Abstract
Purpose
To estimate the rate of surgical treatment of paediatric proximal humerus fractures over time utilizing a large, publicly available national database.
Methods
The Healthcare Cost and Utilization Project Kids’ Inpatient Database was evaluated between the years 2000 and 2012. Proximal humerus fractures were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9 CM) diagnosis codes. ICD-9 CM procedure codes were used to identify patients who received surgical treatment. Univariable and multivariable logistic regression were used to determine variables associated with greater proportions of surgical treatment. All statistical analyses were performed utilizing SAS statistical software v.9.4. Statistical significance was set at p < 0.05.
Results
A total of 7520 proximal humerus fracture admissions were identified; 3247 (43.2%) were treated surgically. The percentage of patients receiving surgery increased from 39.3% in 2000 to 46.4% in 2012 (p < 0.001). After adjustment for potential confounders, increased age, increased ICD-9 derived injury severity scores (ICISS) and more recent year were associated with an increased proportion of patients receiving surgical treatment (p < 0.001). Medicaid payer status (p < 0.001) and admission to a children’s hospital (p = 0.045) were associated with a lower proportion of surgical treatment.
Conclusion
The rate of operative treatment of paediatric proximal humerus fractures increased over time between 2000 and 2012. Increased surgical rates were independently associated with older age, increased ICISS, treatment at a non-children’s hospital and non-Medicaid insurance status. Further study is needed to provide evidence to support improved outcomes after operative treatment of paediatric proximal humerus fractures.
Level of Evidence IV
Keywords: Trauma, shoulder, child
Introduction
Fractures of the proximal humerus account for approximately 2% of all fractures in paediatric patients.1,2 The pattern and displacement of these fractures is often influenced by the patient’s age and mechanism of injury.2 The majority (85%) of paediatric proximal humerus fractures are nondisplaced or minimally displaced.3 Additionally, the remodelling potential of the proximal humerus is substantial since the proximal humeral physis accounts for 80% of the longitudinal growth of the humerus. Therefore, the standard for the management of these nondisplaced or minimally displaced fractures is non-surgical.3 In contrast, the management of significantly displaced fractures remains controversial, particularly in adolescents who may have limited remaining growth and remodelling potential.3
There is a limited amount of literature directly comparing the effectiveness of non-operative with operative treatment for significantly displaced proximal humerus fractures in children and adolescents. Despite this, there are increasing reports of good results with operative management.3–10 The purpose of this study was to estimate the rate of surgical treatment of paediatric proximal humerus fractures over time, utilizing a large, publicly available national database. We hypothesized that the rate of operative treatment is increasing and that certain demographic factors are associated with increased rates of surgery.
Materials and methods
The Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID) is the largest publicly-available all-payer paediatric inpatient database that is compiled, and is based on two to three million annual hospital stays within the United States.11 The database is a result of data collected in the 46 states that have partnered with the Agency for Healthcare Research and Quality and maintain statewide data collection efforts. The database is a sample of all discharges at all of the hospitals in participating states. The large sample size generates data that is generalizable to the national paediatric population.
Paediatric proximal humerus fractures were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9 CM) diagnosis codes; open fracture codes were excluded. ICD-9 CM procedure codes were used to identify patients who received surgical treatment between the years 2000 and 2012. The demographic characteristics collected included sex, age (stratified into age groups of 0 to four, five to nine, ten to 14 and 15 to 20 years old), insurance status (Medicaid, private, self-pay, other) and ICD-9 derived injury severity score (ICISS).12 Hospital-related data collected included hospital type (children’s, general). Standard error and 95% confidence limits were calculated for all variables.
Multivariable logistic regression was used to determine variables associated with greater proportion of surgical treatment. All statistical analyses were performed utilizing SAS statistical software v.9.4 (SAS Institute, Inc. Cary, North Carolina). Statistical significance was set at p < 0.05.
Results
Table 1 represents the demographic characteristics of patients who were identified as having sustained a proximal humerus fracture. In all, 7520 proximal humerus fracture admissions were identified (average 1504 per year queried), with 3247 (43.2%) of these patients treated surgically (Table 2). The percentage of patients receiving surgery to treat proximal humerus fractures increased from 39.3% in 2000 to 46.4% in 2012 (p < 0.001), with the percentage increasing each year (Fig. 1). Of admitted patients with proximal humerus fractures, 64.1% were male and 35.9% were female; 44.9% of male patients were managed surgically, compared with 40.2% of female patients. Surgical management of these fractures was performed in 7.5% of 0- to four-year-old children, 29.3% of five- to nine-year-old children, 51.5% of ten- to 14-year-old children and 51.8% of 15- to 20-year-old children. Patients insured with Medicaid were managed surgically 32.7% of the time, while 47.3% of patients with private, self-pay or other insurance were managed surgically. Surgically treated patients had increased injury severity, with mean ICISS of 0.951 (range 0.001 to 0.999; standard error 0.002), compared with mean ICISS of 0.915 (range 0.001 to 0.999; standard error 0.003) in non-surgically managed patients (p < 0.001). In all, 29.3% of patients admitted to a children’s hospital were managed surgically, while 45.4% of patients receiving care at a general hospital were managed surgically.
Table 1.
Demographics of proximal humerus fracture patients
| Variable | Value | National estimate of patients | Fracture population (%) | 95% confidence interval |
|---|---|---|---|---|
| Sex | Male | 4828 | 64.19 | 62.62 to 65.77 |
| Female | 2693 | 35.81 | 34.23 to 37.38 | |
| Age (yrs) | 0 to 4 | 1034 | 13.75 | 12.50 to 15.01 |
| 5 to 9 | 820 | 10.91 | 9.89 to 11.92 | |
| 10 to 14 | 2453 | 32.62 | 31.03 to 34.22 | |
| 15 to 20 | 3212 | 42.72 | 40.65 to 44.78 | |
| Hospital type | Children’s hospital | 1036 | 13.77 | 11.57 to 15.97 |
| General hospital | 6485 | 86.23 | 84.03 to 88.43 | |
| Insurance status | Medicaid | 2142 | 28.49 | 26.76 to 30.21 |
| Private/self-pay/other | 5378 | 71.51 | 69.79 to 73.24 | |
| Yr | 2000 | 1909 | 25.39 | 23.23 to 27.55 |
| 2003 | 1570 | 20.87 | 19.39 to 22.35 | |
| 2006 | 1493 | 19.85 | 18.33 to 21.36 | |
| 2009 | 1385 | 18.42 | 17.03 to 19.80 | |
| 2012 | 1164 | 15.48 | 13.94 to 17.01 | |
| Total | 7520 | 100 |
Table 2.
Percentage of patients treated surgically by demographic
| Variable | Value | Treated surgically (%) | 95% confidence interval |
|---|---|---|---|
| Sex | Male | 44.85 | 42.66 to 47.04 |
| Female | 40.17 | 37.32 to 43.02 | |
| Age (yrs) | 0 to 4 | 7.47 | 5.46 to 9.48 |
| 5 to 9 | 29.34 | 24.78 to 33.90 | |
| 10 to 14 | 51.51 | 48.59 to 54.44 | |
| 15 to 20 | 51.84 | 49.25 to 54.43 | |
| Hospital type | Children’s hospital | 29.33 | 24.89 to 33.76 |
| General hospital | 45.39 | 43.34 to 47.43 | |
| Insurance status | Medicaid | 32.72 | 29.94 to 35.51 |
| Private/self-pay/other | 47.34 | 45.13 to 49.54 | |
| Yr | 2000 | 39.34 | 34.83 to 43.84 |
| 2003 | 41.91 | 38.44 to 45.39 | |
| 2006 | 44.15 | 40.71 to 47.58 | |
| 2009 | 46.12 | 42.94 to 49.30 | |
| 2012 | 46.41 | 42.44 to 50.39 | |
| Overall | 43.17 | 41.29 to 45.06 |
Fig. 1.
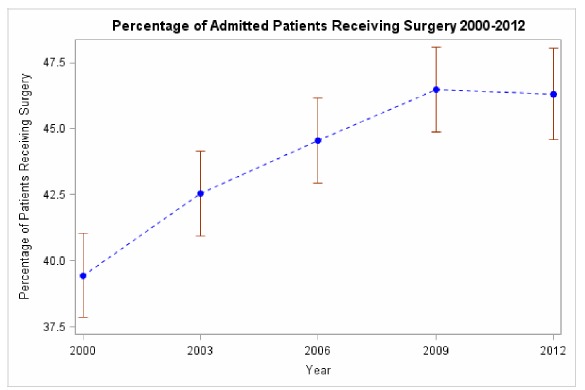
Percent of admitted patients treated surgically between 2000 and 2012.
After multivariable logistic regression to correct for confounding variables, increased age (Fig. 2, Table 2) and more recent year (Fig. 1, Table 2) were associated with a statistically significant increase in the proportion of patients receiving surgical treatment (p < 0.001). Increased injury severity was also associated with increased proportion of surgical treatment (p < 0.001). Medicaid payer status (p < 0.001) and admission to a children’s hospital (p = 0.0345) were associated with a lower proportion of surgical treatment. Patient sex (p = 0.443) was not associated with differing rates of surgical treatment.
Fig. 2.
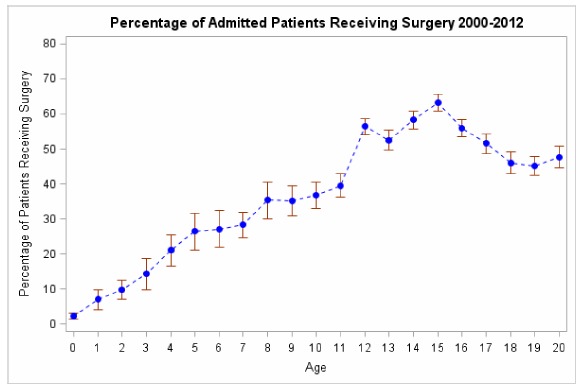
Percentage of admitted patients treated surgically by age.
Discussion
In this study, we found that over a ten-year period, the annual percentage of surgical management of paediatric proximal humerus fractures increased significantly from 39.4% in 2000 to 46.3% in 2012 (p < 0.001). This increase in surgical management corresponds to the time period in which several publications reported favourable outcomes after surgical management of paediatric proximal humerus fractures.3,7–9,13,14 These investigations may have expanded the relative indications for surgical intervention, which may in turn be reflected in national trends of surgical management for paediatric proximal humerus fractures.
The Neer-Horwitz classification system is commonly used to describe paediatric proximal humerus fractures.1,2 It divides paediatric proximal humerus fractures into four grades. Grade I includes fractures with < 5 mm of displacement of the proximal humerus relative to the shaft. Grade II includes fractures that are displaced less than one-third of the width of the shaft. Grade III fractures are displaced two-thirds of the width of the shaft. Grade IV fractures are displaced greater that two-thirds of the width of the shaft. Neer-Horwitz Grade III and IV fractures are associated with higher energy mechanisms of injury and higher degrees of fracture instability.3,15 Several authors have set variable thresholds for surgical management of these fractures and there is a lack of consensus among published studies.3,4,7,9,13,15,16 Additionally, there are few if any high-quality, comparative outcomes studies examining operative versus non-operative management of these injuries in children.8,10
Although there is not one universal displacement or angulation cutoff for operative intervention, the literature suggests that operative intervention should be considered in patients with: 1) Neer-Horwitz Grade III or IV fractures, 2) fractures that are > 60° angulated in patients less than ten years old, and 3) > 30° angulated in patients equal to or more than ten years old. As publications in the last decade have reported good outcomes following operative intervention for Neer-Horwitz Grade III or IV paediatric proximal humerus fractures, this may at least partly account for the increased rate of operative treatment for paediatric proximal humerus fractures found in our study, since patients with higher ICISS scores were more likely to undergo surgical treatment. Presumably, higher ICISS scores are associated with more severe fractures, although we could not directly comment on fracture severity given the limitations of the dataset studied.
Pahlavan et al8 performed a systematic review in an attempt to determine the optimal indications for surgical intervention for paediatric proximal humerus fractures. After applying their inclusion and exclusion criteria, 14 studies were included, and all were uncontrolled cases series (Level IV). The authors recommended that cases of paediatric proximal humerus fractures should be divided into three groups: younger than ten years old, ten to 13 years old and those older than 13 years. They concluded that children less than ten years old can generally be treated nonoperatively, except when the fracture is open or there is neurovascular compromise. Children > 13 years old should be offered surgery to restore anatomical alignment if the amount of displacement or angulation of their fracture warrants surgical intervention (although the threshold amount of displacement and angulation remains poorly defined). Those between ten and 13 years old should be managed on a case-by-case basis. These recommendations correspond to the remodelling capacity of the proximal humerus associated with each age group. The quality of recommendations remains relatively poor and this stems from the limited evidence in the literature.
Our data show that increased patient age is an independent predictor of surgical treatment for proximal humerus fractures. This is expected since the limited literature on the topic supports surgical treatment for older patients. Despite the lack of clear guidelines or comparative outcome studies in paediatric patients with proximal humerus fractures, however, the rate of surgical intervention is also increasing as a function of time. This finding is similar to other studies examining paediatric upper extremity injuries.17–20 Whether surgical treatment results in better outcomes compared with non-surgical treatment in these injuries is certainly unclear and conducting high-quality comparative outcomes studies such as randomized controlled trials (RCT) would be the optimal method to justify one treatment approach over the other. Conducting RCTs in this patient population, however, is logistically difficult and may be ethically questionable since children represent a vulnerable population. Retrospective comparison with matched cohorts is more ethically justifiable and logistically feasible, however, finding appropriately matched cohorts is also challenging.
The strengths of our investigation include the large, national patient sample size, which renders the results generalizable to the national paediatric population and the multivariable regression modelling we conducted to eliminate potential confounding factors that may have influenced our results. The HCUP-KID has been used in multiple other publications representing a variety of medical and surgical disciplines.21–25 There are, however, several limitations to this investigation. First, like any large national database, the HCUP-KID depends on the quality of data entered and is at risk of coding misclassification. Secondly, we were not able to extract particular fracture characteristics, which limits our ability to fully understand how many of the annual admitted paediatric proximal humerus fractures warranted surgical intervention. For example, it is impossible to determine what proportion of fractures were epiphyseal nor was it possible to determine fracture pattern or severity because of the inherent limitations of the coded data in the database. Thirdly, no outcome data was available and therefore we cannot conclude whether surgical treatment for these injuries results in better outcomes. Fourthly, our multivariable logistic regression model is limited by the variables recorded and available for analysis. Finally, the database used in this study only accounts for hospital admissions/discharges. Patients with injuries that did not necessitate admission would not have been captured in this sample which may represent a significant volume since most paediatric proximal humerus fractures can be treated in an outpatient setting.
In conclusion, this investigation found that the rate of operative treatment of paediatric proximal humerus fractures increased over time between 2000 and 2012. Increased surgical rates were associated with older age, treatment at a non-children’s hospital, higher ICISS and non-Medicaid insurance status. Further study is needed to provide evidence to support improved outcomes after operative treatment of paediatric proximal humerus fractures.
COMPLIANCE WITH ETHICAL STANDARDS
FUNDING STATEMENT
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA LICENCE TEXT
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
ETHICAL STATEMENT
Informed consent: This study used publicly available, de-identified data from human subjects. No informed consent was required.
ICMJE CONFLICT OF INTEREST STATEMENT
AHD is a paid consultant for Stryker, Globus, Depuy and Orthofix, receives research support from Orthofix and is an unpaid consultant for Osseous. CPE reports personal fees from Globus Medical and Stryker, outside the submitted work. All other authors declare no conflict of interest.
REFERENCES
- 1.Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B 1997;6:79-83. [DOI] [PubMed] [Google Scholar]
- 2.Popkin CA, Levine WN, Ahmad CS. Evaluation and management of pediatric proximal humerus fractures. J Am Acad Orthop Surg 2015;23:77-86. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez FF, Eberhardt O, Langendörfer M, Wirth T. Treatment of severely displaced proximal humeral fractures in children with retrograde elastic stable intramedullary nailing. Injury 2008;39:1453-1459. [DOI] [PubMed] [Google Scholar]
- 4.Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J Pediatr Orthop 2011;31:617-622. [DOI] [PubMed] [Google Scholar]
- 5.Schwendenwein E, Hajdu S, Gaebler C, Stengg K, Vécsei V. Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg 2004;14:51-55. [DOI] [PubMed] [Google Scholar]
- 6.Di Gennaro GL, Spina M, Lampasi M, Libri R, Donzelli O. Fractures of the proximal humerus in children. Chir Organi Mov 2008;92:89-95. [DOI] [PubMed] [Google Scholar]
- 7.Bahrs C, Zipplies S, Ochs BG, et al. Proximal humeral fractures in children and adolescents. J Pediatr Orthop 2009;29:238-242. [DOI] [PubMed] [Google Scholar]
- 8.Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop 2011;5:187-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop 2003;23:208-215. [PubMed] [Google Scholar]
- 10.Hohloch L, Eberbach H, Wagner FC, et al. Age- and severity-adjusted treatment of proximal humerus fractures in children and adolescents-A systematical review and meta-analysis. PLoS One 2017;12:e0183157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.No authors listed HCUP-US Overview. https://www.hcup-us.ahrq.gov/overview.jsp (date last accessed 01March2018).
- 12.Osler T, Rutledge R, Deis J, Bedrick E. ICISS: an international classification of disease-9 based injury severity score. J Trauma 1996;41:380-386. [DOI] [PubMed] [Google Scholar]
- 13.Beringer DC, Weiner DS, Noble JS, Bell RH. Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop 1998;18: 31-37. [PubMed] [Google Scholar]
- 14.Binder H, Schurz M, Aldrian S, Fialka C, Vécsei V. Physeal injuries of the proximal humerus: long-term results in seventy two patients. Int Orthop 2011;35:1497-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg [Am] 1963;45-A:587-622. [Google Scholar]
- 16.Beaty JH. Fractures of the proximal humerus and shaft in children. Instr Course Lect 1992;41:369-372. [PubMed] [Google Scholar]
- 17.Cruz AI Jr, Kleiner JE, DeFroda SF, et al. Increasing rates of surgical treatment for paediatric diaphyseal forearm fractures: a National Database Study from 2000 to 2012. J Child Orthop 2017;11:201-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury 2012;43:362-366. [DOI] [PubMed] [Google Scholar]
- 19.Sinikumpu JJ, Pokka T, Serlo W. The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg 2013;23:289-296. [DOI] [PubMed] [Google Scholar]
- 20.Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years experience in the operative management of pediatric forearm fractures. J Pediatr Orthop 2010;30:313-319. [DOI] [PubMed] [Google Scholar]
- 21.Fabricant PD, Seeley MA, Anari JB, et al. Medial epicondyle fractures in children and adolescents: shifting care from general hospitals to children’s hospitals? J Pediatr 2015;167:1116-1120. [DOI] [PubMed] [Google Scholar]
- 22.Galano GJ, Vitale MA, Kessler MW, Hyman JE, Vitale MG. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop 2005;25:39-44. [DOI] [PubMed] [Google Scholar]
- 23.Merenstein D, Egleston B, Diener-West M. Lengths of stay and costs associated with children’s hospitals. Pediatrics 2005;115:839-844. [DOI] [PubMed] [Google Scholar]
- 24.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics 2006;118:483-492. [DOI] [PubMed] [Google Scholar]
- 25.Vyas RM, Dickinson BP, Wasson KL, Roostaeian J, Bradley JP. Pediatric facial fractures: current national incidence, distribution, and health care resource use. J Craniofac Surg 2008;19:339-349. [DOI] [PubMed] [Google Scholar]


