Abstract
Purpose:
One of the crucial requirements for the success of implants is to achieve good stability. Two well-accepted quantitative methods to assess implant stability, the insertion torque value (ITV), and resonance frequency analysis (RFA) can be a valuable adjunct to radiological and clinical examination. This study was conducted to assess the relationship between ITVs and implant stability quotient (ISQ) and its influence on timing of functional implant loading, as well as to determine the effect of some of the factors on the stability of implants.
Materials and Methods:
Forty implants were inserted in 37 patients in the posterior mandibular region according to conventional protocol and allowed to heal by placing a healing abutment at the time of placement. For each implant, ITV was measured at the time of the implant placement by manual torque wrench (Nobel Biocare), and the ISQ value was measured by using resonance frequency analyzer (Osstell-ISQ; Integration Diagnostics) at the baseline levels, 3rd week, 7th week, 11th week, and 15th week interval.
Results:
The correlation between ITV and ISQ was found to be moderately positive and significant (r = 0.399) (P = 0.000). The correlation of ITV value at baseline and ISQ values recorded at the subsequent weeks was also found to be statistically significant at week 3 (r = 0.376) (P = 0.000) and week 7 (r = 0.327) (P = 0.000).
Conclusion:
It can be concluded from this study that there is a positive and statistically significant correlation between the ITV and ISQ values.
Keywords: Implant stability quotient, insertion torque value, Osstell-implant stability quotient device, primary stability, resonance frequency analysis, secondary stability, time of loading implants
INTRODUCTION
In the recent years, implant dentistry has evolved from the conventional healing protocol of 3–6 months to the most recent trends of immediate and early loading of implants. The most crucial requirement for the immediate loading protocol is primary stability which is the mechanical interlocking of the implant threads with the bone.[1] Primary stability measures the threshold of the bone-implant interface to withstand the micromovements at implant placement, thereby leading to undisturbed healing leading for the achievement of secondary stability, through bone regeneration and remodeling resulting in osseointegration.[2] This is largely influenced by the factors related to the design, material and surface treatment of the implant, the placement protocol, and the quality and quantity of the bone.[3]
There are various clinical methods available today to measure implant stability such as the histological analysis, radiographs, cutting torque resistance, reverse torque analysis, model analysis, percussion testing, insertion torque, removal torque, percussion test, resonance frequency analysis (RFA).[4,5] Although literature does not support the use of any single method alone to give accurate measurement of the stability, two well-accepted quantitative methods to assess primary implant stability, the insertion torque value (ITV), and RFA can be a valuable adjunct to radiological and clinical examination.[6]
ITV as developed by Johansson and Strid and improved by Frieberg gives an assessment of primary implant stability.[7,8] It is the maximum insertion torque that is required for the placement of implant in the prepared osteotomy site. Testori et al. suggested that good primary stability can be achieved by inserting an implant, with the optimum minimal IT value of 30 Ncm.[9] ITV is also suggestive of the bone density and quality. A higher value of the ITV relates to a denser bone.
Meredith et al. in 1996 developed a noninvasive, relatively easy-to-use clinical method to measure implant stability as RFA, which can be used for multiple number of times both intraoperatively and during the follow-up time.[10] It uses a probe that emits magnetic pulses to a small magnet at the top of a peg which is attached to the implant. The peg starts to vibrate, the probe listens to the tone, and translates it to an ISQ value. It gives it values as 1–100. Literature supports a range of values between 57 and 82 indicating better implant anchorage.[11]
Cehreli et al. in his meta-analysis on methods to assess implant stability reported 47 articles, out of which 2 clinical studies provided the P value, for comparison of correlation of ITV and ISQ, proving it to be statistically significant.[6] Whereas the P value provided by both cadaveric and animal studies proved the correlation between ITV and ISQ as statistically insignificant. To further contribute in this field, the aim of this study was to evaluate the values obtained by both the methods and to investigate the relation between the ITV and resonance frequency values, immediately after implant placement and at different time intervals.
MATERIALS AND METHODS
A total of 47 implants (Nobel Replace Tapered Groovy and Replace Select Tapered partially machined collar (PMC); Nobel Biocare AB) were placed in 37 individuals who visited the Department of Implantology for replacement of a single missing tooth in the mandibular posterior region (Kennedy Classification 3). The implants were inserted according to conventional protocol, ITV, and ISQ were measured, and a healing abutment was placed and sutured. For each implant, the implant design, the length, and the diameter were recorded. Out of the 47 implants placed, two implants were lost during the 3rd week due to lack of integration, one patient dropped out during the 7th week, and four patients were lost for follow-up at the 15th week evaluation. Therefore, a total of 40 implants completed the follow-up followed by a permanent crown cementation at the end of the follow-up period.
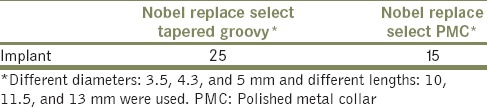
Among the 40 implants, two different implant designs were used, 25 Nobel Replace Select Tapered Groovy Implants, and 15 Nobel Replace Select PMC Implants were placed as shown in Table 1. These implants varied in dimensions as well. Six implants with a wide platform (5 mm), 30 implants with a regular platform (4.3 mm), and 4 implants with a narrow implant (3.5 mm) were placed. Implants placed also varied in lengths; 12 implants of length 10 mm, 22 implants of length 11.5 mm, and 6 implants of length 13 mm were placed. The implant site only with adequate edentulous space and the adequate bone width (a minimum of 1.5 mm of bone was present around the implant placed) were selected based on the following inclusion criteria.
Table 1.
Number of implants used depending on the implant design
Inclusion criteria
Patients presenting with single posterior edentulous spaces in mandibular arch
Patients within the age group of 20–50 years of either sex
Individuals with good systemic health with no known contraindication for surgery
Presence of adequate bone volume to accommodate an implant of appropriate size with 1.5 mm of bone all around the implant
Patient with good oral hygiene.
Exclusion criteria
If there was any anterior edentulous spaces present
If the edentulous sites had any signs of acute infection
If the patient had a medical history that would compromise the treatment outcome
Patients with parafunctional habits and temporal mandibular joint disorders
Pregnant or lactating women
Presence of insufficient bone quantity as determined by clinical bone mapping and preoperative radiographs
Chronic smokers and alcoholics
Patients allergic to any medicines which are likely to be used during the treatment period.
The implant was placed at the prepared site as per the standard protocol. The insertion torque was recorded manually during implant placement with the help of the manual torque driver (Nobel Biocare AB). The maximum ITV is the peak insertion torque reached in the final stage of implant placement into the prepared site. For statistical analysis, the maximum values for each procedure were recorded. At this point, the ISQ value was also measured by resonance frequency analyzer (Osstell-ISQ; Integration Diagnostics AB). All measurements were performed by a single operator. A Smartpeg (Integration Diagnostic AB) was placed onto the implant and was hand-tightened into the implant body by the approximate pressure of 5–10 Ncm. An analyzer probe was held close to the Smartpeg, in both parallel and perpendicular directions to the alveolar ridge of the jaw, and the implant stability quotient (ISQ) value was obtained from the Osstell ISQ. Measurements were made and compared to the ITVs. After the measurements, the healing abutment was placed and sutured. The ISQ value for each of the implant was again measured at 3rd, 7th, 11th, and 15th week follow-up appointment using the resonance frequency analyzer as shown in flowchart 1.
Flowchart 1.

Flowchart on methodology
Descriptive and comparative analysis was performed using the SPSS software version 17.0 (SPSS, Inc., Chicago, IL, USA). Collected data were analyzed by one way ANOVA to compare across the group and for repeated measures across the time period or duration. Post hoc analysis was performed by Bonferroni test. Pearson correlation coefficient was used to investigate the relationship between ITV and ISQ.
RESULTS
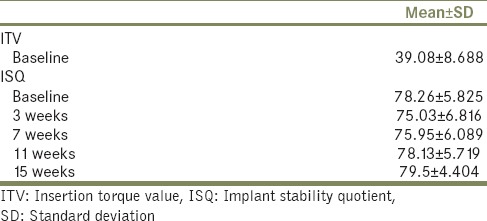
The ITV value recorded ranged from 15 Ncm to 45 Ncm with a mean of 39.08 ± 8.688 Ncm. The mean ISQ value recorded at the baseline was 78.26 ± 5.825. The ISQ mean values recorded at the 3rd, 7th, 11th, and 15th week were 75.03 ± 6.81, 75.95 ± 6.089, 78.13 ± 5.71, 79.50 ± 4.40, respectively, as shown in Table 2. It was observed that the mean ISQ value decreased significantly in week 3 (4.266) and gradually increased significantly through the 7th week up to 15th week for all the implants. Eleven implants however recorded a lower ISQ value at the end of the follow-up when compared to the baseline value, the mean decrease in value being 4.18.
Table 2.
Descriptive analysis of insertion torque value and implant stability quotient of all patients
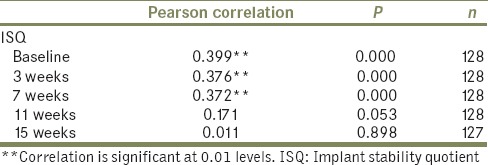
The relation of ITV and ISQ was calculated at the baseline by the Pearson correlation. It was found to be moderately positive and significant (r = 0.399) (P = 0.000) as shown in Figure 1. The correlation of ITV value at baseline and ISQ values recorded at the subsequent weeks was found to be statistically significant at week 3 (r = 0.376) (P = 0.000) and week 7 (r = 0.327) (P = 0.000). There was no significant correlation at 11th (r = 0.171) (P = 0.053) and 15th week (r = 0.011) (P = 0.898) as shown in Table 3.
Figure 1.
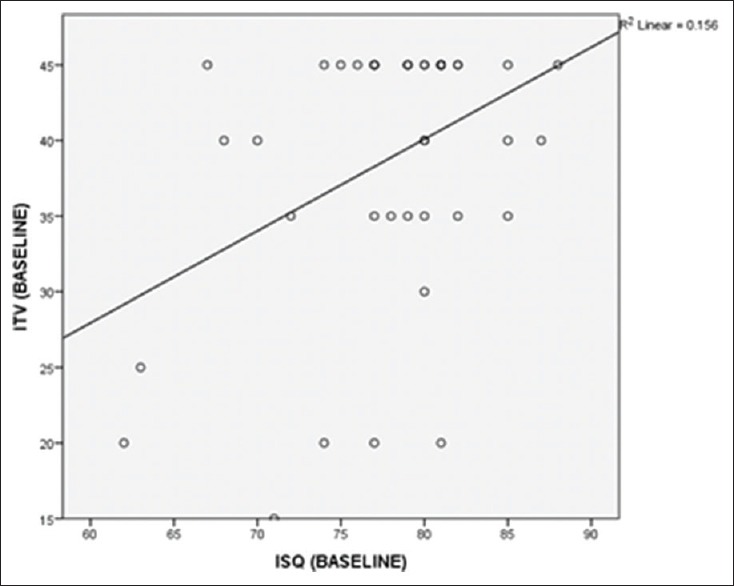
Correlation of insertion torque value and implant stability quotient values at baseline levels
Table 3.
Correlation between insertion torque value and implant stability quotient
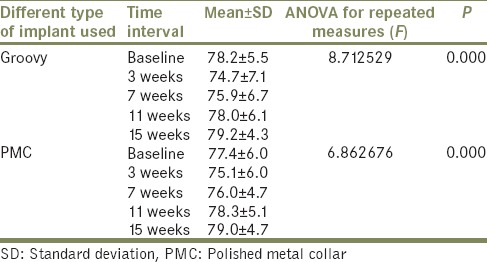
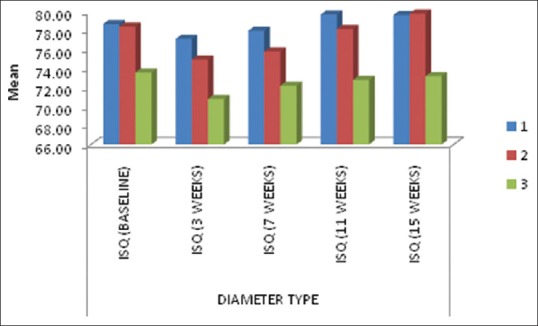
Two different types of implants were used in this study; 15 tissue-level implants Nobel Replace Select PMC and 25 bone-level implants Nobel Replace Select Tapered Groovy. Although the bone-level Groovy implant recorded a higher ITV value (39.2 ± 4.08 Ncm) at baseline when compared to the tissue-level PMC implant (38.2 ± 3.78 Ncm); the difference was not significant as shown in Figure 2 and Table 4. The correlation of ITV and ISQ value at baseline was calculated for the two types of implants used; it was found that there was a significant change in values over the weeks for both. Post hoc analysis showed that the bone-level Groovy implants recorded a lower ISQ value 75.9 ± 6.7 until the 7th week and then increased gradually whereas the tissue-level PMC implants recorded the lowest ISQ value 76 ± 4.7 until the week 7 and then increased gradually. Whereas the tissue-level PMC implants recorded the lowest ISQ value 75.1 ± 6 at the 3rd week and then showed gradual increase as shown in Figure 3 and Table 5.
Figure 2.
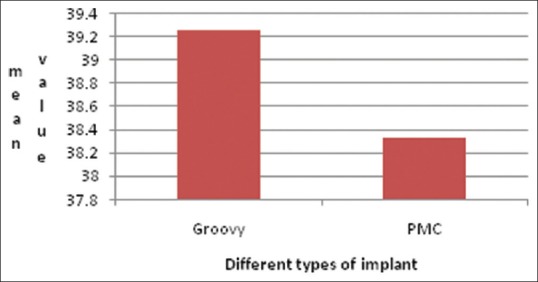
Mean insertion torque values of different implant designs used
Table 4.
Mean values of different variable parameters (diameter, implant type, length)
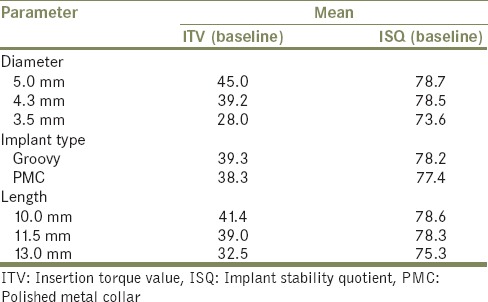
Figure 3.
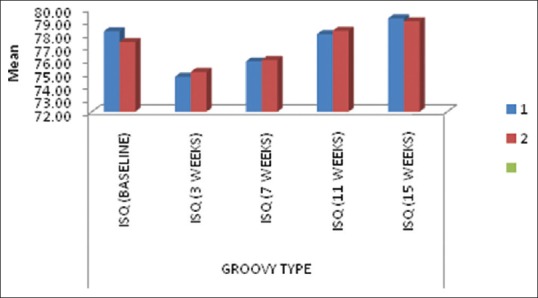
Mean implant stability quotient values of different implant designs used
Table 5.
ANOVA for different types of implants used
Three different diameter types (3.5 mm – 4 implants, 4.3 mm – 30 implants, 5 mm – 6 implants) were used in this study. The mean IT values recorded for the 5 mm implants were significantly higher in comparison to the 3.5 mm implants as shown in Table 3, and there was no significant difference when compared to 4.3 mm implants as shown in Figure 4. No significant changes in ISQ values were seen across the weeks for 5 mm diameter implants with P = 0.199 >0.05. Even in diameter 3.5 mm implants, there was no significant change across the weeks with P = 0.675 >0.05, but in diameter 4.3 mm implants, there was significant change with P = 0.000 <0.001. Further post hoc analysis showed that difference or change was significant at 3rd week as well as at 7th week, but in the 11th and 15th week, the changes were not significant as shown in Table 6 and in Figure 5.
Figure 4.
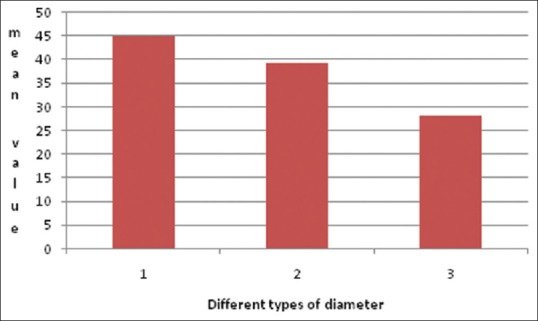
Mean insertion torque value at baseline of different diameter implants
Table 6.
ANOVA for different diameter of implants used
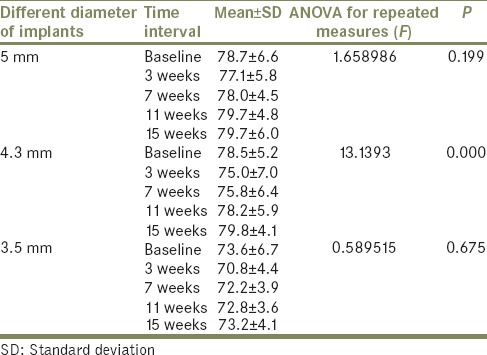
Figure 5.
Mean implant stability quotient recorded for different diameter implants
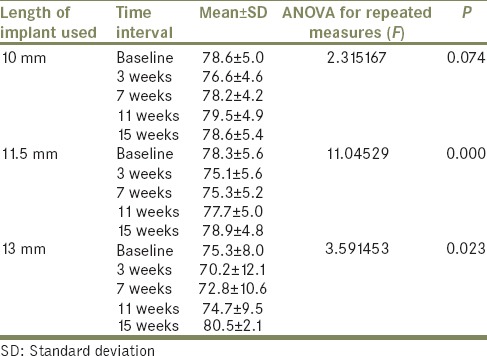
Three implant lengths were used in this study (10 mm length – 12 implants, 11.5 mm – 22 implants and 13 mm – 6 implants). The mean ITV values showed no significant difference in the different lengths of implants used as shown in Table 3 and Figure 6. The ISQ value of 10 mm length implants did not show significant change. Whereas in 11.5 mm and 13 mm lengths, there was significant change, and it was observed till 7th week for 11.5 mm length and till 3rd week for 13 mm length. When the change was compared across the lengths, change was high for 13 mm length compared to 11.5 mm and 10 mm length implants. However, it was not statistically significant in the first follow-up appointment; change at 7th week was high and statistically significant in 11.5 mm and 13 mm implants in comparison to 10 mm implants as shown in Figure 7 and in Table 7. No statistically significant changes were seen after the 7th week for any length of the implants.
Figure 6.
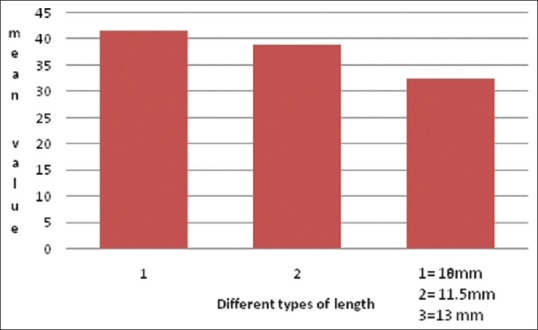
Mean insertion torque value recorded at baseline for different lengths of implants
Figure 7.
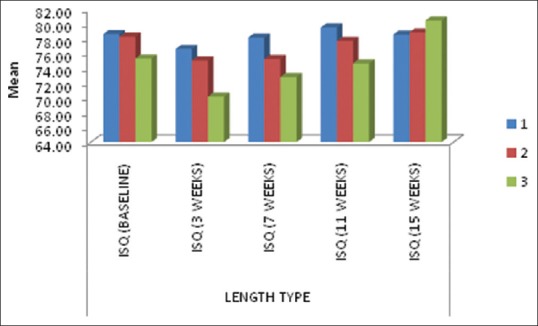
Mean implant stability quotient recorded for different length of implants
Table 7.
ANOVA for different lengths of implants used
DISCUSSION
The time of loading of implants is influenced by the implant stability, and it is one of the most important factors in determining the treatment outcome. Primary stability is the mechanical stability that is achieved immediately after implant insertion, and it is a precursor to achieving good osseointegration. Secondary stability offers biological stability through bone formation and regeneration, and it dictates the time of functional loading.[12]
In the present study, the primary implant stability was measured at baseline by recording the IT value and ISQ using RFA, followed by the measurement of the secondary implant stability by recording the ISQ at weeks 3, 7, 11, and 15 to analyze the dynamic changes that have taken place during the healing period around the implants.
The implant stability is a multifactorial parameter which is influenced by various factors. At implant placement, ITV is a good indicator of primary stability and is influenced by the density of the bone, implant type, surface topography, and the surgical technique used to place the implant.[13] The mean value of ITV at baseline was recorded as 39.08 ± 8.688 Ncm. The ITV in the range of 30–60 Ncm is considered by as a good indicator of primary stability achieved that will ensure a well-osseointegrated implant.[14,15] This value also has been considered as a prerequisite for immediate loading of single implants. ITV is believed to influence the ISQ values. The mean value of ISQ at baseline was recorded as 78.26 ± 5.825 ISQ units. The mean ISQ value at baseline in this study is higher when compared to other studies that ranged from 65.1 to 76.2.[16,17] A moderately positive correlation of ITV and ISQ was found during the course of the present study, and it was significant. The correlation of IT values and ISQ shows the importance of primary stability during initial healing period. This is in agreement to studies which indicate a positive correlation between the two values (Makary et al., 2012 and Filho et al., 2014 found a positive correlation between the ITV and ISQ).[18,19]
The ISQ values which were studied during the course of this study showed a significant decrease in the 3rd week, after which there was a progressive increase in the values till the 15th week. In this study, the dip in ISQ values ranged from 1 to 8 ISQ units which was found to be in agreement with the previous studies, which gave an evidence of a “dip” in the values of the ISQ in the early healing period.[20,21] This dip in the value of the ISQ in the implants during the early healing period can be related to the phases of osseointegration as described in a histological study by Berglundh et al.[22] The author stated that during this dynamic process, the early establishment phase is characterized by bone resorption at the bone-implant interface. This is followed by the maintenance phase which is marked by the rapid bone formation around the implant. Therefore, we can infer that the increased osteoclastic activity is responsible for the significant decrease in the ISQ values during the early healing phase.
The patients included in this study were treated with two different types of implants. The bone-level implant (Nobel Replace Tapered Groovy, Nobel Biocare AB) and tissue-level implant (Nobel Replace Tapered PMC, Nobel Biocare AB). The results showed that ITV was higher for groovy implants when compared to the PMC but not statistically significant. Whereas the ISQ values showed that the bone-level Groovy implants recorded a lower ISQ value (74.89 ± 6.65) until the 7th week and then increased gradually, whereas the tissue-level PMC implants recorded the lowest ISQ value (75.07 ± 6.04) at the 3rd week and then showed gradual increase. This can be attributed to the fact that the PMC type of implant is similar to the groovy implants except for a polished collar of 0.75 mm on its superior surface.
The implant diameter and implant length have also been considered as variables affecting the implant stability. In the present study, 5 mm implants showed statistically significant higher IT values when compared to 3.5 mm, and no difference in values was seen between 4.3 mm and 3.5 mm implants. The ISQ values did not show any significant change across the weeks for all the diameter of implants used, except 4.3 mm implants which recorded statistically significant decrease in ISQ values (P = 0.000) at 3rd and 7th week.
No correlation was found between the implant length and the ITV. However, the values of ITV and ISQ were lowest for the longer implants (13 mm). Decrease in ISQ value at 7th week was high in 11.5 mm (P = 0.000) and 13 mm (P = 0.023) compared to 10 mm length implants which was statistically significant. A study by Makary et al. also concluded by reporting a positive correlation between ISQ values and implant diameter at weeks 3 and 6, whereas no correlation was found to the implant length.[18] Sim and Lang reported in his 12-week follow-up study that ISQ values were influenced by the length of the implants used.[17] A study conducted by Ohta et al. proved no significant correlation between ISQ and the diameter of the implants.[23] Most of the previous publications indicate a low stability associated with shorter implants.[24,25] Telleman et al. reasoned that in comparison to the longer implants, there is lesser bone to implant contact surface for the shorter ones.[26] However, literature suggests a comparable long-term survival rate for both short and long length implants, indicating that the implant stability and hence survival might not be related to the total implant surface.[27] The findings of the present study suggest that implants with larger diameter tend to have good primary stability by having a greater chance to engage the cortical plate, hence providing more bone to implant contact and bicortical engagement. Certain finite element studies have suggested that the wider diameter implant is more favorable in reducing the stress distribution in bone surrounding the implants.[28,29] This will eventually lead to good implant stability and successful integration of the implants.
CONCLUSION
The ITV and ISQ are good indicators of implant stability and can predict the appropriate timing of loading of dental implants and ensure high success rate of this treatment modality. It can be concluded from this study that the ITV and ISQ values recorded at the baseline are statistically significant and that there is a positive correlation between both these values. This ascertains that a higher ITV value can ensure a relatively stable implant during the healing phase, as a higher ITV minimizes the amount or magnitude of micromovements even when loaded immediately which in turn influences the ISQ values.
Even though there was a dip in the ISQ value in week 3–week 7, it was considerably higher than the accepted value for loading an implant (above 60 ISQ units). Therefore, it may be concluded that if the ITV value is more than 30 Ncm, then an implant may be immediately loaded.
There is a positive and statistically significant correlation between the ITV measured using a manual torque wrench and the ISQ measured using RFA. It can be concluded that a higher ITV value ensures greater implant stability during the healing phase and an implant with higher ITV can be loaded immediately without hampering the integration process.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11:491–501. [PubMed] [Google Scholar]
- 2.Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants: A review of the literature. Int J Prosthodont. 1998;11:408–20. [PubMed] [Google Scholar]
- 3.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 4.Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016;16:124–30. doi: 10.4103/0972-4052.176539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Satwalekar P, Nalla S, Reddy R, Chowdary SG. Clinical evaluation of osseointegration using resonance frequency analysis. J Indian Prosthodont Soc. 2015;15:192–9. doi: 10.4103/0972-4052.165171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cehreli MC, Karasoy D, Akca K, Eckert SE. Meta-analysis of methods used to assess implant stability. Int J Oral Maxillofac Implants. 2009;24:1015–32. [PubMed] [Google Scholar]
- 7.Johansson P, Strid K. Assessment of bone quality from cutting resistance during implant surgery. Int J Oral Maxillofac Implants. 1994;9:279–88. [Google Scholar]
- 8.Friberg B, Sennerby L, Meredith N, Lekholm U. A comparison between cutting torque and resonance frequency measurements of maxillary implants. A 20-month clinical study. Int J Oral Maxillofac Surg. 1999;28:297–303. [PubMed] [Google Scholar]
- 9.Testori T, Del Fabbro M, Szmukler-Moncler S, Francetti L, Weinstein RL. Immediate occlusal loading of osseotite implants in the completely edentulous mandible. Int J Oral Maxillofac Implants. 2003;18:544–51. [PubMed] [Google Scholar]
- 10.Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996;7:261–7. doi: 10.1034/j.1600-0501.1996.070308.x. [DOI] [PubMed] [Google Scholar]
- 11.Balleri P, Cozzolino A, Ghelli L, Momicchioli G, Varriale A. Stability measurements of osseointegrated implants using osstell in partially edentulous jaws after 1 year of loading: A pilot study. Clin Implant Dent Relat Res. 2002;4:128–32. doi: 10.1111/j.1708-8208.2002.tb00162.x. [DOI] [PubMed] [Google Scholar]
- 12.Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci. 2013;5:162–7. doi: 10.1556/IMAS.5.2013.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lozano-Carrascal N, Salomó-Coll O, Gilabert-Cerdà M, Farré-Pagés N, Gargallo-Albiol J, Hernández-Alfaro F, et al. Effect of implant macro-design on primary stability: A prospective clinical study. Med Oral Patol Oral Cir Bucal. 2016;21:e214–21. doi: 10.4317/medoral.21024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Testori T, Galli F. Immediate non-occlusal versus early loading of dental implants in practically edentulous patients. Int J Oral Maxillofac Implants. 2007;22:815–22. [PubMed] [Google Scholar]
- 15.Calandierllo R, Rangert B. Immediate functional loading of branemark system wide platform Ti-Unite implants. Clin Implant Dent Relat Res. 2003;5:10–20. doi: 10.1111/j.1708-8208.2003.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 16.Ostman PO, Hellman M, Wendelhag I, Sennerby L. Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont. 2006;19:77–83. [PubMed] [Google Scholar]
- 17.Sim CP, Lang NP. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res. 2010;21:598–604. doi: 10.1111/j.1600-0501.2009.01878.x. [DOI] [PubMed] [Google Scholar]
- 18.Makary C, Rebaudi A, Sammartino G, Naaman N. Implant primary stability determined by resonance frequency analysis: Correlation with insertion torque, histologic bone volume, and torsional stability at 6 weeks. Implant Dent. 2012;21:474–80. doi: 10.1097/ID.0b013e31826918f1. [DOI] [PubMed] [Google Scholar]
- 19.Filho LC, Cirano FR, Hayashi F, Feng HS, Conte A, Dib LL, et al. Assessment of the correlation between insertion torque and resonance frequency analysis of implants placed in bone tissue of different densities. J Oral Implantol. 2014;40:259–62. doi: 10.1563/AAID-JOI-D-11-00183. [DOI] [PubMed] [Google Scholar]
- 20.Ersanli S, Karabuda C, Beck F, Leblebicioglu B. Resonance frequency analysis of one-stage dental implant stability during the osseointegration period. J Periodontol. 2005;76:1066–71. doi: 10.1902/jop.2005.76.7.1066. [DOI] [PubMed] [Google Scholar]
- 21.Balshi SF, Allen FD, Wolfinger GJ, Balshi TJ. A resonance frequency analysis assessment of maxillary and mandibular immediately loaded implants. Int J Oral Maxillofac Implants. 2005;20:584–94. [PubMed] [Google Scholar]
- 22.Berglundh T, Abrahamsson I, Lang NP, Lindhe J. De novo alveolar bone formation adjacent to endosseous implants. A model study in the dog. Clin Oral Implants Res. 2003;14:251–62. doi: 10.1034/j.1600-0501.2003.00972.x. [DOI] [PubMed] [Google Scholar]
- 23.Ohta K, Takechi M, Minami M, Shigeishi H, Hiraoka M, Nishimura M, et al. Influence of factors related to implant stability detected by wireless resonance frequency analysis device. J Oral Rehabil. 2010;37:131–7. doi: 10.1111/j.1365-2842.2009.02032.x. [DOI] [PubMed] [Google Scholar]
- 24.Romeo E, Bivio A, Mosca D, Scanferla M, Ghisolfi M, Storelli S, et al. The use of short dental implants in clinical practice: Literature review. Minerva Stomatol. 2010;59:23–31. [PubMed] [Google Scholar]
- 25.Lee JH, Frias V, Lee KW, Wright RF. Effect of implant size and shape on implant success rates: A literature review. J Prosthet Dent. 2005;94:377–81. doi: 10.1016/j.prosdent.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 26.Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ, et al. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol. 2011;38:667–76. doi: 10.1111/j.1600-051X.2011.01736.x. [DOI] [PubMed] [Google Scholar]
- 27.Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol. 2009;80:1700–18. doi: 10.1902/jop.2009.090107. [DOI] [PubMed] [Google Scholar]
- 28.Himmlová L, Dostálová T, Kácovský A, Konvicková S. Influence of implant length and diameter on stress distribution: A finite element analysis. J Prosthet Dent. 2004;91:20–5. doi: 10.1016/j.prosdent.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Mohammed Ibrahim M, Thulasingam C, Nasser KS, Balaji V, Rajakumar M, Rupkumar P, et al. Evaluation of design parameters of dental implant shape, diameter and length on stress distribution: A finite element analysis. J Indian Prosthodont Soc. 2011;11:165–71. doi: 10.1007/s13191-011-0095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


