Abstract
Background
Previous studies suggest that immediate reconstruction following mastectomy produces superior results over delayed procedures. However, for medical or oncological reasons, some patients may be poor candidates for immediate reconstruction. We compared complications and patient-reported outcomes between immediate and delayed breast reconstructions in a prospective, multicenter study.
Methods
1957 patients (1806 immediate, 151 delayed) met eligibility criteria. Demographic data, major complications, infections, and reconstructive failure rates were evaluated. Patient-reported outcomes were assessed with BREAST-Q, PROMIS, and EORTC QLQ-BR23 surveys, pre- and two years postoperatively. Subscale scores were compared across cohorts using mixed-effects regression models, controlling for patient characteristics and hospitals.
Findings
Complete data were available in 1639 immediate and 147 delayed reconstruction patients. There were significant baseline differences between immediate and delayed cohorts in age, BMI, prevalence of diabetes, lymph node management, use of radiation, and chemotherapy. Controlling for clinical covariates, the delayed group had lower odds of any (OR 0.38, p < 0.001) and major (OR 0.52, p = 0.016) complications, compared with immediate patients. Furthermore, delayed reconstruction was associated with a significantly lower failure rates (6% vs. 1.3%, p = 0.032). However, multivariate analyses found no significant differences in patient satisfaction or in psychosocial, sexual, or physical well-being at two years.
Conclusions
Compared with immediate techniques, delayed reconstruction following mastectomy was associated with lower rates of overall and major complication, while providing equivalent patient satisfaction and quality of life benefits. Although immediate reconstruction is still the preferred choice of most patients and surgeons, delaying reconstruction does not appear to compromise clinical or patient-reported outcomes.
Keywords: Mastectomy, Immediate breast reconstruction, Delayed breast reconstruction, Patient reported outcomes, MROC, BREAST-Q
1. Introduction
Although breast conservation therapy is an effective option for patients with early stage breast cancer, many women still elect to undergo mastectomy for either cancer treatment or prophylaxis. Previous studies have shown that breast reconstruction and the associated improvement in body image positively impact health-related quality of life in women after mastectomy [1–4]. Although reconstruction can be carried out either at the time of mastectomy (“immediate”) or at a later time (“delayed”), immediate reconstruction has become more commonplace, due in part to reports showing superior overall aesthetic outcomes, higher levels of psychosocial well-being post-mastectomy, and lower costs, compared with delayed procedures [5–12]. Despite this recent trend, delayed reconstruction may still be advisable in women with significant medical comorbidities, planned post-mastectomy radiation therapy (PMRT), inflammatory breast cancer, or in patients emotionally unready to make well-informed decisions regarding immediate breast reconstruction. Psychological and emotional distress accompanying a recent breast cancer diagnosis may impair a patient’s decision-making capacity in this setting [13].
While a number of studies have compared complications rates and other clinical outcomes for immediate and delayed breast reconstruction [14–17], few investigators have evaluated the effects of reconstructive timing on patient reported outcomes (PROs). Of the studies analyzing PROs for immediate and delayed reconstruction, most have been limited by their retrospective, cross-sectional designs, small sample sizes, and failure to adequately control for confounding variables. A Cochrane review of all literature sources comparing immediate with delayed breast reconstruction found only one randomized, controlled trial, highlighting the need for more adequately powered studies focusing on clinical and psychological outcomes [18]. Therefore, the aim of the current multicenter analysis was to prospectively compare long-term complications and PROs for immediate and delayed breast reconstruction patients.
2. Methods
The Mastectomy Reconstruction Outcomes Consortium (MROC) Study used a prospective cohort design to evaluate patients from 11 academic and private practices in the United States and Canada. The project was funded by the National Cancer Institute (1R01CA152192) in 2011 and recruited patients from 2012 to 2015. Study centers were selected to encompass an ethnically and geographically diverse patient population. With Institutional Review Board approval at all sites, MROC recruited patients undergoing first time reconstruction after mastectomy for breast cancer treatment or prophylaxis. Patients with two-year complication and PRO survey data were included in the current analyses. Reconstructive procedure types included direct-to-implant (DTI), tissue expanders/implants (E/I), as well as latissimus dorsi (LD, with or without implants), pedicle transverse rectus abdominis musculocutaneous (PTRAM), free transverse rectus abdominis musculocutaneous (FTRAM), deep inferior epigastric perforator (DIEP), superior gluteal artery perforator (S-GAP), inferior gluteal artery perforator (I-GAP), and superficial inferior epigastric perforator (SIEA) flaps. Both immediate and delayed procedures, as well as unilateral and bilateral reconstructions were included.
Women electing to undergo breast reconstruction following complications of breast augmentation, mastopexy, breast reduction, or previous failed attempts at breast reconstruction were excluded from the study due to potential confounding by previous operations. Also excluded were those undergoing bilateral reconstructions with mixed reconstruction timing (i.e., immediate reconstruction on one breast and delayed reconstruction on the contralateral side) or mixed implant and autogenous reconstruction (other than latissimus dorsi). To avoid the confounding effects of recent surgery on PROs, tissue expander patients were included only if they were at least three months from their expander/implant exchange procedure. Finally, patients with failed reconstructions at any stage were also excluded from the PRO analysis, because the full PRO survey panel was not administered following failure of the reconstruction.
Demographic and clinical information was gathered preoperatively and one week postoperatively from the participants’ electronic medical records (EMRs). These data were uploaded onto a Velos eResearch System, a password secure data collection platform. Demographic variables collected included age, race, ethnicity, education, income, marital status, and employment status. Clinical variables included procedure type; timing (immediate versus delayed reconstruction); laterality (unilateral versus bilateral procedures); body mass index (BMI); lymph node management (sentinel node or axillary lymph node dissection); radiation; chemotherapy; diabetes; and smoking status.
One and two years following reconstruction, participants’ EMRs were reviewed again, to gather complication data. A complication was defined as an adverse postoperative, surgery-related event requiring additional treatment. Data were abstracted for each individual adverse event. Complications requiring re-hospitalization or re-operation were designated as “major”. Reconstructive failures, defined as complications necessitating implant or flap removal, were also recorded.
Study patients completed a web-based or paper survey pre-operatively, and at one and two years post-operatively. Of note, only two-year patient-reported outcomes (PRO) data are presented here. Patient reported outcomes data were assessed with the BREAST-Q, PROMIS-29, and EORTC QLQ-BR23 surveys. The BREAST-Q Reconstructive Module is a validated, condition-specific PRO instrument that has been widely used to measure health-related quality of life and satisfaction in breast reconstruction patients [19].1 The BREAST-Q subscales used in this analysis included Satisfaction with Breast, as well as Psychosocial, Physical, and Sexual Well-Being. The Patient-Report Outcomes Measurement Information System (PROMIS) is a self-administered survey for symptoms and other health outcomes in clinical practice [20].2 Subscales from PROMIS assessed in this analysis included Physical Function, Anxiety, Depression, Fatigue, Sleep Disturbance, Participation in Social Roles, and Pain. Finally, the European Organization for Research and Treatment of Cancer-Quality of Life Questionnaire—Breast (EORTC QLQ-BR23) is a breast cancer patient-specific, quality-of-life survey with demonstrated validity and reliability [21].3 The Body Image and Sexual Functioning Subscales from this instrument were included in the current analysis.
2.1. Statistical analysis
Patient characteristics by reconstruction timing (immediate vs. delayed) were analyzed using Student’s t tests for continuous variables and chi-square tests for categorical variables. Postoperative complication rates at two years following reconstruction were summarized by reconstruction timing. The complications were sorted into four categories: any complications, major complications, infection, and reconstruction failure. To compare complications between reconstruction timing cohorts, each subcategory of complication was separately modelled using a mixed-effects logistic regression model, with delayed versus immediate reconstruction timing as the primary predictor. The models were adjusted for patient age, race, BMI, procedure type, diabetes, laterality, radiation, chemotherapy, and lymph node management. We included centers (hospitals) as random intercepts to account for between-center variability.
Preoperative and two-year postoperative PROs were also summarized for immediate and delayed patients. Mixed-effects regression models were employed to compare PROs between the two cohorts while adjusting for preoperative differences in the characteristics potentially predictive of outcome differences. Each separate PRO measure model included reconstruction timing as the primary predictor and included the additional covariates described above for the complication models. The PRO models also included centers (hospitals) as random intercepts to account for between-center variability.
As described below, preoperative PROs differed significantly by reconstruction timing: that is, immediate patients in general had much higher PRO scores than delayed patients prior to reconstruction. Such differences were expected due to the negative impact of mastectomy on the quality of life among delayed patients. Since the variability of preoperative PRO scores was largely a reflection of timing itself and was expected, it was not meaningful to control for preoperative levels of PROs when comparing two-year outcomes between the two reconstruction timing cohorts. As a result, the mixed-effects regression models did not adjust for preoperative PRO scores.
Postoperative PRO scores, as well as certain covariate data, were missing for some patients. To account for such missing data, multiple imputations with chained equations were employed to create 10 complete, imputed data sets, each of which was used to run the regression models specified above. The results were then combined using Rubin’s rules [22]. Statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NC), and statistical significance was set at 0.05.
3. Results
A total of 1957 patients (1806 immediate, 151 delayed) met the eligibility criteria and were included in this study. Demographic and clinical characteristics of the immediate and delayed reconstruction cohorts are summarized in Table 1. In bivariate analyses, statistically significant differences between the cohorts were noted for all variables except race. Compared with immediate reconstructions, the delayed cohort was older and had higher BMIs and a greater prevalence of diabetes. Delayed patients were more likely to undergo autologous reconstructions and unilateral procedures. Finally, use of radiation therapy was more common in delayed patients, while axillary staging procedures (sentinel node biopsy or axillary lymph node dissection) were more common in immediate patients.
Table 1.
Clinical characteristics of patients overall and by reconstruction timing.
| Variable | Overall n = 1957 | Immediate n = 1806 (92.3%) | Delayed n = 151 (7.7%) | p-Value |
|---|---|---|---|---|
| Age, mean (SD) | 50.2 (9.9) | 49.9 (10.0) | 52.9 (8.5) | <0.001 |
| BMI, mean (SD) | 26.8 (5.7) | 26.5 (5.6) | 29.5 (5.8) | <0.001 |
| Race | ||||
| White | 1702 (88.1%) | 1574 (88.1%) | 128 (88.3%) | 0.309 |
| Black | 121 (6.3%) | 109 (6.1%) | 12 (8.3%) | |
| Other | 109 (5.6%) | 104 (5.8%) | 5 (3.4%) | |
| Procedure type | ||||
| Implant | 1302 (66.5%) | 1275 (70.6%) | 27 (17.9%) | <0.001 |
| Lat Dorsi | 63 (3.2%) | 45 (2.5%) | 18 (11.9%) | |
| Autologous | 592 (30.3%) | 486 (26.9%) | 106 (70.2%) | |
| Laterality | ||||
| Unilateral | 942 (48.1%) | 822 (45.5%) | 120 (79.5%) | <0.001 |
| Bilateral | 1015 (51.9%) | 984 (54.5%) | 31 (20.5%) | |
| Lymph node biopsy | ||||
| None | 377 (19.3%) | 247 (13.7%) | 130 (86.1%) | <0.001 |
| SLNB | 994 (50.8%) | 989 (54.8%) | 5 (3.3%) | |
| ALND | 586 (29.9%) | 570 (31.6%) | 16 (10.6%) | |
| Diabetes | ||||
| Yes | 87 (4.4%) | 71 (3.9%) | 16 (10.6%) | <0.001 |
| No | 1870 (95.6%) | 1735 (96.1%) | 135 (89.4%) | |
| Radiation | ||||
| Yes | 648 (33.1%) | 554 (30.7%) | 94 (62.3%) | <0.001 |
| No | 1309 (66.9%) | 1252 (69.3%) | 57 (37.7%) | |
| Chemotherapy | ||||
| During/after reconstruction | 655 (33.5%) | 649 (35.9%) | 6 (4.0%) | <0.001 |
| Not during/after reconstruction | 1302 (66.5%) | 1157 (64.1%) | 145 (96.0%) | |
At two years postoperatively, the immediate cohort had a significantly higher failure rate (6% vs.1.3%, p = 0.032), compared to delayed patients (Table 2). However, rates for any complications, major complications, any infections, and major infections were not significantly different between the two cohorts in bivariate analysis. However, controlling for demographic and clinical covariates, delayed reconstruction was associated with significantly lower odds of any complication (OR 0.38, p < 0.001) and of major complications (OR 0.52, p = 0.016, Table 3), compared with immediate procedures. Further interaction analysis between autologous and implant group showed that delayed autologous patients were at significantly lower risk of complications compared to immediate autologous patients, but this was not the case for implant patients. Stratified models did not converge due to the small cohort size of delayed implant patients.
Table 2.
Two year postoperative complication rate by reconstruction timing.
| Immediate | Delayed | Pa | |
|---|---|---|---|
| No. patients | 1806 | 151 | - |
| Any complication | 617 (34.2%) | 45 (29.8%) | 0.069 |
| Major complication | 419 (23.2%) | 32 (21.2%) | 0.221 |
| Any infection | 167 (9.3%) | 9 (6.0%) | 0.183 |
| Major infection | 90 (5.0%) | 6 (4.0%) | 0.549 |
| Failure | 108 (6%) | 2 (1.3%) | 0.032 |
Based on mixed-effects logistic regression model adjusting for sites (hospitals).
Table 3.
Mixed-effects logistic regression model for two year postoperative complication.
| Complication | Adjusted ORa (Delayed vs. Immediate) | 95% CI | p-Value |
|---|---|---|---|
| Two years post-op | |||
| Any complication | 0.38 | (0.24, 0.62) | <0.001 |
| Major complication | 0.52 | (0.31, 0.89) | 0.016 |
Each model included as covariates age, BMI, race, procedure type, laterality, lymph node biopsy, diabetes, radiation and chemotherapy; Also included are random intercepts for study sites (hospitals).
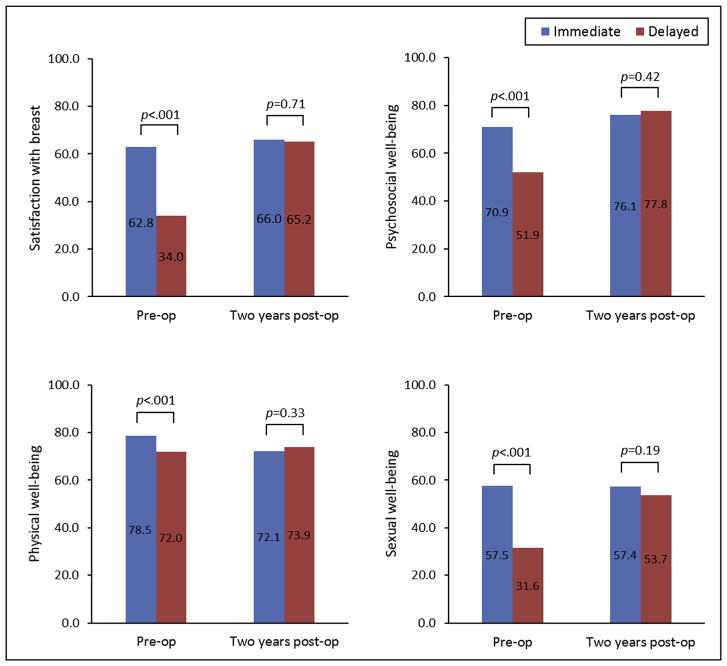
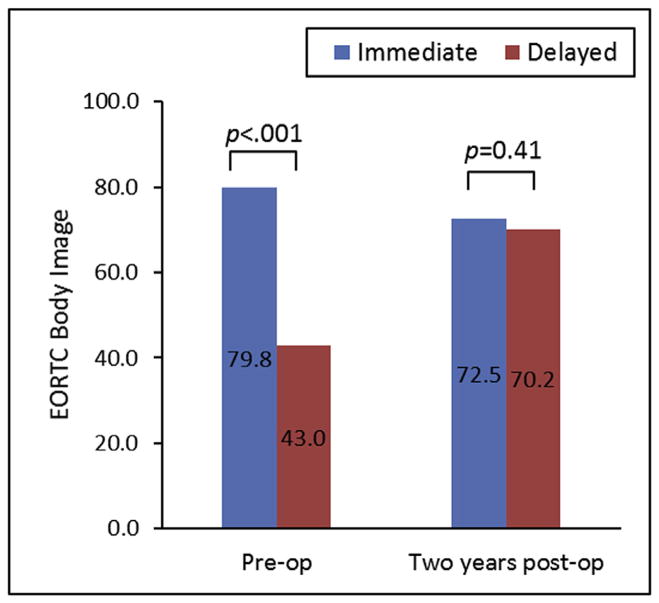
Of the 1957 patients, 108 immediate patients (6%) and two delayed patients (1.3%) failed initial reconstruction attempts, and 61 E/I patients had not been exchanged by three months prior to their two-year follow-up assessments. After excluding these patients, a total of 1786 patients (1639 immediate, 147 delayed) remained for PRO analysis. Mean pre- and two-year postoperative PRO subscale scores and associated bivariate analyses are summarized in Table 4. Compared with women undergoing immediate reconstruction, delayed patients scored significantly lower pre-operatively in all BREAST-Q subscales. On the PROMIS-29, the delayed cohort scored significantly lower for the Physical Function and Anxiety subscales and reported significantly greater pain prior to reconstruction, compared with the immediate group. Lastly, women undergoing delayed procedures fared significantly worse than immediate reconstruction patients on the pre-operative EORTC Body Image and Sexual Functioning subscales.
Table 4.
Unadjusted scores of patient-reported outcomes by immediate (n = 1639) and delayed (n = 147) timing.
| PRO measure | Timing | Pre-op | Two years post-op | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| na | Mean (SD) | p-Valueb | na | Mean (SD) | p-Valueb | ||
| BREAST-Q: Satisfaction with breast | Immediate | 1632 | 62.8 (21.1) | <0.001 | 1073 | 65.1 (18.1) | 0.559 |
| Delayed | 147 | 34.0 (16.3) | 96 | 66.2 (20.6) | |||
| BREAST-Q: Psychosocial well-being | Immediate | 1631 | 70.9 (17.9) | <0.001 | 1065 | 74.4 (19.0) | 0.159 |
| Delayed | 147 | 51.9 (15.1) | 96 | 77.3 (21.4) | |||
| BREAST-Q: Physical well-being | Immediate | 1632 | 78.5 (14.7) | <0.001 | 1061 | 76.3 (14.8) | 0.870 |
| Delayed | 147 | 72.0 (14.3) | 96 | 76.0 (14.4) | |||
| BREAST-Q: Sexual well-being | Immediate | 1585 | 57.5 (19.1) | <0.001 | 1026 | 54.8 (21.4) | 0.823 |
| Delayed | 146 | 31.6 (19.4) | 89 | 54.3 (23.5) | |||
| PROMIS: Physical function | Immediate | 1635 | 53.0 (6.7) | <0.001 | 1049 | 51.8 (6.8) | 0.276 |
| Delayed | 146 | 50.0 (7.5) | 93 | 51.0 (7.4) | |||
| PROMIS: Anxiety | Immediate | 1635 | 58.9 (8.8) | <0.001 | 1048 | 49.7 (9.0) | 0.024 |
| Delayed | 146 | 52.1 (9.7) | 94 | 47.5 (9.4) | |||
| PROMIS: Depression | Immediate | 1635 | 49.8 (8.4) | 0.852 | 1047 | 46.8 (7.8) | 0.383 |
| Delayed | 146 | 49.7 (9.1) | 94 | 46.1 (7.4) | |||
| PROMIS: Fatigue | Immediate | 1635 | 49.8 (9.9) | 0.938 | 1044 | 48.3 (10.0) | 0.477 |
| Delayed | 146 | 49.8 (9.5) | 94 | 49.1 (10.9) | |||
| PROMIS: Sleep disturbance | Immediate | 1632 | 52.0 (3.5) | 0.112 | 1046 | 52.1 (3.9) | 0.102 |
| Delayed | 146 | 52.5 (3.4) | 94 | 52.8 (3.8) | |||
| PROMIS: Satisfaction with participation in social roles | Immediate | 1635 | 51.8 (9.5) | 0.060 | 1046 | 52.9 (9.7) | 0.760 |
| Delayed | 146 | 50.3 (9.5) | 93 | 53.2 (10.9) | |||
| PROMIS: Pain interference | Immediate | 1635 | 45.9 (7.3) | <0.001 | 1047 | 46.4 (7.8) | 0.072 |
| Delayed | 146 | 48.6 (8.3) | 93 | 47.9 (8.5) | |||
| EORTC: Body image | Immediate | 1622 | 79.8 (23.0) | <0.001 | 1042 | 75.3 (24.6) | 0.971 |
| Delayed | 146 | 43.0 (30.1) | 93 | 75.4 (26.1) | |||
| EORTC: Sexual functioning | Immediate | 1614 | 32.0 (24.4) | 0.035 | 1037 | 31.7 (24.6) | 0.229 |
| Delayed | 147 | 27.6 (25.0) | 94 | 28.5 (25.4) | |||
The number of patients with complete PRO.
For the comparison of preoperative PROs between immediate and delayed group.
Adjusted mean cohort differences in PROs at two-year follow-ups are summarized in Table 5. Controlling for baseline demographic and clinical covariates, there were no statistically significant differences between the immediate and delayed reconstruction groups for any of the BREAST-Q, PROMIS-29, or EORTC QLQ-BR23 subscales.
Table 5.
Adjusted mean difference between reconstruction timing (delayed – immediate) in postoperative patient-reported outcomes.
| Adjusted Mean Differencea | 95% CI | p-Value | |
|---|---|---|---|
| BREAST-Q: Satisfaction with breast | −0.88 | (−5.52, 3.76) | 0.707 |
| BREAST-Q: Psychosocial well-being | 1.70 | (−2.39, 5.78) | 0.415 |
| BREAST-Q: Physical well-being | 1.76 | (−1.83, 5.35) | 0.333 |
| BREAST-Q: Sexual well-being | −3.70 | (−9.25, 1.85) | 0.188 |
| PROMIS: Physical function | −0.58 | (−2.01, 0.86) | 0.430 |
| PROMIS: Anxiety | −0.69 | (−2.77, 1.39) | 0.513 |
| PROMIS: Depression | −0.38 | (−2.19, 1.43) | 0.679 |
| PROMIS: Fatigue | 2.09 | (−0.13, 4.32) | 0.065 |
| PROMIS: Sleep disturbance | 0.24 | (−0.68, 1.16) | 0.612 |
| PROMIS: Satisfaction with participation in social roles | −0.71 | (−3.31, 1.90) | 0.590 |
| PROMIS: Pain interference | 0.20 | (−1.83, 2.24) | 0.842 |
| EORTC: Body image | −2.23 | (−7.52, 3.05) | 0.406 |
| EORTC: Sexual functioning | −2.79 | (−8.54, 2.95) | 0.337 |
Obtained from fitting a separate mixed-effects regression model with dependent variable being the corresponding patient-reported outcome. Each model included as covariates age, BMI, race, procedure type, laterality, lymph node biopsy, diabetes, radiation and chemotherapy. Also included are random intercepts for study sites (hospitals). Results were combined based on n = 10 imputation.
4. Discussion
In recent years, immediate breast reconstruction has become the preferred option over delayed techniques among surgeons in the United States. More than 70% of breast reconstructions in the U.S. are performed in conjunction with mastectomy [23]. Reflecting this preference, over 92% of patients in our study underwent immediate reconstruction. In all likelihood, the nationwide trend in the U.S. heavily favoring immediate reconstruction can be traced to several perceived benefits of this approach, including lower hospital costs [11,24–29], psychosocial and quality of life benefits in the immediate postoperative period [24,27], and potentially superior aesthetics [8]. With the widespread acceptance of skin sparing mastectomy, the native breast skin envelope is available in the immediate setting, which may facilitate better cosmetic outcomes.
Despite the benefits of immediate reconstruction, it may not be suitable for every patient. Delayed reconstruction may be preferable when post-mastectomy radiation therapy (PMRT) is required or in patients with significant medical comorbidities, making them poor surgical candidates. It is still the preference of many plastic surgeons and radiation oncologists to complete radiation therapy before reconstruction, based on reports of higher complication rates in patients who receive radiation therapy after immediate reconstruction, compared to women who undergo delayed reconstruction following PMRT [14,30–33]. Up to 47.5% of implant-based reconstruction patients undergoing radiation therapy may require revision reconstruction [34]. In other instances, reconstruction may be postponed due to patient preference. Patients may be unsure of reconstruction options or have family or job obligations which preclude the additional surgeries required for reconstruction. In other instances, the stress and anxiety of a recent breast cancer diagnosis may complicate patient decision-making for immediate breast reconstruction. Studies indicate that immediate reconstruction patients suffer from higher levels of anxiety than the delayed cohort at the time of reconstruction [35–38]. This added psychological burden may impair patients’ abilities to process information and to make informed choices [13].
Prior studies comparing complication rates between immediate and delayed reconstructions have shown mixed results [15–17,39]. Some conclude that delayed E/I reconstructions have lower rates of postoperative complications, including mastectomy flap necrosis, delayed wound healing, infection, and tissue fibrosis, compared to immediate reconstructions [14,39–43]. In addition, immediate reconstruction may be associated with higher rates of long-term complications [33]. Previous investigators have reported that immediate autologous reconstructions receiving PMRT are associated with higher complication rates than delayed autologous reconstructions performed after radiation therapy [14]. By contrast, other studies suggest that delayed reconstruction carries a higher overall risk of postoperative complications, compared with immediate reconstruction. A study using the ACS-NSQIP database from 2005 to 2012 concluded that both medical and surgical complications were more likely in delayed reconstructions, compared with immediate procedures [15].
Our study found that immediate reconstruction was associated with higher risks of both overall and major complications, including reconstructive failure, when compared with delayed procedures. However, infection rates appeared to be comparable between the two groups. Not surprisingly, we observed a lower rate of mastectomy skin flap necrosis in the delayed reconstruction group: Likely, the time interval between mastectomy and subsequent reconstruction allowed the mastectomy flaps to re-vascularize and recover from the initial trauma of the mastectomy. For these cases, the mastectomy may function as a preliminary surgical delay of the skin flaps, thereby making them more tolerant of being remobilized at the time of the delayed reconstruction. Finally, it bears mentioning that assessments of immediate reconstruction do not (and probably cannot) distinguish between mastectomy- and reconstruction-related complications. In essence, complication rates reported for immediate procedures actually describe outcomes for two operations. By contrast, complications in delayed reconstruction are attributable only to the reconstructive procedure. Thus, the combination of two operations (and longer operative times) in immediate reconstruction may explain in part the higher risk of complications observed for this cohort.
In this study, the immediate and delayed breast reconstruction cohorts included very different patient populations. As reflected in Table 1, the delayed group tended to be older and have more medical comorbidities, perhaps making them less ideal candidates for combined mastectomy and reconstruction. Previous studies have observed similar differences in the prevalence of medical comorbidities between delayed and immediate reconstruction groups [15]. Predictably, the delayed group in our analysis was also more likely to have received radiation, another common rationale for postponing reconstruction.
The preoperative differences between the two cohorts were even more striking for PROs: The preoperative survey results clearly demonstrate the adverse impact of mastectomy on psychosocial well-being, physical well-being, sexual functioning, and body image among the delayed cohort, when compared with the immediate group. These findings likely reflect fundamental differences in the clinical scenarios for immediate and delayed reconstruction patients—Women planning immediate reconstruction had not yet had mastectomies and consequently reported relatively higher levels of psychosocial, physical and sexual well-being. By contrast, patients seeking delayed reconstruction had been living with mastectomy scars and the associated psychological and emotional sequelae. The effects of mastectomy on psychosocial functioning and body image have been well-documented in previous studies [44–46]. Thus, the baseline differences we observed in PRO measures between the immediate and delayed reconstruction cohorts are readily explained by the presence or absence of an unreconstructed mastectomy scar.
Despite significant preoperative cohort differences, reconstruction timing had no significant effects on PROs at two years. Postoperatively, both the immediate and delayed cohorts’ unadjusted and adjusted BREAST-Q, PROMIS and EORTC-QLQ-BR23 subscale scores showed no statistically significant differences. These findings suggest that reconstruction either preserves or enhances quality of life and well-being, depending on whether reconstruction is carried out at the time of mastectomy or in a subsequent operation. When combined with mastectomy, reconstruction appears to lessen the adverse effects on psychosocial well-being and body image, in some ways constituting a “reverse mastectomy”. For women choosing delayed reconstruction, the procedure appears to reverse many of mastectomy’s adverse effects on quality of life. As summarized in Figs. 1 and 2, reconstruction appears to achieve comparable levels of satisfaction, psychosocial well-being, sexual well-being and body image, regardless of procedure timing.
Fig. 1.
Preoperative and Two Year Postoperative BREAST-Q Score by Reconstruction Timing. Despite statistically significant differences in patient-reported outcomes preoperatively between immediate and delayed breast reconstruction patients, both cohorts have equivalent quality of life and patient satisfaction at two years postoperatively.
Fig. 2.
Preoperative and Two Year Postoperative EORTC Body Image Score by Reconstruction Timing. The substantially negative body image perception of the delayed reconstruction patients become equivalent with the immediate breast reconstruction patients at two years postoperatively.
Our finding of lower complication rates with delayed reconstruction should not be misconstrued as a recommendation for routinely postponing reconstruction in women who are appropriate candidates for immediate procedures. We are not advocating a return to the decades-ago practice of forcing mastectomy patients to defer reconstruction for fear of recurrence or to reduce risks of complications. However, even with the current widespread acceptance of immediate reconstruction in most centers, there remain patients for whom delayed reconstruction is still the most appropriate choice. Although views on the advisability of immediate reconstruction in the face of post-mastectomy radiation therapy (PMRT) may be changing, many plastic surgeons still recommend delaying reconstruction in this setting to avoid adverse effects of radiation on implant-based or autogenous reconstructions [47,48]. Other women may choose to defer reconstruction for career- or family-related reasons. Finally, some newly-diagnosed breast cancer patients find choosing reconstructive options in parallel with cancer treatment decisions to be emotionally and psychologically overwhelming. In these scenarios, delayed reconstruction may still be the best answer. For women opting for this approach, it may be reassuring to know that delayed procedures achieve equivalent patient-reported outcomes with lower risks, compared to immediate reconstruction.
We believe this study is the first to compare immediate with delayed reconstruction using 1) a prospective, multicenter design; 2) a large study sample size; 3) patient reported outcome (PRO) assessments both preoperatively and postoperatively; 4) and long-term (two year) follow-up data. To date, the few published studies addressing this topic have had significant limitations. A previous report by Duraes and coworkers used the BREAST-Q to assess preoperative PROs in patients receiving immediate or delayed reconstruction, as well as in those undergoing breast reduction or non-breast reconstructive surgeries [49]. However, the investigators did not evaluate postoperative PROs. This study was also limited by its relatively small sample size of 141 immediate and 12 delayed reconstruction patients in a single center. Another report published by Zhong and colleagues evaluated 30 women undergoing immediate reconstruction and 76 women undergoing delayed reconstruction. This prospective study measured both preoperative and postoperative PROs, but was limited by its small sample size and its exclusion of implant-based procedures [50].
Despite its strengths, the current study has its limitations. Because of the growing prevalence of immediate reconstruction, our sample size of delayed reconstructions was relatively small at 151 patients. In total, 92.3% of our study population opted for immediate reconstruction. With a larger number of delayed reconstructions, it is possible that differences observed in the two-year PROs might have become statistically significant. However, closer examination of the mean two-year PRO subscale scores for the two cohorts (Table 4) shows the between-cohort differences in PROs to be small, and thus, a larger population of delayed patients likely would not have significantly impacted our results.
Another limitation of our study was potential selection bias, given the strong preferences for immediate or delayed reconstruction by both surgeons and patients. Although a randomized, controlled trial (RCT) may have controlled for this selection bias, randomization by procedure timing would have presented serious practical and ethical issues, and therefore was not attempted. Despite our use of multivariate analyses, our findings may have been confounded by unknown clinical or demographic variables. Also, patients undergoing reconstruction are self-selected—women whose qualities of life are most severely impacted by mastectomy are also most likely to choose reconstruction. They are not necessarily representative of all mastectomy patients. Finally, our findings may not be generalizable to all patients in all practice settings, since nine of the study sites were academic centers, and all eleven were located in North America. Other practice settings in other geographic regions or cultures may achieve different clinical or quality of life outcomes after breast reconstruction.
5. Conclusion
This prospective multicenter study observed that delayed reconstruction was associated with significantly lower risks of overall or major complications, compared with immediate procedures. Although immediate and delayed reconstruction patients reported vastly different preoperative levels of quality of life, there were no significant differences by procedure timing in patient-reported outcomes at two years following reconstruction. Immediate reconstruction appeared to preserve patients’ preoperative psychosocial functioning, while delayed reconstruction produced substantial improvements in these measures. Based on these findings, we conclude that both immediate and delayed mastectomy reconstruction provide substantial quality of life benefits for women choosing these procedures. Furthermore, patients who postpone reconstruction after mastectomy due to personal preference or by medical necessity can be reassured that this approach is a safe alternative to immediate reconstruction and can provide equivalent quality of life and body image benefits.
Acknowledgments
Funding source
National Cancer Institute (1R01CA152192).
Footnotes
Developed in 1996 by Pusic et al., the BREAST-Q measures patient satisfaction in a total of 6 domains including satisfaction with breasts, overall outcome, process of care, psychosocial, physical, and sexual well-being.
The development of PROMIS in 2004 was funded by the National Institutes of Health to revolutionize the assessment of patient reported outcomes for both patient research and clinical practice. It assesses physical health including physical function, physical symptoms, sleep function, and sexual function as well as mental health (emotional distress, cognitive function, positive psychological function).
The EORTC QLQ-BR23, developed by the European Organization for Research and Treatment of Cancer in 1995, consists of 23 questions that assess symptoms and side effects related to treatment modalities, body image, and sexuality.
- Alfred Yoon: literature search, study design, data analysis, data interpretation, writingmaterials-methods.
- Ji Qi: Data collection, figures, tables, data analysis, writing.
- David Brown: data analysis, data interpretation, writing, conception of project.
- Hyungjin Kim: Data collection, data analysis, data interpretation, writing.
- Jennifer Hamill: data analysis, study design, data interpretation, writingmaterials-methods.
- Jessica Erdmann-Sager: data interpretation, writing.
- Andrea Pusic: study design, data analysis, data interpretation, conception of projectmaterials-methods.
- Edwin Wilkins: literature search, study design, data analysis, data interpretation, writing, conception of projectmaterials-methods.
Conflict of interest statement
Dr. Pusic is a co-developer of the BREAST-Q which is owned by Memorial Sloan Kettering Cancer Center and she receives a portion of the licensing fees. The other authors have no conflicts of interest to disclose.
Ethical approval
Ethical consent not required. IRB approved from all 11 MROC study sites.
References
- 1.Chao LF, Patel KM, Chen SC, Lam HB, Lin CY, Liu HE, et al. Monitoring patient-centered outcomes through the progression of breast reconstruction: a multicentered prospective longitudinal evaluation. Breast Cancer Res Treat. 2014;146(2):299–308. doi: 10.1007/s10549-014-3022-7. [DOI] [PubMed] [Google Scholar]
- 2.Falk Dahl CA, Reinertsen KV, Nesvold IL, Fossa SD, Dahl AA. A study of body image in long-term breast cancer survivors. Cancer. 2010;116(15):3549–57. doi: 10.1002/cncr.25251. [DOI] [PubMed] [Google Scholar]
- 3.Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. J Clin Oncol. 2005;23(15):3322–30. doi: 10.1200/JCO.2005.05.130. [DOI] [PubMed] [Google Scholar]
- 4.Shimozuma K, Ganz PA, Petersen L, Hirji K. Quality of life in the first year after breast cancer surgery: rehabilitation needs and patterns of recovery. Breast Cancer Res Treat. 1999;56(1):45–57. doi: 10.1023/a:1006214830854. [DOI] [PubMed] [Google Scholar]
- 5.Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 2000;26(1):17–9. doi: 10.1053/ejso.1999.0733. [DOI] [PubMed] [Google Scholar]
- 6.Wellisch DK, Schain WS, Noone RB, Little JW., 3rd Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg. 1985;76(5):713–8. doi: 10.1097/00006534-198511000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Stevens LA, McGrath MH, Druss RG, Kister SJ, Gump FE, Forde KA. The psychological impact of immediate breast reconstruction for women with early breast cancer. Plast Reconstr Surg. 1984;73(4):619–28. doi: 10.1097/00006534-198404000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Kroll SS, Coffey JA, Jr, Winn RJ, Schusterman MA. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg. 1995;96(4):860–4. doi: 10.1097/00006534-199509001-00015. [DOI] [PubMed] [Google Scholar]
- 9.Dean C, Chetty U, Forrest AP. Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet. 1983;1(8322):459–62. doi: 10.1016/s0140-6736(83)91452-6. [DOI] [PubMed] [Google Scholar]
- 10.Elkowitz A, Colen S, Slavin S, Seibert J, Weinstein M, Shaw W. Various methods of breast reconstruction after mastectomy: an economic comparison. Plast Reconstr Surg. 1993;92(1):77–83. doi: 10.1097/00006534-199307000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Khoo A, Kroll SS, Reece GP, Miller MJ, Evans GR, Robb GL, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg. 1998;101(4):964–8. doi: 10.1097/00006534-199804040-00011. [DOI] [PubMed] [Google Scholar]
- 12.Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg. 2008;60(5):568–72. doi: 10.1097/SAP.0b013e31815b6ced. [DOI] [PubMed] [Google Scholar]
- 13.Ananthakrishnan P, Lucas A. Options and considerations in the timing of breast reconstruction after mastectomy. Cleve Clin J Med. 2008;75(1):S30–3. doi: 10.3949/ccjm.75.suppl_1.s30. [DOI] [PubMed] [Google Scholar]
- 14.Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving post-mastectomy radiation therapy. Plast Reconstr Surg. 2001;108(1):78–82. doi: 10.1097/00006534-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Sanati-Mehrizy P, Massenburg BB, Rozehnal JM, Gupta N, Rosa JH, Ingargiola MJ, et al. A comparison of postoperative outcomes in immediate versus delayed reconstruction after mastectomy. Eplasty. 2015;30(15) [PMC free article] [PubMed] [Google Scholar]
- 16.Fischer JP, Wes AM, Tuggle CT, Wu LC. Venous thromboembolism risk in mastectomy and immediate breast reconstruction: analysis of the 2005 to 2011 American College of Surgeons National Surgical Quality Improvement Program data sets. Plast Reconstr Surg. 2014;133(3):22. doi: 10.1097/01.prs.0000438062.53914.22. [DOI] [PubMed] [Google Scholar]
- 17.Fischer JP, Tuggle CT, Au A, Kovach SJ. A 30-day risk assessment of mastectomy alone compared to immediate breast reconstruction (IBR) J Plast Surg Hand Surg. 2014;48(3):209–15. doi: 10.3109/2000656X.2013.865633. [DOI] [PubMed] [Google Scholar]
- 18.D’Souza N, Darmanin G, Fedorowicz Z. Immediate versus delayed reconstruction following surgery for breast cancer. Cochrane Database Syst Rev. 2011;6(7) doi: 10.1002/14651858.CD008674.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345–53. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 20.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. Initial adult health item banks and first wave testing of the patient-reported outcomes measurement information System (PROMIS(™)) network: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. 1996;14(10):2756–68. doi: 10.1200/JCO.1996.14.10.2756. [DOI] [PubMed] [Google Scholar]
- 22.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; 2004. [Google Scholar]
- 23.2015 reconstructive breast procedures. American Society of Plastic Surgeons; 2015. 2015 Plastic Surgery Statistics Report. [Google Scholar]
- 24.Chevray PM. Timing of breast reconstruction: immediate versus delayed. Cancer J. 2008;14(4):223–9. doi: 10.1097/PPO.0b013e3181824e37. [DOI] [PubMed] [Google Scholar]
- 25.Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan breast reconstruction outcome study. Plast Reconstr Surg. 2000;106(5):1014–25. doi: 10.1097/00006534-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg. 2004;114(4):950–60. doi: 10.1097/01.prs.0000133200.99826.7f. [DOI] [PubMed] [Google Scholar]
- 27.Elder EE, Brandberg Y, Bjorklund T, Rylander R, Lagergren J, Jurell G, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14(3):201–8. doi: 10.1016/j.breast.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Carnevale A, Scaringi C, Scalabrino G, Campanella B, Osti MF, De Sanctis V, et al. Radiation therapy after breast reconstruction: outcomes, complications, and patient satisfaction. Radiol Med. 2013;118(7):1240–50. doi: 10.1007/s11547-013-0947-6. [DOI] [PubMed] [Google Scholar]
- 29.Hussien M, Salah B, Malyon A, Wieler-Mithoff EM. The effect of radiotherapy on the use of immediate breast reconstruction. Eur J Surg Oncol. 2004;30(5):490–4. doi: 10.1016/j.ejso.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Williams JK, Carlson GW, Bostwick J, 3rd, Bried JT, Mackay G. The effects of radiation treatment after TRAM flap breast reconstruction. Plast Reconstr Surg. 1997;100(5):1153–60. doi: 10.1097/00006534-199710000-00013. [DOI] [PubMed] [Google Scholar]
- 31.von Smitten K, Sundell B. The impact of adjuvant radiotherapy and cytotoxic chemotherapy on the outcome of immediate breast reconstruction by tissue expansion after mastectomy for breast cancer. Eur J Surg Oncol. 1992;18(2):119–23. [PubMed] [Google Scholar]
- 32.Forman DL, Chiu J, Restifo RJ, Ward BA, Haffty B, Ariyan S. Breast reconstruction in previously irradiated patients using tissue expanders and implants: a potentially unfavorable result. Ann Plast Surg. 1998;40(4):360–3. doi: 10.1097/00000637-199804000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Lee M, Reinertsen E, McClure E, Liu S, Kruper L, Tanna N, et al. Surgeon motivations behind the timing of breast reconstruction in patients requiring postmastectomy radiation therapy. J Plast Reconstr Aesthet Surg. 2015;68(11):1536–42. doi: 10.1016/j.bjps.2015.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg. 2000;105(3):930–42. doi: 10.1097/00006534-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 35.Handel N, Silverstein MJ, Waisman E, Waisman JR. Reasons why mastectomy patients do not have breast reconstruction. Plast Reconstr Surg. 1990;86(6):1118–22. [PubMed] [Google Scholar]
- 36.Harcourt DM, Rumsey NJ, Ambler NR, Cawthorn SJ, Reid CD, Maddox PR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg. 2003;111(3):1060–8. doi: 10.1097/01.PRS.0000046249.33122.76. [DOI] [PubMed] [Google Scholar]
- 37.Hopwood P. The assessment of body image in cancer patients. Eur J Cancer. 1993;2:276–81. doi: 10.1016/0959-8049(93)90193-j. [DOI] [PubMed] [Google Scholar]
- 38.Roth RS, Lowery JC, Davis J, Wilkins EG. Quality of life and affective distress in women seeking immediate versus delayed breast reconstruction after mastectomy for breast cancer. Plast Reconstr Surg. 2005;116(4):993–1002. doi: 10.1097/01.prs.0000178395.19992.ca. [DOI] [PubMed] [Google Scholar]
- 39.Seth AK, Silver HR, Hirsch EM, Kim JY, Fine NA. Comparison of delayed and immediate tissue expander breast reconstruction in the setting of post-mastectomy radiation therapy. Ann Plast Surg. 2015;75(5):503–7. doi: 10.1097/SAP.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 40.Anavekar NS, Rozen WM, Le Roux CM, Ashton MW. Achieving autologous breast reconstruction for breast cancer patients in the setting of post-mastectomy radiotherapy. J Cancer Surviv. 2011;5(1):1–7. doi: 10.1007/s11764-010-0155-5. [DOI] [PubMed] [Google Scholar]
- 41.Behranwala KA, Dua RS, Ross GM, Ward A, A’Hern R, Gui GP. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg. 2006;59(10):1043–51. doi: 10.1016/j.bjps.2006.01.051. [DOI] [PubMed] [Google Scholar]
- 42.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in post-mastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109(7):2265–74. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 43.Berry T, Brooks S, Sydow N, Djohan R, Nutter B, Lyons J, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;3:202–10. doi: 10.1245/s10434-010-1261-3. [DOI] [PubMed] [Google Scholar]
- 44.Bransfield DD. Breast cancer and sexual functioning: a review of the literature and implications for future research. Int J Psychiatry Med. 1982;12(3):197–211. doi: 10.2190/bjv3-bw2a-87ba-mqy6. [DOI] [PubMed] [Google Scholar]
- 45.Asken MJ. Psychoemotional aspects of mastectomy: a review of recent literature. Am J Psychiatr. 1975;132(1):56–9. doi: 10.1176/ajp.132.1.56. [DOI] [PubMed] [Google Scholar]
- 46.Silberfarb PM, Maurer LH, Crouthamel CS. Psychosocial aspects of neoplastic disease: I. Functional status of breast cancer patients during different treatment regimens. Am J Psychiatr. 1980;137(4):450–5. doi: 10.1176/ajp.137.4.450. [DOI] [PubMed] [Google Scholar]
- 47.Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011;127(1):15–22. doi: 10.1007/s10549-011-1401-x. [DOI] [PubMed] [Google Scholar]
- 48.Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg. 2009;124(2):395–408. doi: 10.1097/PRS.0b013e3181aee987. [DOI] [PubMed] [Google Scholar]
- 49.Duraes EF, Durand P, Duraes LC, Orra S, Moreira-Gonzalez A, Sousa JB, et al. Comparison of preoperative quality of life in breast reconstruction, breast aesthetic and non-breast plastic surgery patients: a cross-sectional study. J Plast Reconstr Aesthet Surg. 2016;7(16):30200–5. doi: 10.1016/j.bjps.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 50.Zhong T, Hu J, Bagher S, Vo A, O’Neill AC, Butler K, et al. A comparison of psychological response, body image, sexuality, and quality of life between immediate and delayed autologous tissue breast reconstruction: a prospective long-term outcome study. Plast Reconstr Surg. 2016;138(4):772–80. doi: 10.1097/PRS.0000000000002536. [DOI] [PubMed] [Google Scholar]