ABSTRACT
Thiamine (vitamin B1) is an essential vitamin found in most food products in developed nations. Deficiencies in this crucial vitamin lead to diseases related to nutritional needs, metabolic demands, enzymatic function, and neurological inflammation. We present an 18-year-old patient with a history of nasopharyngeal carcinoma and total parenteral nutrition (TPN) dependence who experienced neurological manifestations and heart failure, likely due to underlying thiamine deficiency, dehydration, and vasodilation. The patient exhibited heart failure due to thiamine deficiency that was overlooked by her care team secondary to a reaction to preservatives associated with vitamins in TPN, lapse in communication, and decreased compliance.
KEYWORDS: Myocardial ischemia, thiamine deficiency, total parenteral nutrition, vitamin B1
Thiamine (vitamin B1) is an essential vitamin found in most food products in developed nations. Functioning as an important cofactor for amino acid and carbohydrate metabolism, thiamine serves as a catalyst for the conversion of pyruvate to acetyl coenzyme A. Thiamine has a half-life of 10 to 20 days.1 Thiamine deficiency causes disease related to nutritional needs, metabolic demands, enzymatic function, and neurological inflammation. Deficiencies in this crucial vitamin are observed in alcoholism, malnourishment, malignancy, hyperemesis, and Crohn's disease.2 Lack of thiamine leads to the inability of mitochondria to undergo aerobic metabolism, leading to a buildup of pyruvate that is converted to lactate, which leads to lactic acidosis.3 The objective of this report is to increase awareness of vitamin deficiency, especially thiamine, in total parental nutrition (TPN)-dependent patients, even during claims of adequate oral intake.
CASE REPORT
An 18-year-old woman with a history of nasopharyngeal carcinoma, as well as chemotherapy and radiation that had been completed 2 months previously, was transferred to the pediatric intensive care unit from the floor due to depressed left ventricular function seen on echocardiogram. She presented with vomiting, dyspnea, tachycardia, numbness, and tingling down her left arm and bilateral legs. The patient also complained of occasional abdominal discomfort and dizziness. She had recently lost 26 pounds due to decreased appetite and oral aversion following her cancer treatments. The patient had been receiving TPN 8 hours each evening in replacement of oral nutrition. She had an allergic reaction 3 months prior to the preservatives within the TPN related to vitamin supplementation. Consequently, the vitamins were removed and the patient was instructed to take a multivitamin daily by mouth.
Due to persistent tachycardia during admission, an echocardiogram was obtained, which showed moderately depressed left ventricle function. She was placed on a milrinone drip. Radiography was normal. Shortly after starting the milrinone drip, the patient began complaining of severe epigastric pain, which was unresponsive to morphine and diphenhydramine. She developed progressive hypotension with widening pulse pressure and ST changes noted on telemetry (Figure 1). The milrinone drip was decreased and the patient was given 5% albumin for volume resuscitation with mild improvement. She also began to have intermittent changes in mental status, she was unable to consistently answer questions, and her eyes wandered during apparent lucid intervals. Her labs demonstrated development of a significant metabolic acidosis with a lactic acid of 9.5 mmol/L. She was given bicarbonate, an additional 5% albumin infusion, and calcium gluconate due to persistent hypotension. Milrinone was discontinued and the patient's abdominal pain resolved. Dobutamine was added at 5 mcg/kg/min with some blood pressure improvement. A femoral central catheter was placed for central venous pressure monitoring and secure administration of vasoactive medications.
Figure 1.
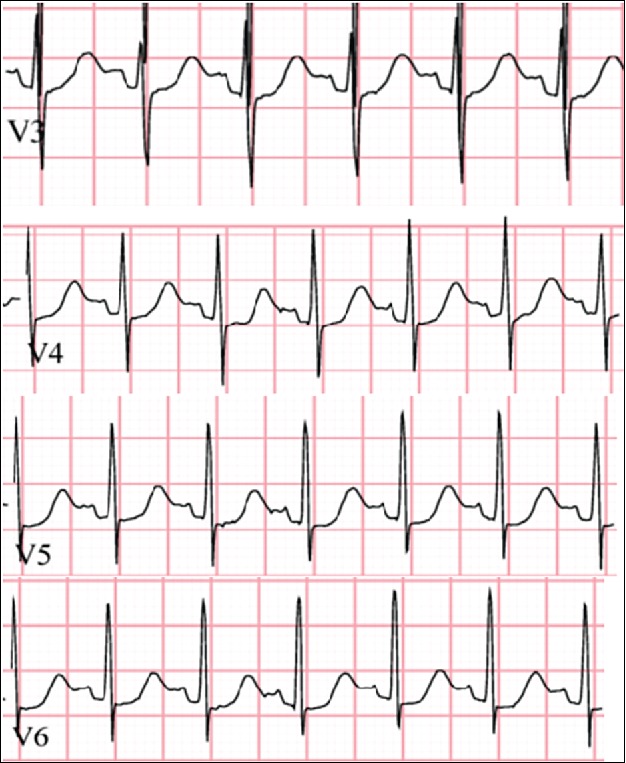
Patient's electrocardiogram following acute heart failure showing ST depression.
Overnight, the patient's blood pressure improved but remained marginal with addition of a modest dopamine infusion. Her central venous pressure remained between 6 and 8 mm Hg, electrolytes were stable, and acidosis improved. Electrocardiogram findings disclosed ST depression in the lateral leads (Figure 1). Repeat labs (creatinine at 1.64 mg/dL, blood urea nitrogen of 52 mg/dL, hemoglobin dropped to 7.0 g/dL, platelets dropped to 75×109) showed deterioration of renal function as well as worsening anemia and persistent thrombocytopenia. Urine output was minimal. The patient was transfused with packed red blood cells. Follow-up labs revealed a thiamine level of 33 pg/mL, well below assay, and peak troponin at 19 ng/mL. She had not taken her oral medications for 3 months. She was diagnosed with acute decompensated heart failure secondary to dehydration and thiamine deficiency.
Heart catheterization showed no chronic signs of coronary artery disease, and an echocardiogram 2 weeks later showed improved function with an ejection fraction around 60%. The patient's brain natriuretic peptide improved and she continued receiving daily thiamine infusions. A gastrostomy-jejunostomy tube was placed to ensure proper enteral nutrition and to avoid further complications.
DISCUSSION
Thiamine deficiency is associated with beriberi (dry and wet), Wernicke-Korsakoff syndrome, and Leigh's syndrome. Wernicke encephalopathy describes the common neurologic symptoms associated with thiamine deficiency, including nystagmus, ophthalmoplegia, ataxia, and confusion. Korsakoff's syndrome describes the chronic neurological condition associated with Wernicke encephalopathy.2
Hematological derangements may also be seen in thiamine deficiency, including neutropenia, thrombocytopenia, and anemia. This finding suggests that regulation of hematopoiesis at the stem cell level may be dependent on thiamine levels as well.4
Multiple case reports of vitamin deficiencies occurring in TPN-dependent patients have been recently published. The first case of thiamine deficiency during TPN was reported in 1985, followed by reports in the mid-1990s during a vitamin shortage.5,6 In 2014, 2 years after the American Society of Parenteral and Enteral Nutrition provided recommendations for management of TPN during multivitamin shortages, a case report presenting a 16-year-old patient with refractory lactic acidosis and multiorgan failure due to thiamine-deficient TPN was published.5,7 The importance of receiving adequate vitamin levels, especially daily thiamine (Table 1), must be stressed among patients and providers in order to prevent similar future occurrences.
Table 1.
Thiamine replacement recommendations
| Critically ill | Recommended daily intake |
|---|---|
| Intravenous or intramuscular 10–25 mg/dose/day OR per oral 10–50 mg/dose/day for 2 weeks followed by per oral 5–10 mg/dose/day for 1 month | 0.2–1.2 mg/day depending on age and sex |
ACKNOWLEDGMENTS
We thank Adam Stephens for his thoughtful manuscript review.
References
- 1.Abdou E, Hazell A. Thiamine deficiency: an update on pathophysiologic mechanisms and future therapeutic considerations. Neurochem Res. 2015;40:353–361. doi: 10.1007/s11064-014-1430-z. [DOI] [PubMed] [Google Scholar]
- 2.Ramsi M, Mowbray C, Hartman G, Pageler N. Severe lactic acidosis and multiorgan failure due to thiamine deficiency during total parenteral nutrition. BMJ Case Rep. 2014:bcr2014205264. doi: 10.1136/bcr-2014-205264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renthal W, Marin-Valencia I, Evans P. Thiamine deficiency secondary to anorexia nervosa: an uncommon cause of peripheral neuropathy and Wernicke encephalopathy in adolescence. Pediatr Neurol. 2014;51:100–103. doi: 10.1016/j.pediatrneurol.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 4.Velez R, Myers B, Guber M.. Severe acute metabolic acidosis (acute beriberi): an avoidable complication of total parenteral nutrition. JPEN J Parenter Enteral Nutr. 1985;9:216–219. doi: 10.1177/0148607185009002216. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Lactic acidosis traced to thiamine deficiency related to nationwide shortage of multivitamins for total parenteral nutrition. MMWR Morb Mortal Wkly Rep. 1997;45:523–528. [PubMed] [Google Scholar]
- 6.American Society of Parenteral and Enteral Nutrition Multivitamin shortage plan. 2012. Available at: http://www.nutritioncare.org. Accessed October 30, 2017. [Google Scholar]
- 7.Bazarbachi A, Muakkit S, Ayas M, et al.. Thiamine-responsive myelodysplasia. Br J Haematol. 1998;102:1098–1100. doi: 10.1046/j.1365-2141.1998.00861.x. [DOI] [PubMed] [Google Scholar]


