Abstract
Our previous research found seven specific factors that cause system delays in ST-elevation Myocardial infarction management in developing countries. These delays, in conjunction with a lack of organized STEMI systems of care, result in inefficient processes to treat AMI in developing countries.
In our present opinion paper, we have specifically explored the three most pertinent causes that afflict the seven specific factors responsible for system delays.
In doing so, we incorporated a unique strategy of global STEMI expertise. With this methodology, the recommendations were provided by expert Indian cardiologist and final guidelines were drafted after comprehensive discussions by the entire group of submitting authors.
We expect these recommendations to be utilitarian in improving STEMI care in developing countries.
Keywords: STEMI, ACC/AHA guidelines, PPCI, Telemedicine
1. Introduction
The barriers for ST- elevation myocardial infarction (STEMI) systems in low and middle-income countries are markedly different than the traditional challenges to STEMI care in developed countries.1 Low and middle-income countries, such as India, are stymied by late presentation and lack of STEMI systems of care.1 Ambulance care is either insufficient, or absent altogether. In addition, there are manifest financial, infrastructures and logistic constraints.1 Comprehension of these significant challenges is paramount before designing STEMI programs in developing countries.
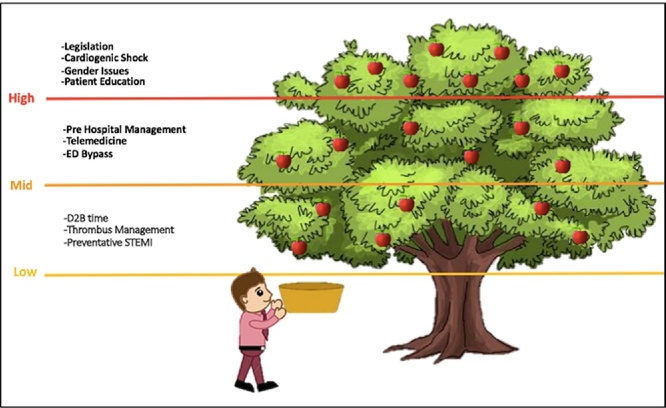
Fig. 1 summarizes the present and future challenges to STEMI interventions in developed countries, such as in the United States and in European nations.2, 3, 4, 5, 6, 7 To confront these challenges, STEMI networks have been fastidiously created in individual communities. Legislative mandates require a STEMI patient to be taken to a PCI-capable institution rather than to the nearest hospital. As a construct of STEMI networks, hospitals have been designated as either a PCI-capable or PCI non-capable facility.6, 7 Sophisticated ambulance networks exist and duration from chest pain to seeking care are declining (recently as low as 47 min in parts of New York State).6, 7 Strict STEMI (24 h/7 day a week) on-call schedules and availability are required at each PCI facility and single page activation is increasingly common. Prehospital management has been improving, including ED bypass. Teamwork is encouraged and stakeholder support is constantly expanded. ACC/AHA STEMI guidelines are rigorously implemented and Mission Lifeline and STENT for Life quality initiatives exist at most hospitals.6, 7 Feedback and quality assurance, critical to the success of STEMI initiatives, are routinely practiced. As a result of the above measures, the majority of STEMI patients have D2B times <90 min.7, 8 These process advances are matched by procedural improvements including appropriate thrombus management, use of drug-eluting stents and optimal pharmacological therapy.
Fig. 1.
Challenges in STEMI Care in Developed Countries.
Despite these remarkable achievements that have contributed to decreasing morbidity and mortality from STEMI, systems in USA and Europe cannot be considered as being perfect.3, 6 Challenges still exist – notable barriers in 2017 include gender disparities, delays in transfer from a non-PCI capable hospital, in-house STEMI, cardiac arrest and cardiogenic shock.5, 9, 10
While reviewing the progress of STEMI care in developed countries, two important lessons can be gained by healthcare providers in low and middle-income countries:
-
a
Progress in USA and Europe did not occur overnight. It was a result of steadfast determination, focused directives from Cardiology Societies and Working Groups which resulted in step-by-step and incremental system improvements.
-
b
A fastidious “can do” attitude that permeated the mindset of each stakeholder and that contributed to steady progress, a systematic deconstruct of chaos and systems improvement.
In “Reducing System Delays in Treatment of ST Elevation Myocardial Infarction and Confronting the Challenges of Late Presentation in Low and Middle Income Countries”, Mehta et al. described seven specific system constraints in STEMI in low and middle income countries.1, 11, 12 These hurdles were comprehensively reviewed in a “Making a Difference Session” at the Lumen Global XVI Annual Scientific Meeting conducted in Jaipur, Rajasthan, on February 25–26th 2017. The deliberations during this remarkable session have been incorporated into Table 1.
Table 1.
Barriers and Solutions for Low and Middle Income Countries.
| Solution 1 | Solution 2 | Solution 3 | |
|---|---|---|---|
| Patient Education | Multi-pronged approach to educate; both cardiologist and family physician should provide unified strategy with clear delineation of care responsibilities | Effective communication tools to educate about warning symptoms and early diagnosis and treatment | Foster trust with patient and family |
| Lack of Insurance | Government sponsored insurance bundling all the costs of STEMI including transportation | Adequate coverage, including pre-existing disease and cashless facility (for more affording) | Awareness and education about treatment costs and importance of insurance (for all) |
| Ambulance Deficits | Approach private and public ambulance systems individually | Have strategic plan at each PCI center regarding ambulance system; continue to improve their reliability and efficiency | Essential components in both public and private ambulance systems include Telemetry monitoring and paramedic training?Prehospital EKG |
| Hospital related Issues | Data: If you don't measure, you cannot improve. | Stakeholders: develop trusting relationships with stakeholders; share progress, advances and challenges. | Feedback and Education: Disseminate STEMI management and its vital contribution to the community and to society |
| Technology Gaps | Making available high definition but low cost ECG machines at first medical contact | Tele-transportation of data from point of first contact to higher center | Organization of systems for first medical contact down to Cath-lab systems that work |
| Physician Issues | Empower the General Physician | Overcome financial disincentives or create financial incentives | 24/7 Cath lab availability |
| Simply Chaos | ECG analysis program and continued training | Better penetration of benefit schemes | Bypassing hurdles at tertiary care & technology development |
2. Discussion
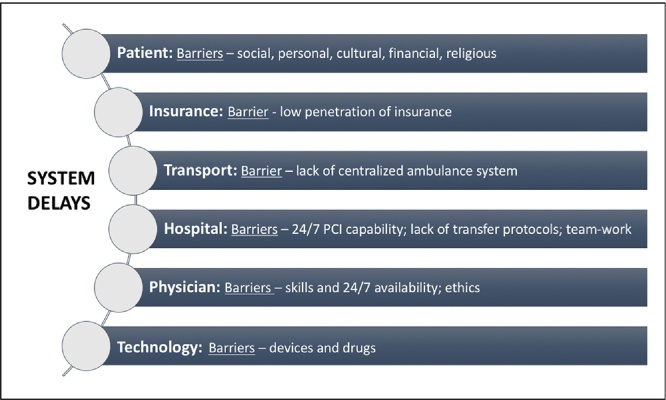
Based upon our previous research, we have focused on the following seven process constraints for STEMI interventions in low and middle-income countries, in particular, in India. These factors include – Patient Education, Lack of Insurance, Ambulance Deficits, Hospital-related Issues, Technology Gaps, Physician Issues and System Chaos, depicted in Fig. 2. Certainly there are additional system limitations, in particular, unique elements relevant in individual countries. However, we believe the factors above play a major role. It is for this precise reason that we have focused on these seven factors.1
Fig. 2.
System Delays in Developing Countries.
To investigate the impact of these factors and to find implementable solutions, a Lumen Foundation Task Force was created. This group comprised of an adept panel of global experts who collaborated on this research. These experienced cardiologists have vast experience in creating efficient models of population-based AMI care. This Task Force also included seven Indian expert cardiologists who were assigned the specific task of suggesting three possible solutions for each of these constraints.
Recommendations of the Task Force are summarized in Table 1 including the solutions that were endorsed to tackle the process limitations. This assignment occurred in the following four stages:
-
1.
Each of the constraint was discussed in detail and each solution was debated during the “Making a Difference” session of the Annual Lumen Global XVI scientific symposium.
-
2.
The global experts recommended notable modifications and improvements to the solution and a final strategy was articulated for each of the seven specific system challenges.
-
3.
Following this session, the Indian experts that postulated the solutions were invited to compile Table 1 and to submit a summary of their rationale.
-
4.
The final recommendations were reviewed by the expert panel that co-authored this publication and these suggestions comprise the frame of this manuscript.
-
5.
The seven process constraints are individually discussed below.
2.1. Patient education
As depicted in Fig. 1, patient education an important yet difficult, “high-hanging fruit” challenge in STEMI management. Its treatise requires cooperation between numerous stakeholders. Although much attention has been devoted to D2B times, the true ischemic time is critically important. This duration begins when the patient experiences chest pain. Unless there is a backward integration of the system, where the education is taken to the patient itself, sole focus on the final event, the D2B is inadequate. Low economic status and an overall lower level of education have been shown to contribute to delayed presentation.
In assembling three implementable solutions to facilitate patient education, the followings are submitted as the most noteworthy:
-
a)
Ignorance of Disease – What is a Heart Attack?
-
b)
When to suspect, how to diagnose? Where and what treatment to be given?
-
c)
Who to trust?
How does one implement these educational goals? Multimedia public education campaigns and community intervention programs aimed at reducing patient delay between symptom onset and hospital presentation and at increasing activation of EMS have had mixed results in various communities.13, 14, 15 In India, the strengths and limitations from the experience of these centers, can guide in planning programs to reach out to the community. A study in Sweden, demonstrated that a 1-year education campaign was associated with a significant reduction in median delay time from 180 to 138 min among patients with confirmed AMI.13 A public campaign in Geneva was associated with a similar reduction of median delay time for patients with confirmed AMI from 196 to 144 min.14 In the REACT Trial, a 4-year study in 20 regions, a community-based campaign to change patterns of response to symptoms of AMI did not significantly reduce patient delays compared to reference areas.15 The lack of effect represents a failure of the intervention to achieve this goal under the conditions of the REACT design. The educational messages may have been flawed, lacked sufficient intensity, duration, or both, or were targeted to the wrong groups. We need to make sure our instructions are written in simple words, comprehensible to all levels of education. By using short words, simple sentences, and clear illustrations, and verbally reinforcing written instructions, the message is well conveyed. Building the message in stories of movies or TV shows may have a greater impact than advertisement campaigns. In a publication from CMC Vellore, with the availability of 24 × 7 Cath Lab and experienced cardiologists, the rate of primary PCI increased from 10.7% to 60.6% over 2 years (2012–2014).13 There were several reasons for this, such as early diagnosis and referral from rural hospitals and general practitioners, available ambulance services, easy availability of government health insurance and growing awareness. In the general population, there is an increased acceptance of primary PCI but this message has to be articulated intelligently.
2.2. Lack of insurance
Issues related to insurance, and the lack of it, constitute one of the biggest causes of system delays and system inefficiencies in an inferior system of STEMI care. The high cost of managing STEMI and the emergent nature of the problem make it essential that the funds be available immediately at any hour of the day or night. This particular and critical problem places a burden on society. It makes the poor patient most vulnerable and leads to costly if not life threatening delays in treatment. As an example, with no ready funds for PCI, a choice is often made for fibrinolytic therapy. Worse, – again related to a lack of immediate and adequate funds, the choice of fibrinolytic agent may be the first generation fibrinolytic, Streptokinase, that is known to produce lower reperfusion rates. Such pragmatic aspects are not always readily acknowledged in literature because of their social and political impact, but they clearly contribute to worse outcomes and higher morbidity and mortality. Lack of insurance, therefore, adversely impacts the poorer patient and it requires local, state and federal response.16, 17 Government sponsored insurance is vital for this group, in a manner such that the major contribution comes from the state and a small, token amount from the patient. Of course, even a small contribution from the patient should be mandatory as it promotes awareness and co-participation in the well-being. The Kerala initiative in South India has shown that this system works very well, covers large populations who were not receiving any or minimal care and was able to reduce their mortality. It has been shown to be cost effective and substantially improved the care of a large population of less affording citizens.17
While contemplating pragmatic solutions for the vexing problem of lack of insurance, we feel that the insurance policies should be directed to bundle cost of travel, thrombolytic or interventional treatment and cost of drugs. This is a most particular issue in India. Where it is likely overall treatment will remain ineffective if these elements are not covered by insurance.
For the more affording patient, the insurance should have three factors. First, it must be adequate for all expenses of STEMI management taking into account the costs over time and the possibility of complications. Secondly, all preexisting diseases must be covered by the insurance. A currently preexisting diabetes or hypertension frequently excludes the patient and makes the insurance coverage worthless following a STEMI. Thirdly, opportunity for cashless payment should be available so that in an emergency, time is not wasted seeking permissions from insurance companies or for collecting money to pay up front.
Finally, education and spread of awareness of STEMI as an emergency life threating issue, the urgency of treatment, and the high costs involved are vital, so that every individual is fully and well covered when struck by STEMI.16, 18, 19
2.3. Ambulance deficits
Both a quantitative and qualitative lack of ambulance systems has hampered improvement in STEMI management in India. Even where ambulances exist, they are mired in two specific problems: 1) Lack of Equipment: in particular, an ability to perform ECG and telemetry is nonexistent; 2) Poor Paramedic Training.
In midst of woeful system deficits, cardiologists in India caring for STEMI patients have resorted to alternative solutions like simply asking a patient to reach the hospital by the fastest means possible (without the ambulance), or sending a motorcycle paramedic to evaluate a patient and to perform an ECG. The latter is a particularly pragmatic situation where resources are constrained and where traffic is an enormous challenge. A motorcycle paramedic can accurately diagnose STEMI before summoning an ambulance – this triage must not be taken lightly as most chest pain presentations are not due to STEMI and valuable resources can be spared in this manner. The issue of traffic compounds the ambulance deficit and it makes ambulance functionality a formidable challenge.1, 19 Finally, there a complete absence of coordinated ambulance systems where ambulances are navigated through a central command – this functionality must remain goals for population-based STEMI care in low and middle income countries.
The three most pragmatic solutions:
-
a)
A complete delineation of ambulance services in the public and private sector: Most hospitals own their own ambulances that will only cater to the patients that are being transported to its own facility. PCI centers must dramatically augment this capacity; they should have ECG and telemetry facilities and train its paramedics in STEMI care. In the public domain, services like 108 (emergency services in India) need similar goals. They have an unsurpassed ability to make a difference in STEMI outcomes and their funding needs to be augmented by local and state agencies.
-
b)
Whether an ambulance system exists or not, it is more important for every institution to have an unambiguous plan of action regarding transportation of the STEMI patient. There must be written directives how the hospital telephone operators respond to patient emergencies of chest pain that seek transport to the hospital. Even a more important situation relates to the transfer patient from a non-PCI capable to a PCI capable institution. In low and middle-income countries, with ambulance deficits and pharmaco-invasive management is required frequently making hospital transfer critically important.
-
c)
Paramedic training is an essential specialty in low and middle-income countries. Meticulous planning and organization are required to train paramedics.1 The authors make strong recommendations to seek assistance in paramedic training from expert institutions in U.S. and Europe where this specialty is greatly advanced.3, 7 This resource and educational networking can speed paramedic training.
2.4. Hospital related issues
Hospital related issues play a significant role in delaying or even denying appropriate STEMI care. The hospital is quite often the first medical contact (FMC) of a STEMI patient, as practically no pre hospital care exists in India. Even if a patient has arrived from elsewhere, the hospital will usually engage its own processes to make a diagnosis and follow a management plan, as previous investigations may not be reliable. This further underscores the need for building STEMI networks to enable a patient to enter a system of care right from the FMC.16, 17, 20, 21
Hospital processes involving the Emergency Department (ED), and the Cardiology services (Cath Lab) are germane to the present discussion, and significant delays occur in both areas. We have identified these two areas contributing to delays in India and we have extensively pondered these vital segments. In the ED, the process deficits include:
-
1.
Arrival to ECG and making the diagnosis of STEMI.
-
2.
Counseling of the patient and his family, consent and Cardiology services activation.
-
3.
Activation of Cath Lab, and transportation.
-
4.
Administrative formalities: admission of the patient and finance counseling.
Specifically, these delays can be greatly reduced by the following pragmatic strategies:
-
•
Not waiting for admission formalities to be completed before initiating PCI.
-
•
Not insisting on up front finance deposit before initiating management.
-
•
Empowering the ED to directly activate Cath lab rather than waiting for Cardiology consultation.
The second hospital challenge is the Cath lab and there are several unique problems that require deliberations. Although the procedure of primary PCI is quite standardized, meeting guideline-mandated timelines reliably is a constant problem. The Cath Lab activation needs to be standardized including off hour activation, holiday rosters and personnel in proximity of the hospital for STEMI call. Procedural details can also benefit from collegiate discussions to construct a standardized approach to issues such as radial or femoral access, routine use or not of thrombus-aspiration, antiplatelet and antithrombotic therapy and choice of coronary stents.
Management of a STEMI patient involves multiple agencies that may not always understand the urgency of care needed, and the system is not inherently built to respond quickly, leading to delays at every level.1, 14, 20
In offering the three pragmatic solutions, the writing group has these three principles that need to be applied to minimize hospital related issues are:
-
1.
If you don’t measure, you cannot improve: All ED processes, once measured and with metrics in place, can be streamlined with feedback and prioritization. Although Door to Balloon (D2B) times are well known, there is limited discussion on its’ various components and how processes may improve. Feedback may identify problem areas and offer solutions. The measurement of patient outcomes such as in-hospital and 30-day mortality, readmission, and recurrent MI or heart failure are excellent indicators of how effective the STEMI system is.
-
2.
Involvement of all hospital stakeholders is crucial as STEMI management is a collaborative effort and requires an understanding of the issues involved for best outcomes. Regular interaction between ED personnel, administrative representatives and cardiologists is desirable improve all aspects of the system.
-
3.
STEMI Management should be a showcase of the hospital and a measure of the robustness of its’ systems. STEMI management can be used as tool to illustrate hospital effectiveness as it involves a complex network of various agencies of the hospital working together under time pressure to ensure a good outcome. This can be leveraged and priority accorded to it to enable some departure from usual hospital protocols to improve efficiency. In the future, when ED bypass, pre hospital care become more commonplace, hospital with excellent STEMI system in place will have the flexibility needed to take the lead and add further improvements in STEMI care, thus enhancing both, its reputation as well as confidence in its systems of care.11, 19, 22 Regular CME updates, involving stakeholders in pre and post lecture opinion poll and in debates can be useful measures.
2.5. Technology gaps
The enduring task and comprehensive solution are to elevate the entire STEMI care system from first medical contact to the state of art Cath Lab facilities. ECG machines, at the point of first contact, need to be upgraded so that they produce reliable, reproducible and high quality tracings that can be accurately interpreted including a good analysis program – an algorithm that is the gold standard and a printout that is absolutely accurate. It should not only be cost effective but should also be able to function in power deficient areas. A mobile-based platform may be a good idea in the current era, as most Indians, irrespective of their social and economic class, possess this device.
Medical personnel who make the first contact with a STEMI patient are unlikely to be physicians.17, 19, 20 Thus tele-transportation of initial clinical data, ECG and vital signs, is an important capacity for an effective STEMI system, especially in the Indian context. Furthermore, this system may be an efficient way to transmit information from remote areas to more sophisticated centers where appropriate clinical and administrative decisions might be taken. Practical examples include when a decision is urgently required whether to administer a fibrinolytic or advise primary PCI and whether to refer to a secondary, PCI-capable center. This capability may even exclude the requirement of first contact physician, (the patient/attendant, using a home telemedicine device such as a smart phone and endowed with a suitable application may transmit their medical data to an advanced center, on which a decision can be taken, thus saving precious time.) This has been demonstrated in studies like the meta-analysis and Meta-regression analysis by ND Brunetti et al. they found that pre-hospital triage with telemedicine is associated with halved time to treatment in AMI.24
We recommend the following three solutions:
-
1.
An app based system to locate the nearest PCI capable hospital. This particular ability is available in India and numerous process-based applications that enable STEMI process can be assembled. These will also create useful templates for other low and middle low income countries.
-
2.
An efficient system where the first contact team can communicate seamlessly with PCI and non-PCI capable centers.
-
3.
Technology-systems improvement that provide directly activating Cath-lab and bypassing the ED. They can also provide systems of interaction between each and every component of EMS to the point of first medical contact and provide data feedback.
2.6. Physician-related issues
The delays in timely treatment of STEMI (including NSTEMI, as recent studies favor more aggressive approach) inherent in developing countries should alone be an incentive to improve and include D2B times that are recommended by ACC/AHA and Stent for Life guidelines. Sadly, these metrics are presently woefully deficient as is evident from data provided by CREATE investigators.16, 17 Provider-related issues, as they pertain to the physician, are important for improving efficiency and to reduce system delays.
The following three factors appear most pertinent:
-
1.
Empowering of the General Physician (GP) is critical. Frequently the GP provides initial contact with the family and the patient. However, this is both an opportunity and a massive challenge, as it translates to educating almost a million GP in India. It is a colossal undertaking whose solution must be multi-pronged. The GP societies need to include a STEMI educational agenda on their scientific deliberations. It may even require a re-construct of the basic training. Continued Medical Education (CME) mandates on this important topic may also be considered. The most vital issue has to be a partnership between the cardiologist and the GP who must work as a team rather than isolated specialists.
-
2.
Financial Alignment – this relates to the often-complex issues of competing providers who must now be forced to worked together and align their financial incentives. A relevant example in India is A physician who administers thrombolytic therapy has a financial disincentive to transfer for PCI. This is a major and frequent challenge that requires careful comprehension and thoughtful analysis. Although STEMI care is not unique in requiring multiple physicians to provide different levels of care, the urgency involved in the case with STEMI necessitates advanced planning and resolution of these matters. Ingenious, profit sharing arrangements appear prudent but they will require honest and open discussion.1, 19
-
3.
A genuine 24/7 discipline – India is plagued with a practice of “thrombolysis during the night and PCI during the day” and this custom requires a forceful termination. It is a most difficult task that has financial, moral, ethical and structural implications but whose sensible resolution must not be delayed any longer.
3. Simply chaos
It is often mentioned, and not incorrectly, that Indians thrive in chaos! Yet, chaos in the middle of a STEMI intervention or preceding events is detrimental and it leads to worse outcomes. To deconstruct STEMI chaos is a rewarding exercise and may contribute to improving functionality for all acute emergencies and in other areas of the hospital. Teamwork, leadership development and communication comprise an important triad and all should be encouraged.2, 3, 4, 5, 6, 7, 8 As it relates to India, the three most pertinent solutions include:
-
a)
ECG issues – since an ECG is the sole requirement of diagnosing STEMI, its immediate and reliable acquisition constitute the first step in eliminating chaos. It must be obtained accurately and efficiently and its interpretation should be equally seamless. Telemedicine, as reported in the Latin America Telemedicine Infarct Network (LATIN), can have pragmatic applications in low and middle-income countries.
-
b)
Payment Schemes – this issue has been individually dealt with, yet, it is important to repeat and emphasize this aspect, as it creates havoc in India for STEMI care. The issue requires open communication and a comprehensive solution. Every citizen of India must know about the STEMI treatment options including the cost. Since most patients pay out of pocket, this unambiguous communication, ahead of the emergent and often catastrophic event, is possibly the most important correctable action to eliminate chaos.
-
c)
Bypassing traditional hurdles – of technology and access are also amenable to correction from collaborative and open communication. Press and media can play an important role in this matter as well as in the issue of payment schemes.
4. Conclusions
Delayed presentation and lack of STEMI systems of care are hampering outcomes in AMI in low and middle-income countries.1, 23 We have identified seven specific process constraints present, in particular, in India. In advocating implementable solutions, we now present a collaborative and global plan of pragmatic resolutions that can provide a template for circumventing some of these obstacles and for improving outcomes in STEMI patients.
References
- 1.Mehta S., Granger C., Henry T. Reducing system delays in treatment of ST elevation myocardial infarction and confronting the challenges of late presentation in low and middle – income countries. IHJ. 2017;(January) doi: 10.1016/j.ihj.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antman E.M., Anbe D.T., Armstrong P.W. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44(3):E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Kaifoszova Z., Kala P., Wijns W. The stent for life initiative: quo vadis? EuroIntervention. 2016;12(May (1)):14–17. doi: 10.4244/EIJV12I1A3. [DOI] [PubMed] [Google Scholar]
- 4.Keeley E.V., Boura J.A., Grines C.L. Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction: quantitative review of randomized trials. Lancet. 2006;367(9510):579–588. doi: 10.1016/S0140-6736(06)68148-8. [DOI] [PubMed] [Google Scholar]
- 5.Jollis J.G., Granger C.B., Henry T.D. Systems of care for ST-segment-elevation myocardial infarction: a report from the American Heart Association’s Mission: lifeline. Circ Cardiovasc Qual Outcomes. 2012;5(4):423–428. doi: 10.1161/CIRCOUTCOMES.111.964668. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs A.K., Antman E.M., Faxon D.P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116(2):217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 7.Krumholz H.M., Bradley E.H., Nallamothu B.K. A campaign to improve the timeliness of primary percutaneous coronary intervention: door-to-balloon: an alliance for quality. JACC Cardiovasc Interv. 2008;1:97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg R.J., Spencer F.A., Fox K.A.A. Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 9.Henry T.D., Atkins J.M., Cunningham M.S. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers: is it time for a national policy for the treatment of ST-segment elevation myocardial infarction? J Am Coll Cardiol. 2006;47:1339–1345. doi: 10.1016/j.jacc.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 10.Henry T.D. From concept to reality: a decade of progress in regional ST- elevation myocardial infarction systems. Circulation. 2012;126:166–168. doi: 10.1161/CIRCULATIONAHA.112.114140. [DOI] [PubMed] [Google Scholar]
- 11.Mehta S., Reynbakh O., Kostela J.C. Building population-based AMI management systems using telemedicine as a foundation pillar. Eur Heart J. 2014;35:569–581. [Google Scholar]
- 12.Mehta S., Botelho R., Rodriguez D. A tale of two cities: STEMI interventions in developed and developing countries and the potential of telemedicine to reduce disparities in care. J Interv Cardiol. 2014;27(2):155–166. doi: 10.1111/joic.12117. [DOI] [PubMed] [Google Scholar]
- 13.Herlitz J., Blohm M., Hartford M. Follow-up of a 1-year media campaign on delay times and ambulance use in suspected acute myocardial infarction. Eur Heart J. 1992;13:171–177. doi: 10.1093/oxfordjournals.eurheartj.a060142. [DOI] [PubMed] [Google Scholar]
- 14.Gaspoz J.M., Unger P.F., Urban P. Impact of a public campaign on pre-hospital delay in patients reporting chest pain. Heart. 1996;76:150–155. doi: 10.1136/hrt.76.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luepker R.V., Raczynski J.M., Osganian S. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease. The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 16.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(April (9622)):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 17.Mohanan P.P., Mathews S., Harikrishnana Presentation, management, and outcomes of 25748 acute coronary syndrome admissions in Kerala, India: results from Kerala ACS registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander T., Mullasari A.S., Kaifoszova Z. Framework for a national STEMI program: consensus document developed by STEMI INDIA, cardiological society of india and association physicians of India. Indian Heart J. 2015;67(5):497–502. doi: 10.1016/j.ihj.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sundip M. Indian Heart J. 2016;60(2) [Google Scholar]
- 20.Negi C.P., Merwaha P., Panday D. Multicenter HP ACS registry. IHJ. 2016;68(2):118–127. doi: 10.1016/j.ihj.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iqbal F., Barkataki J.C. Spectrum of acute coronary syndrome in North Eastern India–a study from a major center. IHJ. 2016;68(2):128–131. doi: 10.1016/j.ihj.2015.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paul V.G., Hooda A., Pati P.K., Varghese L., Lahiri A. Effect of a Government Scheme on Reperfusion Trends in a tertiary care center in South India. Indian Heart J. 2014;66:503–505. doi: 10.1016/j.ihj.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beygui F., Castren M., Brunetti N.D. Pre-hospital management of patients with chest pain and/or dyspnoea of cardiac origin. A position paper of the Acute Cardiovascular Care Association (ACCA) of the ESC. Eur Heart J Acute Cardiovasc Care. 2015:1–23. doi: 10.1177/2048872615604119. [DOI] [PubMed] [Google Scholar]
- 24.Brunetti N.D., De Gennaro L., Correale M. Pre-hospital electrocardiogram triage with telemedicine near halves time to treatment in STEMI: a meta-analysis and meta-regression analysis of non-randomized studies. Int J Cardiol. 2017;232:5–11. doi: 10.1016/j.ijcard.2017.01.055. [DOI] [PubMed] [Google Scholar]