Abstract
Research has linked trauma-sequelae, such as posttraumatic stress disorder, to aggression. However, not all who experience a trauma become violent, suggesting non-trauma factors, such as emotion dysregulation, influence aggression expression and if confirmed, may influence treatment approaches. Aggression can be considered a multifaceted construct with Impulsive Aggression (IA) as emotional, reactive, and uncontrolled and Premeditated Aggression (PA) as deliberate, planned, and instrumental. We hypothesized that parceling apart IA and PA may further refine predictors of aggression in the context of trauma exposure. We tested this hypothesis in undergraduate women (N = 208) who completed trauma, emotion, and aggression measures. Path analysis indicated that Borderline Features, including emotion dysregulation, mediated the relationship between trauma exposure and IA and PA. The finding extends clinical literature by providing evidence that emotion dysregulation influences both IA and PA in a non-clinical sample, while clinical sample research shows emotion dysregulation more specifically mediated the relationship between trauma and IA. Factors responsible for these differences are discussed.
Keywords: Impulsive Aggression, Premeditated Aggression, Emotion dysregulation, Trauma exposure
1. Introduction
Worldwide, violence is one of the leading causes of death for people between the ages of 15 and 44 (World Health Organization, 2002). In the United States, violence and injuries cost more than $406 billion in medical care and lost productivity per year (Finkelstein, Corso, & Miller, 2006). Understanding individual differences in aggression expression may be critical to accurate violence prevention and treatment.
Emotion regulation has been examined in an attempt to understand the underlying mechanisms of aggression. Emotion regulation is the ability to recognize and accept emotions along with the skills to control impulses and utilize context-appropriate regulation strategies (Gratz & Roemer, 2004). Ineffective emotion regulation is referred to as emotion dysregulation and has been related to aggression. In a community sample of violent individuals, emotion dysregulation was associated with aggressive acts even after controlling for normative beliefs about aggression and education level (Roberton, Daffern, & Bucks, 2014). Similarly, in a treatment-seeking sample of individuals with borderline personality disorder (BPD), emotion dysregulation at three months into treatment fully mediated the relationships between BPD and psychological and physical aggression at nine months (Scott, Stepp, & Pilkonis, 2014).
These findings (Roberton et al., 2014; Scott et al., 2014) suggest the inability to regulate emotions is related to overall aggression, yet aggression is not universally considered a one-dimensional construct. Two primary aggression subtypes have been identified— Impulsive and Premeditated (Stanford et al., 2003). Impulsive Aggression can be characterized as emotionally charged, reactive, and uncontrolled. Impulsive Aggression can be contrasted with Premeditated Aggression which is deliberate, instrumental, and planned (Stanford et al., 2003). It is important to note, the construct “Impulsive Aggression” only refers to the nature of the aggression rather than overarching personality structure of the aggressor. For example, a person can be impulsive and not aggressive, and both Impulsive and Premeditated aggressors are generally impulsive and self-report anger (Barratt, Stanford, Kent, & Felthous, 1997b). Although most people primarily engage in one type of aggression, an individual can engage in both aggression types depending on the situation and individual difference factors (e.g. level of arousal, cognitions, and emotional state). The aggression types are not mutually exclusive; however, impulsive aggressors can be distinguished from premeditated aggressors by lower verbal skills, less sensitive neural arousal levels for novel stimuli, and fewer planned aggressive acts (Barratt et al., 1997b). Additionally, impulsive aggressive acts decreased when aggressors were given anticonvulsant medications, while Premeditated Aggression did not (Barratt, Stanford, Felthous, & Kent, 1997a). Therefore, studies that do not take aggression subtypes into account have the potential to obscure or wash-out important within-group variation among aggressive individuals.
Emerging evidence suggests symptoms and difficulties resulting from traumatic events, such as exposure to, or the threat of, death, injury, or sexual violence (American Psychiatric Association, 2013), are uniquely associated with Impulsive Aggression in clinical samples. In Veterans, Impulsive but not Premeditated Aggression was related to posttraumatic stress disorder (PTSD) diagnoses (Teten, Miller, Bailey, Dunn, & Kent, 2008; Teten et al., 2010), suggesting that Veterans with PTSD more often experience emotionally charged, reactive, and uncontrolled aggression rather than planned aggressive acts. Yet, even with this finding, few studies have examined emotion dysregulation and aggression together in trauma-exposed samples or parceled apart Premeditated and Impulsive Aggression. For example, Tull and colleagues (2007) found that for men who both experienced and perpetrated violence, experiential avoidance and lack of emotional expressivity (forms of emotion dysregulation) mediated the relationship between PTSD symptoms and behavioral hostility. However, the authors did not examine Impulsive and Premeditated Aggression separately, a nuance that may further refine predictors of aggression.
Additionally, Tull’s (2007) all-male sample that experienced and perpetrated violence may limit the generalizability of their findings to non-clinical, female samples. In the current study, we addressed this gap by testing if emotion dysregulation was related to Impulsive and Premeditated Aggression in a female, non-clinical sample with varying levels of trauma exposure. We selected a nonclinical sample to provide information on a group that may not be seeking psychiatric care but has a higher risk of experiencing traumatic events. Between 12.5% and 19% of collegiate women experience sexual assault (Krebs, Linquist, Warner, Fisher, & Martin, 2009; Walsh et al., 2012), a trauma that leads to 2.4–8.2 higher odds of victims developing PTSD than non-victims. In addition, young people are at risk for experiencing other traumatic events such as dating violence and motor vehicle accidents (Breiding et al., 2014; Centers for Disease Control and Prevention, 2012). The understanding of how emotion dysregulation influences aggression in these at-risk women has the potential to inform treatments for trauma and aggressive behavior.
In order to understand how collegiate women who may have experienced traumatic events could behave aggressively, we utilize the General Aggression Model (GAM: Anderson & Bushman, 2002). The model proposes that person and situation events (inputs) are registered and filtered through an individual’s present internal states, including affect, cognition, and arousal. This filter influences how the person will appraise a situation and his/her subsequent actions. The appraisal can be thoughtful or impulsive, which can lead to different outcomes. Following the outcome, the individual will appraise the encounter, creating a feedback loop to influence additional input interpretations resulting in general knowledge structures, or typical ways to interpret the environment. The input of a traumatic exposure and an internal state marked by emotion dysregulation may influence the individual to act in an impulsive aggressive manner. The GAM leads to the prediction that emotion dysregulation will mediate the relationship between trauma exposure and Impulsive Aggression (emotional and uncontrolled), but not the relationship between trauma exposure and Premeditated Aggression (controlled and planned).
2. Method
2.1. Participants
Participants were 214 undergraduate women from a private Southern university. Five participants were excluded for failing to meet the validity criteria (outlined below in Instrument and Procedure sections), and one participant was excluded for missing data. The remaining sample consisted of 208 undergraduates with an average age of 19.42 years (SD = 1.43). A mix of grade levels was represented with 40.9% of the participants being freshmen, 20.2% were sophomores, 20.2% were juniors, and 18.8% were seniors. Most participants identified as Caucasian (62.5%), followed by Hispanic (12.0%), Asian/Pacific Islander (11.5%), African American (9.1%), and “other” or multi-racial (4.8%). Participants that were excluded for invalid or missing data did not differ from the current sample in terms of age, gender, race, or year in school.
2.2. Instruments
2.2.1. The Personality Assessment Inventory – Short Form (PAI-SF)
The PAI-SF (Morey, 1991) is an abbreviate version of the 344-item PAI (Morey, 2007). The PAI-SF has 160 items answered on a 4-point scale from 0 (false, not at all true) to 3 (very true). Studies have demonstrated the PAI-SF had reliability (internal consistency) and validity (extra test correlates) comparable to the full PAI in census-matched normative (Morey, 2007), inpatient psychiatric (Sinclair et al., 2009), and forensic (Sinclair et al., 2010) samples. Selected PAI-SF validity and clinical scales were used in the current study (described below).
2.2.2. Validity scales
Infrequency (INF) is a 4-item scale that indicates if the participant is responding to items carelessly, randomly, or idiosyncratically. Raw scores greater than or equal to 5 reflect inconsistent responding. An example item is, “My favorite poet is Raymond Kertezc.” In the current sample, the internal consistently estimate (Cronbach’s alpha) was .17, which is to be expected since the scale measures random responding rather than a psychological construct.
Negative Impression (NIM) is a 4-item scale that assesses if the person is exaggerating or presenting an unfavorable impression. An example item is, “Sometimes I cannot remember who I am.” Raw scores greater than or equal to 6 represent an exaggerated unfavorable impression. The alpha coefficient was .24 in the current sample.
Positive Impression (PIM) is a 4-item scale that measures if the participant is trying to present a favorable impression and does not want to admit minor flaws. An example is the reversed scored item, “Sometimes I let little things bother me too much.” Raw scores greater than 11 represent an overly favorable impression. The alpha coefficient was .65 in the current sample.
2.2.3. Clinical scales
Borderline Features (BOR) is a 13-item scale that focuses on characteristics such as affective liability and instability, unstable and fluctuating interpersonal relations, and uncontrolled anger. This scale was chosen for our emotion dysregulation variable because emotion dysregulation is a core feature of borderline personality disorder (Linehan, 1993; Scott et al., 2014). An example BOR item is “My mood can shift quite suddenly.” Additionally, the scale has extra-test correlates with mood fluctuations, affect regulation measures, and impulse control difficulties (Morey, 2007). No items measure aggressive acts. The alpha coefficient was .86 in the current sample.
Drug problems (DRG) is a 7-item scale that focuses on negative consequences of drug use and dependence. An example item is “Sometimes I use drugs to feel better.” Raw scores equal to or greater than 10 represent a clinical range of drug problems. The alpha coefficient was .46 in the current sample.
Alcohol Problems (ALC) is a 4-item scale that assesses the problematic consequences of alcohol use and dependence. An example item is “There have been times when I’ve had to cut down on my drinking.” Raw scores equal to or greater than 5 represent a clinical level of alcohol problems. The alpha coefficient was .72 in the current sample.
2.2.4. Subtypes of aggression
Impulsive/Premeditated Aggression Scale (IPAS: Stanford, 2011; Stanford et al., 2003) is a 30-item measure that classifies an individual’s aggressive acts as either impulsive or premeditated. It asks participants about their aggressive acts in the past 6 months and has a 1 (strongly disagree) to 5 (strongly agree) scale. The Impulsive Aggression (IA) subscale consists of 10 items and presents a continuous score that ranged from 10 to 42 in the current sample. An IA example item is, “I feel I lost control of my temper during the [aggressive] acts.” The Premeditated Aggression (PA) scale consists of 8 items, and the current sample ranged from 8 to 38. A PA example item is “I planned when and where my anger was expressed.” The IPAS factor structure has been examined in college participants, including both sexes and a range of ethnicities that are representative of college samples (Haden, Scarpa, & Stanford, 2014). Alpha coefficients for the current sample were .81 for PA and .76 for IA.
Because the terms Impulsive Aggression and Borderline Features are used inconsistently in the literature, it is important to define the constructs that the current assessments measure. First, the classical view of borderline Impulsive Aggression involves self-mutilation, suicide, and substance use (Goodman & New, 2000). Our definition/assessment of Impulsive Aggression is “striking and/or verbally insulting another person or breaking/throwing objects” in an emotionally uncontrolled and unplanned way (Stanford, 2011) and does not reflect the individual’s larger personality structure. Additionally, the BOR scale of the PAI-SF measures affect instability and interpersonal difficulties and does not measure aggressive, suicidal, or self-mutilation acts. BOR and IA were chosen to avoid content overlap between the current study’s constructs.
2.2.5. Trauma exposure
The Brief Betrayal Trauma Survey (BBTS; Goldberg & Freyd, 2006) is a 12-item measure that assesses trauma exposure for a range of events from natural disasters to sexual assault. Each trauma type was described, and participants chose one of the following responses to describe how many times they had experienced that particular trauma: 0 (never), 1 (one or two times), and 2 (more than that). The BBTS was scored two ways: 1.) For sample description purposes, we examined the frequencies of low betrayal traumas (natural disasters, motor vehicle accident, or seeing another person to whom you are not close experience a trauma), medium betrayal traumas (being traumatized by someone you are not close to, seeing someone you are very close to committing suicide, being injured, and/or attacking another family member), and high betrayal traumas (trauma was perpetrated by someone the victim was very close to), and 2.) We created a summed variable to count the total number of traumas experienced, with scores greater than 1 indicating the person experienced at least one trauma. Total scores ranged from 0 to 17. Since we used this instrument as a measure of trauma frequencies internal consistency estimates were not relevant (Kazdin, 2003).
2.3. Procedure
As part of an introductory psychology class requirement, all participants were required to participate in psychological research or write a brief psychology-related report. Participants for this study were recruited by an online departmental website. Informed consent and all measures were completed online in the same order for every participant (IPAS, BBTS and PAI-SF). Prior to data collection, the study was approved by the university’s institutional review board and the local Veterans Affairs Research and Development Committee, as this was the IRB of record for the lead author.
2.4. Data analysis
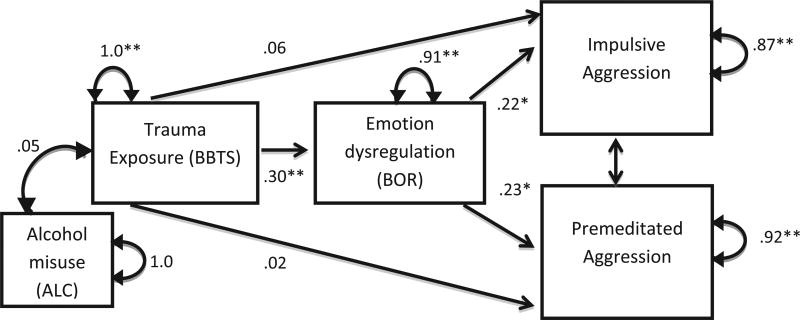
Descriptive statistics were used to examine demographic variables. Means and standard deviations are reported for the IPAS, PAI-SF, and BBTS. Pearson’s correlations examined the relationships between measures. We examined in a path analysis if Borderline Features (BOR) mediated the relationship between trauma exposure (BBTS) and both Impulsive Aggression (IA) and Premeditated Aggression (PA) while controlling for alcohol misuse (ALC; Fig. 1). Age, ACL and DRG were examined for their association with IA in order to detect potential covariates. The path analysis used bootstrapping (1000 samples) to generate 95% bias-correct and accelerated confidence intervals (BCa CIs) for the indirect effects. Bootstrapping takes random samples (with replacement) from the existing data to estimate sampling distribution properties by creating thousands of smaller samples, ordering them into a bootstrap sample, and calculating the mediation effect on the newly created bootstrap sample. Bootstrapping controls for violations of normality and is a more robust method than classical regression to test mediation models. If the BCa CIs do not contain 0, the effect is considered statistically significant (Preacher & Hayes, 2004). All coefficients are reported as standardized estimates.
Fig. 1.
Path analysis examining the mediating role of emotion dysregulation for the relationships between trauma exposure and Impulsive and Premeditated Aggression.
To detect if relationship between BBTS, BOR, and IA was due to shared method variance between the self-report measures BBTS and BOR, we used path analysis to run an additional mediation model predicting IA and PA with BBTS as the mediator and BOR as the independent variable.
3. Results
3.1. Descriptives
The mean number of endorsed traumas was 3.62 (SD = 3.60). The most frequent number of traumas was one (16.3%), and 18.3% of the sample endorsed no trauma exposure. About 64% of the participants reported experiencing a low betrayal trauma, 55.8% reported experiencing a medium betrayal trauma, and 41.3% reported experiencing a high betrayal trauma. The PAI-SF mean scores were all below clinical cutoffs (Table 1).
Table 1.
Measure descriptives and correlations in collegiate women (N = 208).
| M | SD | ALC | DRG | BBTS | BOR | IA | PA | |
|---|---|---|---|---|---|---|---|---|
| ALC | 0.55 | 1.28 | 1 | |||||
| DRG | 1.66 | 2.46 | .24** | 1 | ||||
| BBTS | 3.63 | 3.60 | .26** | .15* | 1 | |||
| BOR | 11.41 | 6.84 | .31** | .29** | .31** | 1 | ||
| IA | 27.13 | 5.43 | .17** | .07 | .11 | .22** | 1 | |
| PA | 21.83 | 5.12 | .13 | .03 | .12 | .26** | .14* | 1 |
Note:
p < .05.
p < .01.
ALC = Alcohol Problems. DRG = Drug Problems. BBTS = Brief Betrayal Trauma Inventory sum score. BOR = Borderline Features. IA = Impulsive Aggression. PA = Premeditated Aggression.
Table 1 also displays correlations between the measures for the total sample. Neither IA nor PA were significantly correlated with BBTS. IA and PA were both related to BOR (r = .22 and r = .26, respectively, p’s < .01). ALC was correlated with IA (r = .17, p = .01), but not PA (r = .13, p = .29).
3.2. Mediation models
Pearson correlations showed that ALC (r = .17, p = .01), but not DRG (r = .07, p = .29) or age (r = −.10, p = .16), was correlated with IA. ALC was entered as the only covariate in the path analyses.
The first path analysis (Fig. 1) tested the mediating role of BOR between trauma exposure (BBTS) and the two types of aggression (IA and PA), while controlling for alcohol problems (ALC). Overall, the model produced good fit as evidenced by a statistically significant Chi-square (X2(9, N = 208) = 69.03, p < .001) and Root Mean Square Error of Approximation (RMSEA) less than .0001. IA and PA were not significantly related, providing additional evidence that the two aggression subtypes represent different constructs (Barratt et al., 1997b). The direct effects of BBTS with impulsive (β = .06, p = .35) or premeditated (β = .02, p = .75) aggression were not significant while holding all other variables constant. However, BOR was significantly related to both types of aggression (impulsive β = .22, p = .004; premeditated β = .23, p = .002), while holding all other variables constant. The model was further clarified by the indirect effects. BOR produced two significant indirect effect between BBTS and IA, (β = .067, SE = .030, BCa CIs = 0.013, 0.122), and the relationship between BBTS and PA (β = .069, SE = .029, BCa CIs = 0.015, 0.123). Significant indirect effects can occur when the independent variable does not directly predict the dependent variable (Hayes, 2009). The model explained 13% of the variance in IA and 8% of variance in PA.
To determine if the relationship between trauma exposure and emotion dysregulation was due to shared method variance between the self-report measures BBTS and BOR, we ran another path analysis with BBTS as the mediator and BOR as the independent variable, while controlling for alcohol misuse. While the model still evidenced good fit [X2(9, N = 208) = 68.75, p < .001) and RMSEA < .0001], BBTS was not a mediator between BOR and IA (indirect effect β = .02, p = .36) or between BOR and PA (indirect effect β = .007, p = .74).
4. Discussion
This study examined the underlying mechanisms of Impulsive and Premeditated Aggression in a non-clinical, collegiate female sample. Most participants endorsed experiencing at least one traumatic event, consistent with previous estimates that 50–90% of people will experience a minimum of one trauma during their lives (Felitti et al., 1998; Norris & Slone, 2007). Even with trauma exposure being common, the participants did not elevate the PAI-SF scales and produced lower aggression scores than previous work that utilized male and female Veteran samples (e.g. Miles et al., in press; Teten et al., 2010).
No direct relationship emerged between trauma exposure and either type of aggression. Given that previous research found positive relationships between PTSD symptoms and aggression (Taft, 2011), particularly Impulsive Aggression (Teten et al., 2008, 2010), the present results could reflect the fact that we did not directly assess PTSD symptoms and the sample scored within the normal range on PAI-SF scales, suggesting the amount of distress was low.
Significant positive correlations between BOR and aggression were found. The correlations of IA and PA with BOR, a scale that measures affective instability, are consistent with previous work that shows IA and PA are both related to impulsivity, anger (Barratt et al., 1997a, 1997b), and emotion dysregulation (Miles et al., in press).
While trauma exposure was not related to aggression in bivariate relationships, the path analysis showed that BOR produced significant indirect paths for the relationships between trauma exposure and IA and PA. A second path analysis showed the results were not simply due to shared method variance between BBTS and BOR. While we predicted the indirect effect of BBTS through BOR to IA, the mediation effect for PA was unexpected based on our work with a clinical sample (Miles et al., in press), but again could have reflected the measurement of trauma exposure rather than PTSD symptoms. In our path analysis both aggression types were entered into one model, providing control over the effects of PA while examining IA, and vice versa. While our prior work indicated that there can be a dominant aggression type (Barratt et al., 1997a, 1997b) aggression subtypes are not mutually exclusive. Entering both aggression types into the same model allowed us to examine both types of outputs; however, this methodology also produced different results than previous studies. Future research with clinical samples should examine both aggression types in the same model.
The mediating role of BOR for trauma exposure and both IA and PA suggest that, unlike in clinical samples, emotion dysregulation may be an underlying mechanism in both Impulsive and Premeditated Aggression in healthy young women. One consequence of this finding is that to address potential aggression in this female sample, assessing emotion regulation abilities may be more important than understanding aggression type. It may be more informative to assess emotion regulation abilities and aggression type when working with psychiatrically severe samples.
Limitations of this study include our measure of emotion dysregulation (BOR), which measures other aspects of borderline personality disorder, such as interpersonal difficulties, in addition to emotion dysregulation. Future research should replicate the results with other emotion dysregulation measures. The cross-sectional nature of the data does not allow causal statements to be made about the directions of the relationships between trauma exposure, borderline features, and aggression; mediation analyses can only technically tested with longitudinal data. Finally, given the high rates of trauma exposure in college women, the sample is an important one to study; however, the sample was one of convenience and may have limited generalizability. Non-clinical samples with different educational backgrounds and clinical samples, such as patients with complex PTSD who likely have more difficulty regulating emotions and aggression, should be studied in the future.
Strengths include the PAI-SF validity scales because invalid response profiles were excluded. We omitted participants who answered questions in an inconsistent, overly positive, or overly negative way. Additionally, having a non-clinical, relatively psychologically healthy sample extends the generalizability of the Tull (2007) findings that emotion dysregulation plays a mediating role between trauma sequelae and aggression. An all female sample is inconsistent with much of the aggression research (Stanford et al., 2003; Teten et al., 2010; Tull et al., 2007), and thus addresses a critical gap.
In summary, research has linked trauma-sequelae, such as PTSD, to aggression (Marshall, Panuzio, & Taft, 2005; Taft et al., 2011). However, not all who experience a trauma become violent, so understanding what other factors influence aggression expression can inform both prevention and treatment of aggression. Impulsive and Premeditated Aggression expressed by individuals with trauma exposure is related to emotion dysregulation, even in relatively healthy young adults. While preventing traumatic events from occurring would be ideal, if an individual experiences trauma, early emotion regulation treatment may reduce the emergence of aggressive behavior and strengthen non-aggressive, problem-solving approaches. Similarly, if treating aggressors, it may be helpful to assess if the offender has trauma-exposure and make trauma processing a treatment goal in order to reduce aggression.
Acknowledgments
Source of funding
This material is based upon work supported (or supported in part) by the Department of Veterans Affairs, Veterans Health Administration, the South Central Mental Illness Research, Education and Clinical Centers (SCMIRECC), the Traumatic Brain Injury, Center of Excellence, and the Houston VA HSR&D Center for Innovations in Quality, Effectiveness, and Safety (CIN13-413), Houston TX. The funding sources had no role in the study design; in the collection, analysis, or interpretation of the data; in the writing of the manuscript; or in the decision to submit the paper for publication. The views expressed, findings, and conclusions in this report are those of the authors and do not necessarily represent the official position or policy of the Centers for Disease Control and Prevention, the Department of Veterans Affairs, the South Central MIRECC, Baylor College of Medicine, or the United States government.
Biographies

Shannon Reynolds Miles, James A. Haley Veterans Hospital
Carla Sharp, University of Houston

Matthew S Stanford, Hope and Healing Center & Institute

Deleene S Menefee, Michael E. DeBakey VA Medical Center
Footnotes
Conflicts of interest
The authors report no financial conflicts of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Anderson CA, Bushman BJ. Human aggression. Annual Review of Psychology. 2002;53:27–51. doi: 10.1146/annurev.psych.53.100901.135231. [DOI] [PubMed] [Google Scholar]
- Barratt ES, Stanford MS, Felthous AR, Kent TA. The effects of phenytoin on impulsive and premeditated aggression: A controlled study. Journal of Clinical Psychopharmacology. 1997a;17:341–349. doi: 10.1097/00004714-199710000-00002. [DOI] [PubMed] [Google Scholar]
- Barratt ES, Stanford MS, Kent TA, Felthous A. Neuropsychological and cognitive psychophysiological substrates of impulsive aggression. Biological Psychiatry. 1997b;41:1045–1061. doi: 10.1016/s0006-3223(96)00175-8. [DOI] [PubMed] [Google Scholar]
- Breiding M, Smith S, Basile K, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization — National intimate partner and sexual violence survey, United States, 2011. Morbidity and Mortality Weekly Report. 2014;63:1–18. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2012 (Online Data file). Retrieved from< http://www.cdc.gov/injury/wisqars/index.html>.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Corso PS, Miller TR. Incidence and economic burden of injuries in the United States. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Goldberg LR, Freyd JJ. Self-reports of potentially traumatic experiences in an adult community sample: Gender differences and test-retest stabilities of the items in a Brief Betrayal–Trauma Survey. Journal of Trauma & Dissociation. 2006;7:39–63. doi: 10.1300/J229v07n03_04. [DOI] [PubMed] [Google Scholar]
- Goodman M, New A. Impulsive aggression in borderline personality disorder. Current Psychiatry Reports. 2000;2:56–61. doi: 10.1007/s11920-000-0043-1. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–55. [Google Scholar]
- Haden SC, Scarpa A, Stanford MS. Validation of the Impulsive/ Premeditated Aggression Scale in college students. Journal of Aggression, Maltreatment, & Trauma. 2014;17I(3):352–373. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. http://dx.doi.org/10.1080/03637750903310360. [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 4. Boston, MA: Allyn & Bacon; 2003. [Google Scholar]
- Krebs CP, Linquist CH, Warner TD, Fisher BS, Martin SL. College women’s experiences with physically forced, alcohol- or other drug-enabled, and drug-facilitated sexual assault before and since entering college. Journal of American College Health. 2009;57:639–647. doi: 10.3200/JACH.57.6.639-649. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Publications Inc.; 1993. [Google Scholar]
- Marshall AD, Panuzio J, Taft CT. Intimate partner violence among military veterans and active duty servicemen. Clinical Psychology Review. 2005;25:862–876. doi: 10.1016/j.cpr.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Miles SR, Menefee D, Wanner J, Tharp AT, Kent T. The relationship between emotion dysregulation and impulsive aggression in veterans with posttraumatic stress disorder symptoms. Journal of Interpersonal Violence. doi: 10.1177/0886260515570746. (in press) [DOI] [PubMed] [Google Scholar]
- Morey LC. The Personality Assessment Inventory professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Morey LC. Personality Assessment Inventory (PAI): Professional manual. 2. Lutz, FL: Psychological Assessment Resources, Inc.; 2007. [Google Scholar]
- Norris FH, Slone LB. The epidemiology of trauma and PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York, NY: The Guildford Press; 2007. pp. 78–98. [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple medication models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Roberton T, Daffern M, Bucks RS. Maladaptive emotion regulation and aggression in adult offenders. Psychology, Crime and Law. 2014;20:933–954. [Google Scholar]
- Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Personality Disorders: Theory, Research, and Treatment. 2014;5:278–288. doi: 10.1037/per0000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair SJ, Antonius D, Shiva A, Siefert CJ, Kehl-Fie K, Lama S, et al. The psychometric properties of the Personality Assessment Inventory-Short Form (PAI-SF) in inpatient forensic and civil samples. Journal of Psychopathology and Behavioral Assessment. 2010;32:406–415. [Google Scholar]
- Sinclair SJ, Siefert CJ, Shorey HS, Antonius D, Shiva A, Kehl-Fie K, et al. A psychometric evaluation of the Personality Assessment Inventory – Short Form clinical scales in an inpatient psychiatric sample. Psychiatry Research. 2009;170:262–266. doi: 10.1016/j.psychres.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Stanford MS. Procedures for the classification of aggressive/violent acts. Waco, TX: Department of Psychology and Neuroscience, Baylor University; 2011. [Google Scholar]
- Stanford MS, Houston RJ, Mathias CW, Vilemarette-Pittman NR, Helfritz LE, Conklin SM. Characterizing aggressive behavior. Assessment. 2003;10:183–190. doi: 10.1177/1073191103010002009. [DOI] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, Monson CM. Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology. 2011;79:22–33. doi: 10.1037/a0022196. [DOI] [PubMed] [Google Scholar]
- Teten AL, Miller LA, Bailey SD, Dunn N, Kent TA. Empathic deficits and alexithymia in trauma-related impulsive aggression. Behavioral Sciences & The Law. 2008;26:823–832. doi: 10.1002/bsl.843. [DOI] [PubMed] [Google Scholar]
- Teten A, Schumacher J, Taft C, Stanley M, Kent T, Bailey S, et al. Intimate partner aggression perpetrated and sustained by male Afghanistan, Iraq, and Vietnam veterans with and without posttraumatic stress disorder. Journal of Interpersonal Violence. 2010;25:1612–1630. doi: 10.1177/0886260509354583. [DOI] [PubMed] [Google Scholar]
- Tull MT, Jakupcak M, Paulson A, Gratz KL. The role of emotional inexpressivity and experiential avoidance in the relationship between posttraumatic stress disorder symptom severity and aggressive behavior among men exposed to interpersonal violence. Anxiety, Stress and Coping. 2007;20:337–351. doi: 10.1080/10615800701379249. [DOI] [PubMed] [Google Scholar]
- Walsh K, Danielson CK, McCauley JL, Saunders BE, Kilpatrick DG, Resnick HS. National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Archives of General Psychiatry. 2012;69(9):935–942. doi: 10.1001/archgenpsychiatry.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. World report on violence and health. Geneva: Author; 2002. [Google Scholar]