Abstract
The annual incidence of sudden cardiac death (SCD) in athletes is significantly lower than the general population. However, when SCD occurs in an athlete during sporting event or training, it sends shockwaves in the society and raises questions about cardiovascular effects of sports and exercise. This document reviews the causes and mechanism of SCD in sports and exercise in young and older athletes. In the Indian context, we suggest a ‘pre-participation screening’ of young and older athletes and consider a ‘supervised, graded exercise regime’ for the uninitiated, older sports participant. Finally, the document proposes medical infrastructure required to successfully revive a victim of sudden cardiac arrest during a sporting event.
Abbreviations: ACLS, advanced cardiac life support; AED, automated external defibrillator; ALCA, anomalous left coronary artery; ARCA, anomalous right coronary artery; ARVC, arrhythmogenic right ventricular cardiomyopathy; ASCVD, atherosclerotic cardiovascular disease; BCLS, basic cardiac life support; CAD, coronary artery disease; CI, confidence interval; CMR, cardiac magnetic resonance; CPR, cardiopulmonary resuscitation; CV, cardiovascular; CPVT, catecholaminergic polymorphic ventricular tachycardia; EMR, emergency medical response; HCM, hypertrophic cardiomyopathy; IDCM, idiopathic dilated cardiomyopathy; LGE, late gadolinium enhancement; LV, left ventricle; LVH, left ventricular hypertrophy; LVWT, left ventricular wall thickness; MI, myocardial infarction; RR, relative risk; RV, right ventricle; SCA, sudden cardiac arrest; SCD, sudden cardiac death; STEMI, ST elevation myocardial infarction; VT, ventricular tachycardia; VF, ventricular fibrillation; WPW, Wolff-Parkinson-White
Keywords: Automated external defibrillator, Exercise, Resuscitation, Sudden cardiac death
1. Introduction
It is widely known and proven consistently by many studies that regular physical exercise significantly reduces the risk of cardiovascular death including SCD compared to sedentary lifestyle.1, 2 However, exercise and sports-related physical activity sometimes result in SCD especially in those athletes with underlying silent or unknown coronary, myocardial or valvular heart disease and channelopathies. This suggests that in predisposed individuals exercise may act as a trigger for the development of malignant arrhythmias. The occurrence of such an event in an athlete especially during a sporting event draws a lot of media attention and often raises doubt about the cardiovascular benefits of exercise.
A pre-participation screening consists of structured history and physical examination, and when necessary ECG and an echocardiogram to identify young, future athletes at risk of SCD. The older uninitiated individuals participating in popular marathons also need to be evaluated, especially for risk factors and symptoms of coronary artery disease (CAD). High-risk individuals may undergo exercise testing and be guided appropriately to primary prevention strategies; they likely will benefit from a supervised exercise program.
This document intends to briefly review the causes and mechanisms of SCD in athletes, sportsperson and marathoners; suggest pre-screening methods to be employed in India; recognize the physiological and pathological ECG and echocardiogram findings; recommend the manner of supervised exercise training and finally the resuscitative measures that should be available and implemented in the rare occurrence of such an event.
This guidance will benefit trainers and organizers of such events, sports physicians and additionally educate the participants. It hopefully will promote governmental sports and health ministry to take necessary steps to prevent SCD in both competitive and leisure athletes and in particular marathon runners, an ever-expanding sporting activity. In India, there is a need for national registries of athletic/sports/marathoners SCD rates and collection of data on pre-participation screening. This should help to frame customized guidelines to prevent SCD in athletes, sportspersons and marathoners.
2. Definition of an athlete
American College of Cardiology Sports and Exercise Cardiology Think Tank defines athlete as any individual who engages in routine vigorous physical exercise in the settings of competition, recreation, or occupation.3
A ‘competitive athlete’ is defined as an individual….
-
1)
Who participates in an organized team or individual sport,
-
2)
Who engages in regular competition against others,
-
3)
Who places a high priority or premium on athletic excellence and achievement,
-
4)
Who engages in vigorous training in a systematic fashion to achieve all the above goals.3, 4, 5, 6, 7
A ‘leisure athlete’ is defined as an individual…
-
1)
Who participates in a variety of informal recreational sports,
-
2)
Who engages in a range of exercise levels from modest to vigorous, either on regular or on inconsistent basis,
-
3)
Who does not necessarily require the pursuit of excellence or competition with others,
-
4)
Who does not necessarily require systematic vigorous training. 4, 5, 8
Most epidemiological studies define ‘older athlete or master athlete’ arbitrarily as an individual >35 year of age.7, 9 Some epidemiological studies define ‘young athlete’ arbitrarily as an individual between 12 and 35 years of age.10, 11
Sudden cardiac death in sports and exercise − is cardiac arrest occurring during or within 1 h of exercise or sports related activity.3
3. Epidemiology and causes of SCD in sports and exercise
The annual incidence of sports-related SCDs was reported to be 4.6 per 1 million population in a five-year prospective study12 as compared to 50–100 per million in the general population. The incidence and underlying cause of sudden death varies depending on the age, gender, race, ethnicity of the athlete, training level of athlete as well as the type of sport. Most sports-related SCD occurs in the middle-age group of 35 years or older13 or recreational athletes14 and 80% of these deaths are due to atherosclerotic CAD. The risk of sudden cardiac arrest (SCA) or SCD during training for the sports event is approximately 5-fold greater. 12 All adverse event rates are higher in occasional runners (1 per 7500–18000) compared with trained marathon runners (1 per 50,000–200,000).15
In younger athletes, the non-medical and traumatic causes constitute more than half of all deaths.16 The prevalence of cardiovascular (CV) diseases that predispose to SCD during sports in young athletes is estimated to be 0.2 to 0.7%.4, 7 The most frequent cardiac causes of SCD in young athletes are Sudden Arrhythmic Death Syndrome (56%), hypertrophic cardiomyopathy (HCM) (36–48%) and congenital anomalous coronary artery origin from opposite sinus (14–17%) while the less frequent causes are arrhythmogenic right ventricular cardiomyopathy (ARVC) (4–11%), myocarditis (6–7%) and ion channelopathies (4%).10, 11, 17, 18, 19 Atherosclerotic CAD is responsible for SCD in only 2–3% of younger athletes. The reported incidence of SCD in young athletes is variable in the literature. Maron et al17 reported 0.6 SCD per 100000 person-years in young competitive athletes in United States. Van Camp et al19 reported 0.4 SCD in 100,000 athletes per year, in high school and college athletes. Among young Italian athletes, Corrado et al10, 11 reported the incidence of SCD 3.6/100,000 person-years before routine pre-participation screening and 0.4/100,000 person-years after starting routine pre-participation screening. Among American Collegiate Athletes, Harmon et al16, 20 reported the overall incidence of SCD 1:53703 athlete-years. The SCD incidence was higher in Black athlete (1:21491 athlete-years) compared to White athletes (1:68354 athlete-years). The SCD incidence was highest in black basketball athletes (1 in 5348 athlete-years).
Various epidemiological studies on athletes and marathon runners published in the last decade have helped to establish the incidence and causes of SCD.21, 22, 23, 24, 25, 26, 27, 28 The causes of SCD in sportspersons are listed in Table 1.
Table 1.
| Types | Subtype | Pathology |
|---|---|---|
| Structural Disorders | Cardiomyopathy | HCM |
| Idiopathic LVH | ||
| ARVC | ||
| IDC | ||
| Marfan | Aortic root dilatation/rupture/dissection | |
| MVP | ||
| Valvular disease | Bicuspid aortic AS | |
| Pulmonic stenosis | ||
| Severe MR/AR | ||
| Disorders of Coronary Circulation | Congenital | ALCA from right sinus |
| ARCA from left sinus | ||
| Acquired | Atherosclerosis | |
| Electrical disorders | Ion channelopathies | Long QT syndrome |
| WPW syndrome | ||
| Brugada syndrome | ||
| Short QT syndrome | ||
| Ventricular Tachycardia | CPVT | |
| Ventricular Fibrillation | Sudden Arrhythmic Death Syndrome | |
| Acquired/Environmental | Sports injury | Commotio Cordis |
| Physical trauma | ||
| Heat stroke | Ventricular fibrillation | |
| Infection | Subacute Myocarditis | |
| Performance enhancing drugs | Myocardial infarction, Ventricular arrhythmias | |
| Hypothermia | Ventricular arrhythmias | |
Abbreviations; − ALCA, Anomalous Left Coronary Artery; AR, Aortic Regurgitation; ARCA, Anomalous Right Coronary Artery; ARVC, Arrhythmogenic Right Ventricular Cardiomyopathy; AS, Aortic Stenosis; CPVT, Catecholaminergic Polymorphic Ventricular Tachycardia; HCM, hypertrophic cardiomyopathy; IDC, Idiopathic Dilated Cardiomyopathy; LVH, Left Ventricular Hypertrophy; MR, Mitral regurgitation; MVP, Mitral Valve Prolapse; SCD, Sudden Cardiac Death; WPW, Wolff-Parkinson-White
4. Mechanism of SCD during sports and exercise
The catecholamine surge during exercise interacts unfavorably with the underlying arrhythmogenic substrate. Intense exercise can cause dehydration, hyperpyrexia, electrolyte imbalance and increased platelet aggregation, further facilitating ventricular tachycardia or fibrillation.21
4.1. Younger athletes
As mentioned earlier, HCM, idiopathic left ventricular hypertrophy (LVH), coronary anomalies, myocarditis, ARVC, Marfan’s syndrome, valvular heart disease, or ion channelopathies form an underlying substrate in the younger athlete. 7, 9, 21 Athletic training itself may unfavorably alter the substrate in HCM, ARVC and Marfan syndrome.29 The sports involving start-stop jolts like basketball and soccer have highest incidence of SCD in younger athletes than the endurance events like running.7, 16, 21, 30
HCM: the myocardial disarray and interstitial fibrosis and microvascular ischemia form a substrate for ventricular tachycardia (VT) or fibrillation (VF).
ARVC: the progressive fibrofatty replacement of the right ventricular (RV) myocardium forms the substrate for the arrhythmia. The propensity to ventricular arrhythmias with sport is more than at rest.10
Congenital coronary artery anomalies: the anomalies causing SCD during sports are left coronary artery origin in the right sinus of Valsalva (ALCA) and right coronary artery origin in the left sinus of Valsalva (ARCA).9 The ALCA or ARCA may have acute-angled take off or slit like ostial stenotic opening or intramural course. The proximal segment of the vessel may get compressed as it courses between the pulmonary artery and ascending aorta. The mechanism of SCD is related to exercise induced acute ischemia in left or the right coronary artery territory.
Marfan syndrome: the tunica media of the aorta may undergo cystic medial necrosis causing aortic root dilatation. The increase in aortic pressure during exercise may cause aortic dissection or rupture.21
Wolff-Parkinson-White syndrome: is characterized by pre-excitation due to anterograde conduction via accessory atrioventricular pathway. Exercise-related atrial fibrillation may cause rapid anterograde conduction via the accessory pathway and result in VF and SCD.31
Congenital Long QT Syndromes: abnormal cardiac repolarization (QTc interval >470 ms in males and >480 ms in females) predisposes to polymorphic VT/VF during exercise. SCD occurs more commonly during swimming or diving due to adrenergic surge with sudden cold-water immersion.32
Brugada Syndrome: SCD is caused by polymorphic VT/VF, that is more frequent at rest. In athletes with Brugada syndrome, the increased parasympathetic tone and core body temperatures >40 °C may precipitate fatal arrhythmias.21
Catecholaminergic Polymorphic VT: exercise provokes multifocal ventricular premature beats or VT with beat to beat alternation of the frontal plane QRS axis (bidirectional VT).
Commotio Cordis: a single blow on the precordium strategically timed 10 to 30 ms before the T-wave peak on the electrocardiogram can induce VF and cardiac arrest in persons with normal heart.21 The Commotio Cordis related SCD is seen in contact sports involving player collisions (football, martial arts etc.) or sports involving projectile objects. Since it occurs in normal heart, it can’t be prevented by screening but can only be treated by prompt resuscitation measures on the field.
Myocarditis: immune mediated myocardial inflammation in viral myocarditis predisposes to VT/VF during exercise. The risk may continue up to 6 months in convalescent period.
Performance-enhancing drugs: These drugs often used illegally can act as trigger or lead to development of an arrhythmogenic substrate. Anabolic androgenic steroids cause premature atherosclerosis, hypertension (HT), dyslipidemia and myocardial infarction. Ephedrine use leads to HT and cardiomyopathy. Recombinant human erythropoietin can cause HT and thromboembolism. Human growth hormone use leads to myocardial hypertrophy and fibrosis.33, 34
Premature coronary artery disease: Familial hypercholesterolemia in young adults causes premature coronary atherosclerosis and susceptibility to ischemia or myocardial infarction (MI).
4.2. Older athletes
In athletes older than 35 years of age, most deaths occur during long distance running sports.7, 9 In RACE Paris registry, SCDs due to CAD were demonstrated to have acute thrombotic occlusion in all cases,15 however, the RACER registry of 10 million runners found that SCD in persons with CAD occurs due to fixed coronary stenosis without any thrombosis.26 An autopsy series of SCD in general population showed higher incidence of plaque erosion (68% versus 23%) and intraplaque hemorrhage (71% versus 41%) in SCD with exercise versus SCD at rest.35
Therefore, there are two plausible hypotheses to explain the occurrence of ventricular tachyarrhythmia and cardiac arrest during sports activity −
1) Fixed coronary stenosis: the coronary flow cannot be augmented during exercise since the coronary vasodilatory reserve beyond stenosis is nearly exhausted and the diastolic period is shortened due to tachycardia. During exercise there is increased myocardial oxygen demand. The ischemia may get exacerbated by abrupt cessation of exercise that leads to reduced venous return, fall in blood pressure in a vasodilated state resulting in coronary hypoperfusion. The acute ischemia is further worsened by electrolyte imbalance, heat stroke36, 37 and excess circulating catecholamines.29 This eventually causes malignant ventricular arrhythmias either at peak effort or immediate post exercise.
2) Acute plaque rupture: The increased wall shear force on vulnerable plaque during exercise and catecholamine induced coronary spasm along with endothelial dysfunction cause erosion of the thin fibrous cap and/or intra-plaque hemorrhage and thrombosis. The high levels of circulating catecholamine potentiate platelet aggregation. The acute ST segment elevation myocardial infarction (STEMI) or non-STEMI leads to malignant ventricular arrhythmias.29
4.3. Exercise paradox or sports paradox
The exercise induced hemodynamic stress and catecholamine surge increase the incidence of acute ischemia, myocardial infarction and SCD during and up to 1 h post-exercise compared to the sedentary hours. The incidence of SCD with exercise is 8–16 times higher38, 39 and the incidence of MI with exercise is 6–10 times higher40, 41 compared to during resting hours. This increased relative risk of SCD and acute MI associated with every bout of vigorous exercise is reduced dramatically, in a dose-dependent fashion in the long term, by habitual and regular exercise. This is known as exercise or sports paradox.
The moderate to high intensity exercise, performed at regular intervals over a long period of time, has positive pleiotropic effects42 in reducing the overall risk of atherosclerosis and acute coronary syndrome. Compared to sedentary individuals, the relative risk of SCD during ‘exercise hours’ is reduced by 7–10 folds and the relative risk of acute MI during ‘exercise hours’ is reduced by 50 folds in individuals performing regular vigorous exercise.12 The intensity and frequency of regular exercise has inverse dose response relationship with relative risk of MI and SCD during exercise bout. Therefore, an active individual will have fifty-fold lower risk of MI during the exercise hour and will have up to two-fold lower risk of MI during the remaining sedentary hours of the day, showing the net benefit of exercise.43
5. Pre-participation screening
Sudden cardiac death in apparently fit appearing athletes mostly occurs in the absence of any warning symptoms or history of heart disease. Pre-participation screening to identify the presence of silent heart diseases can reduce the risk of sports related sudden death.
5.1. Young athletes
History, physical examination and ECG are the least expensive means of pre-participation screening and constitute the primary screening tool in most guidelines.7
5.1.1. History and examination
The current AHA recommendations for pre-participation screening of a young, competitive athlete includes essential elements in history and physical examination.7 This should be undertaken by the athlete’s personal/family physician upon entry into competitive sports at the school or college levels. The physical examination should include careful auscultation (in various positions and with maneuvers if needed) to detect any heart murmur especially a dynamic murmur due to left ventricular outflow tract obstruction. If there is any suggestion or suspicion of any heart disease based on this evaluation, further testing and evaluation by a cardiologist is recommended. The young athlete with family history of SCD or known cardiomyopathy should be evaluated with more elaborate history and clinical examination. This group of athletes should be referred to cardiologists and mandatorily have ECG and echocardiographic evaluation at baseline and at intervals. Further imaging and electrophysiological testing can be planned at the discretion of the cardiologist.
5.1.2. ECG screening
The addition of 12-lead ECG to history and physical examination can increase the sensitivity of pre-participation screening in detecting significant silent cardiac abnormalities.44, 45 ECG screening can identify cardiac diseases that manifest with specific findings such as ion channelopathies (for e.g., Long QT syndrome, Brugada syndrome), WPW syndrome, HCM and ARVC. However, non-specific ECG changes may be present in many individuals who are already performing athletic activities and may create confusion in the diagnosis.46, 47 Pre-participation screening of young athletes with ECG, in Veneto region of Italy, showed reduction of incidence of SCD from 3.6/100,000 person-years to 0.4/100,000 person-years (p < 0.001), representing 90% reduction in sports related mortality.4, 11 Most of the reduced incidence of SCD was achieved by detecting young athletes with cardiomyopathies like HCM and ARVC leading to their disqualification from competition. However, in a study from Israel, pre-participation screening of athletes with ECG and stress test was not associated with reduction in adverse cardiac events. The average incidence in the decade, before and after the mandated screening, was 2.54 and 2.66 events per 100,000 person-years, respectively.48 It is estimated that 30% of lethal CV causes like congenital coronary anomalies, 10–30% cases of cardiomyopathies (HCM/ARVC), aortic dilatation, IDCM and premature CAD cannot be identified by pre-participation screening with ECG.10, 17 There is a concern about sensitivity, specificity, practicality, and cost- effectiveness of ECG screening strategy for the conditions (HCM, ARVC, ion-channelopathy etc.) that have low prevalence in the young population.49 There is a divide in North America versus Europe guidelines regarding incorporating ECG as a mandatory test for pre-participation screening. Importantly, most of the rich sports associations have made ECG mandatory for screening prospective athletes. In Indian ECG is a relatively inexpensive test, and therefore suggested for all athletes/sports-person and marathoners. However, understanding the limitations of ECG is paramount to avoid unnecessarily barring athletes from pursuing their career of choice because of physiological changes in the ECG. At the same time, it should be borne in mind that a normal ECG does not rule out presence of heart diseases. Table 2 outlines the proposed pre-participation screening for young athletes in India.
Table 2.
Pre-participation screening in young, competitive athletes.
| History |
|
| Family History |
|
| Examination |
|
| ECG |
|
Abbreviations: ARVC, Arrhythmogenic Right Ventricular Cardiomyopathy; CPVT, Catecholaminergic Polymorphic Ventricular Tachycardia; SCD, Sudden Cardiac Death; WPW, Wolff-Parkinson-White.
5.2. Older athletes
A stepwise screening process as suggested by Chugh et al12 is likely to be useful in detection of occult heart disease in the older athlete. It essentially involves a detailed history including that of coronary risk factors, physical examination and an ECG in all subjects as the first step. Any suspicion of heart disease or a high risk of CAD will necessitate evaluation by a cardiologist as a part of second step to assess the need for further tests like stress test, echocardiogram, other imaging tests or cardiac catheterization (Table 3).
Table 3.
Steps in pre-participation screening for older athletes.
| Step 1: | History |
|
| Examination | Murmur, abnormal heart sound/s, evidence of cardiomegaly | |
| ECG | Ischemia, infarction, chamber enlargement or channelopathy | |
| If Step 1 negative → Fit for exercise training | ||
| If Step 1 positive → Evaluate Step 2 | ||
| Step 2: | Assessment by cardiologist for necessity of further tests
|
|
Abbreviations: CAD, Coronary Artery Disease; DM, Diabetes Mellitus; HT, Hypertension; MI, Myocardial Infarction; MRI, Magnetic Resonance Imaging; SCD, Sudden Cardiac Death.
5.2.1. Exercise ECG testing
The detection of silent coronary artery disease is one of the goals of pre-participation evaluation of athletes especially above 35 years of age. Exercise ECG testing is often performed as a part of screening in asymptomatic athletes and for evaluation of symptoms suggestive of CAD. The wide availability, low cost and known diagnostic value for detection of critical coronary stenosis in individuals at intermediate risk, make stress test useful in evaluating older athletes. However, the diagnostic accuracy of exercise testing depends on the pre-test probability of the disease and its prevalence in the community. Hence, its usefulness in asymptomatic individuals without coronary risk factors is limited. On the other hand, it can be useful for detection of CAD in those athletes who have coronary risk factors with an estimated 10-year-risk of CAD in the intermediate category.50 Although, an abnormal stress test indicates the presence of significant stenosis of one or more coronary arteries; a stress test cannot detect a non-significant stenosis due to a vulnerable plaque. Since SCD due to acute coronary syndrome can also occur because of rupture of a non-significant vulnerable plaque, the value of exercise ECG testing for predicting occurrence of sudden cardiovascular events during exercise is limited.
Many guidelines have incorporated the use of exercise ECG testing as a pre-participation screening in individuals at higher risk of CAD based on consensus, however scientific data is lacking.51
6. ECG interpretation in athletes
The role of ECG for screening in athletes gets further compounded by the prevalence of abnormal findings on the ECG that occur as a result of athletic training itself in the absence of any heart disease. These “abnormal” ECG manifestations occur either due to increased vagal tone or due to increase in muscle mass and cardiac size. Their occurrence is also influenced by age, sex, race & ethnicity and most importantly by the type of sport and duration of athletic training. Athletes involved in endurance sports like long-distance running are at maximum chance of training-related ECG manifestations.52
The ESC has provided recommendations for ECG interpretation in athletes and have grouped them into those resulting from physiological adaptation of cardiac autonomic nervous system and those that are likely due to underlying heart disease. The physiological adaptation related ECG abnormalities are seen in up to 80% of athletes whereas ECG changes suggesting heart disease are seen in less than 5% and these warrant further cardiac evaluation.47 A summit on “ECG interpretation in athletes” held in Seattle, Washington USA in 2012 involving leading cardiologists from various international societies laid down criteria that if present on ECG indicate possible underlying heart disease requiring further diagnostic evaluation.53
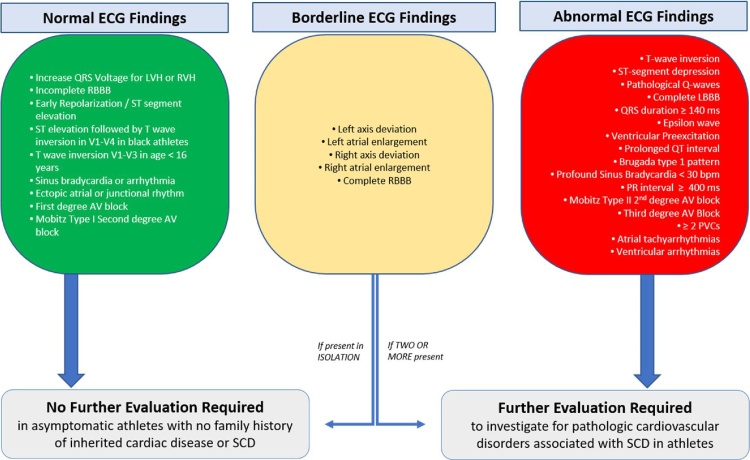
More recently, an international consensus for ECG interpretation in athletes was published that provides expert opinion-based recommendations linking specific ECG abnormalities and the secondary evaluation for conditions associated with SCD.54 The guidelines classified the ECG findings as normal, borderline and abnormal and suggested that further evaluation is required in the presence of abnormal findings or two or more borderline findings. In the absence of cardiac symptoms or family history, presence of normal findings or borderline changes in isolation do not warrant further evaluation. (Fig. 1)
Fig. 1.
Classification of ECG findings based on the International Consensus Standards for ECG interpretation in Athletes54.
7. Athletes heart and its differentiation from pathological states
The electrical, structural and functional cardiac adaptation observed in the athletes is termed as athlete’s heart. The clinician should differentiate these physiological adaptations from pathological changes using clinical, ECG, imaging data and objective functional capacity.
7.1. Athletes heart versus HCM
Athletes show 10–20% increase in left ventricular (LV) wall thickness (LVWT). LVWT of 13–16 mm falls into a ‘grey zone’ and more clinical and imaging data is required to differentiate athlete’s heart from HCM. Echocardiography showing a small LV size, enlarged LA, asymmetric or focal hypertrophy along with abnormal diastolic relaxation suggests HCM. Non-sustained VT on Holter, CMR for LGE and genetic testing further help to establish the diagnosis of HCM.
7.2. Athletes heart versus ARVC
The overall cardiac chamber enlargement in an athlete might be confused with RV dilatation seen in ARVC. Their differentiation is extremely important since exercise not only predisposes a patient with ARVC to SCD, but helps in the progression of the disease and unfavorably modifies the substrate. The RV enlargement compatible with ARVC diagnosis is observed in 22% of black athletes and 29% of white athletes.55, 56, 57 A positive family history along with ECG and echocardiographic findings may help to identify ARVC and typical findings on CMR imaging confirms the diagnosis.
7.3. Athletes heart versus IDCM
Athletes show 10–15% increase in both left and right ventricular cavity size. In Olympic athletes, 45% have LV cavity size more than upper limits of normal and 14% have LV cavity more than 60 mm33 Family history and additional ECG changes (LBBB, T wave inversion in infero-lateral leads) help to establish the diagnosis of IDCM. Diastolic dysfunction and failure of improvement in LV systolic function on exercise echocardiography suggests IDCM. Additionally, low peak VO2 on cardiopulmonary testing, non-sustained VT on Holter, LGE on CMR and positive genetic testing favor a diagnosis of IDCM.
8. Exercise training
Prior to beginning a program of vigorous exercise, usually defined as >6 METS (metabolic equivalents), it is recommended to undergo medical clearance by a physician, familiar with sports medicine. Evaluation should be directed to screen for the presence of cardiovascular, pulmonary and metabolic diseases and their risk factors. This is particularly important for those who do not regularly participate in exercise or sports activities.58
Training plans for full marathons should be at least 16–20 weeks long, after having a baseline ability to run at least 8 km, several times a week. Training plans usually include running distances of 5–10 km, 3–5 days of the week. One day a week, athletes should run for a longer distance (upward of 10 km), building the distances up progressively every week. It is important to increase the weekly mileage in a gradual manner, to lessen the chances of injury; with a rule of thumb being, an increase of not more than ten percent. Athletes should train with optimal individualized dose and intensity59 of exercise or activity under guided supervision. Individuals more than 35 year should undergo supervised or guided exercise training programs with gradually increasing intensity. Also, the program should religiously include ‘warm up’ and ‘cool down’ exercises before and after every bout of vigorous exercise respectively. Training heart rate, should generally be in the range of 60–90% of maximal heart rate (obtained on a symptom-limited graded exercise test, or age-predicted). Participants should acclimatize to the venue climate before the race and should not participate if suffering from fever or respiratory tract infection to prevent heat stroke. They should be made aware of common symptoms of cardiovascular insufficiency, such as chest discomfort and unusual shortness of breath with exertion. Since marathon running is relatively new in India, it is advisable for participants to train under the guidance of a qualified coach.
9. Medical facilities during sporting events
Planning the delivery of medical services at an event should include a risk assessment and buy-in from multiple agencies to ensure that first-aid and medical services are provided for, a thorough communications plan is in place, emergency access/exit routes are mapped out, and staff & volunteers are trained in escalation and evacuation procedures.60 There should be a unified command centre for co-ordinated monitoring and communication of the event. Security approvals should be taken from the concerned government agencies and also have them part of the planning process.
Medical facilities during extreme endurance sporting events are usually made available to take care of the common risks like dehydration, heat exhaustion & sporting injuries. However, cardiovascular events, including cardiac arrest, although uncommon, are of prime concern due to their life-threatening nature, facilities to diagnose and manage these at sporting event venue itself should always be available. These life-threatening events are more frequently observed to occur during the end of the race suggesting a sudden surge in acceleration to reach the finish line setting off a chain of bodily reactions leading to cardiac arrest.15, 61
While planning for medical provisions for an event, factors such as event type, weather (especially heat index), presence of alcohol and/or illicit drugs, number of participants, duration of the event, crowd demographics and venue characteristics should be taken into consideration. Appropriate judgement of the medical problem presentation rate and ambulance transfer time are very useful in understanding the medical needs of a sporting event.62
9.1. Staffing of the event
Number of staff at an event would be determined by the number of participants and the extent of medical coverage required. A marathon requires a mix of facilities with basic medical aid stations and ambulance evacuation. The event should have a medical director, who should preferably be a sports medicine physician, sports cardiologist, cardiologist or general physician with experience of planning mass sporting events. At every medical station, along the route there should be one physical therapist, one nurse and emergency medicine paramedic, with BCLS training and equipment to provide first aid. Majority of medical staff should be diverted toward the finish line as the race moves onwards. There should be at least one medical professional per 100 runners, in events with running distances longer than 10 km.
9.2. Physical infrastructure
Infrastructure to facilitate rapid diagnosis, treatment, and triage to appropriate centres, is essential for optimal care of participants in such mass gatherings. Medical services at mass sporting events can be delivered on foot, on bicycle, on motorbikes, on golf carts or other motorized vehicles, ambulance, first-aid stations and local hospitals. There should be a central medical station set up at the finish line which should be equipped like a mini ICU. There should be one aid station every 3 km of the route. Routes which are out-and-back (loop), make it easier to cover, since runners on both sides of the road can avail the facilities and only ‘half the number of physical structures’ and personnel are required. Volunteers should be stationed as ‘spotters’ who have been trained to identify athletes in distress and who are aware of the medical escalation protocol. Ambulances should be placed at regular intervals along the course of the race, and especially near the finish line and halfway between the first-aid stations.
9.3. Communication
The unified command centre is the main hub to monitor and coordinate all activities related to the event. There should be designated staff for coordinating medical emergencies. Deployed mobile units and staff at first-aid tents should be in touch with one another through mobile phones and walkie-talkies. The latter is preferred as the entire medical team can listen and respond at once. The route map with various facilities should be with every person involved in organizing the event. The chain of command, flowcharts for identification & referral and activating emergency medical response should not only be part of the training module but should also be documented and be part of the essential docket for the event.
9.4. Handling an emergency
First responders should be trained to identify symptoms, trigger the emergency medical system in place, perform Cardio-Pulmonary Resuscitation (CPR), and use AEDs.62, 63 First responders should be able to summon emergency medical units and/or ambulances based on symptoms. The medical aid units should be able to identify and treat hyperthermia. Hyponatremia is a very real and under-recognized life-threatening situation in races.64 Protocols for the assessment of dehydration, asthma, chest pain, syncope, or exercise-induced cramping should be part of the training module as well.65 Local hospitals should be part of the planning process in order to be prepared for life threatening situations at the day of the event, and should be alerted about receiving casualties during the event.
The survival in sports related SCD doubles with active CPR and rapid defibrillation. 14, 15, 66 The SCDs in US Marathons was 1 per 55,000 finishers before 1995, which reduced to 1 per 220,000 finishers during 1995 to 2004 as a result of emergency medical response (EMR) facilities.24 To be effective, the EMR team should conduct regular emergency drills and CPR practice and should have “hotline” to summon emergency medical transportation services. EMR should review the quality metrics like time to CPR/defibrillation and the outcome at least annually.
Communities including athletes, coaches, fitness trainers and spectators, should be trained in recognition of SCA and basic CPR for increasing the chances of immediate bystander CPR during sporting events. “Do Not Start marathon” temperature and air pollution thresholds should be decided to reduce heat-stroke risks during running events in hot and humid places.
10. Conclusion
Sports related SCD could be prevented and minimized by understanding the causes and mechanisms of such events. In the younger athlete, pre-participation screening with history (including family history), physical examination and ECG should help identify those at high risk for SCD and a detailed evaluation by a cardiologist can be considered for those suspected of heart disease or risk on initial screening. The older athlete is more likely to suffer SCD than the younger athlete; and since CAD is the most frequent cause for such events, their pre-participation screening should include evaluation for coronary risk factors and when necessary a stress test. Importantly, preventive strategies should be advised in older athletes with coronary risk factors. Supervised and graded exercise training is likely to prevent coronary events. It needs to be emphasized that regular exercise remarkably reduces the risk of MI and SCD.
Unfortunately, despite the best screening programs and exercise regimes, rare occurrence of SCD during athletic events is a reality. Appropriate planning and co-ordination of sporting events by the various agencies, especially the medical team and the paramedics, should help to identify and revive an athlete with sudden cardiac arrest.
Acknowledgements
The authors wish to acknowledge the Indian Heart Rhythm Society for facilitating this document and Dr. Sagri Negi of the Public Health Foundation of India for the valuable inputs in exercise training.
References
- 1.Arem H., Moore S.C., Patel A. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175:959–967. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shiroma E.J., Lee I.M. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122:743–752. doi: 10.1161/CIRCULATIONAHA.109.914721. [DOI] [PubMed] [Google Scholar]
- 3.Lawless C.E., Asplund C., Asif I.M. Protecting the heart of the American athlete: Proceedings of the American College of Cardiology Sports and Exercise Cardiology Think Tank October 18, 2012, Washington, DC. J Am Coll Cardiol. 2012;2014(64):2146–2171. doi: 10.1016/j.jacc.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 4.Corrado D., Schmied C., Basso C. Risk of sports: do we need a pre-participation screening for competitive and leisure athletes. Eur Heart J. 2011;32:934–944. doi: 10.1093/eurheartj/ehq482. [DOI] [PubMed] [Google Scholar]
- 5.Maron B.J., Chaitman B.R., Ackerman M.J. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109:2807–2816. doi: 10.1161/01.CIR.0000128363.85581.E1. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell J.H., Maron B.J., Epstein S.E. 16th Bethesda Conference: cardiovascular abnormalities in the athlete: recommendations regarding eligibility for competition. Introduction. J Am Coll Cardiol. 1985;6:1189–1190. doi: 10.1016/s0735-1097(85)80200-x. [DOI] [PubMed] [Google Scholar]
- 7.Maron B.J., Thompson P.D., Ackerman M.J. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007;115:1643–1655. doi: 10.1161/CIRCULATIONAHA.107.181423. [DOI] [PubMed] [Google Scholar]
- 8.Maron B.J., Araujo C.G., Thompson P.D. Recommendations for preparticipation screening and the assessment of cardiovascular disease in masters athletes: an advisory for healthcare professionals from the working groups of the World Heart Federation, the International Federation of Sports Medicine, and the American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2001;103:327–334. doi: 10.1161/01.cir.103.2.327. [DOI] [PubMed] [Google Scholar]
- 9.Maron B.J., Epstein S.E., Roberts W.C. Causes of sudden death in competitive athletes. J Am Coll Cardiol. 1986;7:204–214. doi: 10.1016/s0735-1097(86)80283-2. [DOI] [PubMed] [Google Scholar]
- 10.Corrado D., Basso C., Rizzoli G., Schiavon M., Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults. J Am Coll Cardiol. 2003;42:1959–1963. doi: 10.1016/j.jacc.2003.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Corrado D., Basso C., Pavei A., Michieli P., Schiavon M., Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296:1593–1601. doi: 10.1001/jama.296.13.1593. [DOI] [PubMed] [Google Scholar]
- 12.Chugh S.S., Weiss J.B. Sudden cardiac death in the older athlete. J Am Coll Cardiol. 2015;65:493–502. doi: 10.1016/j.jacc.2014.10.064. [DOI] [PubMed] [Google Scholar]
- 13.Marijon E., Tafflet M., Celermajer D.S. Sports-related sudden death in the general population. Circulation. 2011;124:672–681. doi: 10.1161/CIRCULATIONAHA.110.008979. [DOI] [PubMed] [Google Scholar]
- 14.Berdowski J., de Beus M.F., Blom M. Exercise-related out-of-hospital cardiac arrest in the general population: incidence and prognosis. Eur Heart J. 2013;34:3616–3623. doi: 10.1093/eurheartj/eht401. [DOI] [PubMed] [Google Scholar]
- 15.Gerardin B., Collet J.P., Mustafic H. Groupe de Reflexion sur la Cardiologie I. Registry on acute cardiovascular events during endurance running races: the prospective RACE Paris registry. Eur Heart J. 2016;37:2531–2541. doi: 10.1093/eurheartj/ehv675. [DOI] [PubMed] [Google Scholar]
- 16.Harmon K.G., Asif I.M., Klossner D., Drezner J.A. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123:1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622. [DOI] [PubMed] [Google Scholar]
- 17.Maron B.J., Doerer J.J., Haas T.S., Tierney D.M., Mueller F.O. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 18.Finocchiaro G., Papadakis M., Robertus J.L. Etiology of sudden death in sports: insights from a United Kingdom regional registry. J Am Coll Cardiol. 2016;67:2108–2115. doi: 10.1016/j.jacc.2016.02.062. [DOI] [PubMed] [Google Scholar]
- 19.Van Camp S.P., Bloor C.M., Mueller F.O., Cantu R.C., Olson H.G. Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27:641–647. [PubMed] [Google Scholar]
- 20.Harmon K.G., Asif I.M., Maleszewski J.J. Incidence, cause, and comparative frequency of sudden cardiac death in national collegiate athletic association athletes: a decade in review. Circulation. 2015;132:10–19. doi: 10.1161/CIRCULATIONAHA.115.015431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chandra N., Bastiaenen R., Papadakis M., Sharma S. Sudden cardiac death in young athletes: practical challenges and diagnostic dilemmas. J Am Coll Cardiol. 2013;61:1027–1040. doi: 10.1016/j.jacc.2012.08.1032. [DOI] [PubMed] [Google Scholar]
- 22.Baggish A.L., Wood M.J. Athlete's heart and cardiovascular care of the athlete: scientific and clinical update. Circulation. 2011;123:2723–2735. doi: 10.1161/CIRCULATIONAHA.110.981571. [DOI] [PubMed] [Google Scholar]
- 23.Maron B.J., Poliac L.C., Roberts W.O. Risk for sudden cardiac death associated with marathon running. J Am Coll Cardiol. 1996;28:428–431. doi: 10.1016/0735-1097(96)00137-4. [DOI] [PubMed] [Google Scholar]
- 24.Roberts W.O., Maron B.J. Evidence for decreasing occurrence of sudden cardiac death associated with the marathon. J Am Coll Cardiol. 2005;46:1373–1374. doi: 10.1016/j.jacc.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Tunstall Pedoe D.S. Marathon cardiac deaths: the London experience. Sports Med. 2007;37:448–450. doi: 10.2165/00007256-200737040-00046. [DOI] [PubMed] [Google Scholar]
- 26.Kim J.H., Malhotra R., Chiampas G. Race Associated Cardiac Arrest Event Registry (RACER) Study Group. Cardiac arrest during long-distance running races. N Engl J Med. 2012;366:130–140. doi: 10.1056/NEJMoa1106468. [DOI] [PubMed] [Google Scholar]
- 27.Schwabe K., Schwellnus M., Derman W., Swanevelder S., Jordaan E. Medical complications and deaths in 21 and 56 km road race runners: a 4-year prospective study in 65 865 runners–SAFER study I. Br J Sports Med. 2014;48:912–918. doi: 10.1136/bjsports-2014-093470. [DOI] [PubMed] [Google Scholar]
- 28.Yankelson L., Sadeh B., Gershovitz L. Life-threatening events during endurance sports: is heat stroke more prevalent than arrhythmic death. J Am Coll Cardiol. 2014;64:463–469. doi: 10.1016/j.jacc.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 29.Thompson P.D., Franklin B.A., Balady G.J. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115:2358–2368. doi: 10.1161/CIRCULATIONAHA.107.181485. [DOI] [PubMed] [Google Scholar]
- 30.Maron B.J., Shirani J., Poliac L.C., Mathenge R., Roberts W.C., Mueller F.O. Sudden death in young competitive athletes Clinical, demographic, and pathological profiles. JAMA. 1996;276:199–204. [PubMed] [Google Scholar]
- 31.Timmermans C., Smeets J.L., Rodriguez L.M., Vrouchos G., van den Dool A., Wellens H.J. Aborted sudden death in the Wolff-Parkinson-White syndrome. Am J Cardiol. 1995;76:492–494. doi: 10.1016/s0002-9149(99)80136-2. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz P.J., Priori S.G., Spazzolini C. Genotype-phenotype correlation in the long-QT syndrome: gene-specific triggers for life-threatening arrhythmias. Circulation. 2001;103:89–95. doi: 10.1161/01.cir.103.1.89. [DOI] [PubMed] [Google Scholar]
- 33.Sharma S., Merghani A., Mont L. Exercise and the heart: the good, the bad, and the ugly. Eur Heart J. 2015;36:1445–1453. doi: 10.1093/eurheartj/ehv090. [DOI] [PubMed] [Google Scholar]
- 34.Deligiannis A., Bjornstad H., Carre F. ESC study group of sports cardiology position paper on adverse cardiovascular effects of doping in athletes. Eur J Cardiovasc Prev Rehabil. 2006;13:687–694. doi: 10.1097/01.hjr.0000224482.95597.7a. [DOI] [PubMed] [Google Scholar]
- 35.Burke A.P., Farb A., Malcom G.T., Liang Y., Smialek J.E., Virmani R. Plaque rupture and sudden death related to exertion in men with coronary artery disease. JAMA. 1999;281:921–926. doi: 10.1001/jama.281.10.921. [DOI] [PubMed] [Google Scholar]
- 36.Brodeur V.B., Dennett S.R., Griffin L.S. Exertional hyperthermia, ice baths, and emergency care at the Falmouth Road Race. J Emerg Nurs. 1989;15:304–312. [PubMed] [Google Scholar]
- 37.England A.C., 3rd, Fraser D.W., Hightower A.W. Preventing severe heat injury in runners: suggestions from the 1979 Peachtree Road Race experience. Ann Intern Med. 1982;97:196–201. doi: 10.7326/0003-4819-97-2-196. [DOI] [PubMed] [Google Scholar]
- 38.Thompson P.D., Funk E.J., Carleton R.A., Sturner W.Q. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA. 1982;247:2535–2538. [PubMed] [Google Scholar]
- 39.Albert C.M., Mittleman M.A., Chae C.U., Lee I.M., Hennekens C.H., Manson J.E. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343:1355–1361. doi: 10.1056/NEJM200011093431902. [DOI] [PubMed] [Google Scholar]
- 40.Giri S., Thompson P.D., Kiernan F.J. Clinical and angiographic characteristics of exertion-related acute myocardial infarction. JAMA. 1999;282:1731–1736. doi: 10.1001/jama.282.18.1731. [DOI] [PubMed] [Google Scholar]
- 41.Mittleman M.A., Maclure M., Tofler G.H., Sherwood J.B., Goldberg R.J., Muller J.E. Triggering of acute myocardial infarction by heavy physical exertion: protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329:1677–1683. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 42.Burkule N. Marathon running for amateurs: benefits and risks. J Clin Prev Cardiol. 2016;5:113–124. [Google Scholar]
- 43.Franklin B.A. Preventing exercise-related cardiovascular events: is a medical examination more urgent for physical activity or inactivity. Circulation. 2014;129:1081–1084. doi: 10.1161/CIRCULATIONAHA.114.007641. [DOI] [PubMed] [Google Scholar]
- 44.Baggish A.L., Hutter A.M., Jr., Wang F. Cardiovascular screening in college athletes with and without electrocardiography: a cross-sectional study. Ann Intern Med. 2010;152:269–275. doi: 10.7326/0003-4819-152-5-201003020-00004. [DOI] [PubMed] [Google Scholar]
- 45.Malhotra R., West J.J., Dent J. Cost and yield of adding electrocardiography to history and physical in screening Division I intercollegiate athletes: a 5-year experience. Heart Rhythm. 2011;8:721–727. doi: 10.1016/j.hrthm.2010.12.024. [DOI] [PubMed] [Google Scholar]
- 46.Uberoi A., Stein R., Perez M.V. Interpretation of the electrocardiogram of young athletes. Circulation. 2011;124:746–757. doi: 10.1161/CIRCULATIONAHA.110.013078. [DOI] [PubMed] [Google Scholar]
- 47.Corrado D., Pelliccia A., Heidbuchel H. Section of sports cardiology EAoCP, rehabilitation. recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010;31:243–259. doi: 10.1093/eurheartj/ehp473. [DOI] [PubMed] [Google Scholar]
- 48.Steinvil A., Chundadze T., Zeltser D. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death proven fact or wishful thinking. J Am Coll Cardiol. 2011;57:1291–1296. doi: 10.1016/j.jacc.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 49.Link M.S., Estes N.A., 3rd Sudden cardiac death in the athlete: bridging the gaps between evidence, policy, and practice. Circulation. 2012;125:2511–2516. doi: 10.1161/CIRCULATIONAHA.111.023861. [DOI] [PubMed] [Google Scholar]
- 50.Balady G.J., Chaitman B., Driscoll D. Recommendations for cardiovascular screening, staffing, and emergency policies at health/fitness facilities. Circulation. 1998;97:2283–2293. doi: 10.1161/01.cir.97.22.2283. [DOI] [PubMed] [Google Scholar]
- 51.Borjesson M., Urhausen A., Kouidi E. Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18:446–458. doi: 10.1097/HJR.0b013e32833bo969. [DOI] [PubMed] [Google Scholar]
- 52.Sharma S., Whyte G., Elliott P. Electrocardiographic changes in 1000 highly trained junior elite athletes. Br J Sports Med. 1999;33:319–324. doi: 10.1136/bjsm.33.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Drezner J.A., Ackerman M.J., Anderson J. Electrocardiographic interpretation in athletes: the ‘Seattle criteria’. Br J Sports Med. 2013;47:122–124. doi: 10.1136/bjsports-2012-092067. [DOI] [PubMed] [Google Scholar]
- 54.Sharma S., Drezner J.A., Baggish A. International recommendations for electrocardiographic interpretation in athletes. J Am Coll Cardiol. 2017;69:1057–1075. doi: 10.1016/j.jacc.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 55.Zaidi A., Ghani S., Sharma R. Physiological right ventricular adaptation in elite athletes of African and Afro-Caribbean origin. Circulation. 2013;127:1783–1792. doi: 10.1161/CIRCULATIONAHA.112.000270. [DOI] [PubMed] [Google Scholar]
- 56.Oxborough D., Sharma S., Shave R. The right ventricle of the endurance athlete: the relationship between morphology and deformation. J Am Soc Echocardiogr. 2012;25:263–271. doi: 10.1016/j.echo.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 57.Marcus F.I., McKenna W.J., Sherrill D. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010;31:806–814. doi: 10.1093/eurheartj/ehq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Riebe D., Franklin B.A., Thompson P.D. Updating ACSM's recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473–2479. doi: 10.1249/MSS.0000000000000664. [DOI] [PubMed] [Google Scholar]
- 59.Predel H.G. Marathon run: cardiovascular adaptation and cardiovascular risk. Eur Heart J. 2014;35:3091–3098. doi: 10.1093/eurheartj/eht502. [DOI] [PubMed] [Google Scholar]
- 60.Endericks T., McCloskey B., Barbeschi M. WHO; 2015. Public Health for Mass Gatherrings: Key Considerations. [Google Scholar]
- 61.Baggish A.L. Athlete safety is a shared responsibility: insights from the RACE Paris Registry. Eur Heart J. 2016;37:2542–2543. doi: 10.1093/eurheartj/ehv740. [DOI] [PubMed] [Google Scholar]
- 62.Drezner J.A. Preparing for sudden cardiac arrest–the essential role of automated external defibrillators in athletic medicine: a critical review. Br J Sports Med. 2009;43:702–707. doi: 10.1136/bjsm.2008.054890. [DOI] [PubMed] [Google Scholar]
- 63.Toresdahl B., Courson R., Borjesson M., Sharma S., Drezner J. Emergency cardiac care in the athletic setting: from schools to the Olympics. Br J Sports Med. 2012;46(Suppl. 1):i85–9. doi: 10.1136/bjsports-2012-091447. [DOI] [PubMed] [Google Scholar]
- 64.Kratz A., Siegel A.J., Verbalis J.G. Sodium status of collapsed marathon runners. Arch Pathol Lab Med. 2005;129:227–230. doi: 10.5858/2005-129-227-SSOCMR. [DOI] [PubMed] [Google Scholar]
- 65.Glick J., Rixe J., Spurkeland N., Brady J., Silvis M., Olympia R.P. Medical and disaster preparedness of US marathons. Prehosp Disaster Med. 2015;30:344–350. doi: 10.1017/S1049023X15004859. [DOI] [PubMed] [Google Scholar]
- 66.Marijon E., Bougouin W., Celermajer D.S. Major regional disparities in outcomes after sudden cardiac arrest during sports. Eur Heart J. 2013;34:3632–3640. doi: 10.1093/eurheartj/eht282. [DOI] [PubMed] [Google Scholar]