Abstract
AIM
To compare clinical results between toric and spherical periphery design orthokeratology (ortho-k) in myopic children with moderate-to-high corneal astigmatism.
METHODS
This retrospective study enrolled 62 eyes of 62 subjects using toric ortho-k lenses. These subjects were assigned to the toric group. Based on the one-to-one match principle (same age, proximate spherical equivalence and corneal astigmatism), 62 eyes of 62 subjects were enrolled and included in the spherical group. At one-year follow-up visit, visual acuity, corneal astigmatism, treatment zone decentration, axial elongation and adverse reaction were compared between these two groups.
RESULTS
At the one-year visit, corneal astigmatism was significantly lower in the toric group (1.22±0.76 D) than in the spherical group (2.05±0.85 D) (P=0.012). The mean magnitude of the treatment zone decentration was 0.62±0.42 mm in the toric group and 1.07±0.40 mm in the spherical group (P=0.004). Axial elongation was significantly slower in the toric group (0.04±0.13 mm) than in the spherical group (0.09±0.13 mm) (P=0.001). The one-year axial elongation was significantly correlated with initial age (r=-0.487, P<0.001) and periphery design of ortho-k lens (r=0.315, P<0.001). The incidence of corneal staining was lower in the toric group (8.1%) than in the spherical group (19.4%) (P<0.001).
CONCLUSION
Toric periphery design ortho-k lenses may provide lower corneal astigmatism, better centration, slower axial elongation and lower incidence of corneal staining in myopic children with moderate-to-high corneal astigmatism.
Keywords: orthokeratology, toric, myopia, corneal astigmatism, axial elongation
INTRODUCTION
The prevalence of myopia is high in East Asia and an increasing prevalence of myopia in the United States has also been reported[1]–[3]. Hence, preventing myopic progression has attracted the interest of many researchers. Some myopia control treatments have been investigated, such as atropine[4], orthokeratology (ortho-k)[5]–[10], progressive spectacle lenses[11]–[12], and soft bifocal contact lenses[13].
Some previous studies have proved the potential of ortho-k for myopia control[5]–[10]. Moreover, the rate of axial elongation of the eyeball in children wearing ortho-k lenses has been reported to be 32% to 55% slower, compared to those wearing single-vision spectacles or soft contact lenses[5]–[10]. All of these studies used ortho-k lenses of spherical design on myopes with low astigmatism. Clinically, corneal astigmatism greater than 1.50 D (with-the-rule) is not a good indication for spherical design ortho-k lens due to the high possibility of lens decentration and induced astigmatism[14]. Thus, toric periphery design ortho-k has been developed to improve lens centration in such cases. Lyu et al[15] reported improved uncorrected visual acuity (UCVA) and decreased astigmatic refractive error when toric periphery design ortho-k lenses were used in patients with a combined myopia and astigmatism of 1.25 to 4 D. Chen et al[16] also found that toric periphery design ortho-k lenses can slow axial elongation, compared with single-vision spectacles, in myopic children with moderate-to-high astigmatism. To our knowledge, there is no published study on the differences between toric and spherical periphery design ortho-k in myopic children with moderate-to-high corneal astigmatism. The authors aimed to determine whether toric periphery design ortho-k lenses could provide a better myopic control effect.
In recent years, toric periphery design ortho-k lenses have been typically used on myopes with corneal astigmatism greater than 1.50 D. Before 2013, there was limited use of toric periphery design ortho-k in our hospital. Hence, spherical ortho-k lenses were mainly used even in myopic children with moderate-to-high corneal astigmatism. A retrospective study was conducted to compare the visual results and axial elongation between toric and spherical periphery design ortho-k lenses in matched-pairs of myopic children (age, spherical equivalence, corneal astigmatism) with moderate-to-high corneal astigmatism.
SUBJECTS AND METHODS
Subjects
This retrospective cohort study was conducted at Peking University Third Hospital. This study was carried out in accordance with the tenets of the Declaration of Helsinki. An informed consent was obtained from each subject. Sixty-two subjects, who were 8-16 years old, began using toric periphery design ortho-k lenses from 2013 to 2015, and had one-year regular follow-ups, were enrolled in this study. A random eye of each subject was included in the toric group. Before 2013, 1045 eyes were fitted with spherical ortho-k lenses. Among those eyes, 358 eyes had corneal astigmatism more than 1.50 D. For a point of comparison, a one-to-one match was desired for each eye included in the toric group. Every eye in the toric group was matched with one eye of another subject, who was of the same age, and began to use spherical ortho-k lenses with proximate spherical equivalence (<0.50 D) and corneal astigmatism (<0.50 D). In this manner, 62 eyes of 62 subjects were chosen and included in the spherical group.
The inclusion criteria for subjects were as follows: 1) age within 8-16 years old; 2) myopia of 1.00-6.00 D; 3) with-the-rule corneal astigmatism within 1.50-3.50 D; 4) best-corrected visual acuity (BCVA) ≤0.00 logMAR; 5) regular follow-ups for at least one year. The exclusion criteria were: 1) binocular vision problems (e.g. strabismus); 2) ocular surgery, trauma, and infection disease during the follow-up; 3) the use of medications that might affect refractive development (e.g. atropine eye drops); 4) discontinued lens wear of more than two weeks during the follow-up.
Examinations
All subjects underwent a baseline comprehensive eye examination, which involved clinical history, UCVA, cycloplegic refraction, manifest subjective refraction with BCVA, slit-lamp examination, undilated ocular fundus examination, non-contact tonometry, corneal endothelium microscopy, corneal tomography (Sirius, CSO, Italy) and axial length measurement (Zeiss IOLMaster; Zeiss Humphrey Systems, Dublin, CA, USA). Baseline central corneal thickness, keratometry, pupil diameter and E value were automatically measured by Sirius tomography.
The clinical follow-up periods were one day, one week, one month and then every three months for both groups. At one-year follow-up, after 6 to 8h of overnight lens wear cessation, the follow-up examinations involved UCVA measurements, slit-lamp examination, corneal tomography, axial length measurement and lens inspection to assess the condition of the lens. The magnitude of the treatment zone decentration relative to the corneal vertex was measured from the corneal tomography refractive power difference maps[17].
Orthokeratology Lenses Fitting and Wearing
Subjects in the toric group were fitted with Toric LK lens (Lucid Korea, Bonghwa, Korea). Subjects in the spherical group were fitted with Euclid ortho-k lenses (Euclid systems, Herndon, USA) (Table 1). Appropriate trial lenses were chosen according to corneal curvature, corneal astigmatism and corneal diameter. Then, the subjects tried the lenses for 30min. Fluorescein pattern was used to observe the fit of the lens in each eye under a slit lamp. All lenses had a 0.5-1.0 mm range of movement, a 3.0-4.0 mm flat contact area in the center of the cornea, a 1.0-2.0 mm annulus of tear reservoir in the reverse curve, and a 0.5-1.0 mm area of annulus of tear reservoir in the peripheral curve. However, some lenses did not have a good central position in both groups. The magnitude of lens decentration of <1.0 mm was acceptable, and when the corneal condition permitted, lens diameter was increased to 10.8-11.0 mm to improve lens centration.
Table 1. Parameters of ortho-k lenses used in this study.
| Parameters | Lucid toric LK lens | Euclid ortho-k lens |
| Material | Hexafocon A (fluoro silicone acrylate) | Boston EQUALENS II (oprifocon A) |
| Oxygen permeability (cm2·mL O2)/(s·mL·mm Hg) | 100×10−11 | 85×10−11 |
| Diameter (mm) | 10.4-11.0 (0.20 step) | 9.80-11.6 (0.10 step) |
| Radius of curvature (mm) | 6.5-12.0 (0.05 step) | 6.00-12.50 (0.10 step) |
| Central thickness (mm) | 0.21-0.25 | 0.22-0.26 |
| Vertex diopter (D) | +0.00 to +2.00 (+0.25 step) | -5.00 to +5.00 (+0.25 step) |
| Cylinder power (D) | 1.00, 2.00 | None |
The subjects were given clear instructions regarding the wearing and maintenance of ortho-k lenses. All subjects continuously wore the ortho-k lenses for an average of eight hours during sleep, and did not wear the lenses during the day. The maximum allowance for treatment zone decentration was 1.5 mm, if the cornea was healthy and UCVA was satisfactory. Otherwise, the ortho-k treatment was stopped.
Statistical Analysis
Data were analyzed using SPSS 21.0 (SPSS Inc., Chicago, Illinois, USA). Paired sample t-test (normal distribution), Wilcoxon signed-rank test (non-normal distribution) and Pearson Chi-Square test were used to compare the data between these two groups. Partial correlation was used to analyze the correlative factors of axial length elongation during one-year follow-up. A P value <0.05 was considered statistically significant.
RESULTS
Baseline Data in Both Groups
No statistically significant differences were found in baseline values between these two groups in terms of age, spherical equivalence, corneal astigmatism, central corneal thickness, intraocular pressure, endothelial cells density, keratometry, E value, pupil diameter and axial length (P>0.05, paired sample t-test; Table 2).
Table 2. Baseline data of subjects in the toric and spherical groups.
| Parameters | The toric group | The spherical group | t | P |
| Subjects/eyes (n) | 62/62 | 62/62 | ||
| Age (y) | 12.2±2.1 (8-16) | 12.2±2.1 (8-16) | 0 | 1 |
| SE (D) | -4.28±1.61 (-1.00 to -6.00) | -4.24±1.58 (-1.25 to -6.00) | -1.116 | 0.292 |
| CA (D) | 2.35±0.52 (1.50-3.40) | 2.29±0.49 (1.50-3.30) | 1.226 | 0.268 |
| CCT (µm) | 541.4±31.2 | 543.5±30.2 | -0.791 | 0.528 |
| IOP (mm Hg) | 15.11±2.70 | 15.67±2.90 | -1.496 | 0.198 |
| ECD (n/mm2) | 3281.6±276.1 | 3258.2±254.8 | 1.510 | 0.140 |
| Keratometry flat (D) | 42.53±1.18 | 42.64±1.26 | -1.236 | 0.252 |
| Keratometry steep (D) | 44.87±1.34 | 44.95±1.27 | -1.267 | 0.245 |
| E value | 0.54±0.11 | 0.55±0.12 | -1.144 | 0.285 |
| PD (mm) | 3.68±0.53 | 3.71±0.56 | -1.640 | 0.118 |
| AL (mm) | 25.37±0.90 | 25.33±0.91 | 0.879 | 0.451 |
SE: Spherical equivalence; CA: Corneal astigmatism; CCT: Central corneal thickness; IOP: Intraocular pressure; ECD: Endothelial cells density; PD: Pupil diameter; AL: Axial length.
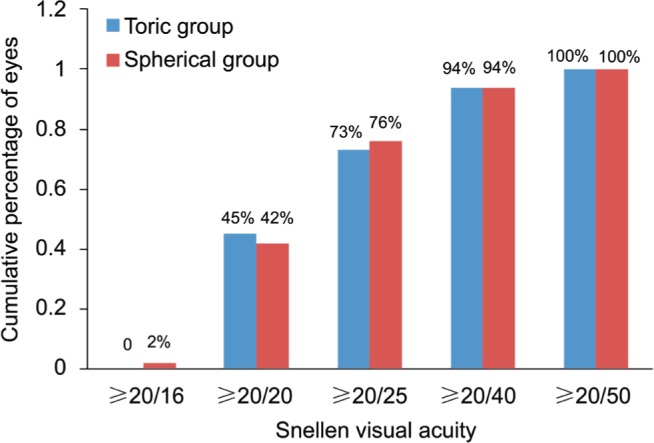
Uncorrected Visual Acuity
At the one-year follow-up, the average visual acuity in the daytime was 0.1 logMAR in both groups, and the difference was not statistically significant (P=0.386, Wilcoxon signed-rank test; Figure 1).
Figure 1. Snellen UCVA in the daytime in the toric and spherical groups.
Corneal Astigmatism
At the one-year follow-up, the mean corneal astigmatism in the toric group was 1.22±0.76 D, which decreased significantly when compared with the baseline value (P=0.018, paired sample t-test). Yet, the mean corneal astigmatism in the spherical group was 2.05±0.85 D, and no statistically significant difference was found when compared with the baseline value (P=0.326). After wearing the ortho-k lenses for one year, corneal astigmatism was significantly lower in the toric group than in the spherical group (P=0.012, paired sample t-test).
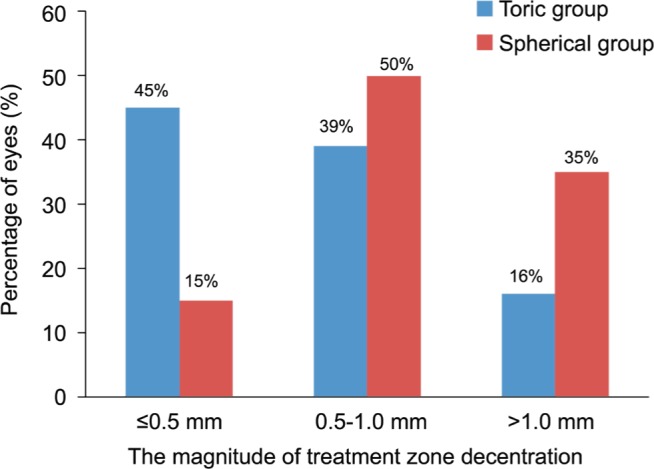
Treatment Zone Decentration
The magnitude of the treatment zone decentration was measured in the refractive power difference map (Figure 2). The distribution of the magnitude of the treatment zone decentraton in the two groups is shown in Figure 3. The mean magnitude of the treatment zone decentration was 0.62±0.42 mm in the toric group and 1.07±0.40 mm in the spherical group, and the difference was of statistical significance (P=0.004, paired sample t-test). Most of the treatment zone decentration was at the temporal (13/62, 21% in the toric group; 26/62, 42% in the spherical group) and inferior temporal (24/62, 39% in the toric group; 20/62, 32% in the spherical group) direction.
Figure 2. Measurement of the magnitude of the treatment zone decentration in the refractive power difference map.
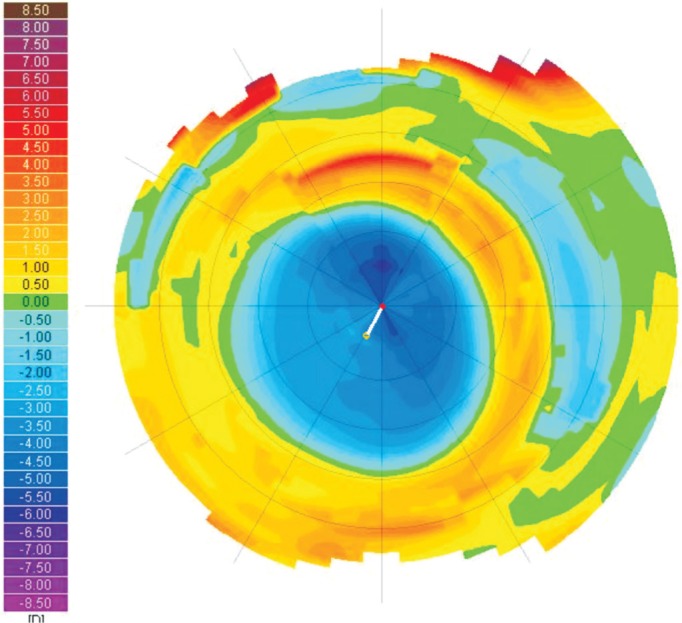
Red point: Corneal vertex; Yellow point: The center of the treatment zone; White line: The distance between the corneal vertex and the center of the treatment zone.
Figure 3. The distribution of the magnitude of the treatment zone decentration in the toric and spherical groups.
Axial Length Elongation
During the one-year follow-up, axial length increased from 25.37±0.90 to 25.41±0.82 mm in the toric group and from 25.33±0.91 to 25.42±0.84 mm in the spherical group. Significant axial elongation was recognized in both groups during the one-year follow-up (P=0.023 and 0.002, respectively; paired sample t-test). Axial elongation was significantly smaller in the toric group (0.04±0.13 mm) than in the spherical group (0.09±0.13 mm) during the one-year follow-up (P=0.001, paired sample t-test).
Correlative Factors of Axial Elongation
In all 124 eyes, factors at baseline and one-year follow-up were analyzed. The one-year axial elongation significantly correlated with initial age (r=-0.487, P<0.001) and the periphery design of ortho-k lens (toric or spherical) (r=0.315, P<0.001), but not with initial spherical equivalence, intraocular pressure, pupil diameter, initial central corneal thickness, initial corneal curvature, initial corneal astigmatism, initial E value, initial axial length and treatment zone decentration at one-year follow-up.
Adverse Reactions
No significant adverse reaction was observed in the subjects of either group. Merely mild corneal staining (grade 1, Efron Grading Scale) was observed in both groups of subjects at one-year follow-up. The incidence of corneal staining in the toric group (5/62, 8.1%) was significantly lower than that in the spherical group (12/62, 19.4%) at the one-year visit (Pearson Chi-square, χ2=22.66; P<0.001). In the toric group, central corneal staining was common. However, superior and inferior corneal staining was common in the spherical group (Table 3).
Table 3 Mild corneal staining at different corneal locations in the two groups at the one-year visit.
| Location | The toric group | The spherical group |
| Central | 2 | 1 |
| Inferior | 1 | 6 |
| Superior | 2 | 5 |
| Nasal | 0 | 0 |
| Temporal | 0 | 0 |
n
DISCUSSION
In 2009, Chan et al[18] first reported a successful case of a child with high corneal astigmatism, who was fitted with a pair of toric ortho-k lenses. At present, many manufacturers have developed toric reverse geometry lens designs (toric reverse and/or alignment zones). The toric periphery design ortho-k can be used not only for the partial reduction of astigmatism, but also for the improvement of lens centration to some degree in myopic subjects with astigmatism greater than 1.50 D[15],[19]–[22]. Chen et al[19] ex-amined the efficacy of toric ortho-k in correcting myopia combined with moderate-to-high astigmatism. In their study, subjects aged 6 to 12y with myopia of 0.50-5.00 D and with with-the-rule astigmatism of 1.25-3.50 D were fitted with toric ortho-k lenses. They reported that manifest myopia was significantly reduced from 2.53±1.31 to 0.41±0.43 D (P<0.001), and that astig-matism was also decreased from 1.91±0.64 to 0.40±0.39 D (P<0.001) after one month of lens wear. Luo et al[21] conducted a self-controlled clinical study, in which 24 subjects (42 eyes) aged 9 to 16y with myopia of 2.50-6.00 D complicated with with-the-rule astigmatism of 1.50-3.50 D were fitted with toric ortho-k lenses. The degree of astigmatism was significantly reduced from -1.81±0.53 to -0.41±0.39 D after one month of lens wear (P<0.01). The mean axial length was 24.47±0.91 mm at baseline, which did not significantly differ from 24.48±0.94 mm after one year of lens wear (P>0.05). Furthermore, Chen et al[16] conducted a two-year non-randomized clinical study. Subjects aged 6 to 12y with myopia of 0.50 to 5.00 D and with with-the-rule astigmatism of 1.25 to 3.50 D were enrolled in the toric ortho-k group (n=35) or single-vision spectacles group (n=23). The average axial elongation in the toric ortho-k group (0.31±0.27 mm) was 52% slower than that in spectacles group (0.64±0.31 mm). This myopia control efficacy was similar to some studies that compared spherical ortho-k lens and single-vision spectacles in myopic children with astigmatism of <1.50 D[5],[7],[10].
To our knowledge, this study is the first to compare visual acuity, topographic change, axial elongation and adverse reaction between toric and spherical ortho-k lenses in myopic children with moderate-to-high corneal astigmatism. In the present study, although the visual acuity in the daytime was similar in these two groups, toric ortho-k lenses can significantly decrease corneal astigmatism by 48.1% (from 2.35 to 1.22 D), while spherical ortho-k lenses can only slightly decrease it by 10.5% (from 2.29 to 2.05 D). Lyu et al[15] and Luo et al[21] reported decreased astigmatic refractive error (30.4%, from 2.07 to 1.44 D; 77.3%, from 1.81 to 0.41 D; respectively) when Lucid toric ortho-k lenses were used by patients with combined myopia and moderate-to-high astigmatism. The present study revealed the moderate effect of toric ortho-k lenses on reducing corneal astigmatism.
In the present study, the mean magnitude of the treatment zone decentration was 0.62±0.42 mm in the toric group, which was significently lower than that in the spherical group (1.07±0.40 mm). This result revealed that toric ortho-k lenses provided better centration in myopic children with moderate-to-high astigmatism. However, this effect was limited, and 16% of eyes continued to exhibit obvious decentration (treatment zone decentration >1.0 mm), because other factors could affect lens centration, such as eyelid asymmetric force and tear film.
It was also found that toric ortho-k lenses had a stronger effect on myopia control, and axial elongation was 55.6% slower compared to spherical ortho-k lenses in myopic children with moderate-to-high astigmatism. This result revealed that toric ortho-k lenses could not only improve lens centration, but also enhance the efficacy of preventing myopia progression, when compared to spherical ortho-k lenses.
In the present study, axial elongation during the one-year ortho-k lens wear was found to be associated with initial age. This result was in agreement with some previous studies, in which a significant negative correlation was revealed between initial age and the change in axial length after one or two years of ortho-k treatment[7]–[8],[16],[23]–[24]. All these studies revealed that younger children had more axial growth when wearing ortho-k lenses, regardless of which design was used. In the present study, a correlation was also found between axial elongation and the periphery design of ortho-k lenses in myopic children with moderate-to-high corneal astigmatism, which conformed to the comparison of axial elongation between these two groups.
Many clinicians have been concerned with the potential increased risk involved in the overnight wear of contact lenses, such as microbial keratitis, peripheral ulcers and conjunctivitis[25]–[26]. In the present study, no significant adverse events were found other than corneal staining in both groups of subjects. Spherical ortho-k lenses wear tended to increase the incidence of corneal staining (spherical: 19.4%; toric: 8.1%). The incidence of corneal staining in the toric group was similar to the report of Chen et al[16]. Central corneal staining may be due to poor lens hygiene or insufficient lubribation by artificial tears before lens removal.
The limitations of the present study were listed as follows. First, this study had a retrospective design. According to the ortho-k fitting principle, a prospective randomized study does not conform to the tenets of the Declaration of Helsinki, and is not warranted. Second, subjects in the spherical group used different brand of ortho-k lenses. It had different material and lens design from Lucid ortho-k lenses, which may have interfered with the comparative results to some degree. Finally, the follow-up period was only one year, and long-term results would have been beneficial.
In conclusion, compared to spherical ortho-k lenses, toric periphery design ortho-k lenses may offer similar visual acuity, lower corneal astigmatism, better treatment zone centration, slower axial elongation and lower incidence of corneal staining in myopic children with moderate-to-high corneal astigmatism. Therefore, toric periphery design ortho-k may be a better choice for myopia combined with moderate or high corneal astigmatism, which is not only for better centration, but also for slower axial growth and lower incidence of corneal staining. Further long-term prospective studies are required to affirm these results.
Acknowledgments
Authors' contributions: Zhang Y: concept and design, data acquisition, data analysis, drafting manuscript; Chen YG: concept and design, critical revision of manuscript, supervision, final approval.
Foundation: Supported by Capital's Funds for Health Improvement and Research (No.2018-2-4092).
Conflicts of Interest: Zhang Y, None; Chen YG, None.
REFERENCES
- 1.Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, Cook DG, Owen CG. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016;100(7):882–890. doi: 10.1136/bjophthalmol-2015-307724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lam CS, Lam CH, Cheng SC, Chan LY. Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over two decades. Ophthalmic Physiol Opt. 2012;32(1):17–24. doi: 10.1111/j.1475-1313.2011.00886.x. [DOI] [PubMed] [Google Scholar]
- 3.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 4.Shih KC, Chan TC, Ng AL, Lai JS, Li WW, Cheng AC, Fan DS. Use of atropine for prevention of childhood myopia progression in clinical practice. Eye Contact Lens. 2016;42(1):16–23. doi: 10.1097/ICL.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 5.Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90(6):530–539. doi: 10.1097/OPX.0b013e318293657d. [DOI] [PubMed] [Google Scholar]
- 6.Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93(9):1181–1185. doi: 10.1136/bjo.2008.151365. [DOI] [PubMed] [Google Scholar]
- 7.Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52(5):2170–2174. doi: 10.1167/iovs.10-5485. [DOI] [PubMed] [Google Scholar]
- 8.Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53(11):7077–7085. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 9.Swarbrick HA, Alharbi A, Watt K, Lum E, Kang P. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology. 2015;122(3):620–630. doi: 10.1016/j.ophtha.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 10.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R, Sugimoto K. Long-term efficacy of orthokeratology contact lens wear in controlling the progression of childhood myopia. Curr Eye Res. 2017;42(5):713–720. doi: 10.1080/02713683.2016.1221979. [DOI] [PubMed] [Google Scholar]
- 11.Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012;53(2):640–649. doi: 10.1167/iovs.11-7769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berntsen DA, Barr CD, Mutti DO, Zadnik K. Peripheral defocus and myopia progression in myopic children randomly assigned to wear single vision and progressive addition lenses. Invest Ophthalmol Vis Sci. 2013;54(8):5761–5770. doi: 10.1167/iovs.13-11904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152–1161. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 14.Cheung SW, Cho P, Chan B. Astigmatic changes in orthokeratology. Optom Vis Sci. 2009;86(12):1352–1358. doi: 10.1097/OPX.0b013e3181be06ff. [DOI] [PubMed] [Google Scholar]
- 15.Lyu B, Hwang KY, Kim SY, Kim SY, Na KS. Effectiveness of toric orthokeratology in the treatment of patients with combined myopia and astigmatism. Korean J Ophthalmol. 2016;30(6):434–442. doi: 10.3341/kjo.2016.30.6.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE Study) Invest Ophthalmol Vis Sci. 2013;54(10):6510–6517. doi: 10.1167/iovs.13-12527. [DOI] [PubMed] [Google Scholar]
- 17.Maseedupally VK, Gifford P, Lum E, Naidu R, Sidawi D, Wang B, Swarbrick HA. Treatment zone decentration during orthokeratology on eyes with corneal toricity. Optom Vis Sci. 2016;93(9):1101–1111. doi: 10.1097/OPX.0000000000000896. [DOI] [PubMed] [Google Scholar]
- 18.Chan B, Cho P, de Vecht A. Toric orthokeratology: a case report. Clin Exp Optom. 2009;92(4):387–391. doi: 10.1111/j.1444-0938.2009.00363.x. [DOI] [PubMed] [Google Scholar]
- 19.Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci. 2012;89(6):849–855. doi: 10.1097/OPX.0b013e318257c20f. [DOI] [PubMed] [Google Scholar]
- 20.Chen C, Cho P. Toric orthokeratology for high myopic and astigmatic subjects for myopic control. Clin Exp Optom. 2012;95(1):103–108. doi: 10.1111/j.1444-0938.2011.00616.x. [DOI] [PubMed] [Google Scholar]
- 21.Luo M, Ma S, Liang N. Clinical efficacy of toric orthokeratology in myopic adolescent with moderate to high astigmatism. Eye Sci. 2014;29(4) [PubMed] [Google Scholar]
- 22.Pauné J, Cardona G, Quevedo L. Toric double tear reservoir contact lens in orthokeratology for astigmatism. Eye Contact Lens. 2012;38(4):245–251. doi: 10.1097/ICL.0b013e318258789e. [DOI] [PubMed] [Google Scholar]
- 23.Tarutta EP, Verzhanskaya TY. Stabilizing effect of orthokeratology lenses (ten-year follow-up results) Vestn Oftalmol. 2017;133(1):49–54. doi: 10.17116/oftalma2017133149-54. [DOI] [PubMed] [Google Scholar]
- 24.Chen Z, Niu L, Xue F, Qu X, Zhou Z, Zhou X, Chu R. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012;89(11):1636–1640. doi: 10.1097/OPX.0b013e31826c1831. [DOI] [PubMed] [Google Scholar]
- 25.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutierrez-Ortega R. Orthokeratology vs spectacles: adverse events and discontinuations. Optom Vis Sci. 2012;89(8):1133–1139. doi: 10.1097/OPX.0b013e318263c5af. [DOI] [PubMed] [Google Scholar]
- 26.Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90(9):937–944. doi: 10.1097/OPX.0b013e31829cac92. [DOI] [PubMed] [Google Scholar]


