Abstract
Child sexual abuse (CSA) is a global problem that affects children of all ages, and the evaluation of these victims by psychologic and gynecologic experts in pediatric emergency departments is an important issue. Few data are available on the characteristics of children admitted to pediatric emergency department with recurrent CSA and delayed reported CSA. The aim of the present study was to describe the clinical features of, and risk factors for, recurrent CSA and delayed reported CSA. The study retrospectively analyzed victims of CSA who were admitted to a pediatric emergency department. Chi-square tests and univariate analyses were performed to assess the risk factors of recurrent or delayed reported CSA. Of the 91 CSA cases, 32 (35.2%) were recurrent assaults. Of the 70 cases recorded the duration of the event, 22 (31.4%) were delayed report cases. Comparisons of the non-recurrent and recurrent CSA assault groups revealed a significant increase in comorbidities (odds ratio [OR]: 4.46, 95% confidence interval [CI]: 1.54–12.93), acute psychiatric problems (OR: 3.18, CI: 1.26–8.06), attempted suicide (OR: 4.23, CI: 1.28–13.99), and the need for treatment with antipsychotic medications (OR: 5.57, CI: 1.37–22.65). Compared with non-delayed reported cases, the delay reported cases of CSA were significantly more likely to have anxiety (P < .05). The CSA victims in the present study exhibited acute medical and/or psychosocial problems, which indicate that pediatric emergency professionals have a responsibility to look for and recognize particular characteristics in these victims.
Keywords: child sexual abuse, delayed reported, recurrent, suicide
1. Introduction
Child sexual abuse (CSA) is a global problem that affects millions of children. Approximately 1% of children experience some form of sexual abuse each year,[1] and these CSA victims are at an increased risk of medical, psychologic, behavioral, and general health impairments.[2–5] The CSA is a serious issue in pediatric medicine. It also remains challenging for pediatricians due to interpretations of findings. In contrast to reporting by adult victims of sexual abuse, child victims of sexual abuse do not always immediately report the assault.[6] Thus, it is rare that a child victim would actively detail the CSA event but common that they delay the reporting of it. Furthermore, children who have been abused are at an increased risk of recurrent abuse and this risk is highest during the period soon after the index episode.[7] The body swabs collected from prepubertal children more than 24 h after a CSA event are unlikely to produce reliable forensic evidence,[8] and the evidence from these physical examinations typically do not predict the yield of the forensic laboratory tests.[9,10] Thus, pediatricians in pediatric emergency departments (PEDs) should always be aware of the acute evaluation and treatment of victims after this type of assault to prevent sexually transmitted infections and other significant medical or behavioral problems and to assess possible suicidal ideations and plans.[11–13]
Therefore, the characteristic medical and psychologic issues of children who have experienced recurrent assaults and who delayed the reporting of a CSA event are critically important. Few data are available on the characteristics of children admitted to PEDs with recurrent CSA and delayed reported CSA. The victims of recurrent assaults and delayed reported CSA may possibly higher risk of physical or psychologic sequelae. To further elucidate these issues, the primary objectives of the present study were to identify the factors associated with recurrent CSA and delayed reported CSA and whether there were any differences in the psychosocial and gynecologic sequelae during their evaluation at a PED.
2. Materials and methods
2.1. Study design
From January 2001 to December 2010, a total of 110 patients who were 18 years of age or younger with a diagnosis of CSA were evaluated at our PED. All data were retrospectively obtained from a review of the case information and consultation medical records. The study was approved by the institutional review board of this hospital. Data regarding the following variables were collected: age, sex, any history of social worker or psychiatric investigation, family relationship of the alleged perpetrator to the child, findings of the physical examination, medication at the PED, outcomes, and the record sheets of the gynecologist, urologist, social worker, and/or psychiatrist.
The CSA was defined as any sexual event that was performed upon a child for the purposes of the sexual behaviors and that was witnessed or disclosed. These behaviors included the fondling of breasts or genital organs, exposure to sexual activity, and oral, anal, penis, or vaginal penetration. Of 110 patients, 91 (82.73%) who had consulted with the multiple disciplines, including gynecologist, urologist, psychiatrist, and/or social worker were finally included in the analysis. Patients older than 18 years of age or who had incomplete medical chart records were excluded from the present study.
Recurrent CSA was defined as the occurrence of one or more events of sexual abuse experienced by the same child. Delayed reported CSA was defined as sexual abuse that was reported in the PED at least 7 days after the event. The non-delayed reported group consisted of children seen within 7 days of the alleged assault.
Poor family support was defined as divorced parents, conflict with family members, the death of one of the parents, or living with a stepfather. A familiar place was defined as an event that occurred at the victim's home, the babysitter's home, kindergarten, or school. Family members included stepfather, mother's boyfriend, and babysitter. Positive genital signs included an acute or old laceration of the hymen, vestibule laceration, bruising of the hymen or penis, erythematous swelling of the vulva, vaginal discharge, or vaginal bleeding.
The sequelae of gynecologic problems were defined as patients who had sexually transmitted diseases, vaginitis, an abortion, or pregnancy. Acute psychiatric problems were considered to be present if the victim had any of the following disorders: acute stress disorder, post-traumatic stress disorder, anxiety disorder, adjustment disorders, depressed mood, attention deficits, disruptive behaviors, sleep disorder, or developmental disorders. Attempted suicide was defined as self-hurting behaviors after the CSA assault.
2.2. Statistical analysis
Chi-square tests or Fisher's exact tests were used to analyze categorical variables and the Mann–Whitney U test was used to analyze continuous variables between the recurrent and non-recurrent groups and the delayed reported CSA and non-delayed group. For all tests, a two-sided P-value of <.05 was considered to indicate statistical significance. All data are expressed as mean ± standard deviations (SDs), and all statistical analyses were performed using SPSS software (ver. 17.0; SPSS, Chicago, IL).
3. Results
3.1. Study population
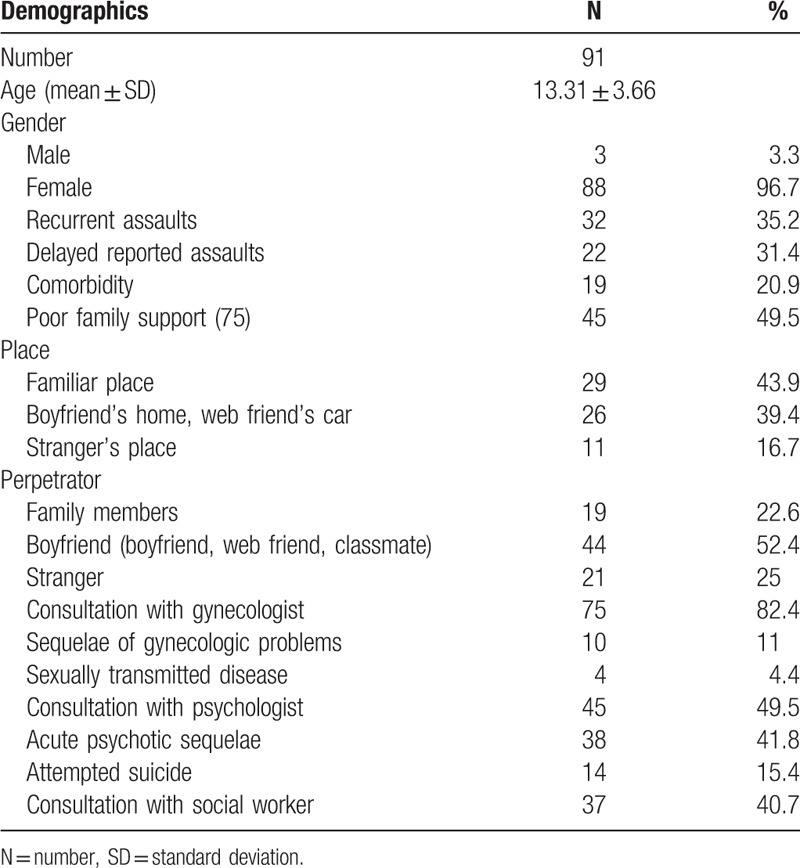
A total of 91 records from the 10-year study period were eligible for review. Of these 91 CSA cases, 3 (3.3%) were males and 88 (96.7%) were females. The mean age of those with CSA was 13.31 ± 3.66 years and 10 cases (11.0%) were younger than 10 years of age. Additionally, 32 cases (35.2%) experienced recurrent assaults, 22 cases (31.4%) were delayed reported.
Nineteen cases (20.9%) had comorbidities, and 45 cases (49.5%) were associated with poor family support. The sequelae of gynecologic problems during follow-up visits were observed in 10 cases (11.0%), 38 cases (41.8%) had acute psychotic problems, and 14 cases (15.4%) had attempted suicide (Table 1).
Table 1.
Demographics of child sexual abuse cases admitted to the pediatric emergency department.
3.2. Comparative analysis of victims with recurrent CSA and those without recurrent CSA
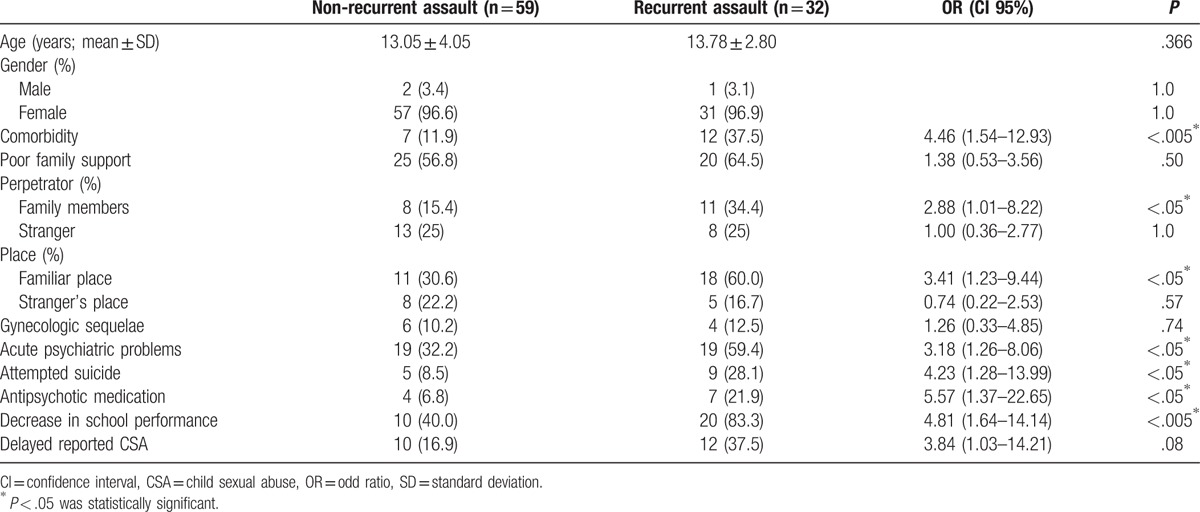
The present study found that 32 CSA cases (35.2%) involved recurrent sexual assaults. Compared with non-recurrent cases, the recurrent cases of CSA were significantly more likely to have comorbidities (odds ratio [OR]: 4.46, 95% confidence interval [CI]: 1.54–12.93), have a caregiver as a perpetrator (OR: 2.88, 95% CI: 1.01–8.22), and have the event occur in a familiar place (OR: 3.41; 95% CI: 1.23–9.44). Additionally, the victims of recurrent assaults had significantly higher rates of acute psychiatric problems (OR: 3.18, 95% CI: 1.26–8.06), attempted suicide (OR: 4.23, 95% CI: 1.28–13.99), the need for treatment with antipsychotic medications (OR: 5.57, 95% CI: 1.37–22.65), and decreased school performance (OR: 4.81, 95% CI: 1.64–14.14). The victims of recurrent assaults had higher rates of poor family support, and the gynecologic sequelae, but did not differ significantly between these two groups (Table 2).
Table 2.
Comparisons of the recurrent child sexual abuse and non-recurrent child sexual abuse victims.
3.3. Comparative analysis of the delayed reported CSA cases and those non-delayed reported CSA
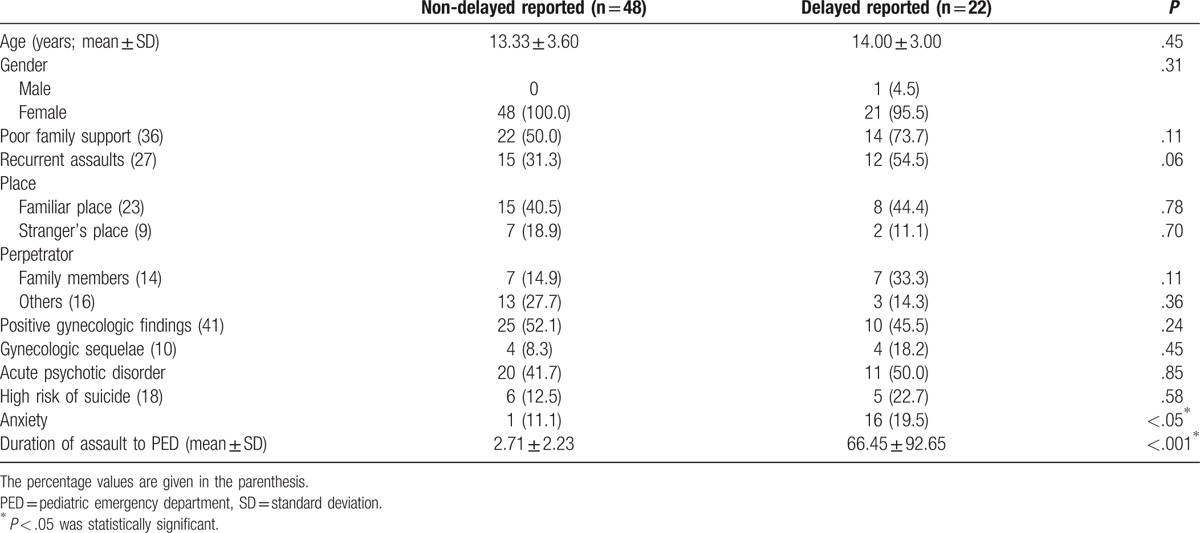
The present study found that only 70 cases were recorded the duration of the event and that 22 of these (31.4%) were reported after a delay. There were no significant differences between the non-delayed reported and delayed reported CSA groups in terms of the sequelae of gynecologic and psychiatric problems. Of those in the delayed reported CSA group, 73.7% victims had poor family support and 54.5% experienced recurrent assaults. Of the cases who consulted a gynecologist and/or a psychologist, 45.5% had documented positive gynecologic problems, 18.2% had gynecologic sequelae, and 22.7% were attempted suicide. Compared with non-delayed reported cases, the delay reported cases of CSA were significantly more likely to have anxiety (P < .05). There were no significant differences between the non-delayed reported and delayed reported CSA groups in terms of the documented positive gynecologic findings (52.1% vs 45.5%; Table 3).
Table 3.
Comparisons of children with delayed reports of CSA.
4. Discussion
This is the first study to analyze the record sheets of the multiple disciplines, including medicine, social work, gynecologist, and psychiatrist in a tertiary PED. Similar to previous reports,[14,15] compared with non-recurrent CSA cases, the present study showed that the victims of recurrent assaults were significantly more likely to have comorbidities (P < .005), have had the event occur at a familiar place (P < .05), and to have had the perpetrators be familiar individuals (P < .05), and that these individuals were at an increased risk for later maltreatment. These findings suggest that follow-up visits with the victims of CSA who exhibit particular characteristics including CSA patients with comorbidities, perpetrators as familiar individuals are necessary and that the promotion of agency policies and procedures is critically important.
Additionally, the victims of recurrent CSA had higher rates of acute psychotic disorders (P < .05), which is similar to the findings of a previous study.[16] Moreover, a national cross-sectional psychiatric survey also showed that there is a multifarious causal association between CSA and psychiatric disorders.[17] Several mechanisms can account for the link between the risk of psychotic disorders in victims of CSA and abnormal neural development, including an abnormal stress response mediated by the hypothalamic-pituitary-adrenal (HPA) axis. For example, increased levels of stress hormones in abused individuals lead to reductions in brain volume.[18] Additionally, the prefrontal cortex is known to be important to the stress response and the regulation of the negative feedback system in the HPA axis,[19] and the experience of CSA reduces activation in the prefrontal cortex as well as causing a bilateral decrease in frontal cortex gray matter volume.[20]
In the present study, the positive gynecologic signs and sequelae of gynecologic problems did not differ among the recurrent, delayed reported CSA cases, which supports previous findings showing that the rapid healing of genital injuries, the limitations of standard physical findings and forensic evidence in prepubertal CSA cases.[21] Thus, the evaluations of gynecologic professionals for children with complaints of recurrent sexual abuse in the PED, even when reported beyond 7 days of the CSA event should still be considered.
In the present study, there were no differences in the impact of psychiatric and medical problems between the delayed reported CSA group and the group who non-delayed reported group, which suggests that cases of delayed reported CSA may also require acute care and the identification of serious psychomedical problems. Of the delayed reported CSA victims who consulted with a gynecologist, 45.5% had a positive genital examination, which differed from the findings of a previous study.[22,23] This discrepancy in conclusions may be due to different study methods and various study limitations. Of the delayed reported CSA victims who consulted with a psychologist, 22.7% had attempted suicide, which suggests that the experience of sexual abuse is associated with several highly significant psychologic consequences and that the psychiatric assessment and management of CSA victims at a PED and their follow-up visits are a major concern.
The present study had several limitations. First, it was a retrospective study, and the sample size was small. Second, it did not include the forensic evidence collected by police department crime laboratories. On the contrary, the strengths of the present study included the fact that the PED from which the patients were recruited treats patients referred from schools, community CSA prevention centers, and crime administrators, which increased the number of complete documentations. Additionally, the reviewed medical records were obtained from a variety of professional offices including those of psychologists, gynecologists, urologists, and social workers and all of the cases were recorded at a PED.
5. Conclusion
In conclusion, the CSA victims in the present study exhibited acute medical and/or psychosocial problems, which indicate that pediatric emergency professionals have a responsibility to look for and recognize particular characteristics in these victims. The development of multidisciplinary techniques for use during the acute stages of CSA continues and these will likely enhance the quality of the recognition, evaluation, and management of CSA cases. These developments will also ensure the optimal assessment, treatment, and protection of vulnerable children and adolescents who have experienced sexual assault.
Acknowledgment
The authors thank Tseng Hsiao-Jung of the Center for Big Data Analytics and Statistics of Chang Gung Memorial Hospital for statistical assistance.
Author contributions
Conceptualization: M.-H. Hu, G.-S. Huang, F.-S. Lo
Data curation: M.-H. Hu, G.-S. Huang, A.-S. Chao.
Formal analysis: M.-H. Hu.
Investigation: M.-H. Hu, F.-S. Lo.
Methodology: M.-H. Hu, G.-S. Huang, F.-S. Lo, H.-P. Wu.
Supervision: J.-L. Huang, C.-T. Wu.
Validation: M.-H. Hu, H.-P. Wu.
Writing – original draft: M.-H. Hu, G.-S. Huang.
Writing – review & editing: M.-H. Hu, G.-S. Huang.
Footnotes
Abbreviations: CI = confidence interval, CSA = child sexual abuse, HPA = hypothalamic-pituitary-adrenal, OR = odds ratio, PED = pediatric emergency department, SD = standard deviation.
MHH, JLH, CTW, ASC, HPW, and FSL reviewed the medical records, and interpreted the data; MMH and GSH drafted the manuscript; MHH and GSH designed and oversaw the study, interpreted the data, and revised the manuscript. All authors have read and approved the final manuscript for publication.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kellogg N. American Academy of Pediatrics Committee on Child Abuse and Neglect. The evaluation of sexual abuse in children. Pediatrics 2005;116:506–12. [DOI] [PubMed] [Google Scholar]
- [2].Committee on Child Abuse and Neglect. Protecting children from sexual abuse by health care providers. Pediatrics 2011;128:407–26. [DOI] [PubMed] [Google Scholar]
- [3].Maniglio R. The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatr Scand 2011;124:30–41. [DOI] [PubMed] [Google Scholar]
- [4].McLean CP, Rosenbach SB, Capaldi S, et al. Social and academic functioning in adolescents with child sexual abuse-related PTSD. Child Abuse Negl 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sapp MV, Vandeven AM. Update on childhood sexual abuse. Curr Opin Pediatr 2005;17:258–64. [DOI] [PubMed] [Google Scholar]
- [6].Denton J, Newton AW, Vandeven AM. Update on child maltreatment: toward refining the evidence base. Curr Opin Pediatr 2011;23:240–8. [DOI] [PubMed] [Google Scholar]
- [7].Hindley N, Ramchandani PG, Jones DP. Risk factors for recurrence of maltreatment: a systematic review. Arch Dis Child 2006;91:744–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Christian CW, Lavelle JM, De Jong AR, et al. Forensic evidence findings in prepubertal victims of sexual assault. Pediatrics 2000;106:100–4. [DOI] [PubMed] [Google Scholar]
- [9].Girardet R, Bolton K, Lahoti S, et al. Collection of forensic evidence from pediatric victims of sexual assault. Pediatrics 2011;128:233–8. [DOI] [PubMed] [Google Scholar]
- [10].Thackeray JD, Hornor G, Benzinger EA, et al. Forensic evidence collection and DNA identification in acute child sexual assault. Pediatrics 2011;128:227–32. [DOI] [PubMed] [Google Scholar]
- [11].Palusci VJ, Cox EO, Shatz EM, et al. Urgent medical assessment after child sexual abuse. Child Abuse Negl 2006;30:367–80. [DOI] [PubMed] [Google Scholar]
- [12].Floyed RL, Hirsh DA, Greenbaum VJ, et al. Development of a screening tool for pediatric sexual assault may reduce emergency-department visits. Pediatrics 2011;128:221–6. [DOI] [PubMed] [Google Scholar]
- [13].Adams JA. Medical evaluation of suspected child sexual abuse. J Pediatr Adolesc Gynecol 2004;17:191–7. [DOI] [PubMed] [Google Scholar]
- [14].Dubowitz H, Kim J, Black MM, et al. Identifying children at high risk for a child maltreatment report. Child Abuse Negl 2011;35:96–104. [DOI] [PubMed] [Google Scholar]
- [15].Annerback EM, Sahlqvist L, Svedin CG, et al. Child physical abuse and concurrence of other types of child abuse in Sweden-Associations with health and risk behaviors. Child Abuse Negl 2012;36:585–95. [DOI] [PubMed] [Google Scholar]
- [16].Sheffield JM, Williams LE, Woodward ND, et al. Reduced gray matter volume in psychotic disorder patients with a history of childhood sexual abuse. Schizophr Res 2013;143:185–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bebbington P, Jonas S, Kuipers E, et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry 2011;199:29–37. [DOI] [PubMed] [Google Scholar]
- [18].Lupien SJ, McEwen BS, Gunnar MR, et al. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 2009;10:434–45. [DOI] [PubMed] [Google Scholar]
- [19].Sullivan RM, Gratton A. Prefrontal cortical regulation of hypothalamic-pituitary-adrenal function in the rat and implications for psychopathology: side matters. Psychoneuroendocrinology 2002;27:99–114. [DOI] [PubMed] [Google Scholar]
- [20].De Bellis MD, Keshavan MS, Shifflett H, et al. Brain structures in pediatric maltreatment-related posttraumatic stress disorder: a sociodemographically matched study. Biol Psychiatry 2002;52:1066–78. [DOI] [PubMed] [Google Scholar]
- [21].McCann J, Miyamoto S, Boyle C, et al. Healing of hymenal injuries in prepubertal and adolescent girls: a descriptive study. Pediatrics 2007;119:e1094–106. [DOI] [PubMed] [Google Scholar]
- [22].Ji K, Finkelhor D, Dunne M. Child sexual abuse in China: a meta-analysis of 27 studies. Child Abuse Negl 2013;37:613–22. [DOI] [PubMed] [Google Scholar]
- [23].Heger A, Ticson L, Velasquez O, et al. Children referred for possible sexual abuse: medical findings in 2384 children. Child Abuse Negl 2002;26:645–59. [DOI] [PubMed] [Google Scholar]


