Abstract
Introduction
Design and provision of good quality maternity care should incorporate what matters to childbearing women. This qualitative systematic review was undertaken to inform WHO intrapartum guidelines.
Methods
Using a pre-determined search strategy, we searched Medline, CINAHL, PsycINFO, AMED, EMBASE, LILACS, AJOL, and reference lists of eligible studies published 1996-August 2016 (updated to January 2018), reporting qualitative data on womens’ childbirth beliefs, expectations, and values. Studies including specific interventions or health conditions were excluded. PRISMA guidelines were followed.
Data collection and analysis
Authors’ findings were extracted, logged on a study-specific data form, and synthesised using meta-ethnographic techniques. Confidence in the quality, coherence, relevance and adequacy of data underpinning the resulting themes was assessed using GRADE-CERQual. A line of argument synthesis was developed.
Results
35 studies (19 countries) were included in the primary search, and 2 in the update. Confidence in most results was moderate to high. What mattered to most women was a positive experience that fulfilled or exceeded their prior personal and socio-cultural beliefs and expectations. This included giving birth to a healthy baby in a clinically and psychologically safe environment with practical and emotional support from birth companions, and competent, reassuring, kind clinical staff. Most wanted a physiological labour and birth, while acknowledging that birth can be unpredictable and frightening, and that they may need to ‘go with the flow’. If intervention was needed or wanted, women wanted to retain a sense of personal achievement and control through active decision-making. These values and expectations were mediated through womens’ embodied (physical and psychosocial) experience of pregnancy and birth; local familial and sociocultural norms; and encounters with local maternity services and staff.
Conclusions
Most healthy childbearing women want a positive birth experience. Safety and psychosocial wellbeing are equally valued. Maternity care should be designed to fulfil or exceed womens’ personal and socio-cultural beliefs and expectations.
Introduction
Optimum outcomes for pregnant women and their babies depend on acceptable, affordable, accessible, high quality provision of maternity care during pregnancy, childbirth, and the postnatal period [1]. However, the overuse of interventions in some contexts, and the underuse in others [2], along with growing evidence of disrespectful and abusive behaviors in some institutional settings [3,4] demonstrates that many maternity services are not meeting these standards. Good quality intrapartum care is vital, both for women and babies who are healthy, and for the minority who experience complications. Basing maternity service design and care provision on what women want and need is essential to maximize uptake of, and continuing access to, service provision [5]. If local maternity care provision is limited, women may report that they are satisfied, even if they have had poor quality care, as they will not be aware of any better alternatives. Finding out what matters to women about labour and birth (rather than only asking about their actual experiences of intrapartum care) offers the potential to establish what women value, irrespective of what is actually on offer. This could provide a basis for service improvement, locally, and internationally.
Transformational health care, as envisioned by the Global Strategy for Women’s, Children’s and Adolescent Health [6], requires maternity services to go beyond survival during childbirth. Understanding what outcomes are important to women is critical to developing clinical guidelines and policies that are women-centered, and that are more likely to ensure that women, babies and families thrive as well as survive following childbirth, with the ultimate aim of positive transformation of their lives, and those of their families and communities, in the short and longer term. The objective of this review was, therefore, to explore what matters to healthy women in relation to labour and birth. The findings have informed the framing and development of WHO intrapartum guideline recommendations, and the scope of outcomes to assess optimal intrapartum maternity care in future.
Methods
We conducted a systematic qualitative review in accordance with the PRISMA guidelines (See S1 Table for PRISMA Checklist). We included studies where the focus was on healthy pregnant women, who are the majority of those accessing intrapartum care around the world. Study assessment included the use of a validated quality appraisal tool [7]. Meta-ethnographic techniques [8] were used for analysis and synthesis, and GRADE-CERQual [9] was applied to the resulting themes.
Reflexive note
In keeping with quality standards for rigor in qualitative research [7] the review authors considered their views and opinions on intrapartum care as possible influences on the decisions made in the design and conduct of the study, and, in turn, on how the emerging results of the study influenced those views and opinions. All authors believed at the outset that most maternity care around the world is currently designed to maximize efficiency and to manage risk through precautionary interventions, with less emphasis on the experience of labour and birth for the mother, baby, and attending birth companions. All believed that positive labour experiences are important for the wellbeing of the mother, baby, and the family, in the short and longer term. Refutational analytic techniques [8] were therefore used to minimize the risk that these pre-suppositions would influence the analysis and the interpretation of the findings.
Search strategy
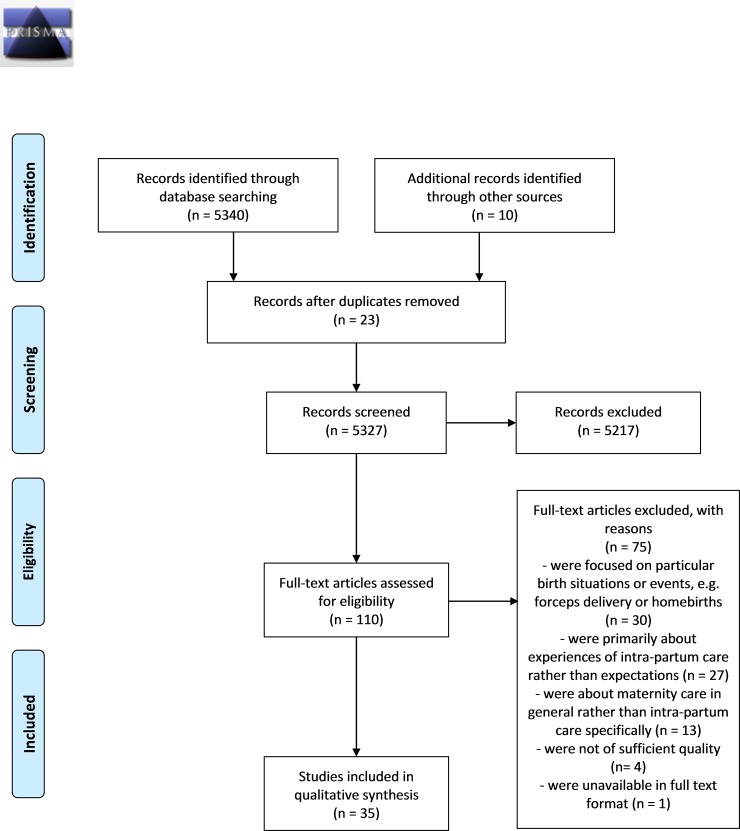
An example of the search terms used is given in Fig 1.
Fig 1. Search strategy [example].
In summary, the search terms were run in four broad strings covering population, intervention, outcome, and study type, with a view to capturing a wide selection of relevant studies. The terms were developed following a number of a priori scoping exercises across several databases. Where possible, relevant qualitative research limiters were used (e.g. Clinical Queries—Qualitative: Best Balance) to ensure that searches for qualitative studies were optimized. In instances where preliminary searches generated more than 3000 hits the Boolean operator ‘NOT’ was used to exclude studies that were unlikely to relate to the topic of interest. For example, NOT breastfeeding or breast-feeding or diabet* or contracepti* or HIV or anomol* [Ti,Ab]
Inclusion/Exclusion criteria
No language restrictions were applied. Titles and/or abstracts of potentially relevant studies published in languages other than English were initially translated using a basic translation package (Google Translate). If this process suggested the study would be relevant, the full text was translated in detail by bi or multi-lingual colleagues at The University of Central Lancashire (UCLan) or the World Health Organization (WHO).
Studies published before 1996 were excluded, to ensure that the findings reflect the current generation of women who encounter modern intra-partum care. Only studies where the main focus was the beliefs and expectations of women about labour and childbirth (and not studies where the intent was to collect reflections on intrapartum services actually provided) were included. Studies were included if they reported on women’s views directly (and not through staff or partner opinion, or observational data), and where the views were of the general population of healthy women. Studies were excluded if they focused on a particular intervention (e.g epidural use) or procedure (e.g. episiotomy) or represented the views of specific subgroups of women with particular health problems (e.g. obesity, diabetes, pre-eclampsia, etc;). The views of women who were expecting to have a caesarean section for clinical reasons were also excluded.
KF screened the initial hits against the inclusion criteria and referred any queries to SD for discussion. Abstracts and full text papers were included based on consensus between KF and SD.
Data sources
We searched the following databases: Medline, CINAHL, PsycINFO, AMED, EMBASE, LILACS (for studies conducted in South America) and AJOL (for studies conducted in Africa). Searches were conducted between 25th July and 4th August 2016. Reference lists of included papers were scrutinized (backchained) and included as appropriate. Zetoc alerts were set up for over 50 relevant journals. Details of included papers were logged on a study specific excel file. An updated search was carried out for papers published between August 2016 and January 2018. The results were used as a confirmability check for the original findings.
Quality assessment
The included studies were subject to quality appraisal using the instrument developed by Walsh and Downe [7] and modified by Downe et al [10]. This is a simple appraisal system that rates studies against 11 criteria, and then allocates a score from A-D to each study, based on the extent to which it demonstrated credibility, transferability, dependability, and conformability.
Studies scoring D (‘Significant flaws that are very likely to affect the credibility, transferability, dependability and/or confirmability of the study’) were excluded on quality grounds. [See S1 Appendix for details of Quality Assessment]
Analytic strategy
The analytic process followed the method of Noblitt and Hare [8], which is derived from the constant comparison method [11]. In step one, the included papers were examined, and an index paper was selected, chosen to best reflect the focus of the review [12]. The themes and findings identified by the authors of this paper were entered onto a spreadsheet, to develop an initial thematic framework. The findings of all the remaining papers were then mapped to this framework, which continued to develop as the data from each paper were added [13]. This process includes looking for what is similar between papers (‘reciprocal analysis’), and for what contradicts (‘disconfirms’) the emerging findings (‘refutational analysis’). For the refutational process, as we added each included paper to the analysis, we consciously looked for data that could disconfirm our emerging themes, or our prior beliefs and views related to the topic of the review. If any disconfirming data were found, the themes were amended, so that they continued to capture all the data from the papers we had already analyzed, as well as taking account of the new insights. This process also ensured that the final analysis had high explanatory power for all the data. [See S1 Appenedix for details of thematic development]
The themes were all agreed by consensus between KF and SD, and subject to appraisal by all members of the review team. All were directly derived from quote material in more than one of the included studies. They were assessed for confidence in the quality, coherence, relevance and adequacy of the data contributing to them using the GRADE-CERQual tool [9]. This is a recently developed instrument, derived from the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach used in quantitative effectiveness reviews. The GRADE-CERQual assessment results in a final classification of confidence in the theme in four categories: ‘high’, ‘moderate’, ‘low’ or ‘very low’. [See S1 Appendix for details of CERQual assessments]
All the themes were translated (or synthesized) into a ‘line of argument synthesis’ [8], based on theoretical concepts that explained the data at a conceptual level. The line of argument is more than the sum of the parts of the review. A robust line of argument has high theoretical transferability beyond the particular included studies, and so it is likely to be applicable in a wider range of settings and circumstances. The line of argument formed the basis for a Statement of Findings that was then used to inform the ‘values’ component of the Evidence to Decision frameworks used as the basis of the development of the WHO Intrapartum Care guideline (2018).
Results
Included studies
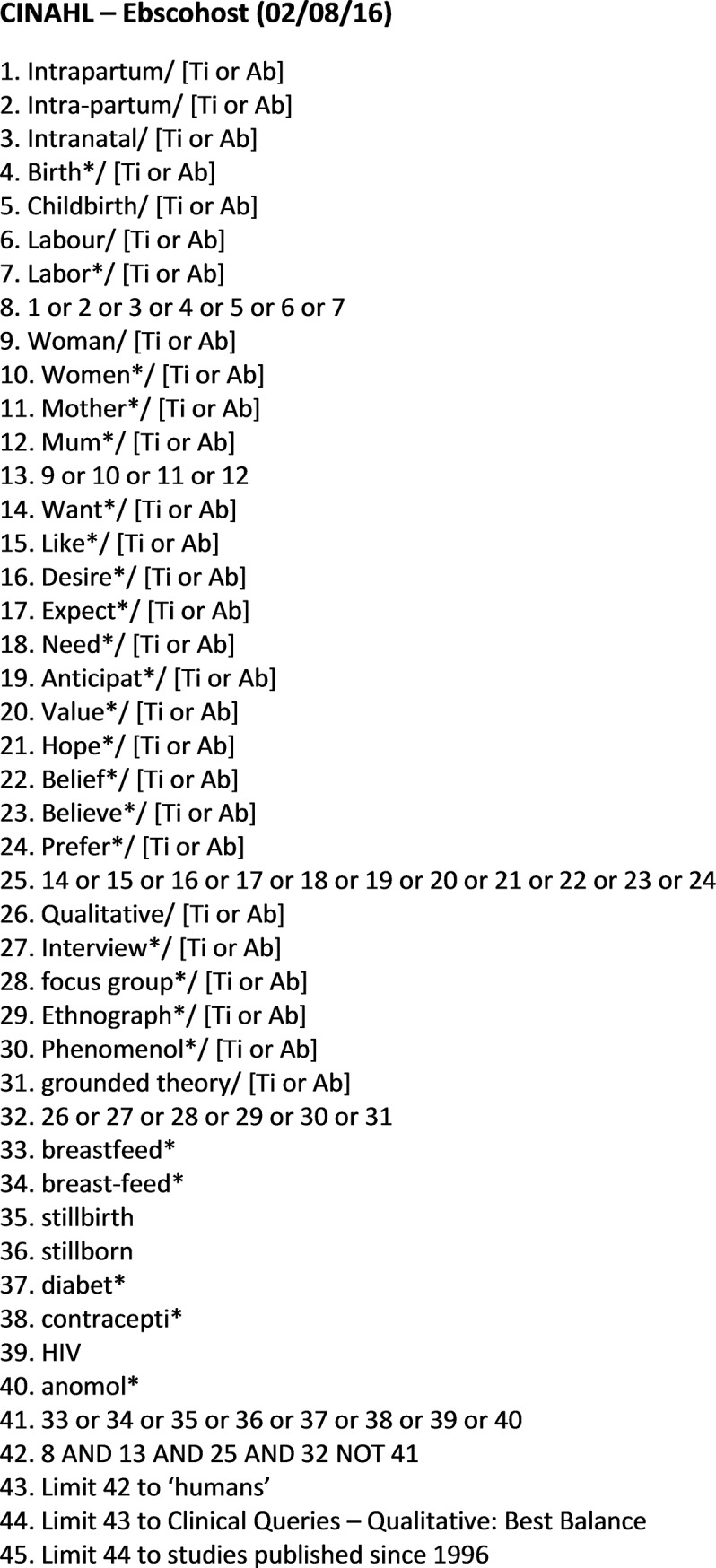
The primary search strategy generated a total of 5350 hits, including 10 already known to the authors. Twenty-three duplicate studies were removed, leaving 5327 to be screened. 5217 of these studies were excluded by title or abstract, primarily because they were deemed to be unrelated to the topic of interest. The remaining 110 were taken forward for full text review. A further 71 were excluded at this stage. The reasons for exclusion are shown in Fig 2.
Fig 2. PRISMA flow diagram.
Of the 39 full text papers, four were excluded after quality appraisal [14–17]. Two were relatively small Brazilian studies with little or no methodological information [14, 15], one was a mixed methods review with limited qualitative data [16] and one had limited methodological information[17]. Thirty five papers were included in the final analysis. Post-hoc examination of the four papers excluded on quality grounds indicated that inclusion of the data within them would not have changed the final themes, line of argument, or Summary of Findings statement.
There were no additional studies from the Zetoc alerts.
The updated search generated 26 hits (after screening by title) and a further 2 studies were identified [18, 19].
Characteristics and quality of included studies (primary search)
The characteristics and quality of the 35 included studies were tabulated, and are summarized in Table 1.
Table 1. Included studies: Characteristics and quality rating (primary search).
| Code | Authors | Setting | Study design | Participant selection | Sample size | Date | Country | Quality |
|---|---|---|---|---|---|---|---|---|
| 2 | Callister, Holt & West Kuhre | Urban | In depth interviews | Convenience sampling | Interviews with 17 women | 2010 | Australia | B+ |
| 3 | Fenwick et al | Urban/rural | Telephone interviews | Random based on response to a newspaper advert | 202 women's narratives: open ended survey question | 2005 | Australia | A- |
| 4 | Maier | Urban | Feminist perspective, interviews | Unclear—randomly recruited at an antenatal clinic | Interviews with 27 women | 2010 | Australia | C+ |
| 5 | Hauck et al | Urban/rural | In depth interviews | Purposive sampling with women from phase 1 of the study (see 15) | Interviews with 20 women (11 multiparous & 9 primiparous) | 2007 | Australia | B+ |
| 6 | Malacrida & Boulton | Largely urban | Feminist Foucaultian ethnographic | Variety of methods including e-mail, adverts and snowball sampling | Interviews with 21 women | 2014 | Canada | B+ |
| 7 | Malacrida & Boulton | Urban | Social constructionism, feminist, interviews | Brief details incorporating random (via e-mail and adverts) and snowball sampling | Interviews with 22 women | 2012 | Canada | B |
| 8 | Callister, Eads & Diel | Urban | In-depth interviews | Snowball sampling | 34 women of Chinese origin | 2011 | China & USA | B |
| 9 | Murray | Urban | Ethnographic: observations, interviews, field notes | Unclear—researcher worked with informants over a 1 year period | Repeated interviews, 16 women, pre & post-natal | 2012 | Chile | C+ |
| 10 | Melender | Urban and rural | In-depth interviews | Purposive sampling; rural and urban locations, low and high risk women | Interviews with 24 pregnant women | 2006 | Finland | A- |
| 11 | Halldorsdottir & Karlsdottir | Urban | Phenomenological interviews | Unclear—'through a network of colleagues' | Reflexive interviews with 14 women | 1996 | Iceland | B- |
| 12 | Aune et al | Urban | In depth interviews informed by salutogenic theory | Selective sampling; women who self- identified with positive birth experience | Interviews with 12 women who had given birth | 2015 | Norway | B+ |
| 13 | Lundgren | Urban | Phenomenological in-depth interviews | Unclear—randomly selected group from a purposive sample via another study | 11 women (5 primiparous & 5 multiparous) | 2005 | Sweden | B- |
| 14 | Rilby et al | Urban | Open ended survey | Follow up to a larger survey based study using prospective sampling | 908 women (respondents to open ended survey) | 2012 | Sweden | B- |
| 15 | Brodrick | Urban | In-depth interviews | Random; those meeting inclusion criteria | 8 women (all primiparous) | 2008 | UK | B |
| 16 | Gibbins & Thomson | Urban | Husserlian Phenomenology | Purposive | 8 women, pre/ postnatal | 2001 | UK | A- |
| 17 | Proctor | Urban | Focus groups and interviews | Limited detail—maximum variation | 33 women (19 pre and 14 post-natal) [and 47 staff] | 1998 | UK | C+ |
| 18 | Highsmith | Urban | In-depth interviews based on pre-natal drawings of participants 'ideal birth' |
No details | 8 women interviewed before and after birth |
2006 | USA | B+ |
| 19 | Martin, Bulmer & Pettker | Urban | Husserlian phenomenology, (semi-structured interviews) | Non probability purposive sampling at an antenatal clinic | Interviews with 7 women | 2013 | USA | B |
| 21 | Marin et al | Urban | In depth interviews | As part of a longitudinal study | Interviews with 7 women | 2009 | Brazil | C+ |
| 22 | Pinheiro & Bittar | Urban | Interviews and observations | No details—random? | 25 pregnant women and 2 postnatal mothers | 2013 | Brazil | C+ |
| 23 | Dias & Deslandes | Urban | Interviews and ethnographic observations | Unclear—purposive sample of multiparous women at a prenatal clinic | Interviews with 22 women | 2006 | Brazil | C+ |
| 24 | Nakano et al | Urban | Social constructionism; in-depth interviews | Convenience: women attending a vaccination clinic at 1 month post-natal | 20 women, 1 month post-natal, attending a vaccination clinic | 2012 | Brazil | B |
| 25 | Raven et al | Rural | Interviews and focus groups | Purposive sampling at a variety of hospitals but no details | 35 individual interviews, 5 focus groups (69 women) | 2015 | China | B- |
| 26 | Craig & Kabylbekova | Urban | Focus groups | Random, then snowball sampling | 2 focus groups (21 women) | 2015 | Kazakhstan | B- |
| 27 | Chuahorm et al | Semi-urban | Grounded theory: interviews, field notes & observations | Purposive initially followed by theoretical sampling based on participant characteristics | 20 women interviewed 48 hours after delivery and again 1 month later | 2007 | Thailand | B |
| 28 | Sercekus & Okumus | Urban | Interviews | Purposive sample of women attending an outpatient clinic | Interviews with 19 women | 2009 | Turkey | B- |
| 29 | Callister et al | Urban | Ethnographic principles: interviews and observations | Unclear—appears to be random on the post-natal ward | Interviews with 32 women | 2010 | Ecuador | B |
| 30 | D'ambruoso, Abbey & Hussein | Semi-urban | Qualitative, focus groups and latterly interviews | Opportunistic as part on a wider study | 2 focus groups with women and a further 21 interviews | 2005 | Ghana | B |
| 31 | Wilkinson & Callister | Rural | Ethnography (health belief model): interviews, observations, field notes | Random selection at clinic then snowball sampling to women in outlying villages | Interviews with 24 women | 2010 | Ghana | A- |
| 32 | Corbett & Callister | Rural | Unclear—ethnographic? | Initially convenience in post-partum unit followed by snowball sampling | Interviews with 22 women | 2012 | India | B+ |
| 33 | Sharma, Christenssen & Johansson | Rural | Grounded theory: focus groups, interviews field notes & observations | Unclear | Focus groups with 85 women (childless, pregnant and mothers) | 2012 | India | A- |
| 34 | Okwako & Symon | Urban | Phenomenological interviews | Convenience sample at an antenatal clinic | 14 In depth interviews with 7 women (pre & post-natal) | 2014 | Kenya | B+ |
| 35 | Gomi | Rural | Qualitative, some ethnographic approaches | Unclear | In depth interviews; 9 women: & stakeholders | 2013 | Bangladesh | C |
| 36 | Kaphle et al | Rural | Social constructionist incorporating theories of oppression and feminism | Purposive sample of a variety of participants in a remote location | Interviews with 25 pregnant or post-natal women and associated stakeholders | 2013 | Nepal | A- |
| 37 | Regmi & Madison | Rural | Unclear—In depth interviews | Unclear—described as purposive but no details of recruitment or strategy | Interviews with 15 women & 8 mothers-in-law; focus group (8 women); | 2009 | Nepal | C+ |
The date range of publication for the results of the primary search was 1996–2015. All regions of the world were represented. By continent, the largest number of studies were based in Europe (n = 9) [20–28], (UK x3, Sweden x2, Finland, Iceland, Norway, Turkey), and Asia (n = 9) [29–37], (China x2, India x2, Nepal x2, Bangladesh, Kazakhstan, Thailand). Six were from South America [38–43], (Brazil x4, Chile, Ecuador), four from North America [44–47], (Canada x2, USA x2), four from Australasia [48–51] and three from Africa [52–54], (Ghana x2, Kenya).
Most data were collected by individual interviews and/or focus or discussion groups. The papers incorporated a range of methodological approaches from relatively small phenomenological studies, to qualitative analysis of free text survey responses. They represented the views of more than 1800 women, from a wide range of ethnic backgrounds, ages (14–49) and socio-demographic groups. The quality was mostly moderate to high (B or above).
The eligible papers from the updated search were scrutinised to assess similarities or differences between the results generated from the primary review, and the themes and findings in the more recent studies.
Findings
Table 2 presents the themes emerging from the synthesis of the data, along with codes, subthemes, and related quotes from the included studies, and the GRADE-CERQual rating of the sub-themes (‘evidence statements’). The numbers used in this table are indexed to the appropriate study in superscript in the reference list below.
Table 2. Themes emerging from the data (primary search).
| Codes | Relevant Studies | CERQual Grading | Supporting data | Subthemes | Summary themes |
|---|---|---|---|---|---|
| Belief in a 'Normal Birth' (without medical intervention). | 18 Studies– 20, 22, 23, 27, 30, 33, 37, 39, 41, 42, 44, 45, 47, 48, 49, 50, 51, 54 | High | It will be a challenging experience both physically and emotionally but yes, I guess my expectations are to be able to give birth naturally with the least amount of intervention49 | There is value in the experience of using one’s own physical and psychosocial capacities to labour, and to give birth to a healthy baby | Hope for a positive birth experience; anticipating triumph and delight, fearing pain and abandonment |
| Want a healthy baby - | 15 Studies– 21, 24, 37, 39, 40, 42, 43, 45, 46, 47, 49, 50, 51, 52, 53 | High | ….after-all what is important is the goal of the activity: to come out as a live and healthy mother with a healthy baby52. | ||
| Belief in the transcendence of birth | 6 Studies– 24, 43, 44, 46, 48, 54 | Low | I didn’t think [about childbirth being a spiritual experience] at the time, but looking back I do. I think it’s just the way you connect with your baby in a way that you’ve probably never connected with anything. It gives you a whole different perspective on your spiritual side48 | ||
| Want to hold their baby | 2 Studies– 45, 46 | Very Low | I didn’t get to hold my baby right away, I didn’t get to look into her eyes undrugged for who knows how long. I did get to hear her cry for the first time, but still, it was kind of delusional with all the medication and everything else … I started crying and thinking, ‘I really, really missed out’45 | ||
| Fear of Childbirth | 13 Studies– 20, 21, 24, 31, 36, 37, 39, 40, 41, 46, 49, 51, 53 | High | I'm worried about delivery. This worries me every day!. . . . And they say 'but do not think about it!'. I say: I doubt there's a pregnant woman who does not think of the time of delivery!39 | Birth is inherently unpredictable, potentially frightening and usually painful: these emotions and sensations can be increased or diminished by expectations or experiences of care provision | |
| Expect to go with the flow | 7 Studies –20, 23, 27, 44, 47, 49, 51 | Moderate | I know what my ideal is however I may need something else for the pain, it may not go to plan… I will just go with the flow20 | ||
| Expect labour and birth to be painful | 7 Studies– 21, 24, 28, 37, 46, 47, 48 | Moderate | I was afraid that my birth might be so difficult that I would need a caesarean birth. I was afraid of exhaustion … I was afraid of pain from being cut. I feared that it would be painful after birth37 | ||
| No expectations | 2 Studies– 21, 26 | Very Low | You see, it all came as a surprise to me. The birth itself and everything. But I presume it is only in the first birth, with the first baby you never know really what to expect26 | ||
| Value the support of a birth companion | 14 Studies– 20, 21, 22, 25, 26, 29, 30, 36, 38, 39, 41, 45, 46, 47 | High | What matters is that he’ll just be there … and as I actually said to my husband, now that I think of this childbirth, I want you to be there just as last time … that you hold me so that I can hide there … I mean … I wouldn’t have coped without him25. | ||
| Want continuity of carer | 4 Studies– 21, 22, 30, 42 | Low | I think it would be good to be looked after in labour by a midwife I know. I like the midwives I have seen. There is one in particular I feel as if I have got on quite well with her. She is very reassuring and I think it would be ideal if she were going to be there, then that would be great. But she won't, it will be a different team of people22 | ||
| Need for a safe and supportive environment | 12 Studies– 20, 25, 26, 27, 28, 30, 32, 45, 46, 52, 53, 54 | High | At a certain stage [in the birth experience] you start to want, you start to yearn for this caring, you start to yearn for. somehow you are exhausted and you have been doing this for so long and then you just want someone to be kind to you and you know., feel sorry for you and just help you. You just realise that you can't do this alone and then you need a midwife., who you can feel is dedicated., that encourages you and …tells you that you can do it, that you are doing OK that it will be OK.26 | ||
| Fear of being alone | 10 Studies– 24, 27, 28, 32, 36, 37, 38, 39, 41, 54 | Moderate | Last time I was left alone and I did not have my sister, mother or anybody around. My husband was turned away54 | ||
| Expectations influenced by family and friends. | 14 Studies– 27, 28, 29, 30, 33, 34, 39, 41, 42, 44, 47, 49, 50, 53 | Moderate | My mum had five children…my mum told us about being born….she had four home births and one hospital birth, so she told me what it was like and what she has gone through so I think that was a big influence49 | Familial and societal norms | The enduring influence of familial and sociocultural norms and beliefs |
| Expectations influenced by media. | 4 Studies– 23, 46, 47, 49 | Very Low | I always go on the Internet, I signed up for all those pregnancy weekly kind of things, and I [sic] always constantly reading my book and everything, and to see about stuff that can happen47 | ||
| Acknowledgment of traditional beliefs. | 5 Studies– 29, 31, 33, 34, 53 | Moderate | if you insult people who are witches, they can plot against you during your [pregnancy] and they can fight at your birth53 | The power of cultural beliefs | |
| Expect staff to be sensitive, caring and kind: | 17 Studies– 20, 22, 23, 24, 25, 26,30, 31, 37, 40, 41, 42, 47, 51, 52, 53, 54 | High | …She [Midwife] was great, she looked straight into my eyes and came to me and touched me warmly, in a personal way …like she was saying 'I am with you' …you know, an empowering touch which makes you stronger because you can sense that someone is with you in this … The birth progressed very fast after she came, incredibly faster than before … and I did not suffer such torment as before she came26 | Staff philosophies, attitudes, behaviours and skills are critically important | Enacting what matters in the context of what is available |
| Fear of staff being distant, insensitive or rude. | 8 Studies– 20, 24, 28, 37, 38, 42, 50, 52 | Moderate | It was inhumane. I came [to a public hospital] with high blood pressure (…) the obstetrician started with a vaginal exam and from then onwards I had contractions every five minutes (…) the older women in the room having their second child told me “Don’t listen and don’t say anything because these fools mistreat you when you complain.” I kept quiet and fainted a few times but no one noticed. I heard a midwife telling the woman next to me saying: “What do you complain about? Didn’t you like “it”?42 | ||
| Expect health professionals to be skilled and competent. | 6 Studies– 22, 24, 25, 30, 32, 51 | Moderate | They should be good at watching labour, doing the delivery, and abdominal delivery. Very good skills. The doctor must not hurry and can control everything, making me feel relaxed30 | ||
| Fear of medical intervention. | 4 Studies– 28, 32, 45, 53 | Low | I really, really was opposed to being induced–I feel that that is the beginning of the end for natural childbirth45 | Childbirth interventions or external controlling forces feared or welcomed | |
| Want to have medical intervention(s). | 6 Studies– 28, 30, 41, 44, 50, 51 | Low |
They are telling me to have a normal delivery. I don’t want a normal delivery, I’m really scared, I want a caesarean, have them put me to sleep and when I wake up I want my baby next to be. That’s what I want.28 |
||
| Hope for a quick labour. | 6 Studies– 21, 25, 29, 38, 45, 54 | Low |
I mean that if childbirth would be prolonged for some reason, the child not beginning to arrive… as some have been in labor for 48 hours or so, I hope of course that it would be easier for me25 |
||
| Handing over control (to medical staff/God). | 10 Studies– 20, 23, 33, 38, 41, 42, 43, 45, 50, 53 | Moderate | You have to pray so that you leave everything to God, so that God will take control… During that time, everything is in prayer. You will be praying… every time. From the time that you knew that you were almost ready to deliver, you start praying and you make your mind set that you are going to give birth to the child53 |
The findings suggest that, with high or moderate confidence, most women around the world hope for a labour and birth experience that enables them to use their inherent physical and psychosocial capacities to labor and give birth to a healthy baby in a clinically, culturally, and psychologically safe environment with continuity of practical and emotional support from a birth companion(s), and with kind, sensitive clinical staff, who provide reassurance and technical competency. Most women place a high value on their capacity to give birth physiologically (expressed variously as ‘normal’ or ‘natural’, or without technical or pharmacological interventions) for the short and longer term physical and psychological wellbeing of themselves, their baby and their family; however, they also acknowledge that birth can be an unpredictable and potentially frightening event, and that they may need to ‘go with the flow’. Even where intervention is needed or wanted, women usually wish to retain a sense of personal achievement and control by being involved in decision making.
This is summarized in three overarching themes: Hoping for a positive birth experience: anticipating triumph and delight, fearing pain and abandonment; the enduring influence of familial and socio- childbirth norms; and Enacting what matters in the context of what is available.
These themes generated the following line of argument:
For most childbearing women across the world, there is inherent value in being able to use one’s own physical and psychosocial capacities to labour, and to give birth to a healthy baby, even when the process is unpredictable and painful. Beliefs about what matters to women are influenced by familial experiences, and local cultural norms and values. The capacity for women to enact what matters to them is affected by anticipated or actual encounters with maternity care staff and services, including the use of desired, required, and/ or feared childbirth interventions.
The themes and findings in the papers included in the updated search confirmed the review findings, suggesting that the analysis is robust, and theoretically transferable to a range of women and settings around the world.
Discussion
For most of the respondents in the included studies, childbirth was an important experience, which had characteristics of what has been termed ‘liminality’: the transition stage between one state and another during a life-changing rite of passage [55]. For a small minority, childbirth was simply a physical process that should be conducted as quickly and painlessly as possible. As with other life-transition experiences, many women were fearful in anticipation of the hard work, pain, and uncertainty of labour, but most of them accepted these (potentially extreme) difficulties as part of the necessary process of achieving a positive, or even transformatory, birth experience for themselves and for their baby. Whatever they thought about the nature of birth, women interpreted their expectations of what could and should happen through the lens of family birth stories, and cultural and social norms. Whether women wanted birth over as quickly and painlessly as possible, or whether they understood it as fundamental to their transition to motherhood, they recognized the potential vulnerability of themselves and their baby through the process, and the essential uncertainty about what might happen. This was associated with a strong desire for safe, supportive, kind, respectful and responsive care during labor and birth. These characteristics applied to birth companions, professional and lay care givers, and to the processes and environment of care. The extent to which women could experience what mattered to them was mediated by the nature of the local maternity care provision that was available to them, including the attitudes and behaviours of staff, the quality of the relationship between women and care providers, and the resources and atmosphere of the local facility.
To our knowledge, this is the first meta-synthesis of what matters to women for labour and birth, as opposed to studies of women’s experiences once they have been through the process. Systematic reviews are inevitably dependent on the nature and quality of data that have already been collected and reported. In reviews of qualitative studies, these data have already been interpreted through the lens of what is seen to be important by the primary authors. Too few studies, from too narrow a cultural context, can limit the external transferability of the findings. Although the intent was to only include studies that reported on womens’ a priori views and expectations about what matters to them for labour and birth, independent of any intrapartum care they may have received, in some cases participants views were inevitably informed by their actual experiences.
However, the findings are strengthened by the inclusion of a large number of studies, covering every region of the world, and by the confirmatory analysis carried out as a result of the updated search.
The use of translation software at the inclusion stage of the review could theoretically have led to the exclusion of some relevant papers. In the event, 4 studies (from the primary search) that were included as a consequence of software translation were in languages other than English (3 in Portuguese and 1 in Japanese). The findings of all of these papers were translated by fluent speakers of the relevant language, and they were consistent with the papers written in English. The final analysis was consistent for women in all regions of the world. GRADE-CERQual assessments indicated that confidence in most of the findings was moderate or high, reflecting the quantity and quality of the included studies, and the wide range of settings, viewpoints, and study types included.
The findings largely reinforce the prior beliefs of the authors, which could suggest that different reviewers might have come to different conclusions. However, this risk was limited by the conscious search for disconfirming data to test the emerging codes, subthemes, and main themes.
The findings apply directly to healthy women of a range of parity, and in a range of cultural and economic settings, who are receiving routine intrapartum care. The review did not include studies that were only focused on women with specific health conditions, such as HIV or diabetes, or women from particular marginalised groups, such as those seen as ethnic or cultural outsiders, or very young or very poor women. However, women from some of these groups were part of the respondent sample in some of the included studies, and individual studies of the views of women who are marginalised suggest that the review findings are highly likely to be transferable [56–59].
Facility birth is generally accepted as a solution to persistently high rates of maternal and neonatal mortality and morbidity. However, since Bowser and Hill published their analysis of disrespect and abuse in institutional birth settings, in 2010 [60], there has been an increasing recognition that, while providing central facilities for maternity care is necessary for the provision of care to women and/or babies with complications, this strategy is not sufficient to ensure optimal outcomes for all women and babies [3]. Recent WHO antenatal guidelines incorporate evidence from qualitative systematic reviews, indicating that women value the psychological, cultural and emotional experience of pregnancy as well as the health of themselves and their growing baby [61, 62]. These reviews have also revealed that women experience pregnancy, birth, and the postnatal period as a psychological and physical continuum, and not as three distinct and un-related states. The current review adds to this body of evidence, by linking what women perceive as a positive labour and birth to local familial and cultural norms that shape the way that childbirth is framed, and by expressing the limitations on how far women believe they can actually enact a positive experience of labour and birth, depending on the available maternity care provision locally.
The findings support the multiple domains of the Lancet Quality of Maternal and Newborn Care Framework [5], and of the 2015 WHO Quality of Care Framework for Maternal and Newborn Health [1]. The former takes a human rights perspective, and incorporates a systematic review of what women want and need. The framework recognizes the importance of safe, accessible, evidence based, respectful care provision, and is based on a philosophy of care that optimizes physiological, psychological and cultural norms and values. The latter links the experience of care with provision of care, evidence based practices for routine care and management of complications, actionable information systems and functional referral systems, as well as competent and motivated human resources and essential physical resources.
The findings of this review also complement the Cochrane effectiveness reviews on midwife-led continuity of care [63] and continuous support in labour [64]. The finding that most women would prefer not to have labour interventions unless they are necessary for the safety of their baby and/or themselves is reinforced by the recent Lancet Maternal Health series, in which the excessive over-use of intrapartum interventions in both HIC and LMIC countries is shown to be potentially as serious a problem at the population level as the lack of availability of such interventions when they are life-saving [2].
Conclusions
This review demonstrates that what matters to women in relation to childbirth is underpinned by three phenomena; the physical and psychosocial narture of birth as an embodied experience; local familial and socio-cultural norms that legitimate or reframe expectations about labour and birth; and how maternity care provision enables or restricts what matters. Whether women perceive childbirth to be a transformatory process that has meaning for them and their baby in the short and longer term, or whether they see it as a necessary process that should be completed as quickly and painlessly as possible, maternity services need to be responsive to their values, beliefs, and needs. What matters to women is also what is likely to generate the safest and most humanized maternity care provision, for mother, baby, and the family. There is now sufficient evidence from a wide range of sources to suggest that it is imperative that maternity services recognize the benefits of providing what matters to women (and the risks of not doing so). Crucially, these factors should become a central component of care provision as a matter of urgency to ensure the optimum uptake of effective and respectful maternity care, and, as a consequence, the health of childbearing women and their babies and families, in both the short and longer-term.
Supporting information
(XLSX)
(DOC)
Acknowledgments
We thank Prof Erika Ota at St Lukes International University in Tokyo for translating the paper published in Japanese[35]. Mercedes Bonnet at the World Health Organization translated the papers published in Portuguese. With thanks also to Maeve Regan and Hannah Tizzard at The University of Central Lancashire for their help with the searching and screening process and to Claire Glenton and Simon Lewin at the Norwegian Institute of Public Health for their advice on using the GRADE CERQual tool.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was commissioned to the University of Central Lancashire, UK by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research, World Health Organization, Switzerland as part of the evidence base preparation for the WHO recommendations on intrapartum care. The development of the WHO recommendations on intrapartum care was financially supported by USAID. OTO, MB, and AMG are paid staff of the Department of Reproductive Health and Research, World Health Organization. SD and KF are members of Research in Childbirth and Health (ReaCH) group, University of Central Lancashire, UK. The manuscript represents the views of the named authors only. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tuncalp Were WM, MacLennan C, Oladapo OT, Gulmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns—the WHO vision. BJOG 2015; 122:1045–49. doi: 10.1111/1471-0528.13451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016. October 29; 388(10056):2176–92 doi: 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- 3.Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: a Mixed-Methods Systematic Review. PLoS Med 2015;12:e1001847 doi: 10.1371/journal.pmed.1001847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet 2014; 384:e42–4 doi: 10.1016/S0140-6736(14)60859-X [DOI] [PubMed] [Google Scholar]
- 5.Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014:384:1129–45 [Accessed 19th February 2018] doi: 10.1016/S0140-6736(14)60789-3 [DOI] [PubMed] [Google Scholar]
- 6.Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). New York: Every Woman Every Child; 2015. Available from http://globalstrategy.everywomaneverychild.org/ [Accessed 19th February 2018] [Google Scholar]
- 7.Walsh D, Downe S. Appraising the quality of qualitative research. Midwifery 2006; 22:108–19. doi: 10.1016/j.midw.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 8.Noblitt GW, Hare RD. Meta-Ethnography: Synthesizing Qualitative Studies Newbury Park, CA: Sage; 1988. [Google Scholar]
- 9.Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using Qualitative Evidence in Decision Making for Health and Social Interventions: An Approach to Assess Confidence in Findings from Qualitative Evidence Syntheses (GRADE-CERQual). PLoS Med 12(10): e1001895 [Accessed 19th February 2018] doi: 10.1371/journal.pmed.1001895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Downe S, Simpson L, Trafford K. Expert intrapartum maternity care: a meta-synthesis. J Adv Nursing 2007; 57:127–40. [DOI] [PubMed] [Google Scholar]
- 11.Strauss A, Corbin J. Grounded Theory in Practice Thousand Oaks, CA: Sage; 1997 [Google Scholar]
- 12.Fenwick J., Hauck Y., Downie J., Butt J. The childbirth expectations of a self-selected cohort of Western Australian women. Midwifery 2005; 21(1):23–35. doi: 10.1016/j.midw.2004.07.001 [DOI] [PubMed] [Google Scholar]
- 13.Schutz A. Collected papers, vol 1 The Hague: Martinus Nijhoff, 1962 [Google Scholar]
- 14.Basso JF, Monticelli M. Expectations of pregnant women and partners concerning their participation in humanized births. Rev. Latino-Am. Enfermagem 2010. May-Jun; 18(3):390–7. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira LA, Silva JAJ, Zuffi FB, Mauzalto ACM, Leite CP, Nunes JS. Expectation of pregnant women in relation to childbirth. R. pesq: cuid. Fundam Online 2013. apr/jun; 5(2):3692–97. doi: 10.9789/2175-5361.2013v5n2p3692 [Google Scholar]
- 16.Moore MF. Multicultural Differences in Women’s Expectations of Birth. The ABNF Journal 2016; 27(2): 39–43. [PubMed] [Google Scholar]
- 17.Bravo P, Uribe C, Contreras A. Care during the process of childbirth: a view from mothers. Rev Chil Obstet Gynecol 2008; 73(3):179–184. [Google Scholar]
- 18.Fleming V, Meyer Y, Frank F, van Gogh S, Schirinzi L, Michoud B, et al. Giving birth: Expectations of first time mothers in Switzerland at the mid point of pregnancy Women and Birth 2017; 30:443–449. doi: 10.1016/j.wombi.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 19.Ojelade OA, Titiloye MA, Bohren MA, Olutayo AO, Olalere AA, Akintan A, et al. The communication and emotional support needs to improve women’s experience of childbirth care in health facilities in Southwest Nigeria: A qualitative study. Int J Gynecol Obstet 2017; 139 (Suppl. 1): 27–37. [DOI] [PubMed] [Google Scholar]
- 20.Brodrick A. Exploring women’s pre-birth expectations of labour and the role of the midwife. Evidence Based Midwifery 2008. Available from https://www.rcm.org.uk/learning-and-career/learning-and-research/ebm-articles/exploring-women%E2%80%99s-pre-birth-expectations-of [Accessed 19th February 2018] [Google Scholar]
- 21.Gibbins J, Thomson AM. Women's expectations and experiences of childbirth. Midwifery 2001; 17: 302–13. doi: 10.1054/midw.2001.0263 [DOI] [PubMed] [Google Scholar]
- 22.Proctor S. What determines quality in maternity care? Comparing the perceptions of childbearing women and midwives. Birth 1998; 25(2):85–93. [DOI] [PubMed] [Google Scholar]
- 23.Lundgren I. Swedish women's experience of childbirth 2 years after birth. Midwifery 2005; 21:346–54 doi: 10.1016/j.midw.2005.01.001 [DOI] [PubMed] [Google Scholar]
- 24.Rilby L, Jansson S, Lindblom B, Martensson LB. A qualitative study of women's feelings about future childbirth: Dread and delight. J Midwifery Womens Health 2012; 57:120–25. doi: 10.1111/j.1542-2011.2011.00113.x [DOI] [PubMed] [Google Scholar]
- 25.Melender HL. "What Constitutes a Good Childbirth? A Qualitative Study of Pregnant Finnish Women". J Midwifery Womens Health 2006; 51:331–39. doi: 10.1016/j.jmwh.2006.02.009 [DOI] [PubMed] [Google Scholar]
- 26.Halldorsdottir S, Karlsdottir SI. Journeying through labour and delivery: perceptions of women who have given birth. Midwifery 1996; 12:48–61. [DOI] [PubMed] [Google Scholar]
- 27.Aune IA, Torvik HM, Selboe ST, Skogås AK, Persen J, Dahlberg U. Promoting a normal birth and a positive birth experience—Norwegian women's perspectives. Midwifery 2015; 31:721–27. doi: 10.1016/j.midw.2015.03.016 [DOI] [PubMed] [Google Scholar]
- 28.Sercekus P, Okumus H. Fears associated with childbirth among nulliparous women in Turkey. Midwifery 2009; 25:155–62. doi: 10.1016/j.midw.2007.02.005 [DOI] [PubMed] [Google Scholar]
- 29.Callister LC, Eads MN, Diel JP. Perceptions of Giving Birth and Adherence to Cultural Practices in Chinese Women. MCN Am J Matern Child Nurs 2011. Nov-Dec;36(6):387–94. doi: 10.1097/NMC.0b013e31822de397 [DOI] [PubMed] [Google Scholar]
- 30.Raven J, van den Broek N, Tao F, Kun H Tolhurst R. The quality of childbirth care in China: women’s voices: a qualitative study. BMC Pregnancy and Childbirth 2015; 15:113 doi: 10.1186/s12884-015-0545-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corbett CA, Callister LC. Giving Birth: the voices of women in Tamil Nadu, India. MCN Am J Matern Child Nurs 2012. September; 37(5):298–305. doi: 10.1097/NMC.0b013e318252ba4d [DOI] [PubMed] [Google Scholar]
- 32.Sharma B, Giri G, Christensson K, Ramani KV, Johansson E. The transition of childbirth practices among tribal women in Gujarat, India: A grounded theory approach. BMC International Health and Human Rights 2013; 13:41 [Accessed 19th February 2018] doi: 10.1186/1472-698X-13-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaphle S, Hancock H, Newman LA. Childbirth traditions and cultural perceptions of safety in Nepal: Critical spaces to ensure the survival of mothers and newborns in remote mountain villages. Midwifery 2013; 29: 1173–81. doi: 10.1016/j.midw.2013.06.002 [DOI] [PubMed] [Google Scholar]
- 34.Regmi K, Madison J. Contemporary childbirth practices in Nepal: Improving outcomes. British Journal of Midwifery June 2009; 17(6):382–87. [Google Scholar]
- 35.Gomi M. Women's delivery care needs in rural Bangladesh: Recommendations for skilled birth attendants. J. Jpn. Acad. Midwif 2013; 27(2):226–36. [Google Scholar]
- 36.Craig BJ, Kabylbekova Z. Culture and Maternity Care in Kazakhstan: What New Mothers Expected. Health Care for Women International 2015; 36:41–56. doi: 10.1080/07399332.2014.942904 [DOI] [PubMed] [Google Scholar]
- 37.Chuahorm U, Sripichyakarn K, Tungpunkom P, Klunklin A, Kennedy HP. Fear and Suffering During Childbirth Among Thai Women. Thai Journal of Nursing Research 2007. Jan-Mar; 11(1):49–61. [Google Scholar]
- 38.Dias MAB, Deslandes SF. Patients' expectations regarding childbirth care at a public maternity hospital in Rio de Janeiro, Brazil: challenges for the humanization of obstetric care. Cad. Saúde Pública Rio de Janeiro. 2006; 22(12):2647–55. http://dx.doi.org/10.1590/S0102-311X2006001200014 [DOI] [PubMed] [Google Scholar]
- 39.Marin AH, Donelli TMS, Lopes RCS, Piccinini CA. Expectations and feelings of single mothers on the birth experience. Aletheia 2009. Jan-Jun; 29:57–72. [Google Scholar]
- 40.Nakano AMS, Ferreira CHJ, Almeida AM, Gomes FA. Childbirth experience according to a group of Brazilian primiparas. Midwifery 2012; 28:e844–e849. doi: 10.1016/j.midw.2011.09.014 [DOI] [PubMed] [Google Scholar]
- 41.Pinheiro BC, Bittar CML. Expectations, perceptions and experiences of normal birth: report of a group of women. Fractal, Rev. Psicol 2013; 25(3):585–602. http://dx.doi.org/10.1590/S1984-02922013000300011. [Google Scholar]
- 42.Murray M. Childbirth in Santiago de Chile: Stratification, intervention, and child centeredness. Medical Anthropology Quarterly 2012; 26(3): 319–37. doi: 10.1111/j.1548-1387.2012.01221 [DOI] [PubMed] [Google Scholar]
- 43.Callister LC, Corbett C, Reed S, Tomao C, Thornton KG. Giving Birth: the voices of Ecuadorian women. J Perinat Neonat Nurs 2009; 24(2):1–9. [DOI] [PubMed] [Google Scholar]
- 44.Malacrida C, Boulton T. Women's perceptions of childbirth choices. Gender & Society 2012; 26(5):748–72. doi: 10.1177/0891243212452630 [Google Scholar]
- 45.Malacrida C, Boulton T. The best laid plans? Women's choices, expectations and experiences in childbirth. Health 2014; 18(1):41–59. doi: 10.1177/1363459313476964 [DOI] [PubMed] [Google Scholar]
- 46.Highsmith S. Primiparas' expectations of childibirth: The impact of consciousness. Journal of Prenatal & Perinatal Psychology & Health Winter 2006; 21(2):141–78. [Google Scholar]
- 47.Martin DK, Bulmer SM & Pettker CM. Childbirth Expectations and Sources of Information among Low- and Moderate-Income Nulliparous Pregnant Women. The Journal of Perinatal Education 2012; 22(2):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Callister LC, Holt ST, Kuhre MW. Giving Birth down under: the voices of Australian women. J Perinat Neonat Nurs 2010; 24(2): 1–9. [DOI] [PubMed] [Google Scholar]
- 49.Fenwick J, Hauck Y, Downie J, Butt J. The childbirth expectations of a self-selected cohort of Western Australian women. Midwifery 2005. March; 21(1):23–35. doi: 10.1016/j.midw.2004.07.001 [DOI] [PubMed] [Google Scholar]
- 50.Maier B. Women's worries about childbirth: making safe choices. British Journal of Midwifery 2010. May; 18(5):293–99. [Google Scholar]
- 51.Hauck Y, Fenwick J, Downie J, Butt J. The influence of childbirth expectations on Western Australian women's perceptions of their birth experience. Midwifery 2007. September; 23(3):235–47. doi: 10.1016/j.midw.2006.02.002 [DOI] [PubMed] [Google Scholar]
- 52.D'ambruoso L, Abbey M, Hussein J. Please understand when I cry out in pain: women's accounts of maternity services during labour and delivery in Ghana. BMC Public Health 2005; 5:140 doi: 10.1186/1471-2458-5-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wilkinson SE, Callister LC. Giving birth: The voices of Ghanaian women. Health Care for Women International 2010; 31(3):201–220, doi: 10.1080/07399330903343858 [DOI] [PubMed] [Google Scholar]
- 54.Okwako JM, Symon AG. Women's expectations and experiences of childbirth in a Kenyan public hospital. African Journal of Midwifery and Women’s Health 2014. Jul-Sep; 8(3):115–21. https://doi.org/10.12968/ajmw.2014.8.3.115 [Google Scholar]
- 55.Van Gennep A. The rites of passage In: Davis-Floyd R, editor. Birth as an American rite of passage. Chicago, IL: University of Chicago Press; 1966. [Google Scholar]
- 56.Nyman VMK, Prebensen AK, Gullvi EM, Flensner GEM. Obese women's experiences of encounters with midwives and physicians during pregnancy and childbirth. Midwifery 2010; 26(4):424–29. doi: 10.1016/j.midw.2008.10.008 [DOI] [PubMed] [Google Scholar]
- 57.Kelly C, Alderdice F, Lohan M, Spence D. 'Every pregnant woman needs a midwife'—The experiences of HIV affected women in maternity care. Midwifery 2013. February; 29(2):132–38. doi: 10.1016/j.midw.2011.12.003 [DOI] [PubMed] [Google Scholar]
- 58.Small R, Roth C, Raval M, Shafiei T, Korfker D, Heaman M et al. Immigrant and non-immigrant women’s experiences of maternity care: a systematic and comparative review of studies in five countries. BMC Pregnancy and Childbirth 2014; 14:152 doi: 10.1186/1471-2393-14-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sauls DJ. Adolescents' Perception of Support During Labor. J Perinat Educ 2004. Fall; 13(4): 36–42. doi: 10.1624/105812404X6216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth: report of a landscape analysis Bethesda, Maryland, USA: USAID-TRAction Project, Harvard School of Public Health and University Research Corporation, LLC; 2010. [Google Scholar]
- 61.Downe S, Finlayson K, Tuncalp Ӧ, Gulmezoglu MA. What matters to women: a systematic scoping review to identify the processes and outcomes of antenatal care provision that are important to healthy pregnant women. BJOG 2016; 123(4):529–39; doi: 10.1111/1471-0528.13819 [DOI] [PubMed] [Google Scholar]
- 62.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience 2016; Geneva, Switzerland: World Health Organization. [PubMed] [Google Scholar]
- 63.Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews 2016, Issue 4 Art. No.: CD004667. doi: 10.1002/14651858.CD004667.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2017, Issue 7 Art. No.: CD003766. doi: 10.1002/14651858.CD003766.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.