Abstract
Background:
This systematic review and meta-analysis aimed to identify whether there is any relationship between fixed orthodontic appliances and malodor, and if self-ligating brackets (SLBs) prevent malodor better than conventional brackets (CBs).
Methods:
The electronic databases PubMed, Ovid, EMBASE, and the Cochrane Library were searched from inception to September 2016; a manual search was also performed. Randomized controlled and clinical controlled trials, in which experimental groups received fixed orthodontic therapy and malodor was measured, were included. Patients treated with fixed orthodontic brackets were compared with those without any treatment, and SLB systems were compared with CB systems. Two reviewers independently selected potentially relevant studies, evaluated the risk for bias, extracted essential data, and synthesized findings using Review Manager version 5.3 (Copenhagen: The. Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Results:
Four studies, involving a total of 152 participants, met the inclusion criteria. Fixed orthodontic appliances caused malodor from the initial visit to 2 to 3 months, but was only significant after the first week (mean difference 20.24 [95% confidence interval [CI]11.75–28.74]; P < .00001). Plaque index, gingival index, and periodontal pocket depths demonstrated no statistical differences between the SLB and CB groups after the first week. However, SLBs significantly controlled malodor better than CBs after the first week (mean difference 4.32 [95% CI 6.02 to 2.61]; P < .00001). The quality of the included studies was relatively low and relevant research in this field is quite scarce.
Conclusions:
Although the evidence base was relatively weak, fixed orthodontic treatment appeared to be a risk factor for malodor, independent of periodontal changes, and SLB systems controlled malodor better than CB systems.
Keywords: meta-analysis, oral malodor, orthodontics, self-ligating brackets
1. Introduction
Foul breath and/or discernible smell originating from the oral cavity is frequently defined as halitosis, which affects 50% of the population.[1] It has been reported that 80% to 90% of the bad breath cases are due to problems in the oral cavity, thus known as oral malodor.[2] It is regarded to be a negative element in one's self-image and affects more aspects of daily life than social relations alone.[3] Researchers have suggested that oral malodor is primarily caused by volatile sulfur compounds produced by microbial metabolism within the saliva, dental plaque, tongue dorsum, and periodontal pockets.[4–7] However, whether there is a definite correlation between plaque index (PI) and oral malodor remains controversial.[8]
One of the risk factors for dental plaque accumulation and periodontal problems is malocclusion. It is broadly recognized that orthodontic treatment of malocclusion facilitates favorable conditions to maintain oral hygiene.[9] However, during the treatment period, fixed brackets, archwires, and other components hamper oral hygiene measurements, thus enhancing plaque attachment, or even lead to gingival inflammation or periodontitis.[9,10]
Recently, some investigators have reported that fixed orthodontic appliances can increase oral malodor,[11,12] and that oral malodor should be regarded as one of potential side effects of orthodontic treatments. Additionally, the effects of self-ligating bracket (SLB) and conventional bracket (CB) systems have been discussed widely, although a previous meta-analysis revealed that SLBs do not outperform CBs in promoting oral health.[13] Some researchers have suggested that SLBs may prevent oral malodor[14]; others, however, disagree.[15]
Therefore, this systematic review and meta-analysis aimed to collect evidence to identify the effects of fixed brackets on oral malodor, and whether the effect of SLB systems differs from that of CB systems.
2. Methods
A systematic review and meta-analysis was performed according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. As a meta-analysis and systematic review, no ethical approval or patient consent was required.
This meta-analysis was designed and conducted according to instructions from the Cochrane Handbook.[16] The study design, participants, interventions, comparisons, and outcomes (i.e., PICO) definition was followed. Randomized controlled and clinical controlled trials that included subjects with permanent dentition, without systemic problems or poor oral hygiene, and experimental groups that received fixed orthodontic therapy were included. Patients treated with fixed orthodontic brackets were compared with those without any treatment, and SLB systems were compared with CB systems. Outcomes included oral malodor scores, PI, gingival index (GI), and periodontal pocket depths.
The following exclusion criteria were applied: clinical studies without comparison(s); reviews; case reports; and letters. Studies involving participants with poor oral condition or systemic diseases, investigations in which no measurement of malodor was performed, or those that included removable orthodontic appliances were also excluded.
2.1. Search strategy
The electronic databases PubMed, Ovid, Embase, and the Cochrane Library, from inception to September 2016, were searched. Search words included: orthodontic∗, brace∗, bracket∗, and halitosis, malodor, bad breath, foul breath, offensive breath, breath odor, and discernible smell. Additionally, a manual search was conducted according the reference lists of relevant literature reports.
2.2. Study selection
Two reviewers (JH and JHJ) independently scanned the titles and abstracts of searched articles and selected potentially relevant studies. Any disagreement was resolved via consultation with a third reviewer (CYL). Relevant full-text studies were downloaded to identify whether they fulfilled the inclusion criteria. Any discrepancies were discussed among the 3 reviewers to reach consensus.
2.3. Bias assessment
According to the Cochrane Handbook, the following 7 aspects of bias were assessed: randomization sequence generation; allocation concealment; blinding of participants; blinding of outcome examiners; incomplete data; selective reporting; and other possible biases.
The risk for bias in research is assessed to be “low” if all 7 aspects are identified as “low,” “high” if any of the aspects identified as “high,” or “unclear” if no aspect identified as “high” but one or more aspects as “unclear.”[16]
2.4. Data extraction
Two reviewers (JH and JHJ) extracted the following data independently: randomization; concealment and blinding; loss to follow-up; demographic data; bracket types; types of ligation; malodor measurements; and PI, GI, and measurement intervals. Any controversies were addressed via consultation with a third reviewer (CYL).
Statistical analyses were performed using Review Manager version 5.3 (Copenhagen: The. Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Heterogeneity was assessed using the I2 statistic at a significance level of α = 0.05, and mean difference (MD) with 95% confidence interval (CI) were adopted. Continuous data are presented as MD, while dichotomous data are expressed as relative risk. Subgroup analyses were performed based on measurement intervals. A random-effect model (REM) was applied when heterogeneity was high (>50%); otherwise, a fixed-effect model (FEM) was used.
3. Results
3.1. Study selection
A total of 355 articles were selected through the electronic search and 8 from the manual search; after removal of 135 duplicates, 228 studies remained. After full-text review of 7 potentially relevant articles, 4 met the inclusion criteria and were included in the systematic review and meta-analysis. The flow of the literature selection process is shown in Fig. 1. Detailed characteristics of the included studies are summarized in Table 1. All 4 studies used a halimeter manufactured by the same company to measure oral malodor and similar methods were used, as reported in Table 2.
Figure 1.
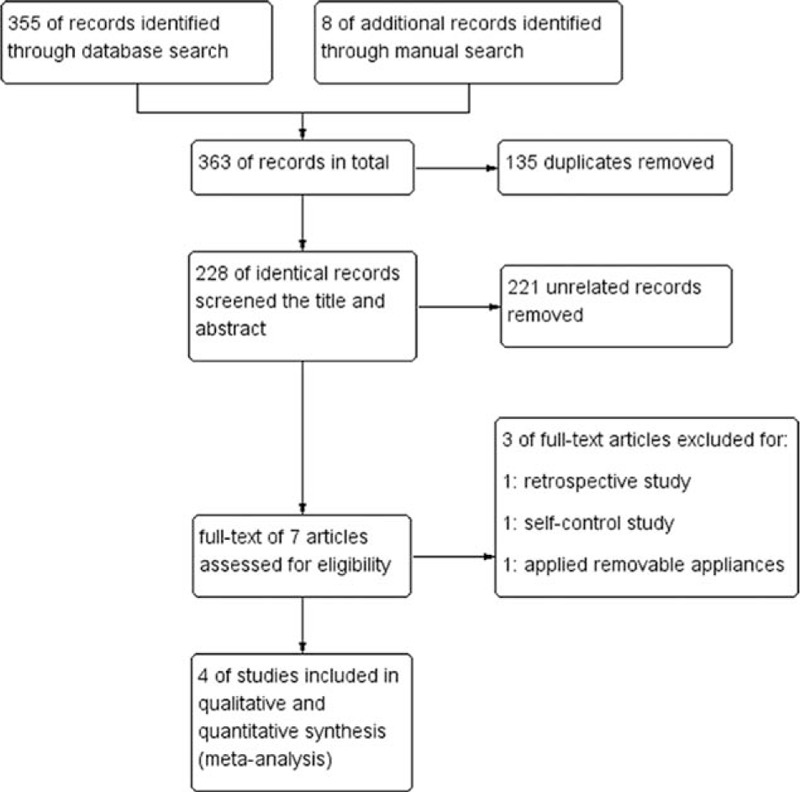
Flow diagram of the literature selection process.
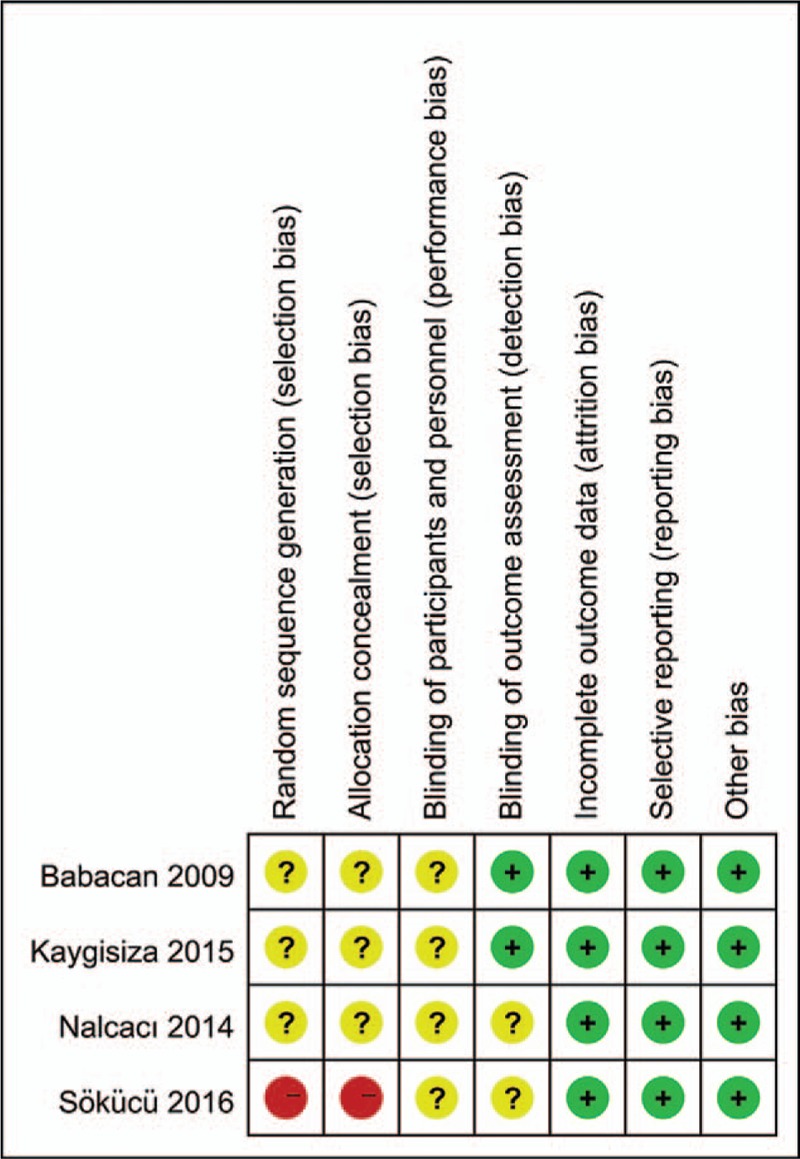
Table 1.
Characteristics of the included studies.
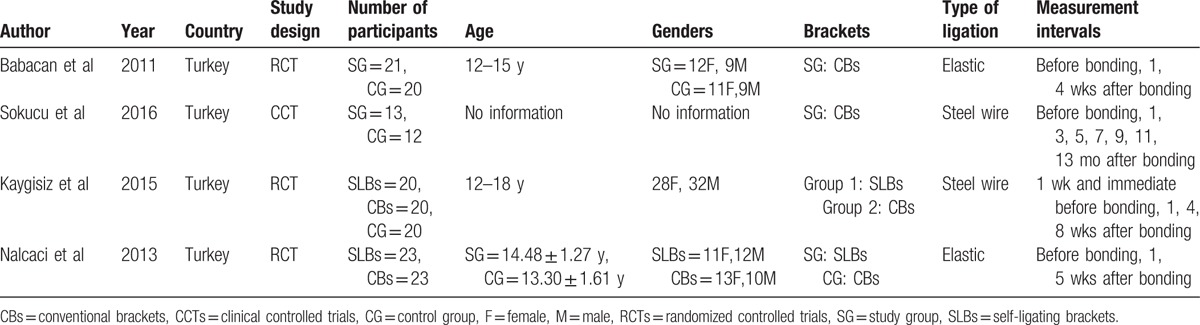
Table 2.
Measurement methods used in the included studies.
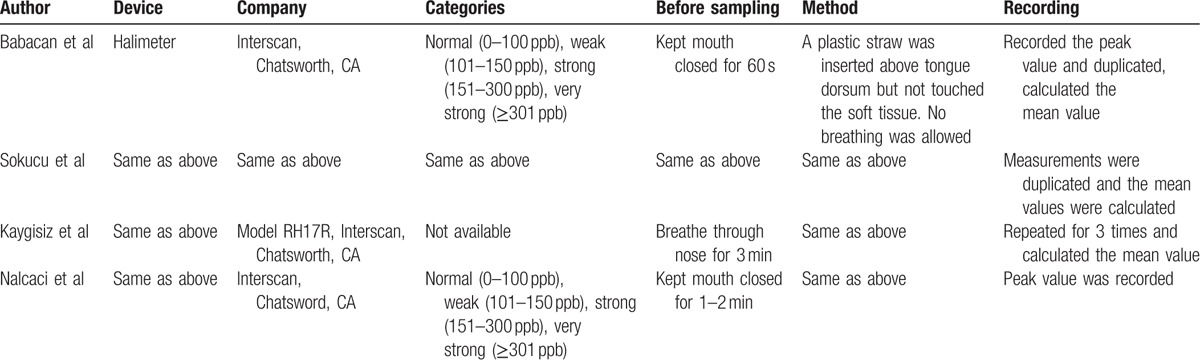
3.2. Bias assessment
Among the 4 included studies, 3 were assessed as unclear risk and the other was evaluated as high risk. The quality of the included articles was relatively low, mainly because it was difficult to maintain participant blinding in the studies, and the randomization methods and concealment of allocation were not well developed. Bias assessment is illustrated in Fig. 2.
Figure 2.
Bias assessment of included studies.
3.3. Fixed orthodontic appliances versus control
Three of the included studies compared differences in the effects of CBs with ligation and an untreated control group. Malodor scores, PI, GI, and periodontal pocket depths were tested at the initial visit for bonding, 1 week after bonding, 1 month (4 or 5 weeks) after bonding, and 2 to 3 months after bonding. The data were synthesized into 3 subgroups based on the measurement intervals. Based on the heterogeneities of the subgroups, both the REM and FEM were applied to pool the MD and 95% CI.
As shown in Fig. 3, malodor scores demonstrated significant differences between the experimental and control groups only at 1 week after bonding (MD 20.24 [95% CI 11.75–28.74]; P < .00001), but was not significant at 1 month after bonding (MD 13.62 [95% CI −11.91–39.14]; P = .30), or 2 to 3 months after bonding (MD 0.14 [95% CI −0.01–0.30]; P = .07).
Figure 3.
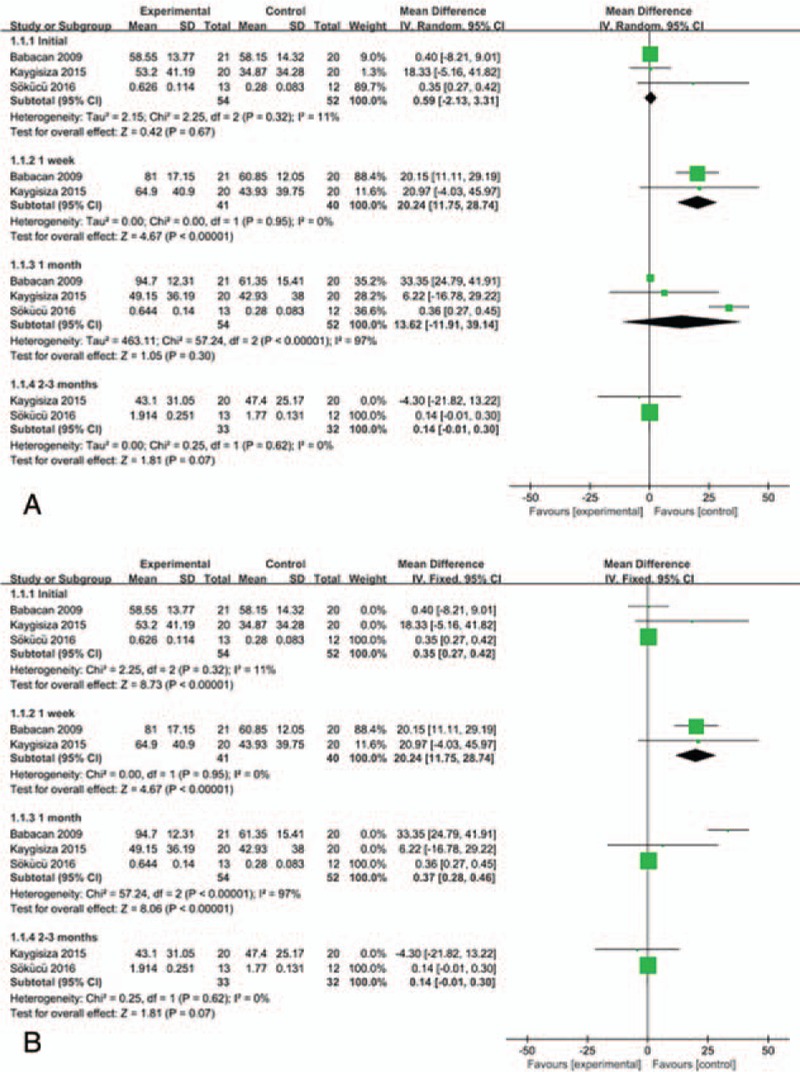
Malodor score at various measurement intervals: experimental groups versus control groups at initial visit, 1 week, 1 month, and 2 to 3 months after bonding, outcome: 1.1 Malodor score. A: Random-effect model; B: Fixed-effect model.
In comparing PIs (Fig. 4), the CB group demonstrated no statistical difference compared with the control group at either the initial visit or 1 week after bonding, but did, however, demonstrate a statistical difference at 1 month after bonding (MD 0.24 [95% CI 0.05–0.43]; P = .01). Similarly, GI was statistically different between the 2 groups only at 1 month after bonding (MD 0.30 [95% CI 0.06–0.54]; P = .01). Periodontal pocket depths demonstrated no statistical changes over the 3-month period after bonding.
Figure 4.
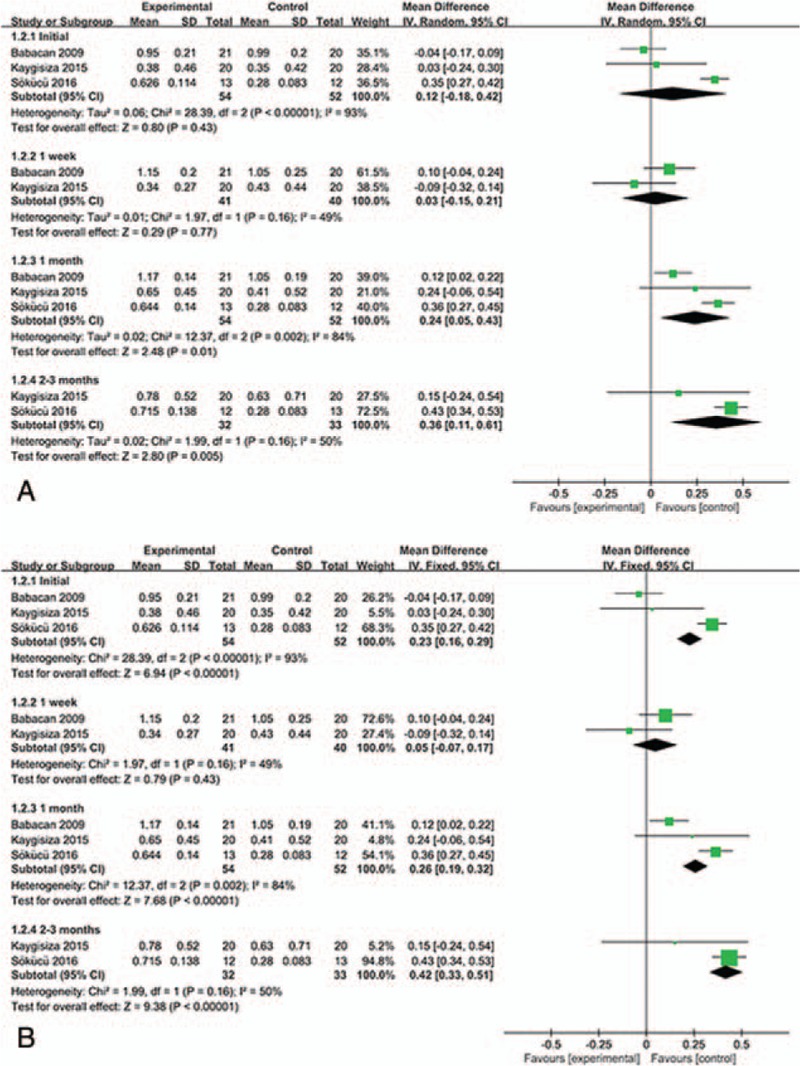
Plaque index (PI) at various measurement intervals: experimental groups versus control groups at initial visit, 1 week, 1 month, and 2 to 3 months after bonding, outcome: 1.2 PI. A: Random-effect model; B: Fixed-effect model.
3.4. CBs versus SLBs
Two included studies compared CBs with ligation and SLBs. The same subgroups were investigated based on measurement intervals, namely initial visit for bonding, 1 week after bonding, and 1 month (4 or 5 weeks) after bonding. Based on the heterogeneities of the subgroups, both REM and FEM were applied to pool the MD and 95% CI.
As illustrated in Fig. 5, the SLB group demonstrated a statistically significant advantage over the CB group 1 week after bonding (MD −4.32 [95% CI −6.02 to −2.61]; P < .00001). Although this advantage persisted 1 month after bonding, the difference was not statistically significant (MD −17.16 [95% CI −44.93 to 10.61]; P = .23).
Figure 5.
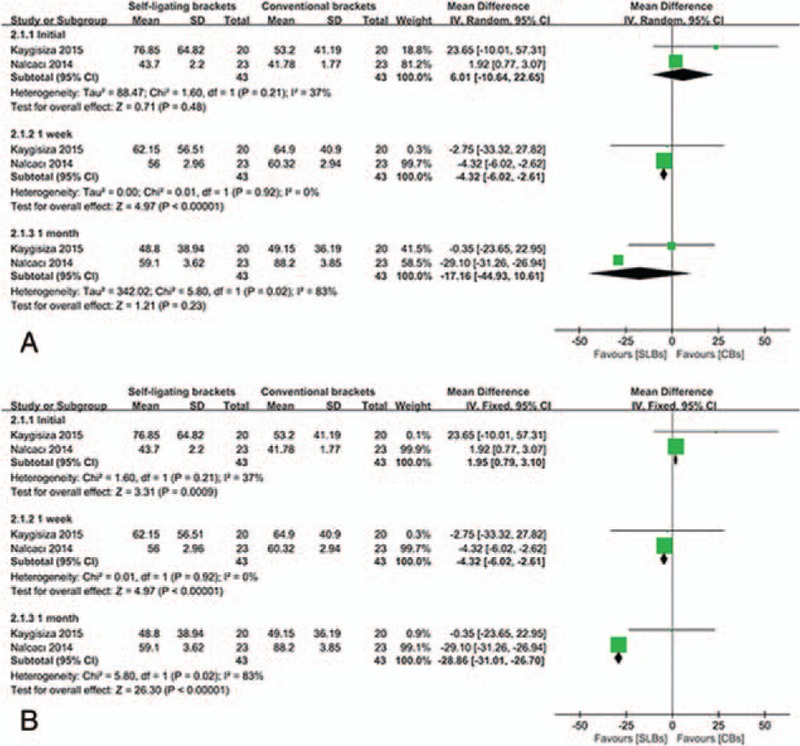
Malodor score at various measurement intervals: self-ligating bracket (SLB) groups versus conventional bracket (CB) groups at initial visit, 1 week, and 1 month after bonding, outcome: 2.1 Malodor score. A: Random-effect model; B: Fixed-effect model.
PI and GI demonstrated similar trends over the first month after bonding, the results of SLB group exceeded that of the CB group 1 week and 1 month after bonding, with a nonsignificant advantage.
4. Discussion
Fixed orthodontic appliances impede oral hygiene measurement and create favorable conditions for plaque accumulation. Studies have demonstrated that periodontal problems are one of the potential side effects of orthodontic treatment,[17–20] although it remains controversial whether plaque is a causative factor of malodor.[8] The present meta-analysis aimed to identify whether there is a relationship between fixed orthodontic appliances and malodor, and whether SLBs could prevent malodor better than CBs.
As shown in Fig. 3, malodor was more serious in the orthodontic group than the control group, although this difference was only significant at the first week and nearly significant at 2 to 3 months. Three of the included studies had observation periods not exceeding 3 months; consequently, we could not ascertain whether obvious malodor persisted after 3 months in orthodontic patients. Zurfluh et al[21] found significant differences in organoleptic measurements on the same subjects between the initial visit and at 3 months. Based on a 1-year observation, Sokucu et al[12] reported that oral malodor in orthodontic patients reached a peak after 7 months and stopped increasing during the ninth month of treatment.
The results of PI analysis revealed no significant difference between the 2 groups after the first week; however, the statistical advantage of the control group was observed at 1 month, and at 2 to 3 months (Fig. 4). As mentioned above, obvious differences in malodor appeared at 1 week, before plaque accumulation increased to a statistically significant level; thus, we suggest that plaque may not be the causative factor of malodor.
In addition, GI demonstrated a significant difference only after the first month, but not after the first week, or at 2 to 3 months, while periodontal pocket depths demonstrated no statistical difference over the measurement intervals. However, given the limited number of subjects involved in this meta-analysis, the relationship between malodor and periodontal condition needs to be confirmed in future, larger-scale research.
On the other hand, SLB systems were expected to better control oral hygiene conditions in orthodontic patients than CB systems because they avoid elastic or steel-wire ligation, thereby reducing retention sites for plaque accumulation.[17,18,22] However, some investigators have reported that this theoretical advantage may disappear in practice because the opening and closing mechanisms of SLBs provide hospitable retention sites for plaque.[13]
Despite the relationship between fixed orthodontic appliances and malodor, we also aimed to address whether SLBs could better control malodor in orthodontic patients compared with CBs. As revealed in Fig. 5, the prevalence of malodor was lower in the SLB group, although only significant at 1 week. In contrast, the results of PI and GI in the SLB group demonstrated a slight advantage over that of the CB group over the first month after bonding.
Because fixed orthodontic appliances led to obvious malodor at week 1, SLBs conquered the CB at the first week in the control of malodor. We suggest with weak evidence that SLB systems could be a consideration for orthodontic patients at high risk for malodor. Whether there is a long-term effect of SLBs needs to be confirmed in future research with longer observational periods.
4.1. Limitations
Only 4 studies were included in this systematic review and meta-analysis, and the quality of these studies was relatively low. More research in this field is necessary to draw definitive conclusions about the effect of orthodontic treatment or bracket types on malodor.
5. Conclusion
Fixed orthodontic therapy is a risk factor for malodor at 1 week after bonding, independent of the change in PI. SLB systems controlled malodor slightly better than CB systems, significantly at the first week after bonding and, thus, could be considered for orthodontic patients at high risk for malodor.
Acknowledgments
The authors appreciate the help from the Center Laboratory of the Peking University, School of Stomatology.
Author contributions
Cui-Ying Li and Jiu-Hui Jiang conceptualized and designed the project. Jing Huang, Cui-Ying Li, and Jiu-Hui Jiang, performed the literature screening, data extraction, bias evaluation, and analyzed the data. Jing Huang drafted the manuscript.
Conceptualization: Jing Huang.
Data curation: Jing Huang, Cui-Ying Li.
Formal analysis: Jing Huang, Cui-Ying Li, Jiu-Hui Jiang.
Funding acquisition: Jiu-Hui Jiang.
Investigation: Jing Huang, Cui-Ying Li.
Methodology: Jing Huang, Cui-Ying Li, Jiu-Hui Jiang.
Project administration: Jiu-Hui Jiang.
Resources: Jing Huang, Cui-Ying Li.
Software: Jing Huang, Cui-Ying Li.
Supervision: Cui-Ying Li, Jiu-Hui Jiang.
Validation: Cui-Ying Li, Jiu-Hui Jiang.
Visualization: Jiu-Hui Jiang.
Writing – original draft: Jing Huang.
Writing – review & editing: Jing Huang.
Footnotes
Abbreviations: CBs = conventional brackets, CCTs = clinical controlled trials, CG = control group, CI = confidence interval, F = female, FEM = fixed-effect model, GI = gingival index, M = male, MD = mean difference, PI = plaque index, RCTs = randomized controlled trials, REM = random-effect model, SG = study group, SLBs = self-ligating brackets, VSCs = volatile sulfur compounds.
This study was supported by the National Natural Science Foundation of China (Nos. 81171006, 81571002), Beijing Natural Science Foundation (No. 7162203), and also by the Beijing Science and Technology Committee. (No.Z121107001012024). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors report no conflicts of interest.
References
- [1].Meskin LH. A breath of fresh air. J Am Dent Assoc 1996;127:1282.1284, 1286 passim. [DOI] [PubMed] [Google Scholar]
- [2].Tonzetich J. Production and origin of oral malodor: a review of mechanisms and methods of analysis. J Periodontol 1977;48:13–20. [DOI] [PubMed] [Google Scholar]
- [3].McKeown L. Social relations and breath odour. Int J Dent Hyg 2003;1:213–7. [DOI] [PubMed] [Google Scholar]
- [4].Morita M, Wang HL. Association between oral malodor and adult periodontitis: a review. J Clin Periodontol 2001;28:813–9. [DOI] [PubMed] [Google Scholar]
- [5].Nalcaci R, Sonmez IS. Evaluation of oral malodor in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:384–8. [DOI] [PubMed] [Google Scholar]
- [6].Quirynen M. Management of oral malodour. J Clin Periodontol 2003;30Suppl:17–8. [DOI] [PubMed] [Google Scholar]
- [7].Quirynen M, Zhao H, van Steenberghe D. Review of the treatment strategies for oral malodour. Clin Oral Investig 2002;6:1–0. [DOI] [PubMed] [Google Scholar]
- [8].De Geest S, Laleman I, Teughels W, et al. 2016. Periodontal diseases as a source of halitosis: a review of the evidence and treatment approaches for dentists and dental hygienists. Periodontol 2000;71:213–27. [DOI] [PubMed] [Google Scholar]
- [9].Mtaya M, Brudvik P, Astrom AN. Prevalence of malocclusion and its relationship with socio-demographic factors, dental caries, and oral hygiene in 12- to 14-year-old Tanzanian schoolchildren. Eur J Orthod 2009;31:467–76. [DOI] [PubMed] [Google Scholar]
- [10].Gray D, McIntyre G. Does oral health promotion influence the oral hygiene and gingival health of patients undergoing fixed appliance orthodontic treatment? A systematic literature review. J Orthod 2008;35:262–9. [DOI] [PubMed] [Google Scholar]
- [11].Babacan H, Sokucu O, Marakoglu I, et al. Effect of fixed appliances on oral malodor. Am J Orthod Dentofacial Orthop 2011;139:351–5. [DOI] [PubMed] [Google Scholar]
- [12].Sokucu O, Akpinar A, Ozdemir H, et al. The effect of fixed appliances on oral malodor from beginning of treatment till 1 year. BMC Oral Health 2016;16:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yang X, Su N, Shi Z, et al. Effects of self-ligating brackets on oral hygiene and discomfort: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Dent Hyg 2017;15:16–22. [DOI] [PubMed] [Google Scholar]
- [14].Kaygisiz E, Uzuner FD, Yuksel S, et al. Effects of self-ligating and conventional brackets on halitosis and periodontal conditions. Angle Orthod 2015;85:468–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nalcaci R, Ozat Y, Cokakoglu S, et al. Effect of bracket type on halitosis, periodontal status, and microbial colonization. Angle Orthod 2014;84:479–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 8. Chichester: John Wiley & Sons; 2008. 1–44. [Google Scholar]
- [17].Lara-Carrillo E, Montiel-Bastida NM, Sanchez-Perez L, et al. Effect of orthodontic treatment on saliva, plaque and the levels of streptococcus mutans and lactobacillus. Med Oral Patol Oral Cir Bucal 2010;15:e924–9. [DOI] [PubMed] [Google Scholar]
- [18].Pellegrini P, Sauerwein R, Finlayson T, et al. Plaque retention by self-ligating vs elastomeric orthodontic brackets: quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop 2009;135:426.e1–9. discussion 426-7. [DOI] [PubMed] [Google Scholar]
- [19].Scheie AA, Arneberg P, Krogstad O. Effect of orthodontic treatment on prevalence of streptococcus mutans in plaque and saliva. Scand J Dent Res 1984;92:211–7. [DOI] [PubMed] [Google Scholar]
- [20].Pandis N, Vlachopoulos K, Polychronopoulou A, et al. Periodontal condition of the mandibular anterior dentition in patients with conventional and self-ligating brackets. Orthod Craniofac Res 2008;11:211–5. [DOI] [PubMed] [Google Scholar]
- [21].Zurfluh MA, van Waes HJ, Filippi A. The influence of fixed orthodontic appliances on halitosis. Schweiz Monatsschr Zahnmed 2013;123:1064–75. [PubMed] [Google Scholar]
- [22].Ogaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Am J Orthod Dentofacial Orthop 1988;94:68–73. [DOI] [PubMed] [Google Scholar]


