Abstract
Purpose
The purpose of this study was to evaluate the management of paediatric torus fractures of the distal forearm in current practice in light of growing evidence supporting a ‘minimalist’ approach with splint immobilization and limited follow-up. We hypothesized that ‘traditional’ cast-based management has persisted despite alternative evidence.
Methods
A retrospective review was performed of a consecutive series of paediatric patients diagnosed with torus fractures of the distal forearm between 2011 and 2014. Records were reviewed to abstract the type of immobilization (splint versus cast) prescribed at each visit, number of radiographic exams, duration of immobilization, number of clinical visits and complications. The primary outcome was the proportion of patients exclusively managed in splints. Injuries were grouped based on treatment into a cast group (CG) and a splint group (SG) for statistical analyses. Additionally, injuries were grouped by epoch of time to determine if immobilization usage patterns evolved.
Results
A total of 240 forty injuries met criteria for inclusion. Of these, 16 (6.7%) were exclusively splinted (SG). Relative to the CG, the SG had fewer clinical visits (p < 0.001), fewer radiographic exams (p < 0.001) and a shorter total encounter time (p = 0.015). No change in immobilization use occurred over the study period. In all, 21 (9.4%) of the CG experienced complications. No clinically significant displacements occurred in either group.
Conclusion
Cast utilization and frequent radiographic follow-up remain prevalent at our institution in the management of paediatric torus fractures. Splint-only management was associated with fewer clinical visits, fewer radiographic exams and a shorter total encounter time.
Level of Evidence Level III
Therapeutic retrospective cohort study
Keywords: Buckle fracture, evidence-based medicine, wrist fracture, closed management
Introduction
Torus (buckle) fractures of the distal forearm are common injuries in children and young adolescents, typically occurring after a fall on an outstretched arm.1 They are stable due to the thick periosteum present in this patient population and, unlike other paediatric wrist and forearm fractures, the risk of future displacement is minimal.2–4
The traditional management of paediatric torus fractures of the distal forearm has mirrored that of other fractures in this region, including cast immobilization and serial radiographic and clinical follow-up to assess for displacement until fracture union. However, emerging literature over the last two decades has supported a ‘minimalist’ approach to managing these injuries. Van Bosse et al5 described treatment with removable splint application at time of injury, appropriate patient and caregiver counselling, a short (three to four week) period of immobilization and either self-discontinuation of the splint at home or a single follow-up appointment with clinical examination only. Radiographs become necessary only in the setting of re-injury or continued pain after the treatment period. Numerous other studies have highlighted safe and efficacious management of these injuries in a similarly ‘minimalist’ fashion.2-4,6-9
In addition to pre-fabricated and removable splints, multiple other non-casting alternatives have been found to be equally safe in the management of paediatric torus fractures of the distal forearm. Soft bandage10 and soft cast,11,12 neither of which require a physician visit for removal, have both been demonstrated to be acceptable treatment options. In the appropriately selected patient, home-based removal of immobilization can further simplify management and has been demonstrated to have equivalent outcomes to clinic-based reexamination and removal.7 By eliminating the additional orthopaedic clinic visits for cast removal and radiographic exams, these management approaches theoretically minimize the burden to the caregiver and patient while simultaneously reducing treatment cost.4
Although recent studies have begun to evaluate provider opinions regarding minimalist strategies in the treatment of buckle fractures of the distal forearm and other paediatric orthopaedic injuries,13,14 to our knowledge, no prior study has examined ‘real world’ provider uptake and implementation of these practices since the emergence of this literature. The purpose of this study was to evaluate the current management of paediatric torus fractures at a single institution by examining the type and duration of immobilization prescribed, the utilization of radiographs in follow-up, and the number and duration of clinical encounters. We hypothesized that despite the evidence supporting a ‘minimalist’ approach, the majority of paediatric patients with torus fractures of the distal forearm in our hospital system would still be managed in a traditional fashion.
Patients and methods
Study design and setting
We performed a retrospective review of a consecutive series of paediatric patients diagnosed with a buckle fracture of the distal forearm between May 2011 and November 2014. The selected study period was chosen to coincide with the introduction of the electronic medical record (EMR) into our institution, which was critical for gathering outcome measures related to time spent receiving care. This study was conducted at a tertiary care academic institution in North Central Florida with an Emergency Department caring for roughly 12 000 children each year. Approval was obtained from the University of Florida Institutional Review Board for all study procedures.
Patient management
Definitive management of all fractures was determined by the treating clinician as per standard operations for this institution. Treating clinicians consisted of a mixed group of operative and nonoperative providers from a multi-specialty Orthopaedics and Rehabilitation Department. No clinicians involved in the care of the studied population were aware this study would be performed and thus their treatment was based on their own clinical experience and training. The vast majority of immobilization (casts and splints) used was below the elbow, except in a small number of children less than four years old. Casts were all fashioned from fibreglass, as is the standard of care at our centre. The splints referred to in this study included a heterogeneous assortment of both sugar-tong and fibreglass slabs applied using cast padding and an ace wrap as well as pre-fabricated Velcro wrist and forearm splints.
Patients
Eligible subjects were identified through a search of the EMR for individuals matching the following inclusion criteria: paediatric patient (17 years old and younger) and diagnosis of torus (buckle) fracture of the distal forearm given by the treating provider during our study period. Two independent radiograph evaluations were performed and compared, one by a radiologist and a second by author BAW, to confirm the diagnosis. Patients with buckle fractures of the distal radius and/or ulna (buckle or styloid fracture) were included. Those with diagnoses by either reviewer discrepant from the clinical record or with concomitant ipsilateral upper extremity fractures affecting definitive management (e.g. ipsilateral supracondylar humerus fracture) were excluded.
Study variables
The EMR was reviewed for extraction of the following variables: age (continuous), gender (dichotomous), location of each presentation (categorical) and the number of days (continuous) between visits. The number of radiographic exams (continuous) performed over the treatment period was tallied for each injury. Two- and three-view wrist series and two-view forearm series were each counted as a single exam. The treatment at each clinical encounter was recorded as either: splint, cast or no immobilization. Patients managed exclusively in a splint throughout the treatment period were assigned to the splint group (SG), while those casted for any period of time were assigned to the cast group (CG). The total clinical encounter time was the summed difference between the recorded check-in and check-out times (rounded to the nearest quarter of an hour) at each clinical encounter. Each patient chart was reviewed from the date of injury to three months post-injury to determine if complications or re-injuries occurred and were managed at our institution during this time frame.
Our primary outcome was the proportion of patients managed exclusively with splints during the study period. Secondary outcome measures included the rate of complications, the duration of follow-up and prescribed immobilization, and use of follow-up radiographs with each of the treatment strategies.
Data collection
Data collection occurred between January 2015 and June 2016 and was performed by three authors (BAW, CAA and DCM). The primary author determined standardized locations for extraction of each recorded variable from the medical record for all reviewers and performed simultaneous reviews of the first ten records for each reviewer to assure accuracy and consistency of data collection. Data were collected in and managed by Research Electronic Data Capture (REDCap)15 hosted at our institution. REDCap is a secure, web-based application designed to support data capture for research studies and facilitate seamless data export to common statistical packages.
Statistical analysis
Statistical analyses were performed using JMP PRO Version 12.0.1 (SAS Institute, Cary, North Carolina). Descriptive statistics were used to analyze the demographic and treatment-related variables across the entire study cohort. Univariate analyses were performed to evaluate for differences between the two treatment approaches (SG versus CG). Given the study was performed over more than a three-year period, we secondarily divided our study period into two epochs to examine whether changes in practice patterns led to differences in management over time. Our study population was divided into two equal sized groups of injuries occurring in the first and second halves of the study period. The ‘early’ group received care from 2011 to mid-2013 and the ‘late’ group received care from mid-2013 to 2014. For all analyses, Student’s t-tests were used for continuous data (age, duration of prescribed immobilization, duration of follow-up, number of radiographic exams and total clinical encounter time). Data are expressed as means and sd. The chi-squared test was used to analyze group differences in proportions of categorical data (gender, form of immobilization). A p-value < 0.05 was considered to be significant.
Results
A total of 300 consecutive records were reviewed and 240 torus fractures of the distal forearm occurring in 236 patients remained after appropriate exclusions (Fig. 1). Five exclusions appeared to be coding errors due to a clearly incorrect diagnosis (e.g. displaced both bone forearm fracture), while a larger number were excluded due to radiograph review demonstrating injuries more consistent with greenstick or minimally displaced transverse fractures (both cortices involved). In all, 70 (29.1%) injuries were referred in after initial management at an outside facility. The duration of clinical visits occurring at outside facilities was not accessible through our EMR, therefore, these injuries were excluded from analyses involving total clinical encounter time.
Fig. 1.
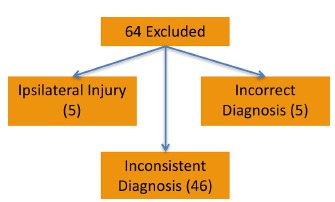
Reasons for subject exclusion.
Age at injury was 7.5 years (sd 3.5) old. A total of 123 (51.3%) fractures occurred in males. Providers exclusively managed buckle fractures of the distal forearm in a splint in 16 (6.7%) cases. All other injuries (93.3%) were managed for all or a portion of the treatment period in a cast. Patients were followed in clinic for an average of 28.9 days (sd 8.3) and prescribed immobilization (cast or splint) for 35.3 days (sd 10.3). Patients underwent 2.3 radiographic exams (sd 0.7) and spent 4.9 hours (sd 2.2) waiting for, and receiving treatment over their clinical course.
Significant differences existed between SG and CG for a number of our demographic and treatment-related variables (Table 1). No significant differences in management strategy were found with respect to gender or prescribed duration of immobilization.
Table 1.
Splint group (SG) versus cast group (CG). Significant differences identified between splint and cast-managed injuries.
| Significant variable | SG (sd) | CG (sd) | p-value |
|---|---|---|---|
| Mean age (yrs) | 9.4 (3.0) | 7.3 (3.5) | 0.016 |
| Mean clinical visits (n) | 2.1 (0.57) | 2.9 (0.69) | < 0.001 |
| Mean radiographic exams (n) | 1.6 (0.62) | 2.3 (0.65) | < 0.001 |
| Mean encounter time (hrs)* | 3.5 (0.89) | 5 (2.2) | 0.015 |
total encounter time included a subset of injuries with all clinical visits occurring at our institution
Comparing the early and late care groups, we found no change in the proportion of patients managed in a splint (early – 6.7% versus late – 6.7%). Additionally, there were no significant differences in duration of patient follow-up, duration of prescribed immobilization practices, total radiographs obtained or total duration of clinical care between the two study epochs.
Follow-up and complications
No radiographic or clinically evident displacement occurred in patients completing follow-up at our institution in the CG or SG. A total of 21 (8.8%) patients were lost to follow-up after treatment at our centre, 19 (8.5%) in the CG and two (12.5%) in the SG. In all, 21 (9.4%) patients in the CG had cast-related problems (e.g. wet or painful cast) requiring an unscheduled clinic visit for cast change or removal while no complications were observed in the SG (Fig. 2).
Fig. 2.
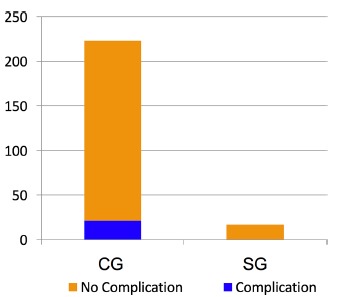
Complication comparison of cast group (CG) and splint group (SG).
Follow-up and complications
In total, 25 (10.4%) patients were lost to follow-up after treatment at our centre, 19 in the CG and six in the SG. In all, 21 cast-related problems (e.g. wet or painful cast) occurred requiring an unscheduled clinic visit for cast change or removal while no splint-related complications were observed (Fig. 2). No radiographic or clinically evident displacement occurred in patients completing follow-up at our institution in either group.
Discussion
The findings of our study identified persistent utilization of traditional management strategies throughout the study period without evidence of practice evolution over the three-year time frame. To our knowledge, this is the first study to examine true provider implementation of the splint approach for distal forearm buckle fractures since emergence of a broad literature base in favour of minimalist strategies over the last two decades.2,6,9,10,16-18
In a recent systematic review of randomized-controlled trials comparing treatment of paediatric torus fractures of the distal forearm, Hill et al16 (2016) found broad support for the use of removable splint over a cast. The benefits of splinting have been seen in regards to function, hygiene, cost, convenience and patient and caregiver satisfaction without increased risk of treatment failure.2,6,9,10,17,18 Furthermore, although we opted to exclude non-torus fractures of the wrist (i.e. greenstick and transverse) from the current study, a 2010 randomized controlled trial by Boutis et al19 suggests that these injuries may also be safely managed with a removable device for four weeks. These authors also identified that splints were superior with regards to patient and parental satisfaction. Other non-casting alternatives such as soft bandage10 and soft cast11,12 have also demonstrated efficacy and ease of use. Although some studies have suggested a potential downside of non-cast options related to higher pain scores at presentation9 and longer periods of pain,18 these findings have not been consistent across all studies. Most importantly, non-cast treatments have not demonstrated any increased risk of fracture displacement or treatment failure across numerous rigorous trials.16
Our findings demonstrate that despite this growing evidence base, traditional practices remain prevalent at our institution. The vast majority of paediatric buckle fractures of the distal forearm at our centre were treated with a cast instead of a splint. Of further concern, the utilization of radiographic and clinical follow-up, the duration of follow-up and the prescribed duration of immobilization were greater than the recent evidence suggests is necessary for safe management.2,6,9,10,17,18 Additionally, when comparing the early and late groups to evaluate for changes in practice patterns over the study period, we identified no statistically significant differences in the metrics studied. Together, these results suggest the enduring tendency to over-treat this injury. We also identified a significant association with fewer clinical visits, fewer radiographic exams and a shorter total encounter time in injuries managed exclusively in splints. Elimination of unnecessary clinic visits and radiographic exams has great potential to reduce caregiver time lost from work and patient time lost from school.
Although the decision to utilize traditional treatment measures is presumably made with the patient’s best interest in mind, it is easy to overlook the risks and inconveniences imposed with overtreatment. Traditional measures can increase healthcare spending, introduce unnecessary radiation exposure to the patient, and create additional financial burden for caregivers due to added travel and time away from work. Most importantly, casting is not benign. Skin complications and burns can occur from ill-fitting or mistreated casts and improper cast removal. Additional inconveniences may also arise, such as unscheduled clinic visits for casts that become wet, uncomfortable or too tight. In this study, nearly 10% of injuries managed in a cast had a complication requiring an unscheduled visit (Fig. 2). Finally, cast application is also more time consuming and labour intensive than splint use and requires follow-up for removal. Therefore, this all begs the question: why are many providers continuing to cast children for these injuries if there exists an equivalent, well-tolerated and evidence-based alternative with fewer complications?
The reasons for discrepancy between evidence-based and actual practice are unclear. Dogmatic and long-standing practices in medicine are often difficult to change despite strong evidence to the contrary. Some potential barriers to adoption of these new standards of practice include a lack of familiarity with recent literature supporting the ‘minimalist’ approach, prior provider experiences, patient and caregiver preferences, concerns regarding splint compliance, and inability or lack of confidence in accurately identifying fractures appropriate for minimalist treatment. Boutis and colleagues explored the barriers to emergency14 and paediatric orthopaedic13 provider utilization of splints in the management of paediatric fractures with low rates of complications. Emergency providers felt constrained by the availability of commercial splinting devices and the support of their orthopaedic colleagues, while both groups expressed concerns about patient compliance and potential complications with removable forms of immobilization. The results of this study, performed in a health system with a mixed group of both operative and nonoperative paediatric and adult providers caring for these injuries, suggest that further exploration of these barriers is certainly warranted.
Quality issues and future directions
Based on our findings, this group of investigators is seeking to identify and quantify barriers to broader acceptance of minimalist strategies via provider, patient and caregiver survey. Once identified, we plan to deconstruct these barriers in order to facilitate front-line provider (primary care and emergency medicine physicians and orthopaedic residents) education and implement institution-wide changes to the treatment algorithm. These didactic measures will also help facilitate improvement in the radiographic recognition and coding accuracy of these injuries, an issue highlighted by a significant proportion of patients excluded from our study.
Limitations
This study was principally limited by the small sample size of patients treated exclusively in a splint and its retrospective design. We relied on the accuracy and consistency of the medical record for identification of patients via diagnosis coding and for many of our collected variables. Additionally, a substantial number of injuries in this cohort were excluded due to discrepant diagnoses. While it is unclear whether this was due to miscoding or misdiagnosis, it does suggest that appropriate identification of injuries acceptably managed in splint alone may be a factor limiting implementation of this treatment strategy. Recent work suggests that even among individuals trained in evaluating paediatric musculoskeletal radiographs, over- and misdiagnosis of buckle fractures of the distal forearm may be a more widespread issue than most would readily acknowledge.20 While our study was not designed to formally address this question, these observations deserve further exploration of strategies for improvement. Finally, the generalizability of our results is uncertain due to the limited number of dedicated paediatric practitioners at our centre during the study period. We recognize that utilization patterns at institutions where providers exclusively care for paediatric patients may be different. Further multicentre and multi-setting studies are necessary to assess how broadly these treatment patterns extend in our present-day healthcare system.
Conclusions
Cast utilization and frequent radiographic follow-up remain common at our institution in the management of paediatric torus fractures despite growing evidence supporting an alternative ‘minimalist’ strategy. Nearly 10% of casted injuries suffered a complication requiring an unscheduled visit while splint-only management of torus fractures of the distal forearm at our institution was associated with fewer clinical visits, fewer radiographic exams and a shorter total encounter time. Measures to increase implementation of this strategy are likely to decrease treatment-related costs and patient/caregiver inconvenience. Future work will explore barriers to implementation of this management practice with the hope of achieving practice change through provider education and institution-wide treatment algorithms.
COMPLIANCE WITH ETHICAL STANDARDS
FUNDING STATEMENT
Research reported in this publication was supported by the University of Florida Clinical and Translational Science Institute, which is supported in part by the NIH National Center for Advancing Translational Sciences under award number UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
OA LICENCE TEXT
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
ETHICAL STATEMENT
Ethical approval: This study involved a retrospective review of the medical record. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Not applicable – retrospective review.
ICMJE CONFLICT OF INTEREST STATEMENT
LCB has received consulting fees from K2M Medical. All other authors declare they have no conflict of interest.
REFERENCES
- 1.Noonan KJ, Price CT. Forearm and distal radius fractures in children. J Am Acad Orthop Surg 1998;6:146-156. [DOI] [PubMed] [Google Scholar]
- 2.Davidson JS, Brown DJ, Barnes SN, Bruce CE. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg [Br] 2001;83-B:1173-1175. [DOI] [PubMed] [Google Scholar]
- 3.Farbman KS, Vinci RJ, Cranley WR, Creevy WR, Bauchner H. The role of serial radiographs in the management of pediatric torus fractures. Arch Pediatr Adolesc Med 1999;153:923-925. [DOI] [PubMed] [Google Scholar]
- 4.Firmin F, Crouch R. Splinting versus casting of “torus” fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs 2009;17:173-178. [DOI] [PubMed] [Google Scholar]
- 5.van Bosse HJP, Patel RJ, Thacker M, Sala DA. Minimalistic approach to treating wrist torus fractures. J Pediatr Orthop 2005;25:495-500. [DOI] [PubMed] [Google Scholar]
- 6.Plint AC, Perry JJ, Correll R, Gaboury I, Lawton L. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics 2006;117:691-697. [DOI] [PubMed] [Google Scholar]
- 7.Symons S, Rowsell M, Bhowal B, Dias JJ. Hospital versus home management of children with buckle fractures of the distal radius. A prospective, randomised trial. J Bone Joint Surg [Br] 2001;83-B:556-560. [DOI] [PubMed] [Google Scholar]
- 8.Neal E. Comparison of splinting and casting in the management of torus fracture. Emerg Nurse 2014;21:22-26. [DOI] [PubMed] [Google Scholar]
- 9.Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care 2013;29:555-559. [DOI] [PubMed] [Google Scholar]
- 10.West S, Andrews J, Bebbington A, Ennis O, Alderman P. Buckle fractures of the distal radius are safely treated in a soft bandage: a randomized prospective trial of bandage versus plaster cast. J Pediatr Orthop 2005;25:322-325. [DOI] [PubMed] [Google Scholar]
- 11.Witney-Lagen C, Smith C, Walsh G. Soft cast versus rigid cast for treatment of distal radius buckle fractures in children. Injury 2013;44:508-513. [DOI] [PubMed] [Google Scholar]
- 12.Khan KS, Grufferty A, Gallagher O, et al. A randomized trial of ‘soft cast’ for distal radius buckle fractures in children. Acta Orthop Belg 2007;73:594-597. [PubMed] [Google Scholar]
- 13.Boutis K, Howard A, Constantine E, et al. Evidence into practice: pediatric orthopaedic surgeon use of removable splints for common pediatric fractures. J Pediatr Orthop 2015;35:18–23. [DOI] [PubMed] [Google Scholar]
- 14.Boutis K, Howard A, Constantine E, Cuomo A, Narayanan U. Evidence into practice: emergency physician management of common pediatric fractures. Pediatr Emerg Care 2014;30:462-468. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hill CE, Masters JPM, Perry DC. A systematic review of alternative splinting versus complete plaster casts for the management of childhood buckle fractures of the wrist. J Pediatr Orthop B 2016;25:183-190. [DOI] [PubMed] [Google Scholar]
- 17.Karimi Mobarakeh M, Nemati A, Noktesanj R, Fallahi A, Safari S. Application of removable wrist splint in the management of distal forearm torus fractures. Trauma Mon 2013;17:370-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oakley EA, Ooi KS, Barnett PL. A randomized controlled trial of 2 methods of immobilizing torus fractures of the distal forearm. Pediatr Emerg Care 2008;24: 65-70. [DOI] [PubMed] [Google Scholar]
- 19.Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ 2010;182:1507-1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terreblanche B, Eismann EA, Laor T, Cornwall R, Little K. Overdiagnosis of distal radius buckle fracture in children [Abstract]. Annual Meeting for the American Association for Hand Surgery (2016). [Google Scholar]


