AIDS Care 2011;23:1282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Jennings L, Mathai M, Linnemayr S, et al. Economic context and HIV vulnerability in adolescents and young adults living in urban slums in Kenya: a qualitative analysis based on scarcity theory. AIDS Behav 2017;21:2784–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Greener R, Sarkar S. Risk and vulnerability: do socioeconomic factors influence the risk of acquiring HIV in Asia? AIDS Behav 2010;24suppl 3:S3–11. [DOI] [PubMed] [Google Scholar]
- [24].Chen YH, McFarland W, Raymond HF. Behavioral surveillance of heterosexual exchange-sex partnerships in San Francisco: context, predictors and implications. AIDS Behav Jan 2011;15:236–42. [DOI] [PubMed] [Google Scholar]
- [25].Nabunya P, Ssewamala FM, Mukasa MN, et al. Peer mentorship program on HIV/AIDS knowledge, beliefs, and prevention attitudes among orphaned adolescents: an evidence based practice. Vulnerable Child Youth Stud 2015;10:345–56. [PMC free article] [PubMed] [Google Scholar]
- [26].Song Y, Kang D, Wang G, et al. HIV/AIDS-related knowledge and behaviors among rural married migrant women in Shandong Province, China: a comparison study. Arch Sex Behav 2015;44:367–74. [DOI] [PubMed] [Google Scholar]


