Abstract
Corneal diseases are among the major causes of global blindness, secondary to cataract. osteo-odonto keratoprosthesis (OOKP) is the ideal treatment for patients with end-stage inflammatory corneal diseases where a portion of tooth along with bone is used to support an optical cylinder to restore vision in such patients. OOKP surgery requires multidisciplinary approach involving dentists, ophthalmologists, and radiologists. Very less is known in dentistry about the role of the periodontium in the field of ophthalmology. This paper highlights OOKP indications, contraindications, surgical procedure, role of oral structures, advantages, and limitations.
Keywords: Corneal blindness, osteo-odonto keratoprosthesis, tooth root
INTRODUCTION
Eyes are the “Windows to the soul;” the cornea is the “Front Window of the eye.” The most grievous yet, unfortunately, the most commonly occurring loss out of all sensory organs is that of an eye.[1] The importance of corneal disease as a major cause of blindness in the world today remains second only to cataract; however, its epidemiology is complicated and encompasses a wide variety of infectious and inflammatory eye diseases. The general treatment for serious corneal disease is corneal graft by penetrating keratoplasty. However, penetrating keratoplasty failure is virtually certain when the ocular surface is severely compromised. Keratoprosthesis represents the only viable option for restoring sight in these patients.[2]
Keratoprosthesis can be divide into two broad categories; those designed for eyes with a good ocular surface, intact tear film and lids, for example, Boston KPro type 1 or those designed to treat severe dry eyes and damaged ocular surfaces, for example, osteo-odonto keratoprosthesis (OOKP), Boston KPro type 2.[3]
A unique approach to the artificial corneal problem, the OOKP, was developed in Italy by Strampelli in 1963. He had noted that gutta-percha will remain in root canal of the tooth indefinitely, but will be rejected if implanted into soft tissues. Hence, it will seem probable that if a plastic acrylic implant could be held in a piece of the patient's tooth and bone, and the whole placed in a corneal envelope, the tooth, and the bone will form an autograft picture frame for the acrylic and so prevent its extrusion.[4] Strampelli's device used a lamina prepared from a single root tooth with surrounding bone sawn from the patient jaw bone, into which the poly (methyl methacrylate) optic was cemented. Following pioneering work of Strampelli, Falcinelli made stepwise improvements to the original technique, ensuring good long-term visual and retention.[3] Over the past few years, the procedure has undergone further refinements, which are referred to as the Rome–Vienna protocol.
IDEAL KERATOPROSTHESIS[5,6]
The ideal device should be able to surpass the natural cornea by having an improved optical quality, with decreased aberrations and specific power. It should
Have excellent biointegration
Provide resistance against infection and life for lifetime of the patient
Replicate some of the properties of the cornea such as drug penetration and allowing intraocular pressure measurement
Be flush with the rest of the ocular surface to enhance comfort and to reduce mechanical shearing forces on it
Be inexpensive.
INDICATIONS
Indications for OOKP surgery are bilateral corneal blindness resulting from
Severe end-stage Stevens–Johnson syndrome
Ocular cicatricial pemphigoid
Chemical or thermal burns, physical injury (fire, liquid aluminum, etc.)
Trachoma end-stage
Multiple failed penetrating keratoplasty
Corneal failure after vitrectomy with silicone oil filling that can’t be removed safely,
Lyell Syndrome
Epidermolysis bullosa acquisita
Loss of the lids (e.g., Crouzon disease)
Vascularized corneas with complete stem cell loss and dryness following other causes
Erythema multiforme
Trauma limited to only cornea
Severe keratitis
Xerosis
Uveitis
Graft versus host disease.
Bilateral blindness with a visual acuity <1/20 in the better eye is mandatory before the procedure is attempted. Only eye will be rehabilitated with OOKP, as the other eye can be considered a spare eye in case of the comparative rare failure of the eye operated first. Experienced surgeons need not to be deterred by patients with only one eye with visual potential.[6]
CONTRAINDICATIONS
OOKP surgery is absolutely contraindicated in patient who are
Happy with their level of vision
Children under the age of 17 (high rate of turnover of bone during growth in this age)
Eyes with no perception of light (surgery will only harm the patient)
Evidence of phthisis (due to high risk of loss of remaining perception of light)
Advanced glaucoma
Irreparable retinal detachment
Smoking and betel nut chewing etc.
Relative contraindications are as follows:
Mentally unstable patients (may be boggled or confused by the surgery)
Unreasonable expectation of outcome and cosmesis
Unable to commit to lifelong follow-up
Defective light perception (which may signify late stage glaucoma) etc.
PREOPERATIVE PATIENT ASSESSMENT
Multidisciplinary approach is required. Surgical team comprises ophthalmologist, oral surgeon, and radiologist. This involves assessment of the eye and the oral structures.
Preoperative ophthalmological assessment
If the patient can discern hand movement or even has finger counting abilities, one an expect a good functional outcome. Assessment involves
Primary diagnosis and previous surgical interventions (detailed general ophthalmic history and careful examination)
Determining intact and functional retina and optic nerve
Echography, A-scan, B-scan, ultrasound examinations A have to be performed.
Preoperative oral assessment
-
Buccal mucosa assessment
- Tissue condition (severe scaring)
-
Quit habits
- Smoking (to improve graft revascularization)
- Betel nut chewing (compromise tissue quality).
-
Dental assessment
- Healthy tooth root
- Oral hygiene, periodontal status
- Mainstay views: orthopantomograms and intraoral periapical radiographs (to evaluate length, girth of the root, presence of caries, intact pulp, periodontal disease, the surrounding bone of the maxilla, and the space to the adjacent teeth).
Edentulism is common in elderly and patients with oral mucosal diseases, it might be possible to obtain a root from the closely related donor. The long-term success, however, again seems to be slightly worse and the use of immunosuppression in the recipient is certainly necessary.[7] De La Paz et al.,[8] used autologous tibial bone as an alternative to alveolar bone.
Most suitable tooth is maxillary canine due to its longest and largest root with greatest quality of alveolar bone. Preference of the upper or lower canine depends on proximity of maxillary sinus and mental foramen. In lower canine, buccal plate is occasionally thin, and lingual periosteum is difficult to preserve. In upper canine, the risk of antrum perforation is there.
Lack of suitable dentition is a limitation for a number of patients in need of OOKP surgery. In case of no suitable tooth available or in case of edentulous patients, allograft is considered.
Liu et al.[9] studied long-term results of OOKP and concluded that human leukocyte antigen-matched allografts underwent greater laminar resorption.
Preoperative psychological assessment
Risk of psychopathology (past years of poor sight)
Expectations (regarding sight and cosmesis)
Financial, time, emotional stress
Risk of complications
Lifelong follow-up.
SURGICAL PROCEDURE
This surgery is staged, labor-intensive, and relatively invasive procedure requiring dental expertise [Figure 1].
Figure 1.
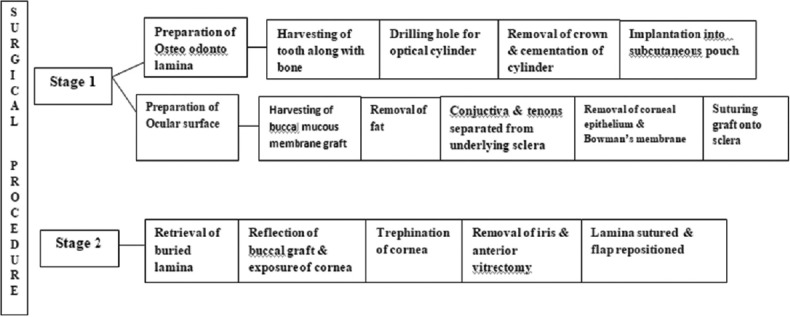
Staged surgical procedure chart
Stage 1 surgery involves covering the ocular surface with buccal mucous membrane graft as well as harvesting a tooth for preparation of OOKP lamina. If the eye is very dry or there is risk if the mucous membrane graft not taking, it may be better to perform Stage 1 surgery into two steps. Otherwise, if there is a significant delay in mucous membrane healing, or if further partial or full repeat mucosal grafting proves necessary, the lamina may be resorbed whilst buried in the lid for an excessively long time.[10]
In Stage 1a, the ocular surface is completely removed and replaced with full-thickness buccal mucosa over the corneal and scleral surface [Figure 2]. This provides a robust mucosal surface to surround and protect the OOKP lamina. The buccal graft must be full-thickness mucosa and of an area large enough to extend from medial to lateral canthi and from upper to lower lid fornices, i.e., harvesting a graft of 3 cm in diameter.[10]
Figure 2.

Eye covered by buccal mucous membrane
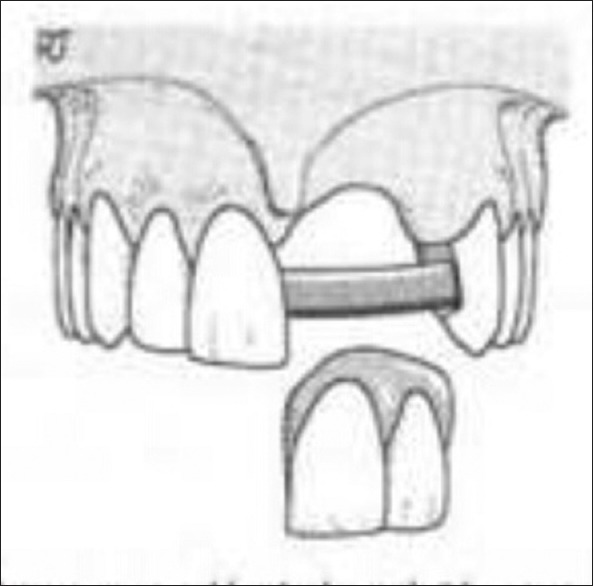
In Stage 1b, a single-rooted tooth and surrounding intact alveolar bone are harvested and used as a biological skirt to surround a PMMA optical cylinder, which is cemented to the dentine of the tooth root [Figure 3]. The competed keratoprosthesis consist of one sagittal half of the canine root with bone ideally measuring 12 mm × 6 mm × 3 mm, carrying an optical cylinder with a margin of dentine of at least 1 mm all around.[11] The implant is then inserted into a subcutaneous or submuscular pouch in the orbitozygomatic area on the contralateral side, where it attains a fibrovascular coating and remains viable.
Figure 3.

Before implantation
Stage 2 usually occurs 2–4 months later, only when the buccal graft is well vascularized and stable. Leaving the lamina for longer than 3 months in the submuscular pouch can result in laminar resorption even before proceeding to the Stage 2. It could necessitate a new lamina preparation, consequently leading to repetition of Stage 1. Therefore, every effort should be made to promptly address mucosal complications and not to prolong the waiting time to 2nd surgery.[12] The implant is then explanted from the subcutaneous or submuscular pouch where it should be covered completely with vascularized connective tissue. The buccal mucosa covering the cornea is partially reflected inferiorly, the center of the cornea is located, and a central trephination is performed. The iris, lens, and anterior vitreous are removed, and the implant is sutured over the cornea, with the posterior optic protruding into the corneal opening. The buccal mucosa is the replaced over the implant and at central 3 mm, trephination exposes the optical cylinder, allowing it to protrude through [Figures 4 and 5].
Figure 4.
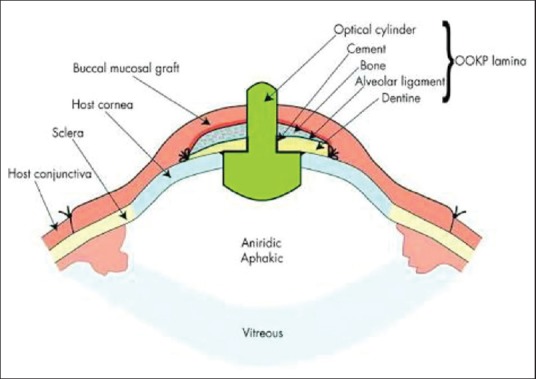
Cross-sectional diagram describing the anatomy and structure of an osteo-odonto keratoprosthesis
Figure 5.

An osteo-odonto keratoprosthesis patient
PROSTHETIC REHABILITATION
Patients are then referred to a prosthodontist for replacement of the missing tooth along with adjacent tissues. The esthetically correct treatment of a localized alveolar ridge defect is a common prosthetic challenge.[13] Anterior ridge defect demands good treatment planning for esthetics and psychological reasons. A successful dentist motivate patients to accept the best possible dental treatment by first determining the basic motives that prompted the patients to seek dental treatment.[14] Young patients often demand fixed prosthesis for the replacement of missing tooth as removable prostheses are less retentive as well as less stable, have poor comfort. However, due to the presence of ridge defect, conventional-fixed prosthesis and implant options prove to be a failure due to poor quality and quantity of bone present. In such situations, Andrew's bridge [Figure 6] is the best option available. Dr. James Andrews of Amite, Louisiana introduced fixed removable Andrew's system.[15] It combines advantages of removable and fixed prosthesis. It consist of crowns over the abutment teeth connected by a bar supporting removable pontics through bar attachment. This option provides better esthetics, phonetics, retention, stability, hygiene, along with reduced bulk. Moreover, torquing forces on the abutment teeth are very less. As OOKP patient has to go for lifelong follow-up visits, so removable portion provides easy access to the underlying tissues. Tissues response remains good due to less impingement of soft tissues.
Figure 6.
Andrew's bridge
FOLLOW-UP VISITS
The follow-up is lifelong and at weekly intervals for 1 month, then monthly for 3 months, then every 2 months for 6 months, and then every 4 months. If stable, then follow-up can be at longer intervals, possibly shared with the referring ophthalmologist. The prosthesis needs careful attention and follow-up and its vulnerability will preclude them from activities with a high risk of contact or contamination.
COMPLICATIONS
During surgery:
Risk of damage to the parotid duct during preparation of the mucous membrane covering
Perforation or leakage of the cornea during preparation of the globe
Oromaxillary fistula formation, fracture of the mandible, and damage to the adjacent teeth during preparation of the lamina
Expulsive hemorrhage during Stage 2 surgery
Choroidal detachment, vitreous hemorrhage, mucous membrane defect, proliferation/Sequestration of bone. However possible
Late postoperative:
Buccal membrane melts or overgrowth
Retroprosthetic membrane formation
Endophthalmitis
Laminar resorption/Osteo odontoacrylic lamina (ODAL) necrosis
Glaucoma, retinal detachment, choroidal detachment, endovitreal hemorrhages, mucosal ulceration/defect/thinning, dental loss, deterioration of visual acuity, hypotonia, etc.
One of the important causes of OOKP failure is laminar resorption. Caiazza et al.,[16] reported the association of early and recurrent bacterial infections due to Staphylococcus epidermidis with extensive laminar resorption.
Postoperative complications are less frequently reported with OOKP than any other materials.
DISCUSSION
The OOKP although described over 50 years ago remains the keratoprosthesis of choice for end-stage corneal blindness.
Nail Onycho keratoprosthesis can be used instead of the tooth, but if it is taken from nail root it is liable to grow in the eye. A piece of cartilage removed from 8th costal cartilage can be used.[4] Some surgeons use tibial bone (temprano keratoprosthesis). Bioceramics can be used but at pH of 6.5-5 associated with infection and inflamed tissue degenerative rate of bioceramics is much higher than bone and tooth.[2]
Strampelli's OOK offers three advantages over alloplastic prostheses (1) permanent fixation of an acrylic lens, (2) insertion of the mucosal epithelium onto the alveolar dental ligament, and (3) long-term retention of the prosthesis due to its complete biological compatibility as far as other pathological conditions do not occur.[17]
The superiority of OOKP over other choices has been proved and supported by various clinical and histological studies as reported by Falcinelli et al.,[18] OOKP is a true heterotrophic autograft made of living human tissue. The dentin, due to its lesser metabolic exchange, provides stability to ODA lamina through a tight and long-lasting contact by means of acrylic resin with the PMMA optical cylinder and gives protection against cylinder extrusion and fistulization.
Hille et al.,[19] reported 100% retention of OOKP lamina in a 5-year follow-up. Iyer et al.,[20] reported a 96% anatomical success of OOKP laminnae in 50 cases with a mean follow-up of 15 months.
In the last decade, research on OOKP has focused on finding new materials that could replace the tooth, while at the same time enhance the adherence between the optical cylinder and the surrounding tissues in the eye.[21,22,23] The introduction of improvements on the surgical technique such as using mitomycin C to prevent epithelial growth over the prosthesis may reduce the rate of postoperative complications significantly and improve the long-term results.[24]
Viitala et al.,[2] compared degradation rate of commercial and natural bioceramics with tooth and bone used in OOKP lamina. Degradation rates were equivalent to tooth and bone at normal physiological pH. degradation rates at lower pH were in the order calcium carbonate corals > biphasic calcium phosphates > hydroxyapatite.
Critical feature for the long-term stability of the OOKP appears to be in the maintenance of osteo-odonto lamina. Reduction in the dimension of laminae can result in aqueous leakage, inflammation, extrusion of the optical cylinder, and endophthalmitis.
It is important to monitor regularly the dimensions and stability of the OOKP lamina as it will help detect cases that are at risk of extrusion of the optical cylinder and consequent endophthalmitis. Fong et al.,[25] recommend a baseline morphological assessment of the OOKP initially by either electron beam tomography or multidetector computed tomography after the OOKP has been implanted to define the dimensions radiologically, and then regularly monitor the dimensions of the OOKP with clinical assessment to identify cases at risk of optic extrusion and consequent endophthalmitis. In the case of patients with significant lamina thinning, prophylactic measures such as removing the OOKP and preparing a new OOKP may be considered to preserve the structure and function of the eye.
Among all, the available biological and synthetic keratoprostheses, the OOKP appears to provide the best long-term anatomical and visual outcomes for the treatment of the severe, end-stage cicatricial, or ocular surface inflammatory diseases.[3] In comparison to OOKP, Boston type 1 KPro surgical procedure is technically less challenging but has a less follow-up record. OOKP, with well-established long-term success, is the gold standard KPro, against which other KPros should be evaluated.[12]
Surgical results demonstrate that modern OOKP surgery has the potential to restore people registered as blind to a level of vision with which they can return to reading, recognizing faces, and navigating around familiar and unfamiliar environments.[10]
CONCLUSION
The OOKP surgical technique has been practiced for the past 50 years. Surgery is extremely demanding and time-consuming and places a great burden on the patients, the relatives, and the surgeon and his team. The rewards will be very satisfying, however, and the patient may regain a quality of life that makes every effort for follow-up and treatment of unavoidable complications worthwhile. The patients will have limited peripheral vision; however, they will be able to navigate, read at least large print, feed, and dress themselves without any assistance.
The creativity to using a tooth as an eye implant should hope to inspire future interprofessionals approaches to ophthalmic practice to provide the best care of the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Choubisa D. A simplified approach to rehabilitate an ocular defect: Ocular prosthesis. J Indian Prosthodont Soc. 2017;17:89–94. doi: 10.4103/0972-4052.179260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viitala R, Franklin V, Green D, Liu C, Lloyd A, Tighe B, et al. Towards a synthetic osteo-odonto-keratoprosthesis. Acta Biomater. 2009;5:438–52. doi: 10.1016/j.actbio.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Tan A, Tan DT, Tan XW, Mehta JS. Osteo-odonto keratoprosthesis: Systematic review of surgical outcomes and complication rates. Ocul Surf. 2012;10:15–25. doi: 10.1016/j.jtos.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Casey TA. Osteo-odonto-keratoprosthesis. Proc R Soc Med. 1966;59:530–1. doi: 10.1177/003591576605900621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu C, Tighe B. The properties of the ideal keratoprosthhesis. An Inst Barraquer. 1999;28:155–6. [Google Scholar]
- 6.Liu C, Tighe B. Striving for the perfect keratoprosthesis. Br J Ophthalmol. 1998;82:3–4. doi: 10.1136/bjo.82.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hille K, Grabner G, Liu C, Colliardo P, Falcinelli G, Taloni M, et al. Standards for modified osteoodontokeratoprosthesis (OOKP) surgery according to Strampelli and Falcinelli: The Rome-Vienna Protocol. Cornea. 2005;24:895–908. doi: 10.1097/01.ico.0000157401.81408.62. [DOI] [PubMed] [Google Scholar]
- 8.De La Paz MF, De Toledo JÁ, Charoenrook V, Sel S, Temprano J, Barraquer RI, et al. Impact of clinical factors on the long-term functional and anatomic outcomes of osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis. Am J Ophthalmol. 2011;151:829–390. doi: 10.1016/j.ajo.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Liu C, Okera S, Tandon R, Herold J, Hull C, Thorp S, et al. Visual rehabilitation in end-stage inflammatory ocular surface disease with the osteo-odonto-keratoprosthesis: Results from the UK. Br J Ophthalmol. 2008;92:1211–7. doi: 10.1136/bjo.2007.130567. [DOI] [PubMed] [Google Scholar]
- 10.Liu C, Paul B, Tandon R, Lee E, Fong K, Mavrikakis I, et al. The osteo-odonto-keratoprosthesis (OOKP) Semin Ophthalmol. 2005;20:113–28. doi: 10.1080/08820530590931386. [DOI] [PubMed] [Google Scholar]
- 11.Manikandan GR, Presanthila J. Modified osteo odonto keratoprosthesis -“tooth for an eye”. Int J Ophthalmol Eye Res. 2015;3:133–7. [Google Scholar]
- 12.Avadhanam VS, Smith HE, Liu C. Keratoprostheses for corneal blindness: A review of contemporary devices. Clin Ophthalmol. 2015;9:697–720. doi: 10.2147/OPTH.S27083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prithviraj DR, Gupta A. An alveolar ridge augmentation using connective tissue graft to improve esthetics in anterior fixed partial denture. J Indian Prosthodont Soc. 2007;7:102–5. [Google Scholar]
- 14.Bandodkar KA, Aras M. Psychological considerations for complete denture patients. J Indian Prosthodont Soc. 2007;7:71–6. [Google Scholar]
- 15.Mueninghoff KA, Johnson MH. Fixed-removable partial denture. J Prosthet Dent. 1982;48:547–50. doi: 10.1016/0022-3913(82)90360-2. [DOI] [PubMed] [Google Scholar]
- 16.Caiazza S, Falcinelli G, Pintucci S. Exceptional case of bone resorption in an osteo-odonto-keratoprosthesis. A scanning electron microscopy and X-ray microanalysis study. Cornea. 1990;9:23–7. [PubMed] [Google Scholar]
- 17.Ricci R, Pecorella I, Ciardi A, Della Rocca C, Di Tondo U, Marchi V, et al. Strampelli's osteo-odonto-keratoprosthesis. Clinical and histological long-term features of three prostheses. Br J Ophthalmol. 1992;76:232–4. doi: 10.1136/bjo.76.4.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falcinelli G, Falsini B, Taloni M, Colliardo P, Falcinelli G. Modified osteo-odonto-keratoprosthesis for treatment of corneal blindness: Long-term anatomical and functional outcomes in 181 cases. Arch Ophthalmol. 2005;123:1319–29. doi: 10.1001/archopht.123.10.1319. [DOI] [PubMed] [Google Scholar]
- 19.Hille K, Hille A, Ruprecht KW. Medium term results in keratoprostheses with biocompatible and biological haptic. Graefes Arch Clin Exp Ophthalmol. 2006;244:696–704. doi: 10.1007/s00417-005-0092-6. [DOI] [PubMed] [Google Scholar]
- 20.Iyer G, Pillai VS, Srinivasan B, Falcinelli G, Padmanabhan P, Guruswami S, et al. Modified osteo-odonto keratoprosthesis – The Indian experience – Results of the first 50 cases. Cornea. 2010;29:771–6. doi: 10.1097/ICO.0b013e3181ca31fc. [DOI] [PubMed] [Google Scholar]
- 21.Tan XW, Perera AP, Tan A, Tan D, Khor KA, Beuerman RW, et al. Comparison of candidate materials for a synthetic osteo-odonto keratoprosthesis device. Invest Ophthalmol Vis Sci. 2011;52:21–9. doi: 10.1167/iovs.10-6186. [DOI] [PubMed] [Google Scholar]
- 22.Tan XW, Beuerman RW, Shi ZL, Neoh KG, Tan D, Khor KA, et al. In vivo evaluation of titanium oxide and hydroxyapatite as an artificial cornea skirt. J Mater Sci Mater Med. 2012;23:1063–72. doi: 10.1007/s10856-012-4578-6. [DOI] [PubMed] [Google Scholar]
- 23.Huhtinen R, Sandeman S, Rose S, Fok E, Howell C, Fröberg L, et al. Examining porous bio-active glass as a potential osteo-odonto-keratoprosthetic skirt material. J Mater Sci Mater Med. 2013;24:1217–27. doi: 10.1007/s10856-013-4881-x. [DOI] [PubMed] [Google Scholar]
- 24.Avadhanam VS, Herold J, Thorp S, Liu CS. Mitomycin-C for mucous membrane overgrowth in OOKP eyes. Cornea. 2014;33:981–4. doi: 10.1097/ICO.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 25.Fong KC, Ferrett CG, Tandon R, Paul B, Herold J, Liu CS, et al. Imaging of osteo-odonto-keratoprosthesis by electron beam tomography. Br J Ophthalmol. 2005;89:956–9. doi: 10.1136/bjo.2004.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]


