Abstract
As understanding of health deficits among people with intellectual and developmental disabilities (IDD) increases, concerns grow about how to develop comprehensive, sustainable surveillance systems to reliably monitor the health of this population over time. This study reviews literature from 12 countries in which retrospective administrative data have been used to estimate population-based prevalence of IDD, identifies promising practices in that literature, and discusses the feasibility of applying those promising practices to other countries. Administrative data sources can be used to identify the number of people with IDD (numerators) in the presence of population estimates from which people with IDD are drawn (denominators) for discrete geographic locations. Case ascertainment methods, age groupings, data years captured, and other methods vary, contributing to a wide variation in prevalence rates. Six methods are identified from five countries that appear to offer the greatest likelihood of expanded applications. Approaches in which administrative data collections are linked with other population-based data sources appear promising as a means of estimating the size and characteristics of populations living with IDD in defined geographic locations. They offer the potential for sustainability, timeliness, accuracy, and efficiency.
Keywords: administrative data, data collections, health surveillance, intellectual and developmental disabilities, prevalence
Background
Intellectual and developmental disabilities are a group of developmental conditions characterized by significant impairment of cognitive functions, which are associated with limitations of learning, adaptive behavior, and skills (Salvador-Carulla et al., 2015). While others have suggested naming this condition “disorders of intellectual disability” (DID) for, among other reasons, the need to be inclusive of individuals for whom the condition is diagnosed at all ages in the life span (Tassé, Ruth Luckasson, & Nygren, 2013), the impairment itself needs to be present in childhood. The American Association on Intellectual and Developmental Disabilities (AAIDD) considers “developmental disabilities” an umbrella term that includes intellectual disabilities (“a disability characterized by significant limitations both in intellectual functioning—reasoning, learning, problem solving—and in adaptive behavior, which covers a range of everyday social and practical skills, originating before the age of 18”) but also includes other disabilities apparent from childhood. Developmental disabilities, occurring before the age of 22, can be cognitive, physical, or both and are usually lifelong. Their definition goes on to state that intellectual disability encompasses the “cognitive” part of developmental disabilities, typically interpreted as thought processes (AAIDD, 2016). While global variation exists, broadly speaking, the condition that includes intellectual disability that appears most frequently in the literature is that of intellectual and developmental disabilities, IDD, which for the purposes of our investigation is the terminology used in this report.
In order to anticipate resource use and provide appropriate services to people with IDD, accurate, ongoing, and detailed surveillance data are essential. Difficulties in monitoring and tracking populations in which clinical conditions are hard to define, such as those with IDD, present a unique challenge for public health (Institute of Medicine, 2007; Mont, 2007; World Health Organization, 2011). This challenge comes at a time when public health surveillance is at a crossroads, facing major issues relating to evolving information science and technology, adapting to new means of data access and use; and efficiently and effectively pursuing new forms of data management, storage, and types of analysis. (Thacker, Qualters, & Lee, 2012). As the entire field of public health surveillance evolves to adapt to these changing needs and technologies coupled with existing challenges in completeness of case identification, ascertaining populations with IDD that were already difficult to reach may become even more difficult.
Population-based surveys, such as the National Health Interview Survey (NHIS) or National Health and Nutrition Examination Survey (NHANES), ask about numerous medical conditions that require valid and reliable case definitions of specific disabilities but exclude potentially large segments of the population living in institutionalized or group settings, in addition to being expensive to administer, subject to bias in parental reporting, and susceptible to misclassification or under ascertainment (Krahn, Fox, Campbell, Ramon, & Jesien, 2010; Larson, Lakin, Anderson, Kwak Lee, & Anderson, 2001). Developing accurate case definitions that lend themselves to phone, mail, or in-person surveys requires input from multiple subject matter experts, often obtained by convening an expert panel. Once a valid and reliable case definition is developed for a survey, implementing it can be costly due to the need to expand sample size based upon anticipated low prevalence and geographically dispersed populations. Follow-up surveys, while helpful at “mining” data in more depth once key targeted subgroups of population surveys are identified, may also be costly to implement.
Population censuses, a second data source for surveillance sometimes used to estimate IDD prevalence, are typically required by governments for electoral apportionment, while also being used to determine funding for health, education, and other human services programs. They are periodic rather than ongoing, although their periodicity varies from nation to nation. Data collected on disability are typically very broad, not including clinical diagnoses and not allowing for case definitions for specific conditions such as IDD. In the United States, for example, six broad functional questions taken from the American Community Survey are now used to capture disability status for people aged five and older around areas of vision, hearing, mobility, cognition, independent living, and societal participation (Brault, 2012). While the question on cognition could include people with IDD (“Because of a physical, mental, or emotional condition, does anyone (in your household) have serious difficulty concentrating, remembering, or making decisions?”), many people with other conditions resulting from trauma, stroke, or episodic stress may also be included.
Administrative data are a third potential data source for implementing surveillance for populations with IDD. Because they are designed to capture information on people for programmatic purposes that may include items such as eligibility determination and service use, including cost and quality, these data can include a rich trove of information. Their primary limitation, however, is that they only include people during discrete periods of time when they meet certain criteria to participate in the program (Krahn et al., 2010). This means that, for example, people with IDD may age out of educational systems, or be subject to intermittent enrollment in health or social services, including health insurance, so that individual encounters may not be captured. Yet their availability both as an existing database and as a source of active record reviews makes them highly desirable as a potential means of surveillance for informing resource needs, even as the challenge of organizing data into accessible and useful formats remains (Lin et al., 2014; Thacker et al., 2012). With this in mind, reviewing experiences of other countries in their use of administrative data for IDD surveillance was considered worthwhile.
Specific Aims
The specific aims of this study are twofold: first, to identify and describe examples of how administrative data have been used to estimate prevalence of intellectual disabilities, using examples from around the globe; and second, to assess the feasibility of using administrative data to estimate prevalence of IDD, within the context of a changing public health surveillance landscape. Countries in which IDD prevalence has been estimated will be identified along with definitions of IDD, methods used to implement these definitions, the number and type of numerator(s) and denominator used, and a summary of prevalence estimates created from these techniques. We discuss the unique challenges in using administrative data to estimate prevalence of IDD relative to the varying approaches employed between countries, while considering potential feasibility for enhancing this approach.
Methods
Literature Search
We searched PubMed and PsycInfo using the following search strategy outlined in Figure 1:
title contains “intellectual disability” or “intellectual disabilities” or “mental retardation” or “learning disability” or “learning disabilities”; AND
text contains ”prevalence”; AND
article was published between 2000 and 2015, inclusive; AND
language of article is English.
FIGURE 1.
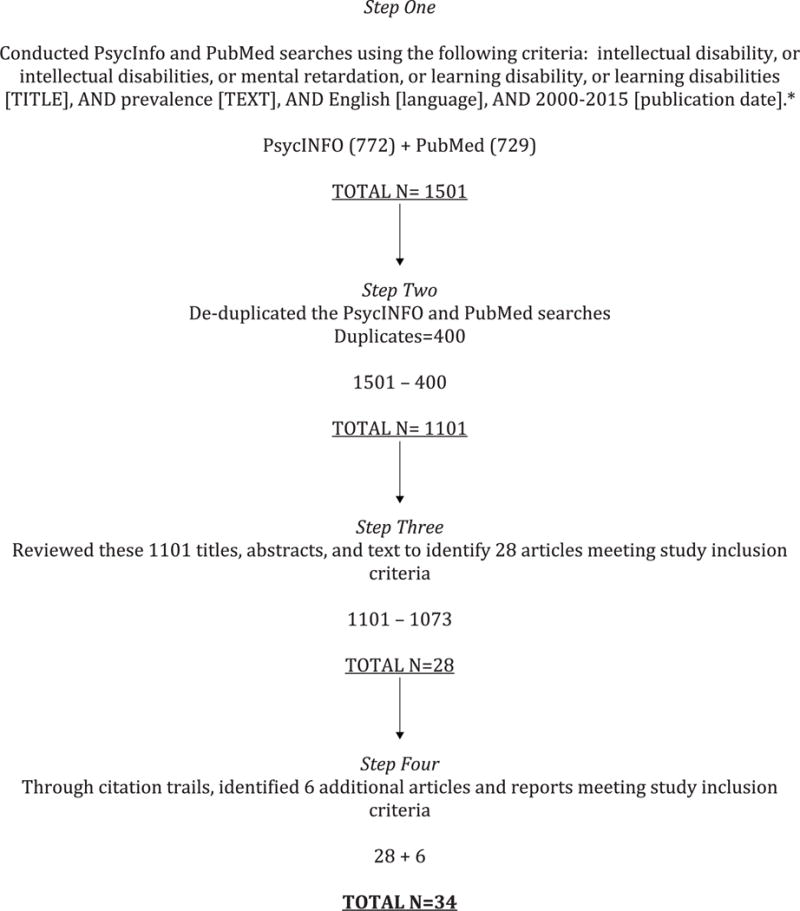
Flowchart of search algorithm.
*Due to a software update that occurred in 2015, PsychInfo search for that year used “prevalence” for anywhere in the article rather than just in the text as was used for 2000-2014. This may have had the effect of bringing in more articles to review for just this year than in previous years.
As the focus of our investigation was on intellectual disabilities as a subset of developmental disabilities, we did not include “developmental disabilities” as a search term by itself.
Study Inclusion Criteria
Types of participants
We included studies whose participants had been assessed for IDD as indicated in large administrative data sets.
Administrative data sets
Administrative data were defined as data resulting from managing health care, education, social services, and income support services (adapted from Iezzoni, Schwartz, & Ash, 2005). The primary purpose of administrative data collection is for determining eligibility and enrolling people in government or related programs; managing health care, educational, social services, and income support programs; and tracking service use.
Type of outcome measure
Our review focused solely on prevalence of intellectual disability.
Types of studies
The two different types of studies included in the search were cohort and cross-sectional studies.
Study Exclusion Criteria
We excluded the following studies: (1) Non-original articles like letters, reviews, editorials, and book chapters reporting on previously published studies; (2) studies that may have used administrative data to expand the epidemiology of IDD populations, but did not specifically generate prevalence estimates; (3) studies describing intellectual disability only in specific population subgroups, such as persons with Down syndrome, specific genetic disorders, or low birth-weight.
The title, abstract, and where necessary, the text of each article were screened to identify relevant articles. References of the selected studies and other relevant studies were hand searched and included if eligible. Two reviewers (DJF and MF) reviewed the selected articles and any disagreements as to eligibility for inclusion were discussed and resolved and, where necessary, adjudicated by a third reviewer (GP).
Data Extraction
Qualitative data extracted from each selected article included study design, sampling method, target population and study period, selection bias (representativeness of the data), case ascertainment, assessment instruments and diagnostic systems used to determine IDD, age and gender distribution, and etiological factors. When multiple articles from the same study were identified, only the most relevant articles (based on the information available) from each unique study were included. Quantitative data included estimates about sample size and prevalence of individuals with diagnosis of intellectual disability.
We used the following categories to classify articles:
Type of population targeted: national; subnational (regions, provinces, cities, etc.)
Age group of study population: adult; child/adolescent; both adult and child/adolescent
Type of study: cross-sectional; cohort
Source of data: medical claims; administrative registry; school based study.
Promising practices towards developing accurate estimates of IDD prevalence were selected based upon the research teams’ evaluation of studies using the following criteria:
credible use of data;
rigorous scientific design;
potential for comparability between countries;
duplicability and generalizability in approach.
Limitations
This review is based upon PubMed and PsychINFO searches and literature identified by following citation trails. As such, it was intended to enhance our understanding of practices currently in place that have been documented in published or grey literature cited in published articles in the English language. It is likely that our review omits practices that are not described in these sources which may be worthy of greater study. Among practices we did identify, we did not verify prevalence findings ourselves, so it is possible that practices described as promising may not, in fact, be accurate or reliable, although appearance in peer-reviewed literature provides some guard against that. We also did not employ meta-analytic statistical techniques to analyze our literature for reasons owing to the two limitations cited above. Because this was a literature review and not a more systematic or scoping review of the literature, we could not run the risk of assuming that studies identified all reported findings which were complete, valid, reliable, and not subject to bias, all key assumptions in undertaking meta-analyses. Related to this, the lack of a standardized “effect size” that could be compared using a common statistical measure that could lead to weighted averages prevented us from examining differences in this more rigorous manner. Given variation in how intellectual disabilities is defined in different countries, and what may be overlap or confusion between the use of that term and “developmental disabilities,” omitting “developmental disabilities” from our search criteria may have led to overlooking some studies that may otherwise have been included.
Findings
Number of Articles and Countries
Literature estimating the prevalence of IDD using administrative data was identified in 34 articles and reports1 from 12 countries: Australia, Canada, Finland, France, Ireland, the Netherlands, Norway, Sweden, Taiwan, Turkey, United Kingdom, and the United States (see Table 1).
TABLE 1.
Using administrative data for estimating prevalence of intellectual disabilities, by country, 2000–2015
| Country and Citation | Databases Used Numerator/Denominator | Case ascertainment methods | Population | Prevalence estimates |
|---|---|---|---|---|
| Australia | ||||
| Leonard et al. (2003) |
|
Disability Services Commission (DSC): (1) IQ <70 on formal testing; (2) condition associated with intellectual disability; or (3) documented with intellectual disability in DSC records. Department of Education: “significant deficits in adaptive behaviour and academic achievement and demonstrate intellectual functioning two or more SD below the mean on an approved measure of cognitive functioning.” |
Live births 1983–1992, surviving to end of 1999 | 14.3/1000 live births - 17.4/1000 live male births - 10.9/1000 live female births 10.6/1000 live births—mild-moderate ID 1.4/1000 live births—severe-profound ID |
| Petterson et al. (2007) | 1) Intellectual Disability Exploring Answers (IDEA) Database Western Australia Birth Defects Registry Births |
IQ <70 and indication of developmental delay before 18 years | Live births 1980–1999, surviving to one year | 13/1000 live births-ID |
| Petterson et al. (2005) |
|
IQ <70 and indication of developmental delay before 18 years | Live births 1983–1996 | 15.2/1000 live births |
| Canada | ||||
| Bradley et al. (2002) | 1) Community agencies and institutions serving the population aged 14 to 20: - Social services - Education - Mental health - Corrections - Residential services - Native centers Population census |
IQ testinga of individuals identified with (a) significant intellectual impairment or marked difficulties in learning, including measured or judged IQ that was borderline or below average, or (regardless of IQ), significant social impairment or marked difficulties relating to others | Ages 14–20 residing in Niagara region in June, 1994 | 7.2/1000 ages 14–20 overall 3.5/1000 ages 14–20— (IQ = 50–75) 3.6/1000 ages 14–20 (IQ<50) |
| Lin et al. (2013) | 1) Ontario Mental Health Reporting System 2) Canadian Institute of Health Information - Discharge Abstract Database - Same Day Surgery - National Ambulatory Care Reporting System 3) Ontario Health Insurance Plan 4) Ontario Registered Persons Canadian Census 2008 |
Intellectual and developmental disabilities (IDD): “lifelong limitations in cognitive and adaptive functioning that originate before the age of 18 and impact on activities of daily living, operationalized in individual data sources through IDD diagnosis (ICD-9, ICD-10, DSM-4 codes, as specified) in any diagnostic field |
Ages 18–64 in Ontario Registered Persons Database, April 2009 | Broad IDD = 8.0/1000b Intermediate IDD criterion=5.2/1000 Narrow IDD criterion= 1.8/1000 |
| Ouellette-Kuntz et al. (2010) | 1) Hospital abstracts database 2) Physician claims database 3) Education enrollment 4) Social Assist. Management Information Network Manitoba Health and Healthy Living health care registrants |
Individuals who met at least one of the following three criteria classified as ID: (1) receiving income assistance for reasons of ID from Manitoba Department of Family Services and Housing; (2) receiving special education from Manitoba Department of Education, Citizenship and Youth for reasons of multiple handicaps usually defined as ID plus one or more physical disabilities; (3) at least one diagnostic code for ID based on International Classification of Diseases | All persons of any age who were living with an ID in Manitoba, 1998–2003 | 4.7/1000—ID overall 4.0/1000—mild ID 0.4/1000—profound ID |
| Finland | ||||
| Arvio & Sillanpaa (2003) | 1) Client register Population estimates |
Clinical assessment of intelligence level IQ ≤70 Severe and profound ID (SPID) IQ ≤35 |
All ages 1995 | 4.3/1000—ID (IQ≤70) 1.3/1000—Severe to profound ID |
| Heikura et al. (2005) | 1) Hospital Discharge 2) Cause of Death 3) National Insurance and Medication Reimbursement Registers 4) Hospital, family counseling, public health center, and institutional, including school, health records at ages 7–8 North Finland Birth Cohort |
Psychometric testing or clinical assessment | 1986 North Finland Birth Cohort, follow-up in 1996 | 11.2/1000 live births—ID (IQ≤70) 7.5/1000—mild ID (IQ=50–70) 3.8/1000—severe ID (IQ≤50) |
| Heikura et al. (2003) | 1) Hospital Discharge 2) Cause of Death 3) National Insurance and Medication Reimbursement Registers 4) Hospital, family counseling, and institutional records 5) Questionnaires Population data, Central Statistical Office |
Psychometric tests, administered by a psychologist, were collected from hospitals, institutions for children with intellectual disability, family counseling centers, and school psychologists. No separate evaluations or examinations were made for the purposes of either of these cohort studies.c | 1966 and 1985–1986 birth cohorts at age 11.5 years 1977 (1966 births) 1996 (1985–86 births) |
1966 births: 11.0/1000—IQ≤70d 5.0/1000—IQ=50–70 2.6/1000—IQ=35–49 2.1/1000—IQ=20–34 1.4/1000—IQ≤20 1985–86 births: 11.2/1000—IQ≤70 7.5/1000—IQ=50–70 1.7/1000—IQ=35–49 0.8/1000— IQ=20–34 1.9/1000—IQ≤20 |
| Patja et al. (2000) | 1) Reports from municipal officials Population estimates |
ID=IQ < 70 and by evaluation of adaptive behavior Municipal officials “asked to report all people suspected or known to have ID. The National Board of Health organized examinations” |
1962: ages 2-64 1995: > 40 1962, 1995 (follow-up) |
1962: 7.0/1000-ID 1995: 4.0/1000—ID, ≥ 40 years of age |
|
Westerinen et al. (2007) Westerinen et al. (2014) |
1) National Pension Institute - Disability, Pensioners’ Care, Funding of Rehabilitation 2) Long-term Medication Registers of Hospital Care and Care for the Intellectually Disabled: - Discharge Reg. of Hospitals - Discharge Reg. of Social Care Population estimates (not specified) |
One to three diagnoses coded for each benefit decision (ICD-9 or ICD-10)e | All individuals recorded in any register listed under Data Source. 2000 |
Combined registers:f 7.0/1000—ID overall 5.3/1000—ages 0–15 7.0/1000—ages 16–39 9.2/1000-ages 40–64 3.8/1000—ages 65+ |
| France | ||||
| Cans et al. (2003) | 1) Registre des Handicaps de l′Enfant et Observatoire Périnatal Population estimate of resident children |
All children with disabilities living in Isere county, aged 7 years, with a clinical feature of a severe deficiency registered. Registration done actively by physician. IQ <50 or mental retardation classified as profound, severe, or moderate. |
Children age 7 1980–1991 | 2.8/1000 resident children age 7— “severe mental retardation” |
| David et al. (2014) | 1) Maisons Départementales des Personnes Handicapées (provides and authorize payment of disability benefits) 2) Department of Education Total population of children born in 1997 residing in Isère in 2008 |
Mild intellectual disability (MID) diagnosed ages 9–13. MID = IQ 50–69. NOTE: all children IQ=46–77 included. | Children born in 1997 residing in Isère County, France, in 2008 | 18/1000—mild intellectual disability |
| Ireland (including Northern Ireland | ||||
| Kelly et al. (2012) | 1) National Intellectual Disability Database Census (2011) |
Service providers, local health office personnel, school principals | Recipients of day, resident, & multidisciplinary support - 2012 | 6.0/1000 ID 2.0/1000—mild ID 3.5/1000—moderate, severe or profound ID |
| McConkey et al. (2006) | 1) National Intellectual Disability Database 2) Regional databases (Northern Ireland): - Child Health System Module V of children with special needs with records retained into adulthood - Soscare system of anyone who made contact with social services, including ‘dormant’ cases Northern Ireland Census Republic of Ireland Census |
Republic of Ireland: All individuals known to have a moderate, severe and profound ID (using ICD-10) or anyone else receiving or needing ID services Northern Ireland: all persons with a ‘learning disability’ ages 20 + and living with family or in their own accommodation identified from the records held by the local statutory HSS Trust. In either jurisdiction, intellectual or learning disability=‘significant impairments of intelligence and social functioning’ with onset in the developmental period. Severe disability= IQ <50, mild disability=IQ 50–78. Classifications by service personnel who completed data records. |
Republic of Ireland: ages 20+ receiving day, residential, and multidisciplinary support Northern Ireland: ages 20+ in contact with statutory health and social services - 2001 |
Republic of Ireland: 6.1/1000 ages 20+ 6.5/1000—males ages 20+ 5.6/1000—females ages 20+ 1.7/1000—ages 20+ mild ID 3.8/1000—ages 20+ severe ID Northern Ireland 7.0/1000 ages 20+ 8.1/1000 males ages 20+ 6.03 females ages 20+ 2.1/1000—ages 20+ mild ID 4.9/1000—ages 20+ severe ID |
| Netherlands | ||||
| van Schrojenstein Lantman-de Valk et al. (2006) | 1) General practice (GP) databases 2) Service providers (residential facilities, group homes, day care facilities, special schools) Population estimates (not specified |
General Practitioner Health Information System (GPHIS), ICPC codes, with follow-up of physicians Service providers to ID populationg |
Individuals with ID identified through GPHIS and service providers, all ages 2001 |
Minimum prevalence estimate: 6.4/1000 ID Maximum prevalence estimate: 7.0/1000 ID |
| Wullink et al. (2007) | 1) General practice (GP) databases 2) Service providers (residential facilities, group homes, day care facilities, special schools) Population estimates (not specified) |
General Practitioner Health Information System (GPHIS), ICPC codes, with follow-up of physicians Service providers to ID population.h |
Individuals with ID identified through GPHIS and service providers, all ages 2001 |
Extrapolation #1: Minimum prevalence estimate: 6.4/1000 ID Maximum prevalence estimate: 7.0/1000 ID Extrapolation #2: Minimum prevalence estimate: 5.4/1000 ID Maximum prevalence estimate: 6.0/1000 ID |
| Norway | ||||
| Søndenaa et al. (2010) | 1) Norwegian Ministry of Local Government and Regional Development statistics for income in local communitiesi Statistics Norway population estimates |
Physician diagnosis using criteria in ICD-10 F70–79. Several examinations during childhood where ID may be discoveredj | All people with ID reported from 430 municipalities 2008 |
4.4/1000–ID |
| Strømme and Hagberg (2000) | 1) Schools for children with learning difficulties 2) Educational psychology services (within school systems) 3) National Epilepsy Centre 4) The National Centre for Child and Adolescent Psychiatry, Department of Medical Genetics, Ullevål Hospital Oslo Medical Birth Registry |
MR=IQ≤ 70, either based on an individually administered standardized psychometric test or formal developmental assessment Mild mental retardation (MMR)=IQ 50 to 70 Severe mental retardation (SMR) = IQ<50 |
All Akershus County births 1980–1985 alive at 1 year of age, at ages 8–13 1992–1997 |
6.2/1000 overall, ages 8–13 |
| Sweden | ||||
| Ng et al. (2015) | 1) Swedish Act concerning Support and Service for Persons with Certain Functional Impairments (LSS) 2) Death registry Total population statistics from the Statistics Sweden database |
“…individuals with ID, autism or pervasive developmental disorders from birth or early age, regardless of the severities of the problem. They are eligible to receive different LSS services, and hence registered in the LSS register.” | Ages 55 + 2004–2012 |
2004: 2.8/1000 (male) 2.1/1000 (female) . . 2012: 3.1/1000 (male) 2.3/1000 (female) |
| Taiwan | ||||
| Lai et al. (2012) | 1) Disability Registry Population estimates (not specified) |
“…IQ score below 70 (more than 2 standard deviations below the mean) in a test administered by a psychologist certified by the government and then been confirmed as having ID by a doctor accredited by the government” | Ages 3–17, 2004–2010 |
5.8/1000—ID, ages 3–17 2.3/1000—ID, ages 3–5 5.9/1000—ID, ages 6–11 6.6/1000—ID, ages 12–14 7.2/1000—ID, ages 15–17 |
| Lin (2009) | 1) Physically and Mentally Disabled Population by Age and Level Department of Statistics 2008a Taiwan General Population by Age (Department of Statistics) |
Cases with “ID classified and defined by the health authorities and registered by the social welfare authorities.” ID defined as “presence of significant intellectual retardation or incomplete mental development during the growth period.”k |
All ages 2000–2007 |
3.9/1000—ID |
| Turkey | ||||
| Ayoglu et al. (2008) | 1) Learning Disability Guidance and Research Center (LDGRC) of Zonguldak records Population estimates (not specified) |
“IQ <44 profound (severe), IQ 45–70 moderate (mild) and IQ 71–89 slow learner (borderline).” | Ages 6+ 1995–2003 |
61.9/1000—male urban 5.4/1000—male rural 38.2/1000—female urban 3.4/1000—female rural |
| United Kingdom (including England and Wales) | ||||
| Emerson (2012) | 1) Income Deprivation Affecting Children Index (areal)* *Used for both numerator and denominator |
“Special Educational Needs co-coordinator and an external professional (e.g., an educational psychologist) identifies and classifies children with special educational needs, including moderate learning difficulties; severe learning difficulties; profound multiple learning difficulties” | School children ages 7–15 2008 |
School Action Plan or Statement or SEN 36/1000—moderate learning disabilities 5/1000—severe learning disabilities 1/1000—profound multiple learning disabilities Statement of SEN 10/1000-moderate learning disabilities 4/1000—severe learning disabilities 1/1000—profound multiple learning disabilities |
| Emerson and Glover (2012) | 1) Department of Education National Pupil Database 2) NHS Information Centre for Health and Social Care 3) Learning disability registers English Spring 2008 School Census* 4) Office for National Statistics population estimates * *Both numerator and denominator |
“Children… [with] Statement of Need (SEN) … at the School Action Plus stage of assessment and had either a primary or secondary SEN of “moderate learning difficulty”, “severe learning difficulty” or “profound multiple learning difficulty”. Adults identified with learning disabilities in GP practice registers | School children ages 5–15 Adults ages 18+ 2010 |
40–50/1000—ages 10–15, SEN total 6–7/1000—ages 20–30 |
| Emerson et al. (2012) | 1) General Practice learning disability registers 2) Department for Education National Pupil Database* *Both numerator and denominator |
Special Educational Needs (SEN) assessments of children in maintained and non-maintained special schools General practice learning disability registers |
School children ages 5–15 Adults ages 18 + 2011–2012 |
29/1000—ages 5–15, primary or secondary SEN associated with learning disabilities 4.5/1000—ages 18 + |
| Kiani et al. (2013) | 1) Leicestershire ID Register National Statistics | Clinical diagnosis with ICD-10 codes | Ages 19+ registered with ID service 2001–2006 | 3.9/1000—moderate to profound ID, with mild ID less well represented |
| McGrother et al. (2002) | 1) Leicestershire Learning Disability Register Population census |
“Dependency on specialist services among adults with severe or profound adaptive behaviour problems associated with a moderate, severe or profound developmental intellectual impairment” | South Asian and white adults 20+ on Register 1991 |
3.6/1000 |
| McGrother et al. (2001) | 1) Leicestershire Learning Disability Register Population census |
“Moderate, severe or profound developmental intellectual impairment with adaptive behavior problems and includes dependency on specialist services;” “Structured home interview using Disability Assessment Schedule” |
Adults over school age reported to Register 1995 | 3.9/1000—prevalence of notified need for LD services 3.4/1000—prevalence of intellectual impairment |
| Morgan et al. (2000) | 1) Inpatient/outpatient services 2) Accident and emergency department visits 3) Social Services District Reg. 4) Long-stay learning disability hospital database 5) Mortality Population estimates |
“(a) inclusion on the social services district register; (b) an in-patient admission within the learning disability specialty or with a diagnostic code of mental handicap (ICD±9 317±319 or ICD±10 F70±79; World Health Organization, 1978, 1986); (c) an out-patient appointment in the learning disability specialty; (d) inclusion on a long-stay learning disability hospital data set” | Resident until April 1996 of South Glamorgan Health Authority 1991–1997 |
3.7/1000 overall 4.1/1000—males 3.2/1000—females |
| United States | ||||
| Bhasin et al. (2006) | 1) Public school systems 2) Georgia Department of Human Resources facilities for children with developmental disabilities 3) Pediatric hospitals and associated clinics 4) Diagnostic and evaluation centers 5) Select private clinicians NCHS intercensal population estimates (1996), Bureau of Census estimates (2000) |
Most recent psychometric test. In the absence of an IQ score and in the context of testing, a written statement by a psychometrist that a child’s intellectual functioning is within the range for severe or profound mental retardation is acceptable. Severity ICD9-CM: ID = IQ <70, mild ID–IQ = 50–70, moderate ID–IQ = 35–49, severe ID–IQ=20–34, profound ID—IQ = <20 |
Children 8 years of age in 1996 or 2000, who met the ID case definition and whose parent or legal guardian resided in 5 counties of metropolitan Atlanta during the respective surveillance year. | 1996: 15.5/1000—ID overall 19.1/1000—ID, males 11.8/1000—ID, females 10.0/1000—ID, mild 4.3/1000—ID, moderate-profound 2000: 12.0/1000—ID overall 14.0/1000—ID, males 9.9/1000—ID, females 7.3/1000—ID, mild 3.3/1000—ID, moderate-profound |
| Chapman et al. (2008) | 1) Public school records Birth certificates |
Florida Department of Education records— “IQ criteria associated [are] … consistent the levels of severity… so EMH, TMH, and PMH will be referred to as mild, moderate/severe, and profound mental retardation” | Sample of 12–14 year olds born in Florida from 1986–1988 and attending public schools from 1999–2000 | 21.8/1000—MR 17.3/1000—MR, mild 3.4/1000—MR, moderate-severe 1.0/1000—MR, profound |
| Van Naarden Braun et al. (2015) | 1) Public school systems 2) Georgia Department of Human Resources facilities for children with developmental disabilities 3) Pediatric hospitals and associated clinics 4) Diagnostic and evaluation centers 5) Select private clinicians National Center for Health Statistics (NCHS) intercensal population estimates for 1991-1996 and 2002–2008 and the NCHS bridged-race decennial population estimates for 2000 and 2010. |
ID is defined as an intelligence quotient (IQ) of sp ≤ 70 on the most recently administered test of intellectual ability. | Children 8 years of age from 1991–2010 | 2002: 13.1/1000—ID overall 16.5/1000—ID, males 9.6/1000—ID, females 7.9/1000—ID, mild 4.6/1000—ID, moderate to profound 2010: 13.6/1000—ID, overall 18.6/1000—ID, males 8.5/1000—ID, females 9.4/1000—ID, mild 3.8/1000—ID, moderate to profound 1991–2010 13.0/1000 ID, overall |
“Measures of nonverbal intelligence included the Performance Scale of the Wechsler Adult Intelligence Scale-Revised (WAIS-R) or Wechsler Intelligence Scale for Children-Revised (WISC-R) and the Merrill-Palmer Scale of Mental Tests (excluding the verbal items) for less-capable individuals. The Peabody Picture Vocabulary Test-R (PPVT-R: Form L) provided an estimate of single word receptive vocabulary. Standard scores from the WAIS-R or WISC-R and equivalents from the Merrill Palmer (converted from mental-age scores) were averaged with standard scores from the Peabody (converted from mental-age equivalents, where necessary) to provide a composite (verbal and nonverbal) IQ score” (p. 654)
“The broad algorithm required only one IDD service contact across all available data and time periods, the intermediate algorithm added the restriction of a minimum of two physician visits while the narrow algorithm added a further restriction that the time period be limited to 2006 onward.”
“The children who potentially had intellectual disability were traced by (a) register data (Hospital Discharge Register, Cause-of-Death Register, National Insurance and Medication Reimbursement Register); (b) hospital, family counseling center, and institutional records; (c) questionnaires filled in by the children themselves and/or parents on health and school achievement, at age 14 in the older cohort and at age 7 and 8 years in the younger cohort; and (d) by results of psychometric tests using children’s social security number.”
“The prevalence of intellectual disability is defined as the number of cases present at the end of the follow-up (June 30, 1977, for the cohort 1966; December 30, 1996, for the cohort 1985–1986) per 1,000 population alive.”
“The diagnosis of ID was not individually ascertained for the study population. Diagnoses were set in normal clinical practice.”
For prevalence estimates for individual years of age for the same population from the same data sources, see: Westerinen et al. (2014). “Age-specific prevalence of intellectual disability in Finland at the beginning of new millennium—multiple register method.”
“Case identification was based on studying files, people were not assessed in person. This was not feasible at the time of the study. The result thus found is not better than the quality of the files, but justified by the fact that we only included people for whom documentation of ID was available in the files. All people without documentation were included as uncertain cases in providing minimum and maximum numbers in extrapolating.”
Ibid.
“The Norwegian municipalities receive funding from the government in proportion to the number of people diagnosed as having ID.”
Possible locations of physician examination and diagnosis include child health centers, preliminary school assessments, assessment for special education and special admission rights for secondary school. “There may be reservations to diagnose ID for at least two reasons. Children with mild ID often have minor needs during adolescence and the medical professionals do not get involved in the educational issues.”
“Those registered ID cases can apply as welfare recipients who will receive living allowances or related welfare benefits from the government.”
Definitions of Intellectual and Developmental Disability
Definitions of “intellectual and developmental disability” varied. Following International Classification of Diseases (ICD) –10 criteria for those countries in which this version of ICD coding was used, intellectual disability was typically defined as having an intelligence quotient (IQ) of less than 70, with 50–69 as mild (coded F70), 35–49 as moderate (coded F71), 20–34 as severe (coded F72), and under 20 as profound (coded F73; Arvio & Sillanpaa, 2003; Bhasin, Brocksen, Avchen, & Van Naarden Braun, 2006; Lai, Tseng, Hou, & Guo, 2012; Kiani, Tyrer, Hodgson, Berkin, & Bhaumik, 2013; Leonard, Petterson, Bower, & Sanders, 2003; Patja, Iivanainen, Vesala, Oksanen, & Ruoppila, 2000; Petterson, Bourke, Leonard, Jacoby, & Bower, 2007; Petterson et al., 2005; Sondenaa, Rasmussen, Nottestad, & Lauvrud, 2010; Stromme & Hagberg, 2000; Van Naarden Braun et al., 2015; World Health Organization, 1996). Equivalent ICD-9 coding was used where ICD-10 had not yet been implemented within countries. Sometimes, but not always, developmental delay before age eighteen was also included within the case definition (Petterson et al., 2005; Petterson et al., 2007; Lin et al., 2013). Other definitions were based upon enrollment in administrative programs, but while criteria for eligibility likely took IQ and/or age at onset of condition into account, these criteria were not specifically identified and likely vary across programs and countries (Ng, Sandberg, & Ahlstrom, 2015; Ouellette-Kuntz et al., 2010; McConkey, Mulvany, & Barron, 2006). Terminology used for IDD varied, and included learning disability in England, adaptive functioning in Canada, intellectual impairment in Ireland, and mental retardation in France and Norway (see Table 1).
Methods Used to Identify IDD
Methods used to identify IDD included formal psychometric testing and sometimes retesting of intelligence and adaptive behaviors using practices that were similar even if their terminology was slightly different (Bhasin et al., 2006; Bradley, Thompson, & Bryson, 2002; Heikura et al., 2003; Heikura et al., 2005; Lai et al., 2012; Leonard et al., 2003; Petterson et al., 2007; Petterson et al., 2005; Stromme & Hagberg, 2000; Van Naarden Braun et al., 2015). Some used search mechanisms for specific clinically-assigned ICD-9, ICD-10, DSM-4, and International Classification of Primary Care (ICPC) codes for IDD diagnoses (Lin et al., 2013; Kiani et al., 2013; Morgan, Ahmed, & Kerr, 2000; van Schronjenstein Lantman-de Valk et al., 2006; Wullink, van Schrojenstein Lantman-de Valk, Dinant, & Metsemakers, 2007; Westerinen, Kaski, Virta, Almqvist, & Iivanainen, 2007; Westerinen, et al., 2007; Sondenaa et al., 2010); others used clinical assessment of intelligence (Arvio & Sillanpaa, 2003; Cans, Guillem, Fauconnier, Rambaud, & Jouk, 2003) or administrative classification for services eligibility or a combination of multiple methods (Ouellette-Kuntz et al., 2010; McGrother, Bhaumik, Thorp, Watson, & Taub, 2002; Lin, 2009; Ng et al., 2015). Working within educational milieux led others to employ what they referred to as educational assessments (Chapman, Scott, & Stanton-Chapman, 2008; Emerson, 2012; Emerson & Glover, 2012; Emerson et al., 2012; Kelly, Kelly, & O’donahoe, 2012; See Table 1).
Types of Numerator Data Sources
Both numerator types and number of sources were identified. Administrative data sources used to determine the numerator for IDD prevalence estimates included linked research databases, care-based registers of individuals with disabilities, educational censuses and education enrollment records, hospitalization abstracts and records, physician claims and records, and social service records. Examples of linked research databases used to estimate IDD prevalence include Western Australia’s Maternal and Child Health Research Data Base (Leonard et al., 2003), the Western Australia Intellectual Disability Database (Petterson et al., 2005; Petterson et al., 2007), Canada’s Manitoba Population Health Research Data Repository (Ouellette-Kuntz et al., 2010), and the U.S.’s Metropolitan Atlanta Developmental Disabilities Surveillance Program (Bhasin et al., 2006; Van Naarden Braun et al., 2015). National, local, and primary care-based registers of individuals with disabilities generally—or IDD specifically—were also used alone or in combination with other numerator data sources to identify IDD prevalence in England (Emerson & Glover, 2012; Emerson et al., 2012; Kiani et al., 2013; McGrother et al., 2002; McGrother, Thorp, Taub, & Machado, 2001), France (Cans et al., 2003), Ireland (Kelly et al., 2012; McConkey, et al. 2006), Sweden (Ng et al., 2015) and Taiwan (Lai et al., 2012). Other numerator data sources used included educational censuses and education enrollment and evaluation records (Bhasin et al., 2006; Bradley, et al. 2002; Chapman et al., 2008; David et al., 2014; Emerson, 2012; Emerson & Glover, 2012; Emerson et al., 2012; Leonard et al., 2003; Ouellette-Kuntz et al., 2010; Petterson et al., 2005; Petterson et al., 2007; Stromme & Hagberg, 2000; Van Naarden Braun et al., 2015), hospitalization abstracts and records (Heikura et al., 2003; Heikura et al., 2005; Lin et al., 2013; Morgan et al., 2000; Westerinen, Kaski, Virta, Almqvist, & Iivanainen, 2014; Westerinen et al., 2007), physician claims and medical care records (Bhasin et al., 2006; Lin et al., 2013; Ouellette-Kuntz et al., 2010; Van Naarden Braun et al., 2015; van Schrojenstein Lantman-de Valk et al., 2006; Wullink et al., 2007), and social service records, including disability service registrants and disability income support (Bradley, et al. 2002; David et al., 2014; Heikura et al., 2003; Heikura et al., 2005; Leonard et al., 2003; Ouellette-Kuntz et al., 2010; Petterson et al., 2005; Morgan et al., 2000; Ng et al., 2015; Westerinen et al., 2007; Westerinen et al., 2014; see Table 1).
Number of Numerator Data Sources
The number of numerator data sources employed to identify persons with IDD varied. Studies using only a single numerator data source to establish prevalence used school censuses in England (Emerson, 2012); national or local intellectual disability registers, as in England (Kiani et al., 2013; McGrother et al., 2002; McGrother et al., 2001); France (Cans et al., 2003), Ireland (Kelly et al., 2012); and Taiwan (Lai et al., 2012); and client registers, as in Finland (Arvio & Sillanpaa, 2003). In other articles, multiple numerator data sources were used to identify persons with IDD (see Table 1). When multiple data sources were used, they were sometimes from within the same sector, such as hospitalization abstracts and ambulatory care records (Lin et al., 2013), and sometimes from several sectors, such as health care, social services, and education (Bhasin et al., 2006; Bradley et al., 2002; Heikura et al., 2003; Heikura et al., 2005; Ouellette-Kuntz et al., 2010; Morgan et al., 2000; Ng et al., 2015; Westerinen et al., 2007; Westerinen et al., 2014; Van Naarden Braun et al., 2015). Estimating ID prevalence with multiple numerator data sources requires individual record linkage using either probabilistic linkage, as in Western Australia (Leonard et al., 2003) and South Glamorgan (United Kingdom [Wales]) (Morgan et al., 2000), or unique personal identifiers, as in Manitoba, Canada (Ouellette-Kuntz, 2010), and Finland (Westerinen et al., 2007; Westerinen et al., 2014). Linkage techniques were not always fully specified in the reviewed articles.
Types of Denominator Data Sources
The types of data sources used as denominators for estimating prevalence of intellectual and developmental disabilities from administrative data included population censuses, estimates, projections, and vital records, including birth registries, and certificates. Population denominators included national and subnational populations, age-specific populations (e.g., see Arvio & Sillanpaa, 2003; Bhasin et al., 2006; Bradley et al., 2002; Emerson & Glover, 2012; Heikura et al., 2003; Kelly et al., 2012; Kiani et al., 2013; Lai et al., 2010; Morgan et al., 2000; Patja et al., 2000; McConkey, Mulvany, & Barron, 2006; Ng et al., 2015; Sondenaa et al., 2010; van Schronjenstein Lantman de-Valk et al., 2006; Van Naarden Braun et al., 2015; Westerinen et al., 2007; Westerinen et al., 2014; Wullink et al., 2007) and live births (e.g., see Leonard et al., 2003; Petterson et al., 2005; Petterson et al., 2007).
Comparing Prevalence Estimates
Notwithstanding potential geographic variations between and within countries, the possibility of outmigration, mortality or study designs contributing to varying rates, differing definitions of denominator populations also limit the ability to compare IDD prevalence estimates from the selected studies (Van Naarden-Braun et al., 2013). For example, denominator populations included live births in 1983–1992 surviving to the end of 1999 (Leonard et al., 2003), live births in 1980–1999 surviving to one year (Petterson et al., 2007), persons aged 14–20 years (Bradley et al., 2002), persons aged 18–64 years (Lin et al., 2013), persons aged 55 and above (Ng et al., 2015), all persons (Ouellette-Kuntz et al., 2010), and school children aged 7–15 years (Emerson, 2012) and 5–15 years (Emerson & Glover, 2012). Among those studies using the entire population as the denominator, IDD prevalence estimates (per 1,000) were 3.7 in South Glamorgan, United Kingdom (Wales) (Morgan et al., 2000), 4.3 in Finland (Arvio & Sillanpaa, 2003), 4.4 in Norway (Sondenaa et al., 2010), 4.7 in Manitoba (Ouellette-Kuntz et al., 2010), 6.4–7.0 in the Netherlands (van Schrojenstein Lantman-de Valk et al., 2006), and 7.0 in Finland (Westerinen et al., 2007).
Discussion
Advantages of Administrative Data to Estimate IDD Prevalence
Using administrative data as a database to estimate IDD prevalence can provide both practical and methodological advantages. Practical advantages can include lower costs than adding IDD items to population-based surveys or censuses, more timely data, and ongoing data collection. Methodological advantages can include using multiple numerator data sources to estimate prevalence rather than relying upon a single data source (Bhasin et al., 2006; David et al., 2014; Van Naarden Braun et al., 2015; Westerinen et al., 2014), ability to analyze over-time prevalence trends, and the potential to investigate health care access and utilization, health conditions, and use of educational and social services for those with IDD (Lin et al., 2014). Our review did not specifically distinguish analyzing large administrative databases from using them for more detailed, active record reviews which can be used to construct episodes of illness or screen for comorbidities in people with IDD, but it is likely that at least some of the studies also employed this approach in their use of these data.
Limitations of Administrative Data to Estimate IDD Prevalence
Estimating IDD prevalence using administrative data sets includes several inherent limitations including differing purposes of data items collected, scope of populations covered by administrative data sets, completeness of case ascertainment, and consistency of IDD case definitions across data sets (Chapman et al., 2008). In addition, in the absence of in-person testing for ID, coding validity can be questioned.
IDD prevalence estimates derived from administrative data sets depend partially upon the specific data sets used as numerators (Leonard et al., 2003; Petterson et al., 2005). In the absence of validation studies comparing IDD prevalence estimates derived from administrative data sets to prevalence estimates derived from population-based surveys, population censuses, or population-based psychometric testing, authors speculate that IDD prevalence estimates based on administrative data may reflect under or, while less likely, over ascertainment of IDD, depending upon the particular administrative data set used at a particular time and place and the particular population studied. Multiple reasons may exist for under ascertainment of IDD in administrative data sets (Ho, 2004). For example, administrative data sets may not include people who do not use health, education, or social services (Fujiura & Rutkowski-Kmitta, 2001; McGrother et al., 2002; Whitaker 2004). Under ascertainment may also be differential, due to such causes as administrative biases and discrimination based upon ethnicity (Emerson & Hatton, 2004), fear of stigma leading to under enrollment in services (Ho, 2004), under enrollment of people with mild intellectual disabilities (Emerson, Felce, & Stancliffe, 2013; Fujuira, 2003; Maulik, Mascarenhas, Mathers, Dua, & Saxena, 2011; Morgan et al., 2000; Sondenaa et al., 2010; Westerinen et al., 2007), which may occur more in rural than urban areas (Ayoglu et al., 2008; Sondenaa et al, 2010); and under enrollment of individuals with IDD who are beyond school age (Emerson & Glover, 2012; Leonard & Wen, 2002; Petterson et al., 2005; Westerinen et al., 2014). This “transition cliff” (Emerson & Glover, 2012) is especially dominant in more moderate forms of IDD but less so where the condition is more severely or profoundly expressed. Presumably, this reflects the ability of young adults with less severe forms of IDD to integrate into society in ways that no longer are captured through routinely collected administrative data. Over ascertainment of IDD may also occur, if people who have died or moved from the geographic area of the denominator population are not removed from the numerator data sets (Leonard & Wen, 2002) or if persons may be identified based upon seeking assessment who may not be actually diagnosed.
Comparing prevalence estimates from multiple administrative data sets, across multiple studies, and across countries or local areas can also be problematic. As indicated above, prevalence estimates can be affected by multiple conceptual and operational factors that may vary across administrative data sets (Emerson & McGrother, 2011), the sectors managing those administrative data sets, and countries. Numerator-related issues affecting comparability of prevalence estimates may include case ascertainment (Sondenaa et al., 2010), case definition (Leonard et al., 2003), and population characteristics (Van Naarden Braun & Yeargin-Allsopp, 2009; van Schrojenstien-Lantman de Valk, 2005), all of which may vary across administrative data sets and even within the same study. The cross-cultural validity of case ascertainment may also be questionable (Emerson & Hatton, 2004). Accuracy of coding may also vary across data sets and across time even within the same data set, and even within the same study (Emerson et al., 2013; Morgan et al., 2000). Denominator-related issues affecting comparability of prevalence estimates may include age distributions, ethnicity, differential migration and/or mortality, and other population characteristics (Emerson & Hatton, 2004; Van Naarden Braun & Yeargin-Allsopp, 2009). Finally, generic issues with administrative data of all types may also affect comparability of prevalence estimates (Glasson & Hussain, 2008; Iezzoni, 2002; Iezzoni et al., 2005). These generic issues can include lack of quality assurance in administrative data, movement from paper to electronic storage, and the inherent limitations of estimating ID prevalence using data collected for administrative purposes.
Promising Practices in Use of Administrative Data to Estimate IDD Prevalence
Despite the actual and potential problems that may affect the accuracy and comparability of IDD prevalence estimates derived from administrative data, promising practices using criteria earlier described in the Methods section exist that can be identified, analyzed, and applied to the use of administrative data to estimate IDD prevalence, as identified in Table 2.
TABLE 2.
Examples of promising practices in literature using administrative data for estimating prevalence of intellectual disabilities, by country, 2000–2015
| Country and citation | Number of numerator data sourcesa | Linkageb | Unique identifierc | Demographic detaild | Ongoing researche |
|---|---|---|---|---|---|
| Australia | |||||
| Leonard et al. (2003) “Prevalence of intellectual disability in Western Australia” | 3 (disability services-1, education-2) | Yes | No | Yes (age, sex, race, urban/rural) | Yes (Maternal and Child Health Research Data Base, Intellectual Disability Exploring Answers) |
| Canada | |||||
| Ouellette-Kuntz et al. (2010) “Estimating administrative prevalence of intellectual disabilities in Manitoba” | 4 (healthcare-2, education-1, social services-1) | Yes | Yes (provincial Personal Health Identifier Number) | Yes (age) | Yes (Manitoba Population Health Research Data Repository) |
| Finland | |||||
| Heikura et al. (2003) “Temporal changes in incidence and prevalence of intellectual disability between two birth cohorts in northern Finland” | 4 (healthcare-2, social services-1, interviews-1) | Not specified | Not specified | Yes (sex) | Yes (two birth cohorts, separated by 20 years) |
| Westerinen et al. (2007) “Prevalence of intellectual disability: a comprehensive study based on national registers” | 8 (social services-7, healthcare-1) | Yes | Yes (national Social Security Code) | Yes (age, sex) | Yes (national registers) |
| Netherlands | |||||
| van Schrojenstein Lantman-de Valk et al. (2006) “The prevalence of intellectual disability in Limburg, the Netherlands” & Wullink et al. (2007) “Prevalence of people with intellectual disability in the Netherlands” | 4 (social services- 3, healthcare-1) | Not specified | Not specified | Yes (age, sex) | No |
| United States | |||||
| Bhasin et al. (2006) “Prevalence of four developmental disabilities among children aged 8 years—Metropolitan Atlanta Developmental Disabilities Surveillance Program, 1996 and 2000” & Van Naaden Braun et al. (2015) | 6 (education-2, social services-1, healthcare-3) | Yes | No | Yes (sex, race, socioeconomic status, birth characteristics) | Yes (Metropolitan Atlanta Developmental Disabilities Surveillance Program) |
Total number of data sources (number of data sources by type).
Linkage of numerator data sources to estimate prevalence.
Unique personal identifier used for linkage.
Prevalence estimates provided for demographic subgroups.
Research based on ongoing program.
Using multiple administrative data sources to estimate prevalence, especially when those data sources are drawn from more than one sector, may improve prevalence estimates (Lin et al., 2014). Analyzing the number of cases uniquely ascertained through each data source, when more than one numerator data source is employed in an individual study, may prove helpful for later research (Bhasin et al., 2006; David et al., 2014; Van Naarden Braun et al., 2015; Westerinen et al., 2014). Linkage of multiple numerator data sources through a unique personal identifier number (Ouellette-Kuntz et al., 2010), such as a health insurance number or a social security number (Westerinen et al., 2007), is optimal. When linkage through a unique personal identifier is not feasible, well-documented probabilistic linkage is also promising (Leonard et al., 2003; Petterson et al., 2005). Presenting IDD prevalence estimates for each of the four standard ICD-10 categories (mild, moderate, severe, and profound) in addition to total IDD prevalence is helpful, as are IDD prevalence estimates by sex (Bhasin et al., 2006; Heikura et al., 2003; Leonard et al., 2003; Ouellette-Kuntz et al., 2010; Van Naarden Braun et al., 2015; Westerinen et al., 2007). These factors are especially important given transition issues in which prevalence appears influenced by severity as persons with IDD age. For this and other reasons that include resource allocation, IDD prevalence estimates by age are also helpful but would be more so if studies employed the same age categories. Extrapolation techniques appear appropriate when systematically applied (van Schrojenstein Lantman-de Valk et al., 2006; Wullink et al., 2007). When these estimates from local to national populations occur, use of more than one extrapolation method is even more desirable (Wullink et al., 2007) as a means of strengthening validity.
Regardless of the specific methods employed in estimating IDD prevalence using administrative data, clear and complete information about data sources, case ascertainment, case definitions, and other methods as described in publications are frequently lacking (Maulik et al., 2011). Research programs that are ongoing and supported by host institutions may be able to employ one or more of these promising practices discussed above when estimating IDD prevalence using administrative data, including programs such as Western Australia’s Maternal and Child Health Research Data Base (Leonard et al., 2003; Leonard et al., 2005) and Intellectual Disability Exploring Answers (IDEA) database (Petterson et al., 2005), the Manitoba Population Health Research Data Repository (Ouellette-Kuntz et al., 2010), and the Metropolitan Atlanta Disabilities Surveillance Program (Bhasin et al., 2006; Van Naarden Braun et al., 2015).
Efforts to use administrative data for estimating IDD prevalence can be strengthened further through systematically increasing the comparability of methods and reporting across data sets, time, and nations. Examples of international cooperation to increase comparability of disability measurement include the Washington Data Group’s efforts to improve overall disability measurement (Altman, 2006; Hendershot, 2006) and the Surveillance of Cerebral Palsy Europe Network’s efforts to improve cerebral palsy measurement (Bakel et al., 2014). Although not specific to IDD, these examples of cooperation might be adapted to increase the comparability across countries of IDD prevalence estimates derived from administrative data. International efforts to increase comparability should focus especially on adopting comparable case definitions, based on ICD-10, International Classification of Functioning, Disability and Health (ICF) or other replicable, widely understood and accepted case ascertainment methods.
International cooperation is also needed to develop and implement suggested guidelines to increase comparability of publication norms using administrative data to estimate IDD prevalence. Such publication norms could be implemented by relevant journals, possibly beginning with those produced by the same publisher, and could start with clear reporting of the purpose for which the administrative data used to estimate IDD prevalence were collected, along with assumptions behind using the data set to estimate IDD prevalence (Fujiura, 2003; Glasson & Husssain, 2008; van Schrojenstein Lantman-de Valk, 2005; Whitaker, 2004). Suggested guidelines could also include clear statements of IDD case definitions and case ascertainment practices (Glasson & Hussain, 2008). These reporting guidelines could require clear descriptions of each numerator data set; each denominator data set together with explanations of whether denominators are based on population counts, off-year census estimates, or projections; presence or absence of linkage and linkage techniques and results; and formulae or algorithms for estimating prevalence.
Conclusion
In summary, a review of the use of administrative data in 12 countries reveals both the challenges and potential promise of using these data sources to expand our ability to estimate prevalence for IDD populations. Practices used in estimating prevalence in five of these countries, building on the ability to link administrative data sets through unique person identifiers, appear to be the most promising from which other countries can learn and build upon. While not without its own set of challenges, the use of administrative data to estimate prevalence for IDD populations offers a potentially viable, feasible alternative to survey methodologies that may use approaches that are becoming increasingly difficult to conduct as case definition, phone use, security, and privacy issues continue to evolve in addition to existing challenges of parental or guardian report.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This count includes a report from Ireland (Kelly et al., 2012) and a report from England (Emerson et al., 2012), both identified through citation trails.
References
- Altman BM. The Washington Group: Origin and purpose. In: Altman BM, Barnartt SN, editors. International views on disability measures: Moving toward comparative measurement. Oxford: Elsevier; 2006. pp. 9–16. [Google Scholar]
- American Association of Intellectual and Developmental Disabilities (AAIDD) 2016 Retrieved from https://aaidd.org/intellectual-disability/definition/faqs-on-intellectual-disability#.WED8JflLMv6 (November 27, 2016)
- Arvio M, Sillanpaa M. Prevalence, etiology and comorbidity of severe and profound intellectual disability in Finland. Journal of Intellectual Disability Research. 2003;47:108–112. doi: 10.1046/j.1365-2788.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- Ayoglu FN, Cabuk F, Kiran S, Ocakci A, Sahin Z, Dursun A. The prevalence of mental retardation by gender, age of diagnosis and location in Zonguldak province, Turkey. Neurosciences. 2008;13:57–60. [PubMed] [Google Scholar]
- Bakel M, Einarsson I, Arnaud C, Craig S, Michelsen SI, Pildava S, Cans C. Monitoring the prevalence of severe intellectual disability in children across Europe: Feasibility of a common database. Developmental Medicine & Child Neurology. 2014;56:361–369. doi: 10.1111/dmcn.12281. [DOI] [PubMed] [Google Scholar]
- Bhasin TK, Brocksen S, Avchen RN, Van Naarden Braun K. Prevalence of four developmental disabilities among children aged 8 years — Metropolitan Atlanta Developmental Disabilities Surveillance Program, 1996 and 2000. Morbidity and Mortality Weekly Report Surveillance Summaries. 2006;55(1):1–9. [PubMed] [Google Scholar]
- Bradley EA, Thompson A, Bryson SE. Mental retardation in teenagers: Prevalence data from the Niagara region, Ontario. Canadian Journal of Psychiatry. 2002;47:652–659. doi: 10.1177/070674370204700707. [DOI] [PubMed] [Google Scholar]
- Brault MW. Current population reports. Washington, DC: U.S. Census Bureau; 2012. Americans With Disabilities: 2010; pp. 70–131. [Google Scholar]
- Cans C, Guillem P, Fauconnier J, Rambaud P, Jouk PS. Disabilities and trends over time in a French county, 1980-91. Archives of Disability in Childhood. 2003;88:114–117. doi: 10.1136/adc.88.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DA, Scott KG, Stanton-Chapman TL. Public health approach to the study of mental retardation. American Journal on Mental Retardation. 2008;113:102–116. doi: 10.1352/0895-8017(2008)113[102:PHATTS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- David M, Dieterich K, Billette de Villemeur A, Jouk PS, Counillon J, Larroque B, Cans C. Prevalence and characteristics of children with mild intellectual disability in a French county. Journal of Intellectual Disability Research. 2014;58:591–602. doi: 10.1111/jir.12057. [DOI] [PubMed] [Google Scholar]
- Emerson E. Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. Journal of Epidemiology and Community Health. 2012;66:218–224. doi: 10.1136/jech.2010.111773. [DOI] [PubMed] [Google Scholar]
- Emerson E, Felce D, Stancliffe RJ. Issues concerning self-report data and population-based data sets involving people with intellectual disabilities. Intellectual and Developmental Disabilities. 2013;51:333–348. doi: 10.1352/1934-9556-51.5.333. [DOI] [PubMed] [Google Scholar]
- Emerson E, Glover G. The “transition cliff” in the administrative prevalence of learning disabilities in England. Tizard Learning Disability Review. 2012;17:139–143. [Google Scholar]
- Emerson E, Hatton C. Response to McGrother et al. Journal of Intellectual Disability Research. 2004;46:299–309. doi: 10.1111/j.1365-2788.2004.00501.x. The prevalence of intellectual disability among South Asian communities in the UK. Journal of Intellectual Disability Research, 48, 201-202. [DOI] [PubMed] [Google Scholar]
- Emerson E, Hatton C, Robertson J, Roberts H, Baines S, Evison F, Glover G. People with learning disabilities in England 2011. Public Health England report. Improving Health and Lives (IHAL) 2012 Available at http://www.improvinghealthandlives.org.uk/publications/1063/People_with_Learning_Disabilities_in_England_2011.
- Emerson E, McGrother C. The use of pooled data from learning disabilities registers: A scoping review. Improving Health and Lives (IHAL): Learning Disabilities Observatory, Department of Health. 2011 Available at http://www.nepho.org.uk/uploads/doc/vid_9057_IHAL2011-01Registers.pdf.
- Fujiura GT. Continuum of intellectual disability: demographic evidence for the “forgotten generation”. Mental Retardation. 2003;41:420–429. doi: 10.1352/0047-6765(2003)41<420:COIDDE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Fujiura GT, Rutkowski-Kmitta V. Counting disability. In: Albrecht G, Seelman K, Bury M, editors. Handbook of disability studies. Thousand Oaks, CA: Sage; 2001. pp. 69–96. [Google Scholar]
- Glasson EJ, Hussain R. Linked data: Opportunities and challenges in disability research. Journal of Intellectual and Developmental Disability. 2008;33:285–291. doi: 10.1080/13668250802441409. [DOI] [PubMed] [Google Scholar]
- Heikura U, Linna SL, Olsén P, Hartikainen AL, Taanila A, Järvelin MR. Etiological survey on intellectual disability in the northern Finland birth cohort 1986. American Journal on Mental Retardation. 2005;110:171–180. doi: 10.1352/0895-8017(2005)110<171:ESOIDI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Heikura U, Taanila A, Olsen P, Hartikainen AL, von Wendt L, Järvelin MR. Temporal changes in incidence and prevalence of intellectual disability between two birth cohorts in northern Finland. American Journal on Mental Retardation. 2003;108:19–31. doi: 10.1352/0895-8017(2003)108<0019:TCIIAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hendershot GE. Survey measurement of disability: A review of international activities and recommendations. In: Altman BM, Barnartt SN, editors. International views on disability measures: moving toward comparative measurement. Oxford: Elsevier; 2006. pp. 17–40. [Google Scholar]
- Ho A. To be labelled, or not to be labelled: That is the question. British Journal of Learning Disabilities. 2004;32:86–92. [Google Scholar]
- Iezzoni LI. Using administrative data to study persons with disabilities. Milbank Quarterly. 2002;80:347–379. doi: 10.1111/1468-0009.t01-1-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI, Schwartz M, Ash AS. Administrative health data. In: Friedman DJ, Hunter EL, Parrish RG, editors. Health statistics: shaping policy and practice to improve the population’s health. Oxford: Oxford University Press; 2005. pp. 139–160. [Google Scholar]
- Institute of Medicine. The future of disability in America. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- Kelly F, Kelly C, O’Donahoe A. Annual report of the national intellectual disability database committee 2012. Dublin, IR: Health Research Board; 2012. [Google Scholar]
- Kiani R, Tyrer F, Hodgson A, Berkin N, Bhaumik S. Urban-rural differences in the nature and prevalence of mental ill-health in adults with intellectual disabilities. Journal of Intellectual Disability Research. 2013;57:119–127. doi: 10.1111/j.1365-2788.2011.01523.x. [DOI] [PubMed] [Google Scholar]
- Krahn GL, Fox MH, Campbell VA, Ramon I, Jesien G. Developing a health surveillance system for people with intellectual disabilities in the United States. Journal of Policy and Practice in Intellectual Disabilities. 2010;7:155–166. [Google Scholar]
- Lai DC, Tseng YC, Hou YM, Guo HR. Gender and geographic differences in the prevalence of intellectual disability in children: Analysis of data from the national disability registry of Taiwan. Research in Developmental Disabilities. 2012;33:2301–2307. doi: 10.1016/j.ridd.2012.07.001. [DOI] [PubMed] [Google Scholar]
- Larson SA, Lakin KC, Anderson L, Kwak Lee N, Anderson D. Prevalence of mental retardation and developmental disabilities: Estimates from the 1994/1995 national health interview survey disability supplements. American Journal of Mental Retardation. 2001;106:231–252. doi: 10.1352/0895-8017(2001)106<0231:POMRAD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Leonard H, Petterson B, Bower C, Sanders R. Prevalence of intellectual disability in Western Australia. Paediatric and Perinatal Epidemiology. 2003;17:58–67. doi: 10.1046/j.1365-3016.2003.00469.x. [DOI] [PubMed] [Google Scholar]
- Leonard H, Petterson B, De Klerk N, Zubrick SR, Glasson E, Sanders R, Bower C. Association of sociodemographic characteristics of children with intellectual disability in Western Australia. Social Science & Medicine. 2005;60:1499–1513. doi: 10.1016/j.socscimed.2004.08.014. [DOI] [PubMed] [Google Scholar]
- Leonard H, Wen X. The epidemiology of mental retardation: Challenges and opportunities in the new millennium. Mental Retardation and Developmental Disabilities Research Reviews. 2002;8:117–134. doi: 10.1002/mrdd.10031. [DOI] [PubMed] [Google Scholar]
- Lin E, Balogh R, Cobigo V, Ouellette-Kuntz H, Wilton AS, Lunsky Y. Using administrative health data to identify individuals with intellectual and developmental disabilities: A comparison of algorithms. Journal of Intellectual Disability Research. 2013;57:462–477. doi: 10.1111/jir.12002. [DOI] [PubMed] [Google Scholar]
- Lin E, Balogh R, Isaacs B, Ouellette-Kuntz H, Selick A, Wilton AS, Lunsky Y. Strengths and limitations of health and disability support administrative databases for population-based health research in intellectual and developmental disabilities. Journal of Policy and Practice in Intellectual Disabilities. 2014;11:235–244. [Google Scholar]
- Lin JD. Population with intellectual disability based on 2000-2007 national registers in Taiwan: Age and gender. Research in Developmental Disabilities. 2009;30:294–300. doi: 10.1016/j.ridd.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: A meta-analysis of population-based studies. Research in Developmental Disabilities. 2011;32:419–436. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- McConkey R, Mulvany F, Barron S. Adult persons with intellectual disabilities on the island of Ireland. Journal of Intellectual Disability Research. 2006;50:227–236. doi: 10.1111/j.1365-2788.2005.00777.x. [DOI] [PubMed] [Google Scholar]
- McGrother CW, Bhaumik S, Thorp CF, Watson JM, Taub NA. Prevalence, morbidity and service need among South Asian and white adults with intellectual disability in Leicestershire, UK. Journal of Intellectual Disability Research. 2002;46:299–309. doi: 10.1046/j.1365-2788.2002.00391.x. [DOI] [PubMed] [Google Scholar]
- McGrother C, Thorp C, Taub N, Machado O. Prevalence, disability and need in adults with severe learning disability. Tizard Learning Disability Review. 2001;6:4–13. [Google Scholar]
- Mont D. SP discussion paper no 0706. Washington, DC: The World Bank; 2007. Monitoring disability prevalence. [Google Scholar]
- Morgan CL, Ahmed Z, Kerr MP. Health care provision for people with a learning disability record-linkage study of epidemiology and factors contributing to hospital care uptake. The British Journal of Psychiatry. 2000;176:37–41. doi: 10.1192/bjp.176.1.37. [DOI] [PubMed] [Google Scholar]
- Ng N, Sandberg M, Ahlstrom G. Prevalence of older people with intellectual disability in Sweden: A spatial epidemiological analysis. Journal of Intellectual Disability Research. 2015;59:1155–1167. doi: 10.1111/jir.12219. [DOI] [PubMed] [Google Scholar]
- Ouellette-Kuntz H, Shooshtari S, Temple B, Brownell M, Burchill C, Yu CT, Hennen B. Estimating administrative prevalence of intellectual disabilities in Manitoba. Journal on Developmental Disabilities. 2010;15:69–80. [Google Scholar]
- Patja K, Iivanainen M, Vesala H, Oksanen H, Ruoppila I. Life expectancy of people with intellectual disability: A 35-year follow-up study. Journal of Intellectual Disability Research. 2000;44:591–599. doi: 10.1046/j.1365-2788.2000.00280.x. [DOI] [PubMed] [Google Scholar]
- Petterson B, Leonard H, Bourke J, Sanders R, Chalmers R, Jacoby P, Bower C. IDEA (Intellectual Disability Exploring Answers): A population-based database for intellectual disability in Western Australia. Annals of Human Biology. 2005;32:37–43. doi: 10.1080/03014460500075035. [DOI] [PubMed] [Google Scholar]
- Petterson B, Bourke J, Leonard H, Jacoby P, Bower C. Cooccurrence of birth defects and intellectual disability. Paediatric and Perinatal Epidemiology. 2007;21:65–75. doi: 10.1111/j.1365-3016.2007.00774.x. [DOI] [PubMed] [Google Scholar]
- Salvador-Carulla L, Reed GM, Vaez-Azizi LM, Cooper SA, Martinez-Leal R, Bertelli M, Luckasson R. A systematic approach to subgroup classification in intellectual disability. Intellectual and Developmental Disabilities. 2015;53:358–366. doi: 10.1352/1934-9556-53.5.358. [DOI] [PubMed] [Google Scholar]
- Søndenaa E, Rasmussen K, Nøttestad JA, Lauvrud C. Prevalence of intellectual disabilities in Norway: Domestic variance. Journal of Intellectual Disability Research. 2010;54:161–167. doi: 10.1111/j.1365-2788.2009.01230.x. [DOI] [PubMed] [Google Scholar]
- Strømme P, Hagberg G. Aetiology in severe and mild mental retardation: A population-based study of Norwegian children. Developmental Medicine & Child Neurology. 2000;42:76–86. doi: 10.1017/s0012162200000165. [DOI] [PubMed] [Google Scholar]
- Tassé MJ, Luckasson R, Nygren M. AAIDD Proposed recommendations for ICD–11 and the condition previously known as mental retardation. Intellectual and Developmental Disabilities. 2013;51:127–131. doi: 10.1352/1934-9556-51.2.127. [DOI] [PubMed] [Google Scholar]
- Thacker SB, Qualters JR, Lee LM. Public health surveillance in the United States: Evolution and challenges. Morbidity and Mortality Weekly Report. 2012;61(Suppl):3–9. [PubMed] [Google Scholar]
- Van Naarden Braun K, Yeargin-Allsopp M. Epidemiology of intellectual disabilities. In: Levene M, Chervenak F, editors. Fetal and neonatal neurology and neurosurgery. London: Elsevier; 2009. pp. 876–897. [Google Scholar]
- Van Naarden Braun K, Christensen D, Doernberg N, Schieve L, Rice C, Wiggins L, Yaergin-Allsopp M. Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan Atlanta, 1991-2010. PLoS One. 2015;10:e0124120. doi: 10.1371/journal.pone.0124120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Schrojenstein Lantman-de Valk HMJ. Health in people with intellectual disabilities: Current knowledge and gaps in knowledge. Journal of Applied Research in Intellectual Disabilities. 2005;18:325–333. [Google Scholar]
- van Schrojenstein Lantman-de Valk HMJ, Wullink M, van den Akker M, van Heurn-Nijsten EWA, Metsemakers JFM, Dinant GJ. The prevalence of intellectual disability in Limburg, The Netherlands. Journal of Intellectual Disability Research. 2006;50:61–68. doi: 10.1111/j.1365-2788.2005.00733.x. [DOI] [PubMed] [Google Scholar]
- Westerinen H, Kaski M, Virta L, Almqvist F, Iivanainen M. Prevalence of intellectual disability: A comprehensive study based on national registers. Journal of Intellectual Disability Research. 2007;51:715–725. doi: 10.1111/j.1365-2788.2007.00970.x. [DOI] [PubMed] [Google Scholar]
- Westerinen H, Kaski M, Virta LJ, Almqvist F, Iivanainen M. Age-specific prevalence of intellectual disability in Finland at the beginning of new millennium – Multiple register method. Journal of Intellectual Disability Research. 2014;58:285–295. doi: 10.1111/jir.12017. [DOI] [PubMed] [Google Scholar]
- Whitaker S. Hidden learning disability. British Journal of Learning Disabilities. 2004;32:139–143. [Google Scholar]
- World Health Organization. ICD-10 guide for mental retardation. Geneva, Switzerland: Author; 1996. [Google Scholar]
- World Health Organization. World report on disability. Geneva, Switzerland: Author; 2011. Retrieved from http://whqlibdoc.who.int/publications/2011/9789240685215_eng.pdf. [Google Scholar]
- Wullink M, van Schrojenstein Lantman-de Valk HMJ, Dinant G, Metsemakers JFM. Prevalence of people with intellectual disability in The Netherlands. Journal of Intellectual Disability Research. 2007;51:511–519. doi: 10.1111/j.1365-2788.2006.00917.x. [DOI] [PubMed] [Google Scholar]


