Abstract
Chronic Total Occlusion (CTO) intervention is a challenging area in interventional cardiology. Presently about 70% of CTO interventions are successful.
Materials and methods
This was a single center prospective study of a cohort of all patients undergoing percutaneous coronary intervention (PCI) as elective or adhoc procedure for CTO from August 2014 to June 2015. Only antegrade CTO interventions were included. In all patients the following data were recorded.
Results
A total of 210 (8.9% of total PCI (2353) during the study period) CTO patients were followed up. The mean age was 56.54 ± 8.9. In the study sixty nine patients (32.9%) presented with chronic stable angina and rest of the patients had history of acute coronary syndrome of which 22.9% (n = 48) had unstable angina (UA) or non ST elevation myocardial infarction (NSTEMI) and 44.2% (n = 93) had ST Elevation Myocardial Infarction (STEMI). In those with history of ACS, 64.78% (n = 92) had ACS during the previous year and remaining 35.22% (n = 49) had ACS prior to that. Single vessel CTO was seen in 89.5% (n = 188) and two vessel CTO in 10.5% (n = 22). LAD was involved in 36.7% (n = 77), RCA in 48.1% (n = 101), and LCX in 15.2% (n = 32). Procedural success in the first attempt was 68.1% (n = 143), which increased to 71.42% (n = 150) after the second attempt. CTO interventions were more frequently successful when the calcium was absent or minimal (p-0.05), CTO length was <10 mm (p < 0.01) and good distal reformation (p < 0.01).
Keywords: CTO intervention, Percutaneous coronary intervention, Coronary angioplasty
1. Introduction
Coronary chronic total occlusion is defined as an occluded coronary segment with thrombolysis in myocardial Infarction (TIMI) flow 0 for ≥three months duration.1,2 In clinical practice, coronary CTOs are commonly encountered, with a prevalence rate of 18–52% among patients undergoing coronary angiography.3,4 The clinical benefit of CTO revascularization continues to be debated. Several observational studies have shown that successful CTO revascularization improves cardiovascular outcomes.5,6 A meta-analysis by Hoebers et al. found that successful revascularization of CTO improved the left ventricular ejection fraction,7 which is not supported by EXPLORE trial results though improvement in subgroup of patient with viable CTO territory was seen.19 The DECISION-CTO trial whose results were presented in ACC 2016 March showed that routine CTO-PCI + OMT is not superior to OMT alone in reducing cardiovascular outcomes among patients with at least one CTO and the management of CTO patients is still a matter of debate.
Chronic Total Occlusion intervention is a demanding area in coronary interventions. CTO interventions are cumbersome requiring more time and hardware and are more costly. CTO interventions have a higher rate of complications when compared to non- CTO interventions. However dedicated equipments and better techniques have kindled the interest in CTO interventions. High rates of success and low rates of complications are now achieved by expert operators, even in complex cases.8,9 The PROGRESS CTO complications scoring is a new and useful scoring system for predicting complications in patients undergoing CTO PCI.18
The last European Society of Cardiology guidelines assigned only a class IIa (level of evidence B) to CTO PCI in ‘patients with expected ischaemia reduction in a corresponding myocardial territory and/or angina relief’,10 which is reasonable in view of the recent results of DECISION CTO trial and Explore trial.19
The J-CTO registry (multicenter CTO registry in Japan) led to the development of J-CTO (Japanese Multicenter CTO registry) score to predict the likelihood of successful guidewire crossing within 30 min.11 Independent angiographic predictors of failure (each given one point) that made up the J-CTO score included prior failed attempt, angiographic evidence of heavy calcification, bending within the occluded segment, blunt proximal stump, and occlusion length >20 mm. Chronic total occlusions were then graded as easy, intermediate, difficult, and very difficult (J-CTO scores of 0, 1, 2, and ≥3, respectively).
2. Materials and methods
The study was a prospective study of a cohort of all patients undergoing PCI as elective or adhoc procedure for CTO in the department of Cardiology Government Medical College, Thiruvananthapuram from August 1st 2014 to June 30th 2015.
2.1. Inclusion criteria
All patients undergoing PCI as elective or adhoc procedure for CTO in the department of Cardiology Government Medical College, Thiruvananthapuram from August 1st 2014 to June 30th 2015 were included in the study.
CTO was defined as a high-grade coronary occlusion with reduced antegrade flow (Thrombolysis in Myocardial Infarction [TIMI] grade 0 flow) with estimated duration of at least 3 months.
2.2. Exclusion criteria
Exclusion criteria included patients with an estimated CTO duration less than 3 months, CTO vessel size <2.5 mm, retrograde approach for CTO intervention, second or third attempt failed CTO interventions and second or third vessel CTO interventions of multi vessel CTO, in-stent total occlusion, status post Coronary Artery Bypass Graft surgery (CABG), Chronic Kidney Disease (CKD) with a baseline e GFR <30 ml/min/1.73 m2, retrograde approach for CTO, inability to take antiplatelets and left ventricular ejection fraction less than 30%.
2.3. Definitions
CTO was defined as a lesion showing a complete occlusion of the coronary vessel with antegrade TIMI 0 flow with an estimated 3 months or more duration.
Procedural success was defined as successful CTO recanalization with achievement of <30% residual diameter stenosis within the treated segment and restoration of TIMI grade-3 antegrade flow.
2.4. Procedure
All patients were pre-treated with aspirin and clopidogrel (a loading dose of 300 mg at least 6 h before the procedure).After the procedure, all patients were on dual antiplatelet therapy with aspirin and one of clopidogrel or prasugrel or ticagrelor. Baseline characteristics procedural and angiographic characteristics were recorded.
Peri-procedural complications were recorded and included coronary perforation with or without tamponade, heart failure (requiring NTG and diuretic), cardiogenic shock, sustained ventricular tachycardia (VT) and atrial fibrillation.
Immediate outcomes before the discharge of the patient which included death, ACS – STEMI, NSTEMI, unstable angina, stroke (ischemic/hemorrhagic), renal failure, need for urgent revascularization(PCI/CABG) and stent thrombosis and six month outcomes in terms of NYHA functional class of angina and dyspnea, death, ACS – STEMI, NSTEMI/UA,stroke-(ischemic/hemorrhagic), renal function, need for urgent revascularization (PCI/CABG),stent thrombosis, target vessel revascularization, heart failure requiring hospitalization, AF and sustained VT were recorded.
2.5. Data analysis
Continuous variables were analyzed by the student T-test, the discrete variables by chi-square test and paired ANOVA test wherever applicable. Statistical significance was assumed as P < 0.05.
3. Results
3.1. Baseline demographics
A total of 210 (8.9% of total PCI (2353) during the study period) CTO patients were followed up. The mean age was 56.54 ± 8.9. In the study sixty nine patients (32.9%) presented with chronic stable angina and rest o had history of acute coronary syndrome of which 22.9% (n = 48) had unstable angina (UA) or non ST elevation myocardial infarction (NSTEMI) and 44.2% (n = 93) had ST Elevation Myocardial Infarction (STEMI). In those with history of ACS, 64.78% (n = 92) had ACS during the previous year and remaining 35.22% (n = 49) had ACS prior to that. The base line patient characteristics are shown in Table 1.
Table 1.
Patient demographics.
| Frequency | Percentage | ||
|---|---|---|---|
| Age | ≤60 | 133 | 63.3 |
| >60 | 77 | 36.7 | |
| Gender | Male | 170 | 81.0 |
| Female | 40 | 19.0 | |
| Diabetes mellitus | No | 139 | 66.2 |
| Yes | 71 | 33.8 | |
| Systemic Hypertension | No | 100 | 47.6 |
| Yes | 110 | 52.4 | |
| Smoking habit | No | 111 | 52.9 |
| Yes | 99 | 47.1 | |
Single vessel CTO was seen in 89.5% (n = 188) and two vessel CTO in 10.5% (n = 22). LAD was involved in 36.7% (n = 77), RCA in 48.1% (n = 101), and LCX in 15.2% (n = 32).
3.2. Lesion characteristics
J-CTO score in the cohort was J- CTO < 1–13.3% (n = 28) J- CTO = 2–50.5% (n = 106), J- CTO > 3–36.2% (n = 76). The lesion characteristics are shown in Table 2.
Table 2.
Nature of CTO Lesion.
| Frequency | Percentage | ||
|---|---|---|---|
| Size OF 1st CTO Vessel | 2.5–2.9 | 94 | 44.8 |
| 3.0–3.9 | 113 | 53.8 | |
| >4 | 3 | 1.4 | |
| Ending of CTO | Blunt | 162 | 77.1 |
| Tapering | 48 | 22.9 | |
| Site of CTO | Ostial | 26 | 12.4 |
| Proximal | 81 | 38.6 | |
| Mid | 77 | 36.7 | |
| Distal | 26 | 12.4 | |
| Calcium | No | 104 | 49.5 |
| Mild | 38 | 18.1 | |
| Moderate | 43 | 20.5 | |
| Severe | 25 | 11.9 | |
| Length of CTO | <10 | 57 | 27.1 |
| 10–20 | 90 | 42.9 | |
| >20 | 63 | 30.0 | |
| Collateral | Absent | 5 | 0.02 |
| Bridging | 98 | 46.7 | |
| Hetro | 27 | 12.9 | |
| Homo | 80 | 38.09 | |
| Distal Reformation | None | 7 | 3.3 |
| Poor | 96 | 45.7 | |
| Good | 107 | 51.0 | |
3.3. Procedural outcomes
Procedural success in the first attempt was 68.1% (n = 143), which increased to 71.42% (n = 150) after the second attempt.
The CTO interventions were more successful in younger patients and females. There were no difference in outcomes among diabetics, hypertensives or smokers. The relation between patient demographics and procedural success are shown in Table 3.
Table 3.
Patient demographic factors and success in the first attempt.
| Success (N = 143) |
Failure (N = 67) |
|||||
|---|---|---|---|---|---|---|
| N | % | N | % | P value | ||
| Age | ≤60 | 97 | 72.9 | 36 | 27.1 | 0.048 |
| >60 | 46 | 59.7 | 31 | 40.3 | ||
| Gender | Male | 106 | 62.4 | 64 | 37.6 | <0.001 |
| Female | 37 | 92.5 | 3 | 7.5 | ||
| Diabetes mellitus | No | 89 | 64 | 50 | 36 | 0.077 |
| Yes | 54 | 76.1 | 17 | 23.9 | ||
| Systemic hypertension | No | 65 | 65 | 35 | 35 | 0.359 |
| Yes | 78 | 70.9 | 32 | 29.1 | ||
| Smoking | No | 71 | 64 | 40 | 36 | 0.174 |
| Yes | 72 | 72.7 | 27 | 27.3 | ||
3.4. Procedural success and lesion characteristics
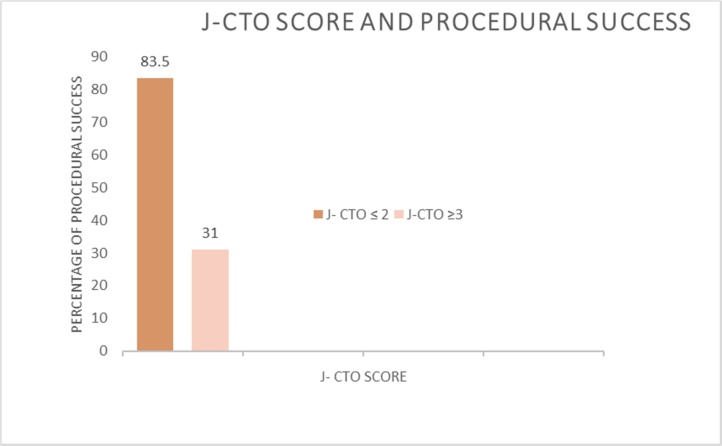
CTO interventions were more frequently successful when the calcium was absent or minimal, CTO length was <10 mm and good distal reformation. Table 4 shows the lesion characteristics and procedural success. Procedural success was more frequent in those with a J CTO score of ≤2 as shown in Fig. 1.
Table 4.
Nature of CTO occlusion lesion and successful intervention.
| Success (N = 143) |
Failure (N = 67) |
|||||
|---|---|---|---|---|---|---|
| N | % | N | % | P value | ||
| CTO stump | Blunt | 110 | 67.9 | 52 | 32.1 | 0.912 |
| Tapering | 33 | 68.8 | 15 | 31.3 | ||
| Site of CTO | Ostial | 17 | 65.4 | 9 | 34.6 | 0.010 |
| Proximal | 45 | 55.6 | 36 | 44.4 | ||
| Mid | 60 | 77.9 | 17 | 22.1 | ||
| Distal | 21 | 80.8 | 5 | 19.2 | ||
| Calcification | No | 75 | 72.1 | 29 | 27.9 | 0.005 |
| Mild | 32 | 84.2 | 6 | 15.8 | ||
| Moderate | 24 | 55.8 | 19 | 44.2 | ||
| Severe | 12 | 48 | 13 | 52 | ||
| Length of CTO | 0.0001 | |||||
| <10 | 56 | 98.2 | 3 | 1.8 | ||
| 10–20 | 58 | 65.2 | 31 | 34.8 | ||
| >20 | 29 | 46.8 | 33 | 53.2 | ||
| Collaterals | Absent | 3 | 60 | 2 | 40 | 0.0001 |
| Bridging | 50 | 51 | 48 | 49 | ||
| Hetro | 22 | 81.5 | 5 | 18.5 | ||
| Homo | 68 | 85 | 12 | 15 | ||
| Distal reformation | 0.003 | |||||
| Poor | 59 | 56.3 | 44 | 43.8 | ||
| Good | 84 | 78.5 | 23 | 21.5 | ||
Fig. 1.
J-CTO score and procedural success.
3.5. Procedural success and procedural characteristics
Femoral route was the access site for most of the complicated lesions and contralateral injections was taken in the most complex lesions. Procedural characteristics are shown in Table 5.
Table 5.
Procedural success and procedural characteristics.
| Success | Failure | |||||||
|---|---|---|---|---|---|---|---|---|
| N = 143 |
N = 67 |
|||||||
| N | % | N | % | Total | p | |||
| Route | Radial | 43 | 74.1 | 15 | 25.9 | 58 | 100 | 0.246 |
| Femoral | 100 | 65.8 | 52 | 34.2 | 152 | 100 | ||
| Contalateral Injection | No | 113 | 71.5 | 45 | 28.5 | 158 | 100 | 0.064 |
| Yes | 30 | 57.7 | 22 | 42.3 | 52 | 100 | ||
| Guide Catheter Size | 7F | 87 | 65.9 | 45 | 34.1 | 132 | 100 | 0.377 |
| 6F | 56 | 71.8 | 22 | 28.2 | 78 | 100 | ||
| Guide Catheter | CLS | 73 | 72.3 | 28 | 27.7 | 101 | 100 | 0.114 |
| JR | 49 | 70 | 21 | 30 | 70 | 100 | ||
| AL | 21 | 55.3 | 17 | 44.7 | 38 | 100 | ||
| JL | 0 | 0 | 1 | 100 | 1 | 100 | ||
| Side Hole | No | 115 | 73.7 | 41 | 26.3 | 156 | 100 | 0.003 |
| Yes | 28 | 51.9 | 26 | 48.1 | 54 | 100 | ||
| Wire Used to Cross the Lesion | BMW | 11 | 100 | 0 | 0 | 11 | 100 | |
| Whisper XT | 16 | 84.2 | 3 | 15.8 | 19 | 100 | ||
| Fielder XT | 11 | 100 | 0 | 0 | 11 | 100 | ||
| Cross IT 100 XT | 48 | 82.8 | 10 | 17.2 | 58 | 100 | ||
| Cross IT 200 XT | 10 | 83.3 | 2 | 16.7 | 12 | 100 | ||
| Cross IT 300 XT | 1 | 50 | 1 | 50 | 2 | 100 | ||
| Progress 40 | 1 | 33.3 | 2 | 66.7 | 3 | 100 | ||
| Progress 80 | 30 | 69.8 | 13 | 30.2 | 43 | 100 | ||
| Progress 120 | 7 | 28 | 18 | 72 | 25 | 100 | ||
| Progress 140 | 7 | 41.2 | 10 | 58.8 | 17 | 100 | ||
| Progress 200 | 1 | 11.1 | 8 | 88.9 | 9 | 100 | ||
3.6. Complications and in hospital outcomes
Access site complications occurred in 16 cases. This included TIMI minor bleed in 14 and pseudoaneurysms in 2 patients both were femoral. There were no major bleeds. Periprocedural myocardial infarction occurred in 10 cases. (4.8%). Coronary perforations occurred in 17 patients (8%), of which 12 were conservatively managed. Three cases required prolonged balloon inflation and two cases required pericardiocentesis. None required surgery. There were no in hospital death, acs or stroke.
3.7. Six months outcome
Angina class improved in 71.3% of those with procedural success and in 18.8% of failed cases. (p < 0.001). Dyspnea improved in 79.7% of those with procedural success and in 25.5% of failed cases. Death occurred in 1.2% (n = 2) and stroke in 1.2% (n = 2). Heart failure requiring hospitalization occurred in 1.5% (n = 3). There was no ACS or need for urgent revascularization.
4. Discussion
A total of 210 (8.9% of total PCI (2353) during the study period) CTO patients were followed up for a period of 6 months. The mean age of the patients was. 56.54 ± 8.9 A higher percentage of males underwent PCI for CTO in this study similar to the large UK registry database (78.8% males of 13443 CTO patients in UK data base).12 33.8% were diabetics, 52.4% were hypertensive and 47.1% were smokers.
There was involvement of LAD in 36.7% (n = 77), RCA in 48.1% (n = 101), and LCX in 15.2% (n = 32.) The JCTO score was ≥3 in 36.2%.
Procedural success in the first attempt was 68.1% (n = 143). The procedural success was similar to other major studies. A meta-analysis by Patel et al.13 of 65 studies with 18,061 patients and 18,941 target CTO vessels showed angiographic success 77%.
The patient demographic predictors of success were younger age, absence of diabetes mellitus and history of ACS. Procedural success was higher in younger patients (<60 years – 72.9% v/s 59.7% for those >60 years, p 0.048) similar to another large study.14 Procedural success was higher in female patients and was statistically significant (92.5% v/s 62.4% in males p < 0.001) which is much higher than seen in another large study (65.4% in females v/s 61.3% in males).12
The angiographic predictors of success were site CTO in mid and distal vessel, good distal reformation, short CTOs and absence of calcification or mild calcification similar to other registry data.12,15
Procedural success however was not affected by presence of bridging collaterals or nature of the stump which are usually highlighted as major negative factors. However a similar finding was observed by Salarifer et al.16 Coronary perforation rate (8%) was similar to the Japanese CTO registry (7.2%).17
5. Limitations
Small vessel CTO s (<2.5 mm) were not included in the study.
Retrograde approach was not included.
6. Conclusions
PCI is now an effective and safe modality of treatment in CTO with relatively high success rates and low complications with use of better wires and other gadgets and refined techniques in the contemporary era. However case selection is crucial and in this regard identifying the predictive factors for successful CTO intervention in a specific population is useful in selecting most suitable candidates for PCI.
A simplified expression of the results of our study is as follows. About 2/3 of the patients who underwent CTO intervention were aged less than 60 years. Nearly 1/3 of the patients were diabetic and ½ were smokers. Roughly ½ had right coronary artery CTO. 1/3 had J CTO score ≥3.
The predictors of procedural success were site of CTO being in the mid or distal portion of the vessel, short segment occlusion, lesions without calcification or minimal calcification and good distal reformation.
The presence of bridging collaterals or absent collaterals or a blunt stump were not found to be significantly affecting the procedural success rates.
Conflict of interest
There is no conflict of interest with any of the authors and the subject dealt.
Finance
No finance was required for the study.
References
- 1.Sianos G., Werner G.S., Galassi A.R. Recanalization of chronic total coronary occlusions: 2012 consensus document from the Euro CTO club. Euro Interv. 2012;8:139–145. doi: 10.4244/EIJV8I1A21. [DOI] [PubMed] [Google Scholar]
- 2.Carlino M., Magri C.J., Uretsky B.F. Treatment of the chronic total occlusion: a call to action for the interventional community. Catheter Cardiovasc Interv. 2015;85:771–778. doi: 10.1002/ccd.25736. [DOI] [PubMed] [Google Scholar]
- 3.Fefer P., Knudtson M.L., Cheema A.N. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59:991–997. doi: 10.1016/j.jacc.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Jeroudi O.M., Alomar M.E., Michael T.T. Prevalence and management of coronary chronic total occlusions in a tertiary Veterans Affairs hospital. Catheter Cardiovasc Interv. 2014;84:637–643. doi: 10.1002/ccd.25264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung C.M., Nakamura S., Tanaka K. Effect of recanalization of chronic total occlusions on global and regional left ventricular function in patients with or without previous myocardial infarction. Catheter Cardiovasc Interv. 2003;60:368–374. doi: 10.1002/ccd.10641. [DOI] [PubMed] [Google Scholar]
- 6.Baks T., van Geuns R.J., Duncker D.J. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J Am Coll Cardiol. 2006;47:721–725. doi: 10.1016/j.jacc.2005.10.042. [DOI] [PubMed] [Google Scholar]
- 7.Hoebers L.P., Claessen B.E., Elias J. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol. 2015;187:90–96. doi: 10.1016/j.ijcard.2015.03.164. [DOI] [PubMed] [Google Scholar]
- 8.Galassi A.R., Ganyukov V., Tomasello S.D. Successful antegrade revascularization by the innovation of composite core dual coil in a three-vessel total occlusive disease for cardiac arrest patient using extracorporeal membrane oxygenation. Eur Heart J. 2014;35:2009. doi: 10.1093/eurheartj/ehu070. [DOI] [PubMed] [Google Scholar]
- 9.Galassi A.R., Boukhris M., Tomasello S.D. Incidence, treatment, and in-hospital outcome of bifurcation lesions in patients undergoing percutaneous coronary interventions for chronic total occlusions. Coron Artery Dis. 2015;26:142–149. doi: 10.1097/MCA.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 10.Windecker S., Kolh P., Alfonso F. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2014;35:2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 11.Morino Y., Abe M., Morimoto T. Predicting successful guide wire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 12.George S., Cockburn J., Clayton T.C. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol. 2014;64:235–243. doi: 10.1016/j.jacc.2014.04.040. [DOI] [PubMed] [Google Scholar]
- 13.Patel Vishal G., Brayton Kimberly M., Tamayo M. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions. A weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6(2):128–136. doi: 10.1016/j.jcin.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 14.Galassi A.R., Sianos G., Werner G.S. Retrograde recanalization of chronic total occlusions in Europe: procedural, in-hospital, and long-term outcomes from the Multicenter ERCTO registry. J Am Coll Cardiol. 2015;65:2388–2400. doi: 10.1016/j.jacc.2015.03.566. [DOI] [PubMed] [Google Scholar]
- 15.Claessen B.E., Dangas G.D., Godino C. Impact of target vessel on long-term survival after percutaneous coronary intervention for chronic total occlusions. Catheter Cardiovasc Interv. 2013;82:76–82. doi: 10.1002/ccd.24579. [DOI] [PubMed] [Google Scholar]
- 16.Salarifar Mojtaba, Mousavi Mohammad-Reza, Sepideh Percutaneous coronary intervention to treat chronic total occlusion: predictors of technical success and one-year clinical outcome. Tex Heart Inst J. 2014;41(1):40–47. doi: 10.14503/THIJ-12-2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morino Y., Kimura T., Hayashi Y. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan) JACC Cardiovasc Interv. 2010;3:143–151. doi: 10.1016/j.jcin.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 18.Danek B.A., Karatasakis A., Karmpaliotis D. Development and validation of a scoring system for predicting periprocedural complications during percutaneous coronary interventions of chronic total occlusions: the prospective global registry for the study of chronic total occlusion intervention (PROGRESS CTO) complications score. J Am Heart Assoc. 2016;5(10):e004272. doi: 10.1161/JAHA.116.004272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elias J., van Dongen I.M., Hoebers L.P. Improved recovery of regional left ventricular function after PCI of chronic total occlusion in STEMI patients: a cardiovascular magnetic resonance study of the randomized controlled EXPLORE trial. J Cardiovasc Magn Reson. 2017;19:53. doi: 10.1186/s12968-017-0369-z. [DOI] [PMC free article] [PubMed] [Google Scholar]