ABSTRACT
Intracytoplasmic green granules in neutrophils have been the subject of conjecture and discussion. Sometimes nicknamed “death cells,” these granules are often associated with severe liver disease and have been said to predict acute bad outcomes in severely ill patients. Some recommend that the laboratory community report these granules to treating clinicians as an indication of poor prognosis. We report two patients presenting with secondary liver disease who were found to have blue-green neutrophilic inclusions on the peripheral blood smear. One patient died, while the other patient recovered. We propose that this morphologic finding is likely transient and is related to liver disease and that recovery is possible. Additionally, prognosis in intensive care units continues to be determined by a number of variables, such as age, comorbidities, and severity of illness.
KEYWORDS: Granules, green granules, WBC granules, WBC inclusions
Within the past year, we have noted in our facility and in publications patients who present with intracytoplasmic green granules in the neutrophils and monocytes on peripheral blood smear (Figure 1). These granules are composed of lipopigments. The composition of these inclusions can vary between cell types, but all forms are undegradable because of aldehydes that cross-link peptides and form an indestructible plastic-like substance.1 These granules or inclusions are believed to be composed of approximately two-thirds protein, one-third lipid,2 and <2% of a metal element such as iron, and can be seen by fluorescence or laser scanning microscopy.3 Currently, two forms of lipopigments with similar biochemical properties are recognized: lipofuscin, sometimes referred to as an “age pigment,”3 and ceroid, purported to accumulate in pathological conditions.2 Both lipofuscin and ceroid accumulate in the lysosomes of cells. There are several theories as to why the accumulation occurs, and the question of whether the lipopigment accumulation compromises the overall function of the lysosome remains unanswered.2 Some reports suggest these inclusions are an indication of poor prognosis and are possibly directly linked to mortality in patients with multisystem organ failure. We report two cases of patients with green inclusions.
Figure 1.
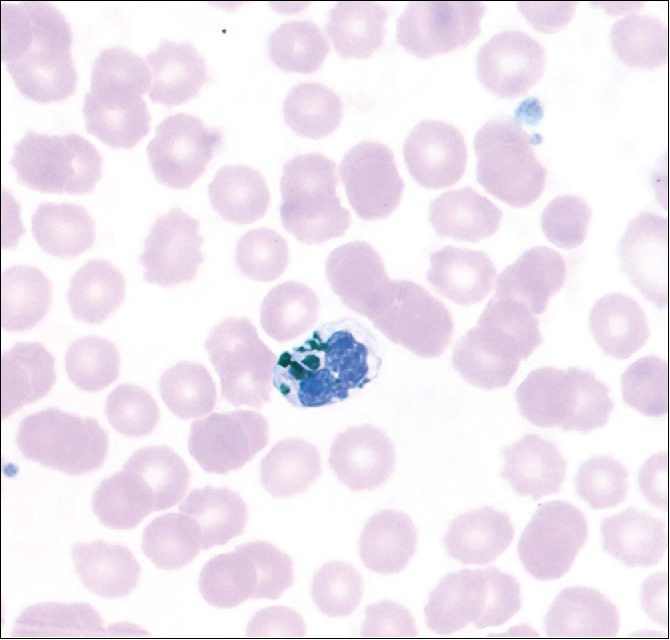
Coarse, bright blue-green granular inclusions identified in a neutrophil.
CASE 1
A 72-year-old man with polycystic kidney disease presented for an elective laparoscopic procedure for a small mass in the inferior pole of the right kidney concerning for early renal cell carcinoma. His past medical history was significant for chronic obstructive pulmonary disease, heart failure, end-stage renal failure on hemodialysis, secondary hyperparathyroidism, hypertension, and coronary artery disease. Two days after admission, the patient developed pulseless electrical activity, was resuscitated, and was transferred to the intensive care unit. A battery of laboratory tests was performed that included aspartate aminotransferase (2090 U/L) and alanine aminotransferase (2234 U/L) (Table 1). Rare, large irregular blue-green granules were incidentally found on tech review of the peripheral blood smear. Twelve hours after admission to the intensive care unit, the patient died.
Table 1.
Summary of patient data
| Variables | Reference range | Patient 1 | Patient 2 | ||||
|---|---|---|---|---|---|---|---|
| Age (years) | 72 | 34 | |||||
| Sex | Male | Female | |||||
| Comorbidities | |||||||
| Hypertension | + | + | |||||
| Heart failure | + | + | |||||
| Kidney disease | + | + | |||||
| Hemodialysis | + | 0 | |||||
| Chronic obstructive pulmonary disease | + | 0 | |||||
| Systemic lupus erythematosus | 0 | + | |||||
|
Draw |
Draw |
||||||
| Laboratory values | 1 | 2 | 3 | 1 | 2 | 3 | |
| Aspartate aminotransferase (U/L) | 0–40 | 66 | 2090 | 3895 | 18 | 228 | 156 |
| Alanine aminotransferase (U/L) | 0–68 | 52 | 2237 | 3422 | 6 | 54 | 44 |
| Carbon dioxide (mEq/L) | 23–31 | 21 | 10 | 6 | 26 | 19 | 19 |
| Lactic acid (mmol/L) | 0.5–2.2 | — | 22.7 | 24.5 | — | 3.9 | 1.0 |
| Bilirubin, total (mg/dL) | 0.2–1.2 | — | 1.3 | 1.7 | 0.3 | 2.1 | 1.9 |
| Blood urea nitrogen (mg/dL) | 8–27 | 22 | 27 | 29 | 50 | 64 | 71 |
| Creatinine (mg/dL) | 0.60–1.60 | 7.00 | 6.39 | 6.53 | 5.39 | 6.37 | 7.00 |
| Alkaline phosphatase (U/L) | 34–130 | 66 | 59 | 92 | 128 | 404 | 328 |
| Calcium (mg/dL) | 8.6–10.5 | 9.8 | 8.5 | 7.6 | 7.5 | 5.0 | 4.7 |
| Protein, total (g/dL) | 6.0–8.0 | 7.6 | 3.8 | 3.7 | 6.3 | 4.8 | 4.7 |
| Albumin (g/dL) | 3.2–4.6 | 3.6 | 1.8 | 1.8 | 2.9 | 2.2 | 2.0 |
| Sodium (mEq/L) | 136–145 | 140 | 151 | 153 | 142 | 139 | 136 |
| Potassium (mEq/L) | 3.5–5.3 | 4.5 | 4.3 | 4.1 | 4.1 | 4.2 | 5.2 |
| Chloride (mEq/dL) | 97–111 | 97 | 104 | 109 | 105 | 103 | 103 |
| White blood cell count (×109/L) | 4.8–10.8 | 9.6 | — | 7.2 | 9.6 | — | — |
| Platelet count (×109/L) | 150–450 | 74 | — | 69 | 74 | — | — |
| Prothrombin time (sec) | 12.2–15.3 | 2.1 | — | 3.1 | 2.1 | — | — |
| Partial thromboplastin time (sec) | 23.0–36.0 | 54.1 | — | 71.6 | 54.1 | — | — |
CASE 2
A 34-year-old woman presented to the emergency department with a severe headache and was found to have accelerated hypertension. She had chronic kidney disease, heart failure, depression, and drug-seeking behavior. On presentation, her blood pressure was 80/40 mm Hg, and she was found to have bilateral pleural effusions, metabolic acidosis, and acute respiratory failure. She was admitted to the intensive care unit with worsening respiratory status. The aspartate aminotransferase was 228 U/L and her alanine aminotransferase was 54 U/L (Table 1). Green granules were incidentally found on tech review. She developed pneumonia but then subsequently improved, was extubated, and was transferred from the intensive care unit to a lower level of care and eventually discharged.
DISCUSSION
Bright green-blue granular inclusions in neutrophils on a peripheral blood smear are being increasingly recognized and reported. One case report called them “green granules of death.”4 With this, the moniker “death cell” has been born. The true nature of these granules, their morphologic definition, and their constituents are poorly understood. Some have argued that these granules are composed of biliverdin, resulting from release of liver components secondary to acute necrotizing hepatitis,5 or that these granules are related to the aging process.1 In most cases, identification of these granules is difficult and often missed because they are so few in number.
Some argue that we should report these granules because of the association with poor prognosis.4–6 This view is based on findings such as those of Hodgson et al, who found that 65% of patients who had green granules identified on peripheral blood smear died shortly after identification (12–72 h).7 Yet, there are significant problems with this argument. Most cases involve intensive care unit patients admitted for severe disease, most frequently sepsis, who subsequently develop multisystem organ failure, including acute hepatitis. Our patients were also in the intensive care unit. Admission to such a unit carries with it marked mortality, highly dependent on age, severity of disease, and many other factors.8 Severe sepsis alone has a mortality rate as high as 30%.9 In fact, the length of time spent in an intensive care unit carries an independent risk of increased mortality.10 Simply stated, patients who are severely ill and admitted to an intensive care unit are more likely to develop multisystem organ failure, including liver failure, leading to death, whether or not green granules can be identified on peripheral blood smear, and clinicians are acutely aware of this. Overall, the number of reported cases of green granules is extremely low. We believe that these granules should not be reported as an indication of poor prognosis for a number of reasons, not the least being the potential to change clinical decisions that may result in withdrawal of care or other harm to the patient.
References
- 1.Brunk UT, Terman A. Lipofuscin: mechanisms of age-related accumulation and influence on cell function. Free Radic Biol Med. 2002;33(5):611–619. doi: 10.1016/S0891-5849(02)00959-0. PMID:12208347. [DOI] [PubMed] [Google Scholar]
- 2.Seehafer SS, Pearce DA. You say lipofuscin, we say ceroid: defining autofluorescent storage material. Neurobiol Aging. 2006;27(4):576–588. doi: 10.1016/j.neurobiolaging.2005.12.006. PMID:16455164. [DOI] [PubMed] [Google Scholar]
- 3.Terman A, Brunk UT. Lipofuscin. Int J Biochem Cell Biol. 2004;36(8):1400–1404. doi: 10.1016/j.biocel.2003.08.009. PMID:15147719. [DOI] [PubMed] [Google Scholar]
- 4.Jazaerly T, Gabali AM. Green neutrophilic inclusions could be a sign of impending death! Blood. 2014;123(5):614. doi: 10.1182/blood-2013-10-535856. PMID:24624440. [DOI] [PubMed] [Google Scholar]
- 5.Courville EL, Crisman S, Linden MA, Yohe S. Green neutrophilic inclusions are frequently associated with liver injury and may portend short-term mortality in critically ill patients. Lab Med. 2017;48(1):18–23. doi: 10.1093/labmed/lmw064. PMID:28039379. [DOI] [PubMed] [Google Scholar]
- 6.Harris VN, Malysz J, Smith MD. Green neutrophilic inclusions in liver disease. J Clin Pathol. 2009;62(9):853–854. doi: 10.1136/jcp.2009.064766. PMID:19734487. [DOI] [PubMed] [Google Scholar]
- 7.Hodgson TO, Ruskova A, Shugg CJ, McCallum VJ, Morison IM. Green neutrophil and monocyte inclusions—time to acknowledge and report. Br J Haematol. 2015;170(2):229–235. doi: 10.1111/bjh.13434. PMID:25892703. [DOI] [PubMed] [Google Scholar]
- 8.Singer AJ, Ng J, Thode HC, Spiegel R, Weingart S. Quick SOFA scores predict mortality in adult emergency department patients with and without suspected infection. Ann Emerg Med. 2017;69(4):475–479. doi: 10.1016/j.annemergmed.2016.10.007. PMID:28110990. [DOI] [PubMed] [Google Scholar]
- 9.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. PMID:11445675. [DOI] [PubMed] [Google Scholar]
- 10.Moitra VK, Guerra C, Linde-Zwirble WT, Wunsch H. Relationship between ICU length of stay and long-term mortality for elderly ICU survivors. Crit Care Med. 2016;44(4):655–662. PMID:26571190. [DOI] [PMC free article] [PubMed] [Google Scholar]


