Abstract
An 83-year-old Japanese man was admitted with dysarthria and right hemiparesis. He had had a large intracranial aneurysm on the left internal carotid artery 5 years before admission and had been followed up under conservative treatment. On admission, diffusion-weighted imaging revealed a hyperintense signal on the left anterior choroidal artery territory. Time-of-flight magnetic resonance angiography demonstrated poor visibility of the middle and anterior cerebral arteries and the inferior giant aneurysm, suggesting distal emboli from aneurysm thrombosis or a reduction of blood outflow due to aneurysm thrombosis. Arterial spin labeling (ASL) signal increased in the giant aneurysm, suggesting blood stagnation within the aneurysmal sac, and decreased in the left hemisphere. We diagnosed cerebral infarction due to aneurysm thrombosis, and started antithrombotic therapy. On day 2, he suddenly died of subarachnoid hemorrhage due to rupturing of the giant aneurysm. When thrombosis occurs in a giant aneurysm, increasing ASL signal within the aneurysm and decreasing ASL signal with poor visibility on magnetic resonance angiography in the same arterial territory may indicate the danger of impending rupture of the giant aneurysm.
Keywords: Giant aneurysm, Cerebral infarction, Subarachnoid hemorrhage, Arterial spin labeling, Impending rupture
Introduction
Giant intracranial aneurysms, defined as having a diameter > 25 mm, represent approximately 5% of intracranial aneurysms [1]. The natural history of giant cerebral aneurysms is classified into thrombosis, growth, and rupture [1]. Although aneurysm thrombosis is a common phenomenon in giant intracranial aneurysms [2], cerebral infarction due to aneurysm thrombosis in giant intracranial aneurysms is a rare manifestation [1]. Patients with ischemic stroke distal to an unruptured intracranial aneurysm experienced subarachnoid hemorrhage (SAH) soon after the ischemic stroke [3]. Therefore, it is important to detect the signs of impending rupture of SAH in giant intracranial aneurysms.
Arterial spin labeling (ASL) is a noninvasive magnetic resonance imaging (MRI) technique. ASL can rapidly assess cerebral blood flow using magnetically labeled water in blood as an endogenous tracer. ASL is useful for the evaluation of penumbra zones, localization of the arterial thrombus, post-therapeutic hyperperfusion, and the diagnosis of stroke mimics [4]. However, whether ASL is a useful technique for evaluating the impending rupture of giant intracranial aneurysms is unknown.
We herein describe ASL findings in a patient with a giant intracranial aneurysm leading to SAH following cerebral infarction.
Case Report
An 83-year-old Japanese man was admitted with dysarthria and right hemiparesis. At onset, he experienced an aphasic episode that improved in 2 h. Five years previously, he had had a large intracranial aneurysm on the left internal carotid artery (ICA) (Fig. 1a). A neurosurgeon decided to treat this conservatively because surgical and/or endovascular intervention is a high risk. His medical history included hypertension, Alzheimer's disease, and adverse cutaneous reactions for contrast media.
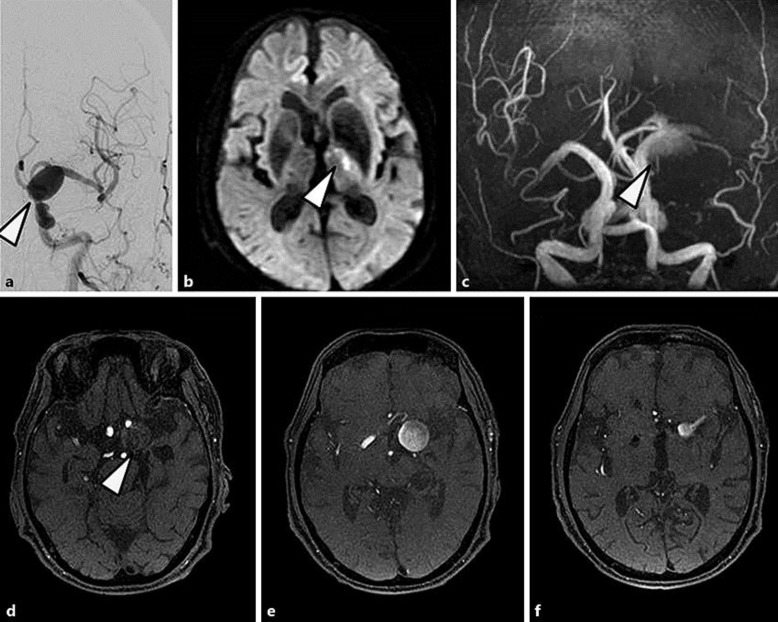
Fig. 1.
Digital subtraction angiography (a) obtained 5 years before admission. Magnetic resonance imaging (b–f) obtained on admission. a Left carotid angiography displays a large intracranial aneurysm (arrowhead; maximum diameter 21 mm) on the left internal carotid artery. b Diffusion-weighted imaging reveals a hyperintense signal on the left anterior choroidal artery territory (arrowhead). c–e Time-of-flight magnetic resonance angiography demonstrated poor visibility of the middle and anterior cerebral arteries and the inferior part of the giant aneurysm (maximum diameter 28 mm), suggesting aneurysm thrombosis (arrowheads).
On admission (4 h after the onset), his vital signs were: blood pressure, 135/82 mm Hg; heart rate, 70 beats/min; body temperature, 36.6°C; pulse oximetry reading (SpO2), 97% on room air; respiratory rate, 20 breaths/min. His Glasgow Coma Scale score was 14 (E4V4M6). A neurological examination revealed right hemiparesis and dysarthria. His National Institutes of Health Stroke Scale score was 5 points, laboratory evaluations were unremarkable, and his electrocardiogram showed sinus rhythm. Diffusion-weighted imaging (DWI) revealed a hyperintense signal on the left anterior choroidal artery territory (Fig. 1b). Time-of-flight magnetic resonance angiography (MRA) demonstrated poor visibility of the middle and anterior cerebral arteries and the inferior part of the giant aneurysm, suggesting aneurysm thrombosis (Fig. 1c–e). ASL signal increased in the giant aneurysm and decreased in the left hemisphere (Fig. 2a, b).
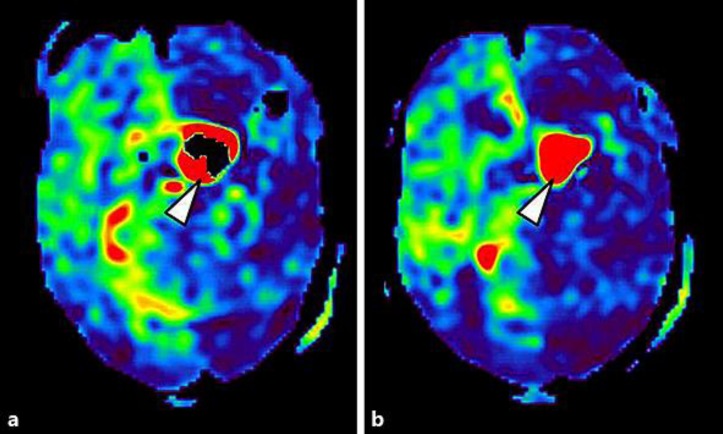
Fig. 2.
Arterial spin labeling obtained on admission. Arterial spin labeling signals increased in the giant aneurysm (arrowheads) and decreased in the left hemisphere.
Brain MRI was obtained using a 3.0-T MR scanner (Discovery MR750w; GE Healthcare) at admission. ASL (pulsed continuous ASL) was prepared using a three-dimensional spiral fast spin-echo sequence. The following ASL protocol was used: repeat time, 4,800 ms; echo time, 10.7 ms; slice thickness, 4.0 mm; number of excitations, 3; number of slices, 36; arms, 6; points, 512; field of view, 24 × 24 cm2; effective resolution, 4.44 mm; post-labeling delay (PLD), 2,025 ms; acquisition time, 3 min 34 s.
We diagnosed cerebral infarction due to aneurysm thrombosis, and started argatroban and edaravone. On day 2 after admission, he suddenly developed respiratory arrest and consciousness disturbance (3/15 score on Glasgow Coma Scale) and died of SAH due to the ruptured giant aneurysm.
Discussion
This case suggests that when thrombosis occurs in a giant aneurysm, increasing ASL signal within the aneurysm and decreasing ASL signal with poor visibility of MRA in the same arterial territory may indicate the danger of impending rupture of the giant aneurysm. To the best of our knowledge, this case is the first ASL finding of giant intracranial aneurysm resulting in SAH.
The mechanism of cerebral infarction due to unruptured aneurysms may be as follows: distal emboli, extension of thrombosis, and compression [1]. In this case, thrombosis was formed in the inferior part of the aneurysm, resulting in an infarction in the anterior choroidal artery territory owing to extension of the thrombosis. Although DWI did not demonstrate the shower embolism, poor visibility and decreasing ASL signal in the middle and anterior cerebral arteries could suggest distal emboli from aneurysm thrombosis or reduction of blood outflow due to aneurysm thrombosis, as indicated by the patient's aphasic episode at the onset.
The ASL PLD should be optimal because incorrect PLD settings can misrepresent cerebral blood flow [4]. In adults aged > 70 years old or patients with a suspected neurological condition, it is recommended that PLD be set to 2,000 ms [5]. Another solution for misdiagnosis by ASL is that other sequences, such as DWI or MRA, may be useful in confirming the correct diagnosis [4]. Because this patient's age was 83 years, and his neurological signs suggested the possibility of stroke, ASL was performed with a PLD of 2,025 ms, according to the above recommendation [5]. As a result, increasing ASL signal and decreasing ASL signal was detected in the giant intracranial aneurysm on the left ICA and left hemisphere perfused by the left ICA, respectively. MRA also showed the poor visibility of the middle and anterior cerebral arteries in the same arterial territory. ASL shows a bright vessel appearance by the accumulation of protons in labelled arterial blood upstream from the arterial occlusion [4]. The bright vessel sign can also reveal certain distal arterial occlusions not initially detected on the MRA [4]. In this case, ASL and MRA showed the bright vessel sign in the giant intracranial aneurysm, reflecting blood stagnation within the aneurysmal sac. We believe that these changes affected the blood pressure load on the aneurysm and caused SAH.
Conclusion
When thrombosis occurs in a giant aneurysm, the combination of ASL and MRA may be useful for detecting the impending rupture of a giant aneurysm.
Statement of Ethics
The man's family provided informed written consent for the publication of this case.
Disclosure Statement
The authors have no conflicts of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
We thank Wendy Brooks, PhD, from Edanz Group (www.edanzediting.com/ac) for English language editing of a draft of the manuscript.
References
- 1.Lonjon M, Pennes F, Sedat J, Bataille B. Epidemiology, genetic, natural history and clinical presentation of giant cerebral aneurysms. Neurochirurgie. 2015;61:361–365. doi: 10.1016/j.neuchi.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Rosta L, Battaglia R, Pasqualin A, Beltramello A. Italian cooperative study on giant intracranial aneurysms: 2. Radiological data. Acta Neurochir Suppl (Wien) 1988;42:53–59. doi: 10.1007/978-3-7091-8975-7_11. [DOI] [PubMed] [Google Scholar]
- 3.Guillon B, Daumas-Duport B, Delaroche O, Warin-Fresse K, Sevin M, Herisson F, Auffray-Calvier E, Desal H. Cerebral ischemia complicating intracranial aneurysm: a warning sign of imminent rupture? AJNR Am J Neuroradiol. 2011;32:1862–1865. doi: 10.3174/ajnr.A2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verclytte S, Fisch O, Colas L, Vanaerde O, Toledano M, Budzik JF. ASL and susceptibility-weighted imaging contribution to the management of acute ischaemic stroke. Insights Imaging. 2017;8:91–100. doi: 10.1007/s13244-016-0529-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alsop DC, Detre JA, Golay X, Gunther M, Hendrikse J, Hernandez-Garcia L, Lu H, MacIntosh BJ, Parkes LM, Smits M, van Osch MJ, Wang DJ, Wong EC, Zaharchuk G. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73:102–116. doi: 10.1002/mrm.25197. [DOI] [PMC free article] [PubMed] [Google Scholar]