Abstract
Study Objective
Survival into adulthood is now a reality for many adolescents facing cancer. FP (Fertility Preservation) is a rapidly advancing field, but oncology providers and health systems struggle to incorporate the newest FP technologies into the clinical care of adolescents. Our objective was to systematically review and synthesize the available data regarding the perspectives, experiences, and preferences of adolescents, parents, and oncology providers about FP to inform clinical implementation of FP technologies.
Design
Five electronic databases (PubMed, Embase, Web of Knowledge, CINAHL, PsychInfo) were systematically searched for studies published between January 1999 and May 2014. Adolescents were defined as 12-18y at diagnosis or designated as pubertal/post pubertal and <18yrs. Studies were assessed for methodological quality, data were extracted using a standardized form, and results were synthesized using guidelines for a narrative syntheses of both quantitative and qualitative data.
Results
In total, 1237 records were identified, with 22 articles, 17 unique studies meeting the inclusion criteria. The following topics were consistently observed across studies and populations: 1. “Fertility in Trust”, 2. Decision Making Challenges, 3. Provider Knowledge and Practices, and 4. Discrepancies between Desired and Actual Experiences.
Conclusions
Despite the challenges associated with a new cancer diagnosis, adolescents and parents value the opportunity to discuss fertility concerns and preservation options. Providers play an important role in addressing these topics for families and efforts should be made to incorporate FP discussions into routine cancer care for all adolescents, with attention paid to the unique needs of adolescents and their parents.
Keywords: adolescents, fertility preservation, oncology, parents, patient preferences
Increased survival of adolescents with cancer(1, 2) has shifted the focus of cancer treatment to prevention of late effects, including reproductive outcomes and fertility impairment. Recent advances have expanded fertility preservation (FP) options to include oocyte, ovarian tissue, and testicular tissue cryopreservation, all of which can be used in pediatric and adolescent patients. Initially only available in research settings, FP is considered standard of care(3-6), but remains unavailable to many patients facing cancer diagnoses (7-11). In part, because little is known about the optimal timing, content, and approach to FP counseling for adolescents. Practice guidelines from the American Academy of Pediatrics (AAP)(12), American Society of Clinical Oncology (ASCO)(11), and American Society of Reproductive Medicine (ASRM)(13) recommend discussing fertility complications and preservation options regardless of age and as early as possible, but incorporating these recommendations into clinical practice has proven difficult and raised many important ethical considerations(14-17). Some challenges to offering FP to adolescents include multiple stakeholders’ (adolescents, parents, and providers) in a shared decision making process, the sensitivity of the topic, and timing coincident with a new cancer diagnosis, when adolescents are vulnerable and families are focused on survival, rather than prevention of late effects(18-20). A synthesis of what is known about provider, parent and adolescent preferences, barriers and facilitators to fertility preservation counseling, and the optimal timing, content and approach, is necessary to operationalize these best practices guidelines.
There exists a growing literature on this topic and a systematic approach to synthesizing these data in a clinically relevant summary has the potential to further research and improve care. This emerging and heterogeneous literature includes a variety of study designs (primarily observational, many qualitative), target populations, sampling approaches, measures, and outcomes, and thus requires a systematic review approach that integrates mixed methods data.
Evidence-based medicine (EBM) recognizes the importance of including qualitative studies in systematic reviews to capture additional data and enhance conclusions drawn from quantitative analyses (21-24). Several EBM groups provide guidance on systematic reviews of mixed methods and observational studies (21, 24-27). Because of the heterogeneity of qualitative data, guidance is general, and includes a systematic search of the literature, content and quality assessments, and data summaries (21, 22, 24, 28).
Other published reviews on fertility preservation have focused more broadly on preservation methods, on adult populations, or failed to include all key participants in the shared decision making process unique to adolescent patients (6, 14, 29, 30). The purpose of this mixed methods review is to systematically identify, analyze, and synthesize studies of the perspectives, experiences and preferences regarding FP of all stakeholders (adolescents, parents, and providers) in the shared-decision making process.
Methods
The review was conducted June 2013 to May 2014, and informed by guidance from the Cochrane Qualitative and Implementation Methods Group(25, 31-34) and ESRC Methods Programme Guidance on the Conduct of a Narrative Synthesis in Systematic Review(35).
Study Identification & Selection
Given the relative lack of published research related to fertility preservation prior to 1999, studies published between January, 1999 and May, 2014 were eligible and identified by searching electronic databases, reviewing reference lists, and consulting investigators in the field. Five electronic databases (PubMed, Embase, Web of Knowledge, Cumulative Index to Nursing and Allied Health Literature [CINAHL], PsychInfo) were searched using combinations of the following key terms and synonyms in English language publications: “fertility” (infertility, fertility preservation, cryopreservation, oncofertility) AND “cancer” (oncology, oncologic, neoplasm, tumor, cancer survivor) AND “pediatric” (child, youth, adolescent, teen, childhood) AND “parent”(parental) AND “information” (communication, informational needs, attitudes, beliefs, decision making).
Studies were screened based on title and abstract. Those relevant to adolescent, parent or provider perspectives, experiences and preferences about fertility preservation were selected for full-text review. Findings from a single study in multiple publications were linked and assessed together. See Table 1 for inclusion criteria. If the articles did not provide enough information to determine eligibility, the corresponding author was contacted.
Table 1.
Study Inclusion Criteria
| Included studies met the following inclusion criteria: |
|---|
| 1. Original research article |
| 2. Full text available (i.e. not just a conference abstract) |
| 3. Include at least one question specific to fertility preservation, |
|
For studies including adolescents and parents: |
| 4. The mean mean/median age at diagnosis had to be between 12 and 18 years, or clearly defined as pubertal/post-pubertal and less than 18 years. |
| 5. Mean/median age at study <30 y, and/or |
| 6. Pubertal participants analyzed separately |
|
For studies that included providers: |
| 7 The majority of providers cared for pediatric patients, or the pediatric providers were analyzed separately. |
Quality Assessment
Two researchers (JT, MO) independently assessed quality using established critical appraisal tools. Quantitative data were assessed using the STROBE Checklist for Cross-Sectional Studies(36). Qualitative data were evaluated using criteria(22) that emphasize relevance and validity as key measures of quality. Differences of opinion were resolved through consensus. A quality score was calculated for each study. Because of the range of qualitative methodologies, and because most studies fell into a “moderate” quality range, we set pre-determined minimum score for inclusion.
Data Extraction & Analysis
Studies meeting inclusion criteria and quality standards were reviewed and the following data extracted: research design, setting and country of origin, sample characteristics (age at diagnosis, age at study, gender), study length, measures related to fertility preservation, and results. Because of marked heterogeneity of both quantitative and qualitative studies in populations, design, theoretical frameworks and outcomes, we were unable to calculate summary statistics using meta-analytic techniques. We instead adapted Narrative Synthesis, a flexible and iterative analytic approach driven by text rather than numeric data. Narrative synthesis (categorized as thematic analysis by Cochrane(26)) is an approach to systematic review that relies on the use of words and text to review, summarize and explain the findings of the synthesis(35).
We used a Narrative Synthesis approach which adapts well to inform clinical practice guidelines. Our analytic approach included the following key elements of Narrative Synthesis in an iterative manner: (1) Preliminary synthesis, (2) Exploring relationships, and (3) Assessing the product for robustness. Data extraction was informed by emerging themes identified in preliminary readings of the articles. All qualitative data, in results and representative quotes, identified as relevant to the review question were extracted. Quantitative data were examined in a textual manner rather than a formal cumulative numeric fashion.
The preliminary synthesis included tabulation, grouping, translation, and thematic analysis(22, 28). As the data were extracted into a tabulated format, initial descriptions of studies and characteristics were used to identify patterns, comparisons, and additional categories for the extraction of data from other studies. Studies were grouped according to methodological similarities and study population characteristics, and compared.
Using an iterative approach, we explored relationships, comparing and contrasting findings from different studies to better understand similarities and differences. Analysis focused on generating new understandings by grouping preliminary themes and diagraming relationship between these groupings. A visual representation of key themes and interactions was developed into an explanatory conceptual model to help elaborate similarities and differences as well as reciprocal relationships. (See Figure 1).
Figure 1.
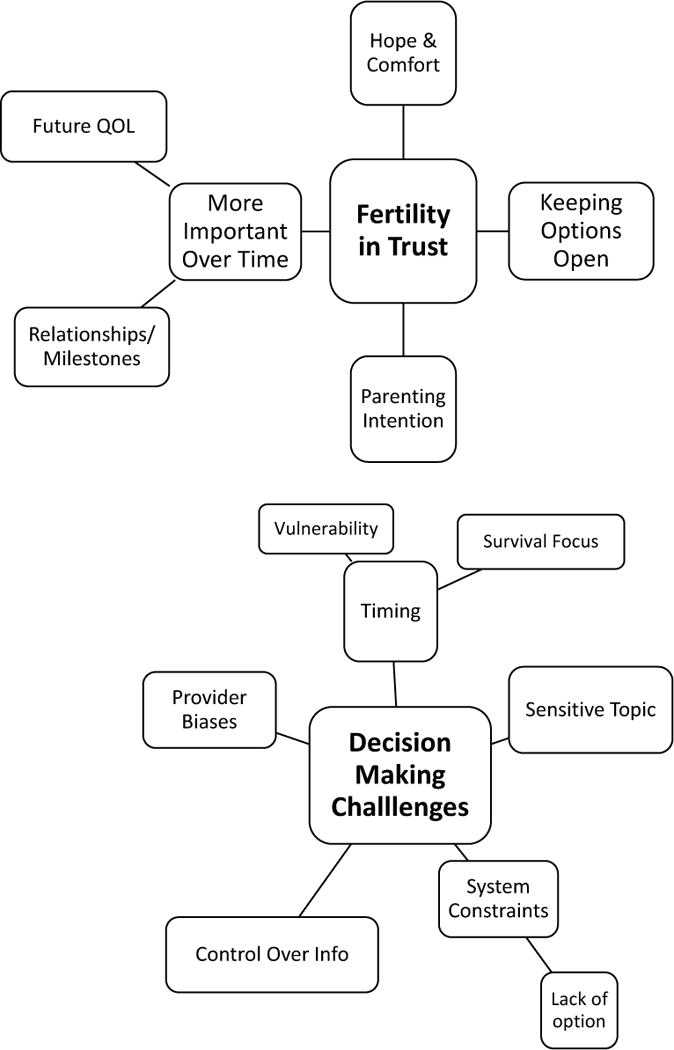
Key Concepts and Relationships
We used two methods to ensure the robustness of the final synthesis product. First, our specific inclusion criteria and quality assessment of studies resulted in the elimination of non-relevant and low quality studies. Second, a post-hoc analysis was undertaken to examine the resulting themes for consistency. The identified themes were consistent across studies, regardless of study quality; and across populations and study designs, with the exception of geographic differences in some themes with the largest difference being between studies from the United States and the United Kingdom.
Results
Study Identification
Figure 2 describes the database search, screening and assessment of eligibility. In total, 17 unique studies (37-58) met the inclusion criteria. Among articles assessed, exclusion due to mean age and length of time between diagnosis (and hence fertility discussions) and data collection were common.
Figure 2.
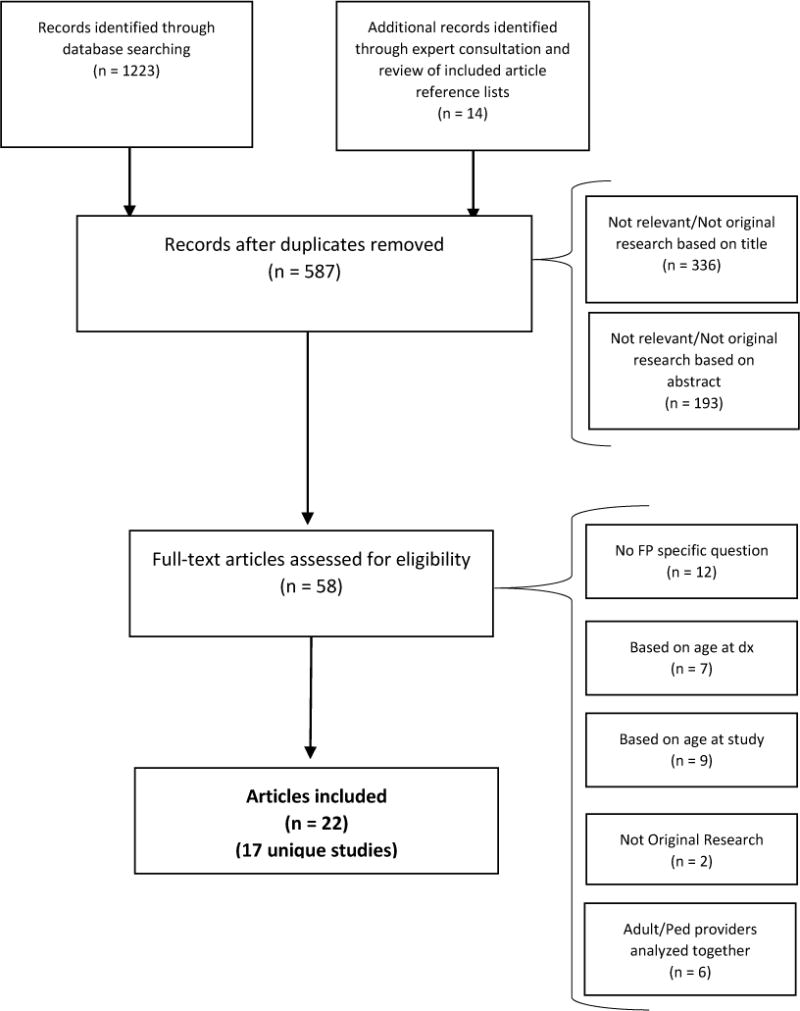
Study Identification & Selection Flow Diagram
Quality Assessment
Quality assessment was performed on all 17 unique studies. One article was excluded because it failed to report sufficient methodological detail.
Study Characteristics
Ten studies were quantitative and cross-sectional, employing surveys, and seven were qualitative, employing in-depth interviews or focus groups. The studies originated in four countries, with the majority from the United States (9 studies) and United Kingdom (5 studies). Eight studies included adolescents, five included parents, and eight included providers. Included studies are designated A1-A17 in Table 2.
Table 2.
Study Characteristics
| Study Reference Number | Study | Location/Setting | Study Population | Methods | Fertility Preservation Related Questions | Themes |
|---|---|---|---|---|---|---|
| Adolescents | ||||||
| A1 | (Edge, Holmes et al. 2006) | UK/Identified from the Manchester Children’s Tumour Registry and from hospital records at Royal Manchester Children’s Hospital and the Christie Hospital. | Male, (n=55) Aged 13–21 years who had been offered sperm banking. The average interval between diagnosis and interview was 2.1 years (0–5) |
Questionnaires | • Feelings about their future fertility, their diagnosis, • Their understanding of sperm banking both at diagnosis and at time of interview, • The ease with which they and their families could talk about fertility, on simple 1 to 10 visual analogue scales. |
Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Sensitive Topic Control of Information & Decision Making Discrepancy between Desired & Actual Experiences |
| A2 | (Chapple, Salinas et al. 2007) | UK/Recruited via doctors, nurses and support groups. Drawn from a wider study, conducted by one of the authors (MS), which explored young people’s experiences of cancer, for Youth Health Talk. | Male, (n=21) previously Diagnosed with cancer. 6 aged 16–18y and 12 age 19-26 at time of interview. |
Narrative interviews | • How they learned about the risk of infertility • Information needs • How some experienced sperm banking • Their feelings about possible infertility. |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Hope and Comfort Sensitive Topic Vulnerable Time Control of Information & Decision Making Discrepancy between Desired & Actual Experiences |
| A3a*linked (Craw2009, Craw2004) | (Crawshaw, Glaser et al. 2008) | UK/Recruitment through 3 Regional Pediatric and Adolescent Cancer Units. Purposive sampling | Males, (n=16) Aged 13 to 20 at diagnosis. Median time since diagnosis was 3 years. |
Single in-depth interviews | • Experiences, concerns or satisfactions with sperm banking. | Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Hope and Comfort Sensitive Topic Vulnerable Time Control of Information & Decision Making Constrained by Options Discrepancy between Desired & Actual Experiences |
| A3b *linked (Craw2009, Craw2004) | (Crawshaw, Glaser et al. 2009) | UK/Recruitment through 3 Regional Pediatric and Adolescent Cancer Units in the North of England using purposive sampling | Male & female (n=38) Diagnosed between 13-20 years. Median length of time since diagnosis among teenagers was 3 years, among adults was 7 years. |
• Experiences of having fertility and associated decision-making matters raised at diagnosis | ||
| A4 | (Ginsberg, Ogle et al. 2008) | US/CHOP between 2002 and 2006. | Males, (n=45) 45 At least Tanner Stage III, who were approached to sperm bank |
Questionnaires | • Understanding of the impact of therapy on future fertility. • The timing and approach of the clinical staff. • The beliefs that influenced the decision process. • The extent of parental involvement in the final decision. • Impact of delaying treatment in order to sperm bank • Actual experience of specimen collection |
Keeping Options Open Future Quality of Life & Milestone Achievement Sensitive Topic Vulnerable Time Control of Information & Decision Making |
| A5 | (Gorman, Bailey et al. 2012) | US/Recruitment from Moores Cancer Center at the University of California San Diego, Rady Children’s Hospital San Diego, and community-based recruitment methods. | Female, (n=22) Diagnosed with cancer between 0-35. Mean age at diagnosis 16.8 yrs., at study 26.1 yrs. |
Focus Groups | • Knowledge about the relationship between fertility and cancer treatment • Access to information and care, including fertility preservation options • Feelings toward fertility, pregnancy, and parenthood |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Sensitive Topic Vulnerable Time Constrained by Options Discrepancy between Desired & Actual Experiences |
| A6 | (Yeomanson, Morgan et al. 2013) | UK/Teenage Cancer Trust Conference “Finding your sense of tumour” | Males & Females (N=150 in 2004, 140 in 2011). Current and former patients. Median age M 18, F 17 in 2004, M 18, F 19 in 2011. |
Questionnaires | • Was there a fertility discussion? What was the Timing? • Were you given the option to bank sperm/freeze eggs? |
Sensitive Topic Vulnerable Time Control of Information & Decision Making Discrepancy between Desired & Actual Experiences |
| Adolescents & Parents | ||||||
| A7 | (Burns, Boudreau et al. 2006) | US/Oncology Clinic at Children’s Hospital of Wisconsin. Convenience sample. | Females & Parent, (n=39 parent/adolescent pairs, 3 parent-only responses, and 8 adolescent-only responses) Diagnosed with cancer between the ages of 10 to 21. Median age 15y, Median months since diagnosis 22 mos. |
Cross-sectional survey | • Adolescent has thought about the future. • Someone has talked to them about how their treatment might affect fertility • They have interest in pursuing research-based fertility preservation techniques • They are willing to wait 1 or more months to start therapy. |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Sensitive Topic Control of Information & Decision Making Discrepancy between Desired & Actual Experiences |
| A8 | (Nieman, Kinahan et al. 2007) | US/Recruitment from the Survivors Taking Action & Responsibility (STAR Program) at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, IL | Female & Parent, (n= 10 adolescents, 10 parents) Diagnosed/treated for cancer between 13-21yrs. |
Focus Groups | • Attitudes about fertility at the time of diagnosis and presently. • Reactions to a proposed clinical research study in ovarian tissue preservation. |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Hope and Comfort Sensitive Topic Vulnerable Time Control of Information & Decision Making Constrained by Options Discrepancy between Desired & Actual Experiences |
| Parents | ||||||
| A9 | (van den Berg, Repping et al. 2007) | Netherlands/Emma Children Hospital AMC, 1995-2003 | Parents of male survivors diagnosed from 0-17yrs, (n=117) *Pubertal sample analyzed separately |
Questionnaires | • Whether at initial diagnosis information on possible secondary infertility was provided • Parental expectation whether their child would be infertile. |
Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Sensitive Topic Discrepancy between Desired & Actual Experiences |
| A10 | (Sadri-Ardekani, Akhondi et al. 2013) | Tehran, Iran/Mahak Institute (tertiary cancer center) | Parents of male survivors diagnosed between (n =365) still. Mean age at dx 13 yrs., *Pubertal sample analyzed separately |
Survey | • Fertility knowledge. • Opinion on Fertility Preservation options, given risk of infertility, and chance of success. |
Keeping Options Open Sensitive Topic Vulnerable Time Discrepancy between Desired & Actual Experiences |
| Parents & Providers | ||||||
| A11 | (de Vries, Bresters et al. 2009) | Netherlands/Data was collected as part of a larger qualitative multi-centre project | Parents (n = 15) of male adolescents (aged 8–18 years) undergoing cancer treatment at the paediatric oncology units and physicians (n=14) | Semi-structured interviews | The perceived role of parents in decision making regarding cancer therapy and related treatments, like fertility preservation options. • The physician–patient–parent relationship, especially concerning decisions regarding therapy and related treatments, like fertility preservation options. |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Sensitive Topic Vulnerable Time Control of Information & Decision Making Discrepancy between Desired & Actual Experiences |
| Providers | ||||||
| A3c *linked (Craw2009, Craw2004) | (Crawshaw, Glaser et al. 2004) | UK/2 Regional Pediatric Oncology Centres in the North of England and Referral Centres for Assisted Conception | Health and social work professionals (n=22): 4 doctors, 2 nurses, and 4 scientists from Assisted Conception Units; 6 Doctors, 4 nurses, and 2 social workers from Pediatric Oncology Centres. | Semi-structured interviews | • Common practices, areas of variance and issues experienced by professionals in UK regional paediatric oncology centres and licensed assisted conception centres. | Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Hope and Comfort Sensitive Topic Vulnerable Time Control of Information & Decision Making Constrained by Options Discrepancy between Desired & Actual Experiences |
| A12 | (Reebals, Brown et al. 2006) | US/Hospital in Southeastern US, 4 hospital units and clinics | Providers (n =27) RN, NP that provide care to Males age 14-18 | Questionnaire | • Attitude about sperm banking, factors that may influence willingness to offer sperm banking, | Keeping Options Open Pregnancy/Parenting Intention Hope and Comfort Provider Variability Provider Knowledge and Practice |
| A13 | (Goodwin, Oosterhuis et al. 2007) | US/Lucile Packard Children’s Hospital | Health Care Providers (n =30) (46% NPs & RN, 53% physicians, fellows) | Survey | • Referral Practices & Difficulties • Beliefs regarding fertility preservation, including: timing, cost, efficacy, training, etc. |
Keeping Options Open Sensitive Topic Vulnerable Time Constrained by Options Provider Knowledge and Practice |
| A14a* linked (Vad 2007, Clayton 2008) | (Vadaparampil, Clayton et al. 2007) | US/FL Assoc of Ped Tumor Programs Conference 2005 | Nurses (n=103) RN, AP | Survey | • Knowledge of Fertility Preservation • Provider attitudes toward patient factors that may affect the discussion of Fertility Preservation |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Pregnancy/Parenting Intention Provider Variability Provider Knowledge and Practice |
| A14b* linked (Vad 2007, Clayton 2008) | (Clayton, Quinn et al. 2008) | US/FL Assoc of Ped Tumor Programs Conference 2016 | Nurses (n =95) RN, AP | |||
| A15 | (Anderson, Weddell et al. 2008) | UK/recruited 2003-2004, new dx of cancer registered at Children’s Cancer and Leukaemia Group centre. (22 centres in UK, 17 participated) | 1030 patient forms (68% at participating centres), 15% pubertal, 9% post-pubertal | Prospective Observational: oncologists assessed fertility risk, indicate whether FP was discussed | • Have fertility preservation techniques been discussed? If yes, at whose instigation. If no, why? • What fertility preservation techniques were discussed? Check lists for male and female including ‘not specified’ • Whether the patient was referred to a fertility centre |
Keeping Options Open Hope and Comfort Sensitive Topic Constrained by Options Provider Variability Provider Knowledge and Practice |
| A16a*linked (V2008, Q2009, Q(2)2009) | (Vadaparampil, Quinn et al. 2008) | US/Recruitment from 13/15 children’s cancer centers in Florida | Pediatric oncologists (n=24) | Semi-structured, in-depth interviews | • What does fertility preservation mean to you? • What procedures are you aware of? • Do you typically refer FP patients for consults or services? • What priority level do you think FP discussions are to your patients (high, med, low)? |
Keeping Options Open Pregnancy/Parenting Intention Sensitive Topic Vulnerable Time Control of Information & Decision Making Constrained by Options Provider Variability Provider Knowledge and Practice |
| A16b*linked (V2008, Q2009, Q(2)2009) | (Quinn and Vadaparampil 2009) | US/subset of data from a larger study examining the knowledge, attitudes, and behaviors of pediatric oncologists | ||||
| A16c*linked (V2008, Q2009, Q(2)2009) | (Quinn, Vadaparampil et al. 2009) | US/Recruitment from 13/15 children’s cancer centers in Florida | Pediatric Oncologists (n =26) | |||
| A17 | (Kohler, Kondapalli et al. 2011) | US/National Pediatric Oncology subspecialty group via the group’s list serv | Providers (n=180), 167 (93%) oncologist, 5 (3%) NP, 2 (1%) reprod endo, 6 (3%) no/other | Survey | • Fertility preservation attitudes and practice patterns for both pre-pubertal (1–12 years of age) and pubertal (13–18 years of age) cancer patients, stratified for males and females. • Knowledge of specific fertility preservation methods, their familiarity with ASCOR, and their practice patterns with regard to fertility preservation |
Keeping Options Open Future Quality of Life & Milestone Achievement Fertility Becomes More Important Over Time Sensitive Topic Vulnerable Time Constrained by Options Provider Knowledge and Practice |
Sample Characteristics
Sample sizes were 10-38 for qualitative studies and 27-1030 for quantitative studies. Three (A4, A6, A7) studies assessed adolescent perspectives within, on average, 2 years of diagnosis, two (A1, A3a) within 5 years of diagnosis, two (A8, A3b) more than 5 years after diagnosis, and two (A2, A5) did not specify a time interval. Four studies (A1, A2, A3a, A4) included only male adolescents, three (A7,A8, A5) included only female adolescents, and two (A3b, A6) included both. Parent perspectives were included in five (A7, A8, A9, A10, A11) studies with variable time since diagnosis. Eight (A3c, A11, A12, A13, A14a, A14b, A15, A16Aa, A16Ab, A16Ac, A17) provider studies included nurses, advanced practice nurses, and physicians who provided oncology care or reproductive services to adolescents.
Major Themes
The following topics were consistently observed across studies and across adolescents, parents, and providers: 1. “Fertility in Trust”, 2. Decision Making Challenges, 3. Provider Knowledge and Practices, and 4. Discrepancies between Desired and Actual Experiences. These themes are presented below, with details provided about perceptions of adolescents, parents, and providers. Representative quotations are included in Table 3.
Table 3.
Representative Quotations
| Quote Reference Number | Respondent | Quote | Study |
|---|---|---|---|
| Fertility In Trust | |||
| Keeping Options Open | |||
| Q1 | Adolescent | “I decided there and then and it’s question of [um] it’s just a hundred things running through your mind, but at the end of the day it’s best to have that option left open.” | A2 |
| Q2 | Adolescent | “…Cos if I didn’t [bank] and it came out at the end of treatment that I was infertile then, I dunno, it would be a … bugger, really, yeah, er, cos like in later life if you ever wanted to have children, like you wouldn’t have anything.” | A3b |
| Q3 | Parent | “Whether she wants to have children or not, you want them to be…capable of having a choice.” | A8 |
| Q4 | Parent | “I don’t want to deny him choices in the future by deciding for him now.” | A11 |
| Q5 | Provider | “I think it’s our duty as oncologists to offer fertility preservation, because only before start of treatment is there the possibility to do so.” | A11 |
| Future QOL & Milestone Achievement | |||
| Q6 | Adolescent | ““Well, the whole opening up thing and telling someone, it’s really hard because I don’t want a pity party. I don’t want someone to feel sorry for me. I don’t want them to judge me.” | A5 |
| Q7 | Adolescent | “How do I go into a relationship and say, “I can’t have children,” am I gonna face instant rejection?” | A2 |
| Q8 | Parent | “What counted for us was the thought that, well, let’s suppose that he wants to start a family, that his future wife has a strong child wish, and we would have blocked the way.” | A11 |
| More Important Over Time | |||
| Q9 | Adolescent | “I didn’t think a thing about fertility until I was 20 and people started getting married and talking about babies and stuff.” | A5 |
| Q10 | Adolescent | “Well I declined and it’s a decision which [pause] I think was the wrong decision now, but it’s easy to look back and say that it was the wrong decision, when you’re in that situation, you know, maybe it is.” | A2 |
| Q11 | Parent | “It became more and more important as you saw them getting well…” | A8 |
| Q12 | Provider | “And maybe later on, when they are 25 years old they come back to me and ask: doctor, why didn’t you offer it to me?” | A11 |
| Pregnancy/Parenting Intention | |||
| Q13 | Adolescent | “So I thought well if I say no, that’s my chances of having a kid gone, so best option is saying yes.” | A2 |
| Q14 | Adolescent | “…And children I suppose, not being able to have children. That did pop into my head, even at 15 it popped into my head.” | A2 |
| Q15 | Adolescent | “I feel like I’ve known from a young age that I love kids…the thought of not being able to go through…that process of being pregnant was very, very scary for me.” | A8 |
| Q16 | Adolescent | “…I didn’t want to continue with treatment after they told me that I had ovarian failure. You know it was…it was very traumatic.” | A8 |
| Hope & Comfort | |||
| Q17 | Parent | “I think it also gives a large measure of hope and expectation to someone at the front-end of it.” | A8 |
| Q18 | Provider | “It does in a way give a ray of hope… with boys if you don’t do the sperm banking early, you miss your chance.” | A16a |
| Q19 | Provider | “You are giving a message that says I expect your kid to live.’ | A16a |
| Q20 | Provider | “‘If I know the patient has a very curable disease… then I will bring it up. You don’t give caviar to the poor person who does not have enough to buy bread. | (A16b) |
| Decision Making Challenges | |||
| Sensitive Topic | |||
| Q21 | Adolescent | “The doctor who told me this was really sort of, really weird as well, the way he told me. He made me feel like a kid or something. It was really embarrassing.” | A2 |
| Q22 | Adolescent | “Which was a slightly embarrassing situation to be in. To be given a pot with your parents down there and to go in the room and fill in, was embarrassing.” | A2 |
| Q23 | Adolescent | “When my Dad came in and asked me if I knew how [to masturbate], I was very embarrassed…” | A3b |
| Q24 | Adolescent | “I just think you need to know your options. Even though it might seem kind of weird at first you know, I mean thinking about that when you are so young. It still has to be presented to the parents and the patient.” | A8 |
| Q25 | Parent | “Is it reasonable then to confront him with this side-effect? We told the physician not to mention it to him”. | A11 |
| Q26 | Provider | “I am uncomfortable contributing to the stress of the situation by bringing up fertility issues, even without a cancer diagnosis this can be an embarrassing topic.” | A16c |
| Q27 | Provider | “There is a certain degree of embarrassment (with parents). It’s hard in that kind of emotional situation.” | A16c |
| Q28 | Provider | “It’s important that you (the physician) not be embarrassed about it…but some parents don’t want to deal with it. They don’t want to think about their kid masturbating.” | A16b |
| Vulnerable Time | |||
| Q29 | Adolescent | “And it was a bit, all a bit rushed and I was thinking really more about the treatment and was it going to kill me rather than anything else.” | A2 |
| Q30 | Adolescent | “That yes it’s not a very nice thing to hear, and yes you’ve got a lot going through your mind at the time and the last thing you need is to be told is there’s a chance you could be infertile at the end of it … it’s better than not being told.” | A3b |
| Q31 | Parent | “The evening before the start of the chemotherapy he [the child] was told about possible infertility and semen preservation. Later on we told them [the physicians] that the timing was really bad. We felt it was mentioned too late. They should have mentioned it during the first conversation.” | A11 |
| Q32 | Provider | “It’s too much all at once – diagnosis, treatment, future, and parents often do not want to hear it anyway so I don’t add to their stress or mine.” | A16c |
| Q33 | Provider | I think that part of what happens. is (parents).. don’t give a damn about the rest of it. All they care about is if their kid (going to live). | A16b |
| Q34 | Provider | “It’s very emotional … it’s sort of like adding insult to injury, to many families the (infertility) is even worse than the cancer.” | A16a |
| Q35 | Provider | “An overwhelming amount of information is being presented in a short-time. Even if you’ve got it on video tape they don’t remember.” | A16a |
| Control of Information & Decision Making | |||
| Q36 | Adolescent | “I didn’t really think about it, to be honest. I just said yeah pretty much on the spot.” | A3b |
| Q37 | Parent | “I think the sequence is wrong. You should first contact me, when you want to discuss things with my child.” | A11 |
| Q38 | Provider | “Some families have different beliefs or religions and we don’t find out what the kid wants because the parents don’t continue the discussion.” | A16b |
| Q39 | Provider | “Some parents just don’t want to hear about it.” | A16a |
| Q40 | Provider | “I think it should be offered and I feel justified in passing over the parents. If I think the child is ready and parents doubt that, then I think it’s in the best interest of the child to go ahead.” | A11 |
| Constrained by Options | |||
| Q41 | Adolescent | “…If the boys get told why don’t the girls?” | A3b |
| Q42 | Adolescent | “I do remember thinking it was just totally unfair that guys could freeze their sperm and there really were no options for women.” | A8 |
| Q43 | Parent | “I kind of felt it was either you did this or she’ll die…I mean it didn’t seem like there was a choice…” | A8 |
| Q44 | Provider | “And for some young kids (pre-pubertal) there is nothing they can be offered so why make everyone worry?” | A16c |
| Q45 | Provider | “First of all, there is no one within this community who would be willing to do cryopreservation if it involved a cancer site – so I don’t like to present options to patients that are unrealistic.” | A16c |
| Provider Variability | |||
| Q46 | Provider | “I feel really challenged by the whole discussion (FP) – I wish there were a counselor who did this… a specialized nurse… you start adding in different cultural backgrounds and religious preferences and the time factor and this is an important, but messy topic | A16c |
| Q47 | Provider | “Talking about this with males mean talking about masturbation and in some Hispanic families that is not acceptable. Having to talk through an interpreter also makes it awkward for everyone.” | A16c |
| Provider Knowledge & Practice | |||
| Q48 | Provider | “Someone with more information than me should be talking to these patients – I’m not comfortable with the topic or the emotional aspects of this.” | A16c |
| Q49 | Provider | “I must say I doubt that I’m any kind of authority on this, uh, and but, you know, I am willing to bring it up because I know it’s a problem.” | A16a |
| Q50 | Provider | “It’s a problem we run into in this town—there is just no place (to send patients).” | A16a |
| Discrepancy Between desired and actual experiences | |||
| Q51 | Adolescent | “I will just add that … I think I remember being shocked like after treatment they are like, oh well fertility is an issue, and I am like it is? Like I was shocked”. | A8 |
| Q52 | Adolescent | “And I think it was very recently that anyone brought up that it was possible that they could’ve done some preventative measures at the time. And that was more disheartening than anything, that no one discussed that.” | A5 |
| Q53 | Adolescent | “I think there would be a lot of angry and upset girls if they weren’t told from day one.” | A3b |
I. Fertility in trust
We defined fertility in trust as an obligation to recognize the long-term importance of fertility, and to act in a manner that supports adolescents’ current and developing autonomy with a focus on preserving future self-determination with respect to parenthood decisions. Fertility was seen as a long-term issue influenced by short term decisions, and thus it was necessary for adolescents (and, to some extent, parents) to put their fertility “in trust” to providers. Subthemes included the emphasis on keeping future options open, the importance of fertility in future quality of life, especially regarding future relationships/milestones, the recognition that fertility becomes increasingly important over time, that some adolescent patients already have parenthood goals, and that preserving fertility offers some hope to families.
Keeping Options Open
Ten studies (A2, A3a/A3b, A4, A7, A8, A10, A11, A12, A14a, A17) presented data relevant to fertility preservation as a tool to preserve all future options. In many studies (A2, A3b, A5, A8), adolescents identified the need to keep options open as a reason to pursue fertility preservation, without reference to a specific parenting intention, (Quotes Q1, Q2).
In most studies (A4, A7, A8, A10, A11), parents commented on the importance of future choice and maintaining options or responded to fertility preservation options positively. Many parents felt a duty to preserve fertility or to hold it “in trust” until the young person was at a stage in life when parenthood would be a more serious consideration, (Quotes Q3, Q4).
Providers (A11, A12, A13, A14a, A15, A16c, A17) perceived fertility as an important concern in treating adolescent patients. In one study (A17), 80-83% of providers identified fertility threats to male and female patients as a major concern. Another study (A13) found that 97% of pediatric oncology providers agreed that, when infertility is a potential side effect of cancer treatment, providers should discuss preservation options. In qualitative studies (A11, A16c, A15), providers elaborated on the importance of fertility preservation, and felt a duty to protect parenthood as a potential future option, even when the adolescent (and/or parent) was not able to consider the future (Quote Q5).
The Importance of Fertility in Future Quality of Life & Milestone Achievement
Adolescents (A2, A3b, A5, A8), especially those further out from treatment, perceived fertility as a significant component of romantic relationships, (Quotes Q6, Q7). There was a strong perception that fertility status can affect relationships developed over time, with older adolescents and survivors were more likely to comment on relationships and marriage as factors to consider when addressing fertility preservation.
Parents and providers were invested in the future quality of life for adolescents and identified relationship concerns and future desires for children as factors in considering fertility preservation. Four quantitative studies (A4, A7, A8, A9) found fertility preservation procedures to be acceptable to parents, regardless of procedural requirements, experimental nature, or study location, suggesting parents place high importance on fertility. For parents of male adolescents, one study found that 80% of parents’ initial response to sperm banking was “Great idea, this is the right thing for me/my son.” (A4) and in the same study, 100% of parents whose son experienced a delay in treatment due to sperm banking agreed that, “banking was important enough to delay treatment” (A4). In qualitative studies, parents reported wanting to keep options open to ensure their child’s future quality of life (A8, A11) (Quote Q8).
Providers (A11, A12, A14a, A17) identified the role fertility plays in survivorship and future life goals as a reason that providers have a duty to discuss fertility options. Some providers (37%, 67%) responded that they would be more likely to offer fertility preservation when a, “patient is engaged or recently married” suggesting that providers recognize the importance of fertility in relationships. (A12, A14a).
Fertility Becomes Increasingly Important Over Time
Including studies with recently diagnosed adolescents and survivors enabled us to examine the relationship between time since diagnosis and the importance of fertility preservation. Across studies, adolescent and young adult survivors identified fertility preservation and parenthood as increasingly important during survivorship (A8, A2, A5, A3a/A3b). At diagnosis, adolescents identified survival as the most pressing concern (A1, A2 A7, A8,) with one study of females receiving or having recently received treatment reporting that, adolescents ranked, “to have good health” higher than “to have children of their own” (A7). Retrospectively (A2, A3a, A5, A8) survivors described the growing importance of fertility with some patients regretting earlier decisions or wishing there were more options available to them (Quote Q9 and Q10).
Studies of parents similarly described a sense that survival was the most pressing concern at time of diagnosis (A7, A8, A9, A11). One study asked for parental perspectives on fertility preservation options for pubertal males at time of diagnosis and at the time of the survey, with, higher (but not statistically significant) rates of approval for all methods of FP at time of survey completion (A9). Similar to adolescents, biologic parenthood and fertility concerns became more important for parents as their child’s survival seemed increasingly assured (A8, A11) (Quote Q11).
In one quantitative study, providers were asked why families refused sperm banking, with the most common responses being, “the desire to initiate treatment as soon as possible, not wanting to be concerned with possible infertility, and the patients (or their parents) not being concerned with parenthood at the time of treatment,” (A17) similarly emphasizing that survival and treatment take precedence for everyone. In two qualitative studies (A11, A14a), providers themselves worried about the importance fertility would play in the future for their adolescent patients, (Quote Q12).
Pregnancy/Parenting intention
Only four quantitative studies asked about parenting intentions (A1, A5, A12, A14a). However, most qualitative studies (A2, A3a/A3b, A5, A8) with adolescents addressed parenting intention (Quotes Q13, Q14). Others described adolescent distress at learning that their fertility might be compromised (Quotes Q14, Q15). While not all adolescents expressed strong parenting desires, adolescents of both genders identified desires for biologic parenthood as an important factor in fertility decisions. In one study of adolescent males, those who successfully banked sperm had a higher concern about future fertility (A1). In contrast to adolescents, parents focused on fertility preservation as a means to ensure future choices, rather than an extension of current parenting desires, (Quote Q3).
Providers were influenced by an adolescent’s stated desire to have a family in the future, with 83% (A14a) to 85% (A12) of providers agreeing that they are more likely to mention fertility preservation if the adolescent brings up fertility or states a desire for future children.
Hope and Comfort
Providing hope and comfort is a potentially overlooked benefit of fertility preservation conversations. Both adolescents and parents in three studies (A2, A3a/A3b, A8) perceived fertility preservation discussions as a prediction of survival and a suggestion of hope (Quote Q17).
In one study (A15), providers explicitly acknowledged that fertility preservation provides hope to some adolescents and their families (Quotes Q18, Q19). In other studies (A12, A15, A16a/A16b), the fact that providers avoid offering fertility preservation to adolescents with poor prognoses, supports the idea that fertility discussion may provide hope, or for some, a false hope (Quote Q20).
II. Decision-Making Challenges
Challenges included the sensitivity of fertility discussions, the difficult timing of many preservation procedures, variations in desired control of information and timing, constraints intrinsic to health care systems or to available technologies, and provider biases.
Sensitive topic
Fertility preservation was perceived by adolescents (A1, A2, A3a/A3b, A4, A8) as a sensitive topic with the potential for embarrassment (Quote Q21). The inclusion of parents in the discussion contributed to awkwardness for some adolescents (A1, A2, A3a) (Quotes Q22, Q23) but not others (A3a, A3b). Fertility preservation for males typically includes masturbation and male adolescents noted that the sperm banking facilities (A2), parental involvement (A3a, A3b), and their own anxiety (A1) influenced their experience of discomfort. Anxiety was independently associated with unsuccessful sperm banking in one study (A1) suggesting that the sensitive nature of the topic and emotional state of male adolescents may influence their ability to successfully bank sperm. In the same and other studies (A2, A3b, A5, A6, A8) adolescents appreciated matter of fact discussions that were not awkward. In four studies (A3b, A5, A8, A6) adolescents commented that fertility discussions are important regardless of their sensitive nature (Quote Q24).
High levels of parent support for fertility preservation discussions between providers and adolescents was observed across studies, regardless of its sensitive nature (A4, A8, A7, A9, A10). The exception was one (A11) study in which some parents expressed concern about fertility preservation being distressing and too mature (Quote Q25). Other parents in the same study were more supportive.
In contrast to adolescents’ and parents’ support for fertility discussions, provider studies identified the sensitive nature of fertility preservation as a major factor influencing providers’ own comfort with the topic (A3c, A13, A15, A16a/A16b/A16c) (Quotes Q26-28). Providers perceive fertility conversations as potentially embarrassing, and modified their fertility discussions/recommendations based on age, gender, religion, and or cultural practices (A16a/A16b). Two provider studies (A11, A17) did not find fertility preservation to be a sensitive subject, with one study reporting that discomfort with discussing sperm banking was the least likely reason for providers to not recommend sperm banking (A17).
There was some geographic variation in provider perceptions. In a study from the Netherlands, providers reporting talking to adolescents directly about fertility preservations, independent of parents (A11). No US studies had this finding. It is possible that the Dutch practice of discussing FP with the adolescent alone may contribute to the parent discomfort described in the same study (A11).
Vulnerable time
Conversations about fertility preservation ideally occur after diagnosis, but before starting therapy, which was identified as a period of vulnerability by all parties. In all qualitative studies (A2, A3a/A3b, A5, A8), adolescents reported feeling overwhelmed after diagnosis. However, in in these same studies (A2, A3a/A3b, A5, A8), adolescents also recognized the importance of receiving fertility information early enough that preservation might be an option (Quotes Q29-Q30). The timing of fertility conversations and procedures were important factors for adolescents and parents regardless of gender (A2, A3a/A3b, A4, A5, A6, A8, A10, A11) (Quote Q31). In quantitative studies (A4, A6, A10), timing was specifically addressed with 64% of parents of pubertal males in one study citing time constraints as a reason they were unable to pursue fertility preservation (A10). In another study, the majority of parents (83%) and adolescents (65%) who received information or referral soon after diagnosis generally felt that the timing was appropriate (A4). Providers reported (A3c, A13, A16a/A16b/A16c, A17), being keenly aware of the stress on adolescents and families after receiving a cancer diagnosis, which influenced their willingness to broach the topic of fertility preservation (Quotes Q32-35).
Control of Information & Decision Making
Perceptions about the ease or difficulty of fertility preservation decisions were influenced by experiences of control over the decision, parental participation, information provided, and satisfaction with information or options. There were marked differences between studies of male versus female adolescents. When asked about their decision to pursue or forgo fertility preservation (A2, A3a/A3b, A4), male adolescents perceived being in control of the final decision to pursue fertility preservation. In one study (A4), only a small minority (6.3%) of adolescent males perceived that their parents alone made the decision to bank sperm, the remainder felt they made the decision alone (33.3%) or in conjunction with parents (58.3%). Studies examining adolescent preferences for parent participation in fertility discussions (A4, A2, A3a, A1, A3b), reported two contrasting opinions. Many adolescents desired parental involvement in decision making while also wanting to maintain control over the decision as to who was present during conversations or a trip to the sperm banking facility. In one study (A4), 56% of males would have preferred to hear about sperm banking with their parents, while 44% would have preferred to hear about sperm banking alone initially. Data were not available on predictors of desiring parental involvement. In qualitative studies (A2, A3a/A3b) the decision to preserve fertility was experienced as straightforward for males and, in UK studies, where sperm baking is protocolized, the decision was occasionally seen as something that was just part of their treatment (Quote Q36).
For female adolescents, quantitative studies found that only 62% (A6) to 69% (A7) recalled fertility conversations occurring, and satisfaction regarding those conversations was markedly lower than that reported by male adolescents (A6). In qualitative studies (A3b, A5, A8), female adolescents perceived the limited availability of fertility preservation options as a factor that led to less quality information and less control over decisions. Some adolescent females perceived the only option would be to delay treatment, which was not acceptable (A3b, A5, A8).
There was no consensus amongst parents about how fertility preservation conversations should progress with their adolescent. In three studies (A4, A8, A11), parents preferred control over the content and timing of information provided to their adolescents about FP, but also supported adolescents’ ability to participate in decisions. Some parents (A8, A11) perceived the need to protect their children from potentially upsetting or sensitive information, citing their child’s age, maturity, and severity of illness (Quote Q37). In one study (A8) parents also felt that much of the FP decision making rested with providers. In one study, parents’ and adolescents’ perceptions of decision-making control of the same decision were at odds, with parents perceiving the decision to be made jointly with their son (80%), while only a minority of males perceived a joint decision (14%) (A4).
Studies (A11, A16a/A16b) of how much providers defer decision-making control to parents showed a range of responses (Quotes Q38-Q40). Two US studies (A16a/A16b) found that some providers will defer informational and decisional control to parents; a study from the Netherlands (A11) found that some providers felt justified in discussing FP information with adolescents regardless of parents’ preferences.
Constraints intrinsic to health care systems or to available technologies
The limited options available also contribute to the challenging nature of fertility preservation discussions. Female adolescents especially, (A5, A3b, A8) commented on gender differences and the experience of being told about fertility complications without preservation options being available (Quotes Q41, Q42). In one study (A8), parents of female adolescents, commented on the perceived lack of options (Quote Q43).
Provider studies (A13, A15, A16a/A16b/A16c) also described the lack of non-experimental options for adolescent females and of readily available resources as additional challenges (Quotes Q44, Q45). This may, in part, explain the discrepancy in a provider study between providers’ beliefs that all adolescent females should be referred to a fertility preservation specialist prior to therapy (73%), and actual referrals (23%) (A17).
Provider Variability
Providers (A12, A14a/A14b, A15, A16b/A16c) demonstrated marked bias in whether and when to discuss fertility preservation options with adolescents. Factors including adolescents’ age, gender, severity of illness, concern about cultural differences, adolescent’s direct request for information, relationship status, and sexual orientation all influenced providers” willingness to discuss fertility preservation (Quotes Q46, Q47).
III. Provider Knowledge and Practice
Most studies (A13, A14a/A14b, A15, A16a/A16b/A16c) reported discrepancies between providers’ knowledge of and support for fertility preservation, and actual practices. Knowledge of fertility preservation was variable, with accurate knowledge ranging from 22% to 50% (A13) to 74% (A17) to 100% (A12), depending upon the type of provider (RN, NP, Physician, etc.) and the specific fertility preservation question. Consistent across studies, even providers with knowledge of fertility preservation identified lack of training, resources, or referral options as potential barriers (A13, A14a, A15, A16b/A16c). Despite variable knowledge, providers’ support for fertility preservation was generally high (See sections on Keeping Options Open and Fertility Becomes More Important).
Qualitative provider studies (A16a/A16b/A16c) identified a lack of prior experience, lack of training/education, cost of fertility preservation (especially for females), and uncertain benefit of some methods as barriers to providing fertility preservation to adolescents (Quotes Q48, Q49). Some providers also perceived being constrained by their own inexperience with fertility preservation as well as system limitations regarding access to specialists (Quote Q50).
IV. Discrepancy between desired & actual experiences of adolescents and parents
Many studies (A1, A2, A3a/A3b, A5, A6, A8, A11) reported differences between adolescents’ and parents’ expectations and the actual fertility preservation information they received. Across studies (A2, A3a/A3b, A5, A8), most adolescents and parents desired more information sooner (Quotes Q51-Q53).
Adolescents and parents in three studies (A2, A5, A8) requested more in-depth information regarding fertility preservation options and would prefer that this come from a medical provider. In several studies (A2, A3a/A3b, A5, A8) adolescents wanted information provided to all adolescents regardless of age. In two of these studies, (A2, A3a/A3b) adolescents identified important provider qualities that facilitate open communication about fertility preservation, including friendliness, a matter-of-fact approach without awkwardness, and respect for the adolescent as a decision maker. Four studies (A7, A8, A9, A10) reported that adolescents and parents would consider experimental procedures, although it is unclear whether these options are presented to families as no studies asked participants to recall this information.
Discussion
Combining adolescent, parent and provider perspectives as key stakeholders in a shared decision making process highlights the importance of engaging in discussions of fertility complications and preservation options early in treatment, as part of routine cancer care, and providing additional support as necessary to aid all participants navigate these complicated decisions. Similar to reviews that have included adult survivor, all stakeholders find fertility preservation discussions challenging, but necessary(8).
The notion of “fertility in trust” underscores reports from adolescents and parents that, while fertility decisions at the time of diagnosis are difficult, fertility grew in importance over time. It also emphasizes the pivotal role that providers play, as trusted advisors, in discussing fertility and addressing preservation options despite a family’s initial vulnerability immediately after diagnosis. Given that families report feeling overwhelmed, providers need to make additional time and resources available for conversations about the possibly devastating long-term effects on fertility. It is also important to note the support that adolescents and parents gave for having these conversations, even in the absence of options. The importance of early and frequent conversations is supported by other studies that have looked at the lack of congruence between adolescents and parents, the coping styles of adolescent females, and gender disparities in fertility related services(59, 60).
Similar to adult providers (61, 62), pediatric providers demonstrated a great deal of variability and biases around fertility preservation counseling. The fact that providers are influenced by a stated desire for parenthood is in contrast to many adolescents’ perception that fertility preservation is a means of preserving a future choice rather than a statement about parenting intention. A clinical approach that standardizes the offering of such services may address the needs of adolescents and parents and overcome potential barriers identified by providers and has been recommended for young adults facing fertility decisions (63). Incorporating and normalizing these services and ongoing conversations about sexual and reproductive health will meet the needs of adolescents as they continue along their developmental trajectory and transition to survivor care. Adult models for fertility and reproductive care during cancer diagnosis utilize standing protocols and navigators that streamline the process for families, reduce the workload on providers who feel ill equipped to provide the information families desire, and ensure that feedback from families is incorporated into ongoing quality improvement(64-67). Initiating conversations and referrals early in the treatment process would meet adolescents’ and parents’ needs and address the growing number of experimental and clinically available options for fertility preservation in this population.
Acknowledgments
NIH,U54HD071598 (DA Flockhart & JL Renbarger, Co-PI) & LEAH Training Grant HRSA T71MC00008. This work was presented at a poster session for the 2014 Society for Adolescent Medicine Annual Meeting.
List of abbreviations
- FP
fertility preservation
References
- 1.Smith MA, Altekruse SF, Adamson PC, Reaman GH, Seibel NL. Declining childhood and adolescent cancer mortality. Cancer. 2014;120(16):2497–506. doi: 10.1002/cncr.28748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nature Reviews Cancer. 2014;14(1):61–70. doi: 10.1038/nrc3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005;83(6):1622–8. doi: 10.1016/j.fertnstert.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Fallat ME, Hutter J. Preservation of fertility in pediatric and adolescent patients with cancer. Pediatrics. 2008;121(5):e1461–9. doi: 10.1542/peds.2008-0593. [DOI] [PubMed] [Google Scholar]
- 5.Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: american society of clinical oncology clinical practice guideline update. J Clin Oncol. 2013 Jul 1;31(19):2500–10. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matthews ML, Hurst BS, Marshburn PB, Usadi RS, Papadakis MA, Sarantou T. Cancer, fertility preservation, and future pregnancy: a comprehensive review. Obstetrics and gynecology international. 2012;2012 doi: 10.1155/2012/953937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawshaw M. Psychosocial oncofertility issues faced by adolescents and young adults over their lifetime: a review of the research. Human Fertility. 2013;16(1):59–63. doi: 10.3109/14647273.2012.733480. [DOI] [PubMed] [Google Scholar]
- 8.Goossens J, Delbaere I, Van Lancker A, Beeckman D, Verhaeghe S, Van Hecke A. Cancer patients’ and professional caregivers’ needs, preferences and factors associated with receiving and providing fertility-related information: A mixed-methods systematic review. Int J Nurs Stud. 2013 Jul 16; doi: 10.1016/j.ijnurstu.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer. 2013 Apr 30;108(8):1602–15. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vadaparampil ST, Hutchins NM, Quinn GP. Reproductive Health in the Adolescent and Young Adult Cancer Patient: an Innovative Training Program for Oncology Nurses. Journal of Cancer Education. 2013 Mar;28(1):197–208. doi: 10.1007/s13187-012-0435-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loren AW, Brazauskas R, Chow EJ, Gilleece M, Halter J, Jacobsohn DA, et al. Physician perceptions and practice patterns regarding fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplant. 2013 Aug;48(8):1091–7. doi: 10.1038/bmt.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fallat ME, Hutter J. Preservation of fertility in pediatric and adolescent patients with cancer. Pediatrics. 2008;121(5):e1461–9. doi: 10.1542/peds.2008-0593. [DOI] [PubMed] [Google Scholar]
- 13.Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005 Jun;83(6):1622–8. doi: 10.1016/j.fertnstert.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Quinn GP, Murphy D, Knapp C, Stearsman DK, Bradley-Klug KL, Sawczyn K, et al. Who Decides? Decision Making and Fertility Preservation in Teens With Cancer: A Review of the Literature. Journal of adolescent health. 2011;49(4):337–46. doi: 10.1016/j.jadohealth.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clayman M, Galvin K, Arntson P. Oncofertility Fertility Preservation for Cancer Survivors. US: Springer; 2007. Shared decision making: fertility and pediatric cancers; pp. 149–160. [DOI] [PubMed] [Google Scholar]
- 16.Galvin KM, Clayman ML. Whose future is it? Ethical family decision making about daughters’ treatment in the oncofertility context. Cancer Treat Res. 2010;156:429–45. doi: 10.1007/978-1-4419-6518-9_33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bower B, Quinn GP. Fertility preservation in cancer patients: Ethical considerations. In: Quinn GP, Vadaparampil ST, editors. Reproductive health and cancer in adolescents and young adults. New York, NY US: Springer Science + Business Media; 2012. pp. 187–96. [DOI] [PubMed] [Google Scholar]
- 18.Bjork M, Wiebe T, Hallstrom I. Striving to survive: families’ lived experiences when a child is diagnosed with cancer. J Pediatr Oncol Nurs. 2005 Sep-Oct;22(5):265–75. doi: 10.1177/1043454205279303. [DOI] [PubMed] [Google Scholar]
- 19.Kars MC, Duijnstee MS, Pool A, Van Delden JJ, Grypdonck MH. Being there: parenting the child with acute lymphoblastic leukaemia. J Clin Nurs. 2008;17(12):1553–62. doi: 10.1111/j.1365-2702.2007.02235.x. [DOI] [PubMed] [Google Scholar]
- 20.Woodgate RL, Degner LF. A substantive theory of Keeping the Spirit Alive: the Spirit Within children with cancer and their families. J Pediatr Oncol Nurs. 2003 May-Jun;20(3):103–19. doi: 10.1053/jpon.2003.75. [DOI] [PubMed] [Google Scholar]
- 21.Dixon-Woods M, Bonas S, Booth A, Jones DR, Miller T, Sutton AJ, et al. How can systematic reviews incorporate qualitative research? A critical perspective. Qualitative research. 2006;6(1):27–44. [Google Scholar]
- 22.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005 Jul;10(Suppl 1):6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 23.McDermott E, Graham H, Hamilton V. Experiences of being a teenage mother in the UK: A report of a systematic review of qualitative studies. Lancaster University; Lancaster: 2004. [Google Scholar]
- 24.Thomas J, Harden A, Oakley A, Oliver S, Sutcliffe K, Rees R, et al. Integrating qualitative research with trials in systematic reviews. BMJ. 2004 Apr 24;328(7446):1010–2. doi: 10.1136/bmj.328.7446.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris J. Using qualitative research to develop robust effectiveness questions and protocols for Cochrane systematic reviews. In: Noyes J, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. 1st. Cochrane Collaboration Qualitative Methods Group; Aug, 2011. [Google Scholar]
- 26.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008. [Google Scholar]
- 27.Centre for reviews, dissemination (CRD) Systematic reviews: CRD’s guidance for undertaking reviews in health care. Centre for Reviews and Dissemination; 2009. [Google Scholar]
- 28.Harden A, Thomas J. Methodological issues in combining diverse study types in systematic reviews. International Journal of Social Research Methodology. 2005;8(3):257–71. [Google Scholar]
- 29.Levine J, Canada A, Stern CJ. Fertility preservation in adolescents and young adults with cancer. J Clin Oncol. 2010 Nov 10;28(32):4831–41. doi: 10.1200/JCO.2009.22.8312. [DOI] [PubMed] [Google Scholar]
- 30.Goossens J, Delbaere I, Van Lancker A, Beeckman D, Verhaeghe S, Van Hecke A. Cancer patients’ and professional caregivers’ needs, preferences and factors associated with receiving and providing fertility-related information: A mixed-methods systematic review. Int J Nurs Stud. 2013 Jul 16; doi: 10.1016/j.ijnurstu.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 31.Booth A. Chapter 3: Searching for Studies. In: Noyes J, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Cochrane Collaboration Qualitative Methods Group; 2011. [Google Scholar]
- 32.Noyes J, Lewin S. Chapter 6: Supplemental Guidance on Selecting a Method of Qualitative Evidence Synthesis, and Integrating Qualitative Evidence with Cochrane Intervention Reviews. In: Noyes J, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. 1st. Cochrane Collaboration Qualitative Methods Group; Aug, 2011. [Google Scholar]
- 33.Hannes K. Chapter 4: Critical appraisal of qualitative research. In: Noyes J, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. 1st. Cochrane Collaboration Qualitative Methods Group; Aug, 2011. [Google Scholar]
- 34.Noyes J, Lewin S. Chapter 5: Extracting qualitative evidence. In: Noyes J, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. 1st. Cochrane Collaboration Qualitative Methods Group; Aug, 2011. [Google Scholar]
- 35.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme. 2006;1 Version. [Google Scholar]
- 36.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Preventive medicine. 2007;45(4):247–51. doi: 10.1016/j.ypmed.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 37.Edge B, Holmes D, Makin G. Sperm banking in adolescent cancer patients. Archives of Disease in Childhood. 2006;91(2):149–52. doi: 10.1136/adc.2005.075242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chapple A, Salinas M, Ziebland S, McPherson A, Macfarlane A. Fertility issues: the perceptions and experiences of young men recently diagnosed and treated for cancer. Journal of adolescent health. 2007;40(1):69–75. doi: 10.1016/j.jadohealth.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 39.Crawshaw MA, Glaser AW, Hale JP, Sloper P. Young males’ experiences of sperm banking following a cancer diagnosis - a qualitative study. Hum Fertil (Camb) 2008 Dec;11(4):238–45. doi: 10.1080/14647270802132752. [DOI] [PubMed] [Google Scholar]
- 40.Crawshaw MA, Glaser AW, Hale JP, Sloper P. Male and female experiences of having fertility matters raised alongside a cancer diagnosis during the teenage and young adult years. Eur J Cancer Care (Engl) 2009 Jul;18(4):381–90. doi: 10.1111/j.1365-2354.2008.01003.x. [DOI] [PubMed] [Google Scholar]
- 41.Ginsberg JP, Ogle SK, Tuchman LK, Carlson CA, Reilly MM, Hobbie WL, et al. Sperm banking for adolescent and young adult cancer patients: sperm quality, patient, and parent perspectives. Pediatr Blood Cancer. 2008 Mar;50(3):594–8. doi: 10.1002/pbc.21257. [DOI] [PubMed] [Google Scholar]
- 42.Gorman JR, Bailey S, Pierce JP, Su HI. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012 Jun;6(2):200–9. doi: 10.1007/s11764-011-0211-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yeomanson DJ, Morgan S, Pacey AA. Discussing fertility preservation at the time of cancer diagnosis: Dissatisfaction of young females. Pediatr Blood Cancer. 2013 Jul;:8. doi: 10.1002/pbc.24672. [DOI] [PubMed] [Google Scholar]
- 44.Burns KC, Boudreau C, Panepinto JA. Attitudes regarding fertility preservation in female adolescent cancer patients. Journal of Pediatric Hematology/Oncology. 2006;28(6):350–4. doi: 10.1097/00043426-200606000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Nieman CL, Kinahan KE, Yount SE, Rosenbloom SK, Yost KJ, Hahn EA, et al. Fertility preservation and adolescent cancer patients: lessons from adult survivors of childhood cancer and their parents. Cancer Treat Res. 2007;138:201–17. doi: 10.1007/978-0-387-72293-1_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van den Berg H, Repping S, van der Veen F. Parental desire and acceptability of spermatogonial stem cell cryopreservation in boys with cancer. Hum Reprod. 2007 Feb;22(2):594–7. doi: 10.1093/humrep/del375. [DOI] [PubMed] [Google Scholar]
- 47.Sadri-Ardekani H, Akhondi MM, Vossough P, Maleki H, Sedighnejad S, Kamali K, et al. Parental attitudes toward fertility preservation in boys with cancer: context of different risk levels of infertility and success rates of fertility restoration. Fertil Steril. 2013 Mar 1;99(3):796–802. doi: 10.1016/j.fertnstert.2012.11.030. [DOI] [PubMed] [Google Scholar]
- 48.de Vries MC, Bresters D, Engberts DP, Wit JM, van Leeuwen E. Attitudes of physicians and parents towards discussing infertility risks and semen cryopreservation with male adolescents diagnosed with cancer. Pediatr Blood Cancer. 2009 Sep;53(3):386–91. doi: 10.1002/pbc.22091. [DOI] [PubMed] [Google Scholar]
- 49.Crawshaw M, Glaser A, Hale J, Sloper P. Professionals’ view on the issues and challenges arising from providing a fertility preservations service sperm banking to teenage males with cancer. Human Fertility. 2004;7(1):23–30. doi: 10.1080/1464727042000198087. [DOI] [PubMed] [Google Scholar]
- 50.Reebals JF, Brown R, Buckner EB. Nurse practice issues regarding sperm banking in adolescent male cancer patients. J Pediatr Oncol Nurs. 2006 Jul-Aug;23(4):182–8. doi: 10.1177/1043454206289868. [DOI] [PubMed] [Google Scholar]
- 51.Goodwin T, Oosterhuis BE, Kiernan M, Hudson MM, Dahl GV. Attitudes and practices of pediatric oncology providers regarding fertility issues. Pediatric Blood and Cancer. 2007;48(1):80–5. doi: 10.1002/pbc.20814. [DOI] [PubMed] [Google Scholar]
- 52.Vadaparampil ST, Clayton H, Quinn GP, King LM, Nieder M, Wilson C. Pediatric oncology nurses’ attitudes related to discussing fertility preservation with pediatric cancer patients and their families. J Pediatr Oncol Nurs. 2007 Sep-Oct;24(5):255–63. doi: 10.1177/1043454207303878. [DOI] [PubMed] [Google Scholar]
- 53.Clayton H, Quinn GP, Lee J, King LM, Miree CA, Nieder M, et al. Trends in clinical practice and nurses’ attitudes about fertility preservation for pediatric patients with cancer. Oncology Nursing Forum. 2008;35(2):249–55. doi: 10.1188/08.ONF.249-255. [DOI] [PubMed] [Google Scholar]
- 54.Anderson RA, Weddell A, Spoudeas HA, Douglas C, Shalet SM, Levitt G, et al. Do doctors discuss fertility issues before they treat young patients with cancer? Hum Reprod. 2008 Oct;23(10):2246–51. doi: 10.1093/humrep/den252. [DOI] [PubMed] [Google Scholar]
- 55.Vadaparampil S, Quinn G, King L, Wilson C, Nieder M. Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns. 2008 Sep;72(3):402–10. doi: 10.1016/j.pec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 56.Quinn GP, Vadaparampil ST, King L, Miree CA, Wilson C, Raj O, et al. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009 Dec;77(3):338–43. doi: 10.1016/j.pec.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 57.Quinn GP, Vadaparampil ST. Fertility Preservation and Adolescent/Young Adult Cancer Patients: Physician Communication Challenges. Journal of adolescent health. 2009;44(4):394–400. doi: 10.1016/j.jadohealth.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 58.Kohler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J Assist Reprod Genet. 2011 Mar;28(3):269–77. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quinn GP, Knapp C, Murphy D, Sawczyn K, Sender L. Congruence of reproductive concerns among adolescents with cancer and parents: pilot testing an adapted instrument. Pediatrics. 2012 Apr;129(4):e930–6. doi: 10.1542/peds.2011-2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Quinn GP, Murphy D, Knapp CA, Christie J, Phares V, Wells KJ. Coping styles of female adolescent cancer patients with potential fertility loss. Journal of adolescent and young adult oncology. 2013;2(2):66–71. doi: 10.1089/jayao.2012.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer. 2013 Apr 30;108(8):1602–15. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shimizu C, Kato T, Tamura N, Bando H, Asada Y, Mizota Y, et al. Perception and needs of reproductive specialists with regard to fertility preservation of young breast cancer patients. International journal of clinical oncology. 2014;20(1):82–9. doi: 10.1007/s10147-014-0676-4. [DOI] [PubMed] [Google Scholar]
- 63.Linkeviciute A, Boniolo G, Chiavari L, Peccatori FA. Fertility preservation in cancer patients: the global framework. Cancer Treat Rev. 2014;40(8):1019–27. doi: 10.1016/j.ctrv.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 64.Kelvin JF, Reinecke J. Institutional approaches to implementing fertility preservation for cancer patients. In: Quinn GP, Vadaparampil ST, editors. Reproductive health and cancer in adolescents and young adults. New York, NY US: Springer Science + Business Media; 2012. pp. 165–73. [DOI] [PubMed] [Google Scholar]
- 65.Reinecke JD, Kelvin JF, Arvey SR, Quinn GP, Levine J, Beck LN, et al. Implementing a systematic approach to meeting patients’ cancer and fertility needs: a review of the Fertile Hope Centers Of Excellence program. J Oncol Pract. 2012 Sep;8(5):303–8. doi: 10.1200/JOP.2011.000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scott-Trainer J. The role of a patient navigator in fertility preservation In: Oncofertility. Springer; 2010. pp. 469–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sheth KR, Sharma V, Helfand BT, Cashy J, Smith K, Hedges JC, et al. Improved fertility preservation care for male patients with cancer after establishment of formalized oncofertility program. J Urol. 2012 Mar;187(3):979–86. doi: 10.1016/j.juro.2011.10.154. [DOI] [PubMed] [Google Scholar]


