Abstract
Purpose
To review the initial deformity and subsequent remodelling in posteromedial bowing of the tibia and the outcome of limb reconstruction in this condition.
Patients and Methods
In all, 38 patients with posteromedial bowing of the tibia presenting between 2000 and 2016 were identified. Mean follow-up from presentation was 78 months. A total of 17 patients underwent lengthening and deformity correction surgery, whilst three further patients are awaiting lengthening and deformity correction procedures.
Results
The greatest correction of deformity occurred in the first year of life, but after the age of four years, remodelling was limited. The absolute leg-length discrepancy (LLD) increased throughout growth with a mean 14.3% discrepancy in tibial length. In the lengthening group, mean length gained per episode was 45 mm (35 to 60). Mean duration in frame was 192 days, with a mean healing index of 42.4 days/cm. Significantly higher rates of recurrence in LLD were seen in those undergoing lengthening under the age of ten years (p = 0.046). Four contralateral epiphysiodeses were also performed.
Conclusion
Posteromedial bowing of the tibia improves spontaneously during the first years of life, but in 20/38 (53%) patients, limb reconstruction was indicated for significant residual deformity and/or worsening LLD. For larger discrepancies and persistent deformity, limb reconstruction with a hexapod external fixator should be considered as part of the treatment options.
Level of evidence
Level IV (Case series)
Keywords: Posteromedial bowing, tibia, limb reconstruction, tibial recurvatum
Introduction
Congenital posteromedial bowing of the tibia is a rare condition first described by Heyman and Herndon in 19491 which has also been termed kyphoscoliosis of the tibia2 or tibial recurvatum.3 The literature on this condition is limited; the largest series describing the natural history to date is by Pappas (1984),4 which describes a group of 33 patients.
Traditionally, posteromedial bowing is considered a ‘benign condition’5 in view of its potential to remodel,2,4,6 particularly in comparison with the less favourable associations of anterolateral bowing with tibial pseudarthrosis or anteromedial bowing with fibular hemimelia.
It is accepted that remodelling is not usually complete, and that leg-length discrepancy (LLD) increases with age and may be up to 7 cm at maturity.4,5,7 Some authors have suggested that surgery should play a greater role in the management of posteromedial bowing than simple epiphysiodesis, either through the use of osteotomy for deformity correction7-9 and/or limb lengthening techniques.7,10
The aim of this study was firstly to review the initial remodelling of deformity in the condition in cases presenting to two tertiary centres prior to any intervention, and secondly to assess the outcome of limb reconstruction and other surgeries for limb-length equalization and deformity correction, in order to better define management protocols.
Patients and methods
Cases were identified from the patient databases of two tertiary referral hospitals. Inclusion criteria were any cases of posteromedial bow of the tibia seen during the study period between 2000 and 2016. Local clinical governance and audit registration was obtained prior to data collection (Royal National Orthopaedic Hospital, Stanmore, UK, registration number SE17.031; Great Ormond Street Hospital, London, UK, registration number 2232). Exclusion criteria were a lack of radiographic data (three patients), or if the patient was only seen for initial assessment with ongoing follow-up being within a local hospital (one patient). A total of 42 patients were identified with four exclusions, providing a total of 38 patients for analysis. Demographic data is shown in Table 1. In all, 22 patients were seen from under six months of age; the remaining 16 patients were referred later in childhood.
Table 1.
Demographic details for all patients included in study (n = 38)
| Demographic | Result |
|---|---|
| Mean (range) age at presentation in months | 33 (0 to 221) |
| Male:Female | 16:22 |
| Left:Right | 22:16 (all cases were unilateral) |
| Mean (range) follow-up in months | 78 (9 to 197) |
The analysis consisted of two parts: the initial deformity/remodelling and the limb reconstruction group.
Initial deformity and remodelling
To assess the initial deformity and remodelling in posteromedial bowing, data was collected from clinical notes and radiographs. Measurements included: severity of deformity at presentation, type of foot deformity and change of angulation on standardized sequential radiographs in the anteroposterior and lateral planes. Shortening was assessed clinically and radiographically with long-leg standing radiographs to record the relative shortening of the affected tibia in relation to the normal side. If a patient underwent intervention for deformity or LLD, the data following this intervention was not used in the assessment of natural history.
Limb reconstruction group
Patients who went on to require lengthening and/or deformity correction formed the second part of the study. A total of 17 patients underwent lengthening with 19 separate lengthening episodes. Three further patients are planned for lengthening/deformity correction as their primary procedure at a future date according to predicted LLD (between 45 mm and 80 mm). Medical notes and radiographs determined length gained, time in frame, bone healing index and any complications. Any recurrence of LLD was noted in the follow-up, along with requirement for further procedures. Indications for epiphysiodesis alone were a predicted LLD > 2 cm with no significant angular deformity. Indications for limb reconstruction included a predicted LLD of > 5 cm or symptomatic residual angular deformity after the age of four years with an associated LLD. No patients were seen with angular deformity alone, without a LLD.
Statistical analysis
This was performed using SPSS 23 (IBM, New York, New York) for Mac. Unless otherwise stated, categorical variables are expressed as frequency (percentage) and continuous variables are expressed as mean (range) with p < 0.05 considered as statistically significant. Non-parametric group comparisons of continuous data were made with the Mann-Whitney U test. Correlation coefficients were calculated using Spearman’s test. Fisher’s exact test was used for categorical data.
Results
Initial deformity and remodelling
A prenatal diagnosis of a lower limb abnormality was made in 16/24 (66%) of patients from the 20-week anomaly scans. Only one patient received a correct diagnosis of posteromedial bowing on the anomaly scan, the remaining patients being reported as: tibia/fibula shortening (nine patients), congenital talipes equinovarus (three patients), fibular hemimelia (two patients) or ‘lower limb abnormality’ (one patient). For the 22 patients presenting within six months of birth, a calcaneovalgus foot was described in 17 patients, and a normal foot/ankle appearance in five patients.
Angular deformity
On initial presentation, in the subgroup of 22 patients who were seen at less than six months of age, the mean medial bow was measured as 43° (5° to 70°) and the mean posterior bow 35° (7° to 71°). For all patients, the degree of bow was seen to improve over time, with the greatest rates of correction seen within the first year of life. Figures 1 and 2 demonstrate the radiographic appearances of the deformity and subsequent improvement over time. Figures 3 and 4 graphically demonstrate the improvement in tibial bowing over time divided into the posterior and medial components of the deformity. There is a greater time period over which the medial bow measurements are available, reflecting the greater number of long-leg radiographs taken in comparison with lateral views in the older patients.
Fig. 1.
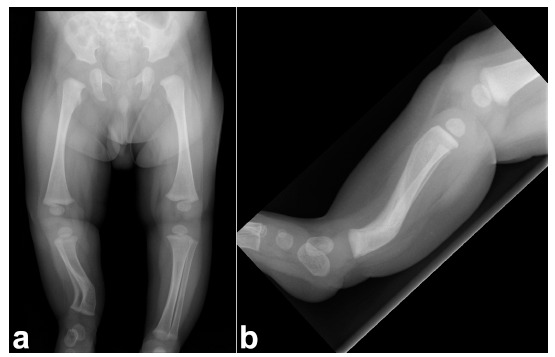
(a) Long-leg anteroposterior (AP) radiograph demonstrating posteromedial bowing of the right tibia at presentation aged three months; (b) lateral radiograph demonstrating posteromedial bowing of the right tibia at presentation aged three months.
Fig. 2.
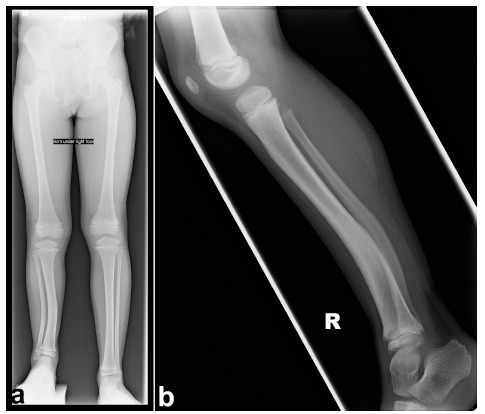
(a) Long-leg anteroposterior radiograph demonstrating some remodelling of right tibia, with increase to 4 cm leg-length discrepancy aged six years; (b) lateral radiograph demonstrating some remodelling of right tibia, with increase to 4 cm leg-length discrepancy aged six years.
Fig. 3.
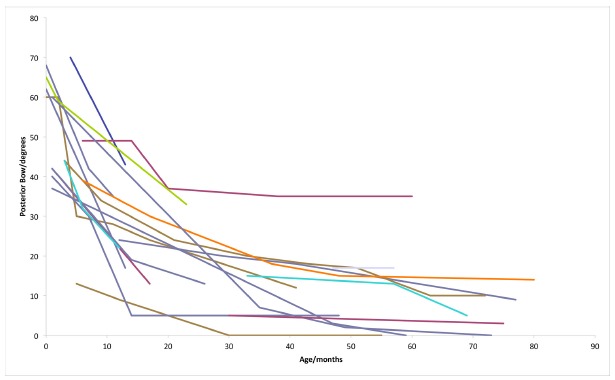
Graph demonstrating improvement in posterior bowing with increasing age. Each line represents the change in one patient.
Fig. 4.
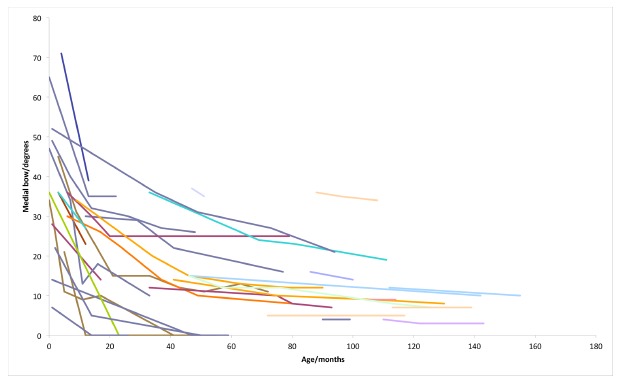
Graph demonstrating improvement in medial bowing with increasing age. Each line represents the change in one patient.
Table 2 shows the rate of correction of the posterior and medial components of the bow over differing time periods. There is a non-significant trend for a greater rate of correction of the posterior bow in comparison with the medial bow (p = 0.158). Although there is not a clear cut-off for the point at which remodelling ceases, most of the improvement is seen in the first four years of life.
Table 2.
Rate of improvement in bowing over first five years of life. All figures in degrees per month
| Year | 1 | 2 | 3 | 4 | 5 | >5 |
|---|---|---|---|---|---|---|
| Medial bowing | 1.78 | 0.553 | 0.306 | 0.21 | 0.11 | 0.085 |
| Posterior bow | 2.43 | 0.755 | 0.315 | 0.175 | 0.052 | 0.0375 |
LLD
The femur did not contribute to LLD. Figure 5 demonstrates the progressive increase in clinical LLD with time (Spearman’s R = 0.848, p < 0.001). The mean percentage shortening of the tibia was not seen to change over time in each patient, with a mean across all patients of 14.3% (4% to 25%). There was a significant association between severity of bow and percentage LLD for posterior bowing (Spearman’s R = 0.851, p = 0.015), but not as strong for medial bowing (Spearman’s R = 0.619, p = 0.075).
Fig. 5.
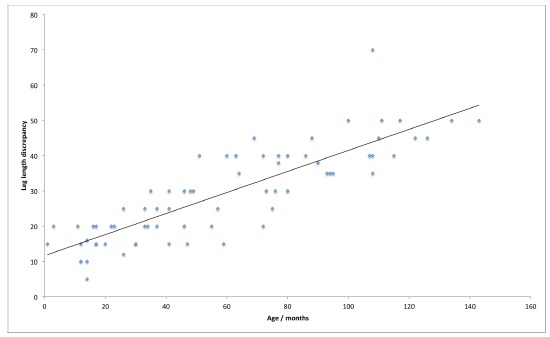
Scatter graph demonstrating increasing leg-length discrepancy as age of patient increases.
Table 3 summarizes the interventions required within the patient group studied. Four patients underwent proximal tibial epiphysiodesis and four patients are awaiting epiphysiodesis, according to predicted LLD, as their primary treatment. One patient with a significant LLD declined intervention as her underlying psychological/behavioural issues precluded limb reconstruction and insufficient growth was remaining for an epiphysiodesis. Of the nine patients managed conservatively, eight are under continuing observation, as they are under the age of four years. The final patient has remodelled the angular deformity but has a predicted LLD of > 5 cm, although the family have not yet made a decision about limb length equalization.
Table 3.
Summary of the primary treatments undergone
| Treatment | n = 38 |
|---|---|
| Lengthening/deformity correction Awaiting due to predicted LLD Declined lengthening |
17 patients (19 episodes) 3 patients (predicted LLD 45 mm to 80 mm) 1 patient (LLD 70 mm) |
| Proximal tibial epiphysiodesis Awaiting due to predicted LLD |
4 patients performed 4 patients awaited |
| Continued observation/nonoperative | 8 patients aged < 4 yrs 1 patient undecided (predicted LLD 5.4 cm) |
Limb reconstruction group
In all, 17 patients underwent 19 episodes of limb reconstruction during the study period. All patients except one (18/19 episodes) underwent limb reconstruction using the Taylor Spatial Frame (TSF; Smith & Nephew, Memphis, Tennessee), the remaining one being performed with a monolateral fixator (Stryker, Newbury, United Kingdom). Figures 6 and 7 demonstrate an example of the radiographic appearances of the tibia both during and following the lengthening procedure with the TSF.
Fig. 6.
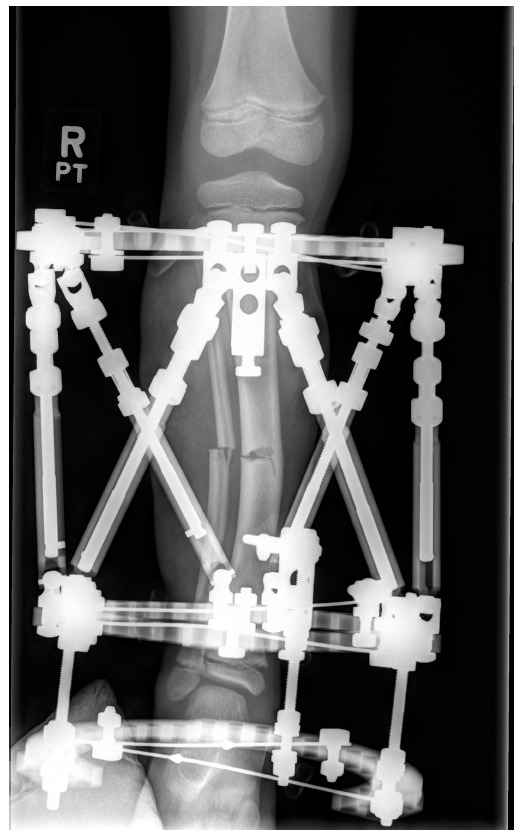
Anteroposterior radiograph of the right tibia during frame correction of deformity and lengthening.
Fig. 7.

(a) Anteroposterior radiograph demonstrating appearance of right tibia following correction; (b) lateral radiograph demonstrating appearance of right tibia following correction.
Bifocal lengthening (‘Stacked TSF’) was used in three cases, in which deformity correction was achieved at the distal osteotomy with further lengthening at the proximal osteotomy to limit time in the frame, due to the better healing potential of a metaphyseal osteotomy.11 This technique was considered where the angular deformity necessitated a mid-diaphyseal osteotomy with > 3 cm lengthening required. As this is a retrospective multi-surgeon series, the final decision for the frame construct was down to surgeon choice.
The aim of limb reconstruction was to correct deformity and equalize leg lengths: it was understood that, in the presence of pathology that affected growth, a discrepancy would return over time.
The demographics and details of deformity correction are summarized in Table 4. Torsional deformities could not be assessed from radiographs, but from the clinical notes where not thought to be a significant element of the deformity requiring correction. Target length was achieved in 18/19 lengthening episodes, with one stopped early due to development of an equinus contracture, which subsequently improved with physiotherapy alone.
Table 4.
Demographics and details of deformity correction in limb reconstruction group (n =17)
| Criteria | Result |
|---|---|
| Age at time of surgery (range) | 10 yrs (4 to 18) |
| Method of deformity correction | Taylor Spatial Frame - 18 episodes Monolateral fixator - 1 episode |
| Inclusion of heel in fixator construct | 10/19 episodes |
| Mean deformity at time of surgery (range) | Medial bow 13.3° (0° to 35°) Posterior bow 9.9° (0° to 32°) |
| Mean deformity at latest follow-up (range; significant improvement) | Medial bow 2.8° (-3° to 12°; p = 0.001) Posterior bow 2.3° (0° to 9°; p = 0.003) |
| Mean length gained (range) | 45 mm (35 to 60) |
| Mean duration in frame (range) | 192 days (129 to 287) |
| Mean healing index (range) | 42.4 days/cm (31.1 to 60.9) |
| Mean follow-up from removal of frame (range) | 32 months (2 to 80) |
| Skeletal maturity at latest follow-up | 10/17 patients |
Complications and recurrence
Complications from lengthening and recurrences are summarized in Table 5. It was noted that all of the patients requiring surgical intervention for joint contracture did not have the heel included in the frame construct for the lengthening process. No nerve injuries, episodes of nonunion or fractures following frame removal were seen.
Table 5.
Summary of complications and recurrences of leg-length discrepancy in limb reconstruction group (n = 17)
| Complication | n | Treatment |
|---|---|---|
| Superficial pin site infection | 5 | Oral antibiotics |
| Deformity of regenerate | 1 | Corrected with wedged long-leg plaster |
| Premature consolidation of proximal osteotomy in bifocal lengthening | 1 | Target length obtained from distal osteotomy |
| Joint contractures | 9 | 6 responded to physiotherapy 3 required surgery 1 posteromedial release 1 tendoachilles lengthening 1 manipulation under anaesthesia at frame removal |
At the time of latest follow-up the mean LLD in the lengthening group was 10mm (0 mm to 30 mm). Significant recurrent LLD (> 10 mm) was seen in six patients. Out of these six patients, two underwent a subsequent epiphysiodesis, two underwent a second period of lengthening and two patients declined any further treatment. The age of intervention was shown to be important with 4/6 patients lengthened under the age of ten years developing significant further LLD, while only 2/13 of those lengthened over the age of ten years showed significant recurrence at latest follow-up (Fishers exact test, p = 0.046). Age at latest follow-up was a mean of 13.8 years (8 to 21) with ten patients having reached skeletal maturity.
Discussion
This study represents the largest series of patients presenting with posteromedial bowing of the tibia that has been described to date. The series has replicated the perceived understanding that the bowing deformity improves with time, if not completely. The rate of correction was seen to be greatest during the first year, with decline after this. There is no clear point at which remodelling ceases, although our data does support the suggestion that after four years, no further clinically important remodelling occurs.4,7-9 There was a non-significant trend for a faster rate of correction of the posterior component of the bow than the medial. This is consistent with the theory that deformities correct more rapidly in the plane of movement of the adjacent joints than those perpendicular to that plane.9,12
The initial degree of bowing showed a strong correlation to the proportional LLD. This was also commented upon by Shah et al,9 who conversely observed a greater correlation with the medial bow than the posterior, in a small subgroup of their patients where the data was available. As the posteromedial bow represents an oblique plane deformity,13 it would seem sensible that it is the total magnitude of the bow that predicts the discrepancy, rather than one plane in particular.
The LLD was seen to increase relentlessly throughout growth (as demonstrated in Figure 5), although the percentage growth inhibition remained constant in comparison with the normal side. This is consistent with a congenital (Type 1) picture of LLD as described by Shapiro,14 which should allow for an accurate prediction of final discrepancy from population data.15 In the infant, the accuracy of measurement of percentage shortening may not be reliable to use for prediction, but by the age of four years both the quality of radiographs and the absolute size of the patient should allow for sufficient accuracy of measurement to provide a more useful prediction of final LLD to develop a surgical plan. The relative tibial shortening seen in this series was comparable with the previous published data of a mean of 12% to 15%,4,9 although there is a range of severity. Although the aetiology of posteromedial bowing is not fully understood,16,17 a true congenital cause rather than intrauterine fracture or crowding would better explain the ongoing growth disturbance. Our data would support this due to the presence of abnormality from the time of the 20-week anomaly scan. Impaired function of the distal tibial physis has been suggested as the source for the shortening, which persists throughout growth.4,10
In this series of 19 episodes of lengthening in 17 patients, the required length was achieved in 18/19 procedures. The healing index of 42 days/cm was comparable with the literature for lengthening of congenital tibial deformity,10,18,19 with no significant problems seen in regenerate formation or bone healing. The previously published use of limb-lengthening techniques in posteromedial bowing of the tibia is limited, with Shah9 reporting two patients, Johari7 six patients and Kaufmann et al10 describing a series of 11 patients undergoing limb lengthening with the Ilizarov method. Newer techniques may prove to further shorten the time in frame such as lengthening over flexible nails20,21 or lengthening and then plating,22,23 although these techniques have not been reported in this cohort of patients.
The main complications seen, beyond pin site infections, were related to soft-tissue and joint contractures. Including the heel in the frame construct may reduce the risk of equinus contracture, although other methods have also been described to overcome such contracture during tibial lengthening, including pre-emptive soft-tissue release24 and temporary extra articular arthrodesis.25 As a retrospective study between two centres, there was no set indication for including the foot in this series. However, the current practice among the authors is now to include the foot in the construct if lengthening of greater than 2 cm is required. One patient (the earliest undergoing lengthening) was treated with a monolateral fixator, who went on to develop a deformity of the regenerate. This complication was not seen in the remaining patients treated with the TSF, which reflects the greater control achieved with a hexapod fixator,10,26 rather than the surgeon’s learning curve.
We have demonstrated that the risks of recurrence of LLD are significantly higher if lengthening is performed before the age of ten years. With an ongoing growth inhibition, the risk of recurrence is important to consider both in the decision for timing of surgery and in counselling of parents. If the child still has significant bowing deformity beyond the age of four years, then expected further remodelling will be limited. At this time, correction of deformity with lengthening could be considered, with the understanding that if the length is not corrected according to the predicted discrepancy at maturity, (i.e. overlengthening the tibia at initial treatment) the patient will likely require further treatment. This may include either a subsequent period of lengthening or a contralateral epiphysiodesis to correct the ongoing growth disturbance. Calculation of the magnitude of the predicted discrepancy at maturity should help guide which of these options would be preferable. If, however, the bowing deformity has remodelled to an extent that it does not cause functional or significant cosmetic impairment, then our preference is to wait until closer to skeletal maturity to perform lengthening. This serves to not only limit the number of procedures required but also, the more mature child may manage the lengthening process better. The age at which lengthening is performed may also affect the residual growth from the physis, although this effect has not been fully quantified.27
As this study was carried out between two tertiary centres, along with the benefit of providing a large patient group, it does bring limitations. The older patients referred on to a tertiary centre are likely to represent the worse end of the spectrum of the condition and as such are more likely to require intervention. This may have led to an overestimation of the number of patients requiring limb lengthening (greater than 50% in this series). As a large proportion of the patients underwent intervention, this limits the assessment of the true natural history, with assessment focussed on the period before a surgical intervention. The retrospective design relies on the radiographic data that is available, with radiographs taken at variable time points according to when patients attended clinic. Despite this limitation, due to the usual care involving regular monitoring of the deformity, a reasonable number of data points have been obtained for this patient group.
The same device was used for the majority of the lengthening procedures, however, these were performed by five different surgeons in two independent centres, without standardization of treatment, so specific learning points relating to the technique should be taken with care. As not all patients were skeletally mature at the time of latest follow-up, the study may underestimate late complications and recurrence. Indeed, smaller increases in LLD (< 10 mm) were seen at follow-up in most of the lengthening patients with growth remaining, which would be consistent with an ongoing congenital growth disturbance. However, logic would suggest that this is unlikely to change the finding that the patient undergoing lengthening at a younger age is at higher risk of recurrence.
In conclusion, congenital posteromedial bowing of the tibia does improve significantly during the first years of life, although may leave residual deformities and worsening LLD. For larger discrepancies and those associated with angular deformity, limb lengthening with a hexapod external fixator should be considered as part of the treatment options, although careful consideration is required in both selection and timing of limb equalization procedures.
COMPLIANCE WITH ETHICAL STANDARDS
FUNDING STATEMENT
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA LICENCE TEXT
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
ETHICAL STATEMENT
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was not required for this work.
REFERENCES
- 1.Heyman CH, Herndon CH.. Congenital posterior angulation of the tibia. J Bone Joint Surg [Am] 1949;31-A:571-580. [PubMed] [Google Scholar]
- 2.Rathgeb JM, Ramsey PL, Cowell HR.. Congenital kyphoscoliosis of the tibia. Clin Orthop Relat Res 1974;103:178-90. [DOI] [PubMed] [Google Scholar]
- 3.Hill R. Congenital Posteromedial Bowing of the Tibia (Congenital Tibia Recurvatum). In: Rozbruch SR, Hamdy R, eds Limb Lengthening and Reconstruction Surgery Case Atlas. Berlin: Springer, 2014:1-5. [Google Scholar]
- 4.Pappas AM. Congenital posteromedial bowing of the tibia and fibula. J Pediatr Orthop 1984;4:525-531. [PubMed] [Google Scholar]
- 5.Hofmann A, Wenger DR.. Posteromedial bowing of the tibia. Progression of discrepancy in leg lengths. J Bone Joint Surg [Am] 1981;63-A:384-388. [PubMed] [Google Scholar]
- 6.Yadav SS, Thomas S.. Congenital posteromedial bowing of the tibia. Acta Orthop Scand 1980;51:311-313. [DOI] [PubMed] [Google Scholar]
- 7.Johari AN, Dhawale AA, Salaskar A, Aroojis AJ.. Congenital postero-medial bowing of the tibia and fibula: is early surgery worthwhile? J Pediatr Orthop B 2010;19:479-486. [DOI] [PubMed] [Google Scholar]
- 8.Napiontek M, Shadi M.. Congenital posteromedial bowing of the tibia and fibula: treatment option by multilevel osteotomy. J Pediatr Orthop B 2014;23:130-134. [DOI] [PubMed] [Google Scholar]
- 9.Shah HH, Doddabasappa SN, Joseph B.. Congenital posteromedial bowing of the tibia: a retrospective analysis of growth abnormalities in the leg. J Pediatr Orthop B 2009;18:120-128. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman SD, Fagg JA, Jones S, et al. Limb lengthening in congenital posteromedial bow of the tibia. Strategies Trauma Limb Reconstr 2012;7:147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischgrund J, Paley D, Suter C.. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res 1994;301:31-37. [PubMed] [Google Scholar]
- 12.Friberg KS. Remodelling after distal forearm fractures in children. II. The final orientation of the distal and proximal epiphyseal plates of the radius. Acta Orthop Scand 1979;50:731-739. [DOI] [PubMed] [Google Scholar]
- 13.Paley D. Oblique plane deformity. In: Principles of Deformity Correction. Berlin: Springer, 2002:175-194. [Google Scholar]
- 14.Shapiro F. Developmental patterns in lower-extremity length discrepancies. J Bone Joint Surg [Am] 1982;64-A:639-651. [PubMed] [Google Scholar]
- 15.Paley D, Bhave A, Herzenberg JE, Bowen JR.. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg [Am] 2000;82-A:1432-1446. [DOI] [PubMed] [Google Scholar]
- 16.De Maio F, Corsi A, Roggini M, et al. Congenital unilateral posteromedial bowing of the tibia and fibula: insights regarding pathogenesis from prenatal pathology. A case report. J Bone Joint Surg [Am] 2005;87-A:1601-1605. [DOI] [PubMed] [Google Scholar]
- 17.Nogami H, Oohira A, Kuroyanagi M, Mizutani A.. Congenital bowing of long bones: clinical and experimental study. Teratology 1986;33:1-7. [DOI] [PubMed] [Google Scholar]
- 18.Catagni MA, Radwan M, Lovisetti L, Guerreschi F, Elmoghazy NA.. Limb lengthening and deformity correction by the Ilizarov technique in type III fibular hemimelia: an alternative to amputation. Clin Orthop Relat Res 2011;469:1175-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saleh M, Goonatillake HD.. Management of congenital leg length inequality: value of early axis correction. J Pediatr Orthop B 1995;4:150-158. [DOI] [PubMed] [Google Scholar]
- 20.Popkov AV, Kononovich NA, Gorbach EN, et al. Bone healing by using Ilizarov external fixation combined with flexible intramedullary nailing versus Ilizarov external fixation alone in the repair of tibial shaft fractures: experimental study. ScientificWorldJournal 2014;2014:239791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Popkov D, Lascombes P, Journeau P, Popkov A.. Current approaches to flexible intramedullary nailing for bone lengthening in children. J Child Orthop 2016;10:499-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Georgiadis AG, Rossow JK, Laine JC, Iobst CA, Dahl MT.. Plate-assisted Lengthening of the Femur and Tibia in Pediatric Patients. J Pediatr Orthop 2017;37:473-478. [DOI] [PubMed] [Google Scholar]
- 23.Harbacheuski R, Fragomen AT, Rozbruch SR.. Does lengthening and then plating (LAP) shorten duration of external fixation? Clin Orthop Relat Res 2012;470:1771-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rozbruch SR, Zonshayn S, Muthusamy S, et al. What risk factors predict usage of gastrocsoleus recession during tibial lengthening? Clin Orthop Relat Res 2014;472:3842-3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Belthur MV, Paley D, Jindal G, et al. Tibial lengthening: extraarticular calcaneotibial screw to prevent ankle equinus. Clin Orthop Relat Res 2008;466:3003-3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gordon JE, Schoenecker PL, Oda JE, et al. A comparison of monolateral and circular external fixation of unstable diaphyseal tibial fractures in children. J Pediatr Orthop B 2003;12:338-345. [DOI] [PubMed] [Google Scholar]
- 27.Journeau P, Lascombes P, Barbier D, Popkov D.. Residual bone growth after lengthening procedures. J Child Orthop 2016;10:613-617. [DOI] [PMC free article] [PubMed] [Google Scholar]


