Abstract
Background:
precursor emissions have declined over the course of several decades, following the implementation of local, state, and federal air quality policies. Estimating the corresponding change in population exposure and risk of death prior to the year 2000 is made difficult by the lack of monitoring data.
Objectives:
We used a new technique to estimate historical concentrations, and estimated the effects of changes in population exposures on mortality in adults (age ), and on life expectancy at birth, in the contiguous United States during 1980–2010.
Methods:
We estimated annual mean county-level concentrations in 1980, 1990, 2000, and 2010 using universal kriging incorporating geographic variables. County-level death rates and national life tables for each year were obtained from the U.S. Census and Centers for Disease Control and Prevention. We used log-linear and nonlinear concentration–response coefficients from previous studies to estimate changes in the numbers of deaths and in life years and life expectancy at birth, attributable to changes in .
Results:
Between 1980 and 2010, population-weighted exposures fell by about half, and the estimated number of excess deaths declined by about a third. The States of California, Virginia, New Jersey, and Georgia had some of the largest estimated reductions in deaths. Relative to a counterfactual population with exposures held constant at 1980 levels, we estimated that people born in 2050 would experience an increase in life expectancy at birth, and that there would be a cumulative gain of 4.4 million life years among adults of age.
Conclusions:
Our estimates suggest that declines in exposures between 1980 and 2010 have benefitted public health. https://doi.org/10.1289/EHP507
Introduction
Implementing the Clean Air Act has markedly improved outdoor air quality in the United States (U.S. EPA 2011a, 1997). The National Ambient Air Quality Standards for common air pollutants, first promulgated in the 1970s, set health-based ambient standards for six criteria pollutants: particulate matter, ground-level ozone, carbon monoxide, sulfur dioxide (), nitrogen dioxide (NOx), and lead (Bachmann 2007). Emissions of these pollutants have declined by about 60% since 1980 (U.S. EPA 2016). While ambient data for fine particle matter concentrations (those and smaller: ) were not regularly collected on an extensive spatial scale until the late 1990s (U.S. EPA 2016), concentrations of monitored pollutants that are precursors to , including in particular, have declined by approximately 80% during the period from 1980 to 2010 (U.S. EPA 2016).
Fine particles are of particular interest to health scientists and policy makers because of evidence from controlled human exposure, toxicological, and epidemiological studies that acute exposure (over hours or days) is associated with adverse health outcomes, including aggravated asthma, hospital and emergency department visits, and premature death (Brook et al. 2010; U.S. EPA 2009; WHO 2013). In addition, epidemiologic studies have consistently reported that chronic (i.e., years-long) exposure to fine particles is associated with an increased risk of premature death (U.S. EPA 2009; WHO 2013). Systematic reviews by the U.S. Environmental Protection Agency (U.S. EPA) and the World Health Organization have concluded that there is a causal relationship between short- and long-term exposure to fine particles and the risk of premature death (U.S. EPA 2009; WHO 2013).
Air pollution human health impact assessments have used findings from epidemiological studies to estimate the human health impacts of air quality policies. These assessments model emissions, air quality, and exposure to estimate counts and rates of adverse outcomes (Anenberg et al. 2011; Caiazzo et al. 2013; Fann et al. 2011a, 2011b, 2013; Lim et al. 2012; U.S. EPA 2009). Results of these analyses can help inform a chain of accountability that describes the events linking air quality policies to human health outcomes. As described by the Health Effects Institute, this chain includes five stages: a) regulatory action; b) changes in emissions; c) changes in ambient air quality; d) changes in exposure/dose; and e) human health responses (Health Effects Institute 2003). However, incomplete data on emissions, monitoring, personal exposure, and health outcomes have made it difficult to elucidate the links in this chain.
Photochemical transport models, such as the Community Multi-scale Air Quality Model, use archival emissions and meteorology data to predict pollutant concentrations (Byun and Schere 2006; U.S. EPA 2012a). The resolution of emissions inventories across sources and locations has improved since 2000, making it possible to model changes in air quality with greater confidence. However, prior to the advent of the extensive national regulatory monitoring network in late 1990s, it was difficult to characterize changes in ambient exposures over time and space, or estimate the subsequent effects of these changes on public health.
The Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air) developed a statistical model to estimate annual average concentrations during 1980–2010 at locations throughout the continental United States (Kim et al. 2017). This national point prediction model does not rely on inventoried emissions data, and can be used to estimate long-term average concentrations during 1980–2010 at any locations throughout the continental United States (Kim et al. 2017). This national point prediction model can be applied to estimate area-level long-term average concentrations that are representative of population exposures during 1980, 1990, 2000, and 2010. For the present analysis, we used this prediction model to estimate decadal trends in population-representative annual mean exposures to residents of the contiguous United States, and performed two analyses to estimate the influence of these multidecade changes in exposure on health. We used the first analysis to estimate the number of deaths that were avoided due to falling exposures during 1980–2010. Because air pollution health impact assessments report the number of individuals who die prematurely, but not the degree to which exposure to shortens their life spans, we also used a life table approach to estimate changes in population longevity through the year 2050. By estimating the human health effects of changes in exposures, these two assessments inform the final stage of the chain of accountability (HEI 2003).
Methods
Estimating Annual Mean Concentrations in 1980, 1990, 2000, and 2010
We estimated county average concentrations using a previously developed point-wise spatiotemporal prediction model of annual average concentrations in the contiguous United States for 1980–2010, as described elsewhere (Kim et al. 2017). This spatiotemporal prediction model for 1980–2010 was developed based on annual average concentration data from 1999 through 2010 obtained from the U.S. EPA Federal Reference Method and the Interagency Monitoring of Protected Visual Environments (IMPROVE) networks (Hand et al. 2011; U.S. EPA 2009) and backward projection of pollutant trends. The model included terms for a spatially varying long-term mean and a time trend, as well as spatial smoothing of available data from nearby monitors (Kim et al. 2017). The overall time trend was estimated using monitoring data for 1999–2010, which was back-extrapolated to estimate the temporal trend before 1999 based on extensive sensitivity analyses of trends for sulfate and visibility. The long-term mean and time trends were characterized in a universal kriging framework with geographic variables, and spatial smoothing was modeled by using an exponential covariance function. External validation of the model using other sources of data showed good model performance (Kim et al. 2017). For example, values were based on the data for 1990–1999 from IMPROVE and the Children’s Health Study (Peters et al. 1999; Sisler and Malm 2000). Incorporating emission and meteorological data did not significantly improve the performance of the model (Kim et al. 2017).
Using the spatiotemporal prediction model, we predicted annual average concentrations for 1980, 1990, 2000, and 2010 at about 70,000 census tract centroids from the 2010 census, which we assumed were representative of residence locations. These census tract centroids were created by using the 2010 census boundary maps downloaded from the National Historical Geographic Information System website (https://www.nhgis.org/). We next computed population-weighted county-level averages of predictions across census tract centroids within a county for each year, where the population weight was the census tract population divided by the total county population.
Estimating the Number of Deaths
Similar to previous studies (Hubbell et al. 2009a; Levy et al. 2002; Voorhees et al. 2011), we estimated the number of deaths using a health impact function. The function combines relative risk estimates from epidemiological studies (i.e., concentration–response functions representing the association between exposure and mortality) with estimated annual mean concentrations, population data, and baseline death rates for each county in each year. We derived these estimates using the Benefits Mapping and Analysis Program—Community Edition (BenMAP-CE, version 1.1, U.S. EPA) tool as described below.
We estimated the number of total deaths () during each year (, 1990, 2000, 2010) among adults aged 30 and above in each county ( where is the total number of counties) as
| [1] |
where is the risk coefficient for all-cause mortality for adults in association with exposure, is the baseline all-cause mortality rate for adults aged in county in year stratified in 10-y age bins, is annual mean concentration in county in year , and is the number of county adult residents aged in county in year stratified into 5-y age bins.
U.S. Census data for age-stratified population counts and county boundaries were stored within the BenMAP-CE tool for 3,109 contiguous U.S. counties in 2000 and 2010 (http://www.factfinder.census.gov); and corresponding data for 3,109 and 3,111 counties in 1980 and 1990, respectively, were obtained from the U.S. Census (NHGIS Database). County boundaries change over time, and so we assigned each set of death rates to the appropriate county boundary file for each year (NHGIS Database).
For baseline rates of death for adults aged 30–99, we selected county-level age-stratified all-cause death rates from the Centers for Disease Control (WONDER) database for each of the four years (CDC Wonder Database). In each of the four decadal periods in each county, we matched the age-stratified rate of death with the population count in that age range.
We used risk coefficients () drawn from a broadly cited long-term air pollution study of the extended American Cancer Society cohort (American Cancer Society Cancer Prevention Study II, CPS-II) (Krewski et al. 2009) and an impact assessment study of the same cohort (Nasari et al. 2016) to define concentration–response functions (Table 1). The first risk coefficient was the long-term hazard ratio for all-cause mortality reported in the most recent extended analysis of the CPS-II cohort (ages 30 and older) [hazard ratio 1.06; 95% confidence interval (CI): 1.04, 1.08 per increase in average concentrations in 1999–2000, adjusted for all individual-level and ecologic covariates] (Krewski et al. 2009) (Table 1). This risk coefficient has been applied in several recent air pollution health impact analyses (U.S. EPA 2011a, 2011c; Fann et al. 2011a, 2011c, 2012, 2013).
Table 1.
Risk coefficients of all-cause mortality for concentrations applied to the health impact function.
| Study | Study population | Likelihood weightc | (percentile)d | e | |
|---|---|---|---|---|---|
| Krewski et al. (2009)a | American Cancer Society Population ages | 0.005826 (0.000962) | – | – | – |
| Nasari et al. (2016)b | American Cancer Society Cancer Prevention Study ages | 0.0930 (0.00984)f | 0.036 | −5.43 (−5%) | 0.1 |
| 0.0802 (0.00843) | 0.080 | 1.38 (0%) | 0.1 | ||
| 0.0433 (0.00446) | 0.460 | 8.19 (5%) | 0.1 | ||
| 0.0398 (0.00412) | 0.324 | 9.04 (10%) | 0.1 | ||
| 0.0351 (0.00369) | 0.056 | 10.55 (25%) | 0.1 | ||
| 0.0666 (0.00704) | 0.044 | 1.38 (0%) | 0.2 |
Long-term hazard ratio for all-cause mortality reported in the most recent extended analysis of the American Cancer Society Cancer Prevention Study II (ages 30 and older) [hazard ratio 1.06; 95% confidence interval (CI): 1.04, 1.08 per increase in average concentrations in 1999–2000, adjusted for all individual-level and ecologic covariates).
This is the effect coefficient (per ) and standard error for each of the six log-linear concentration–response functions within a specific concentration range. Adjusted for individual-level and ecologic covariates.
We weighted the average of the six results using these likelihood weights.
This term determines the air quality level at which the c-r function curves.
Parameter controls the curvature of the weighting function, with larger values yielding shapes with less curvature.
This function would be specified in the BenMAP-CE tool as: .
The risk coefficient assumes a log-linear relationship between and mortality over all possible values of , such that there is no threshold concentration below which mortality falls to zero. This assumption is consistent with findings in previous studies, which reported no evidence of a population-level threshold in the relationship between long-term exposure to and mortality, and so we elected not to apply one in this health impact function (Crouse et al. 2012; Schwartz et al. 2008; U.S. EPA 2009).
There is some evidence suggesting that the assumption of a log-linear association between and mortality may not hold at high concentrations (Burnett et al. 2014; Pope et al. 2009b). In addition, the maximum concentration predicted for counties in the present analysis (about ) is higher than the maximum exposure in the CPS-II population from which the Krewski et al. (2009) risk coefficient was derived (about ). Therefore, we derived a second set of attributable mortality estimates using a nonlinear form of the concentration–response relationship reported by Nasari et al. (2016) that was also based on the extended CPS-II study population.
This nonlinear risk function allows the risk of mortality to vary at different concentrations, conditional on the values of two parameters, and . Nasari et al. (2016) used CPS-II population data to derive a concentration–response curve and 95% CIs based on an ensemble analysis of models with different values of and , with likelihood-based weights used to summarize the results. We used the same parameters [six paired values of and that contributed to the models in Nasari et al. (2016); these covered all weights greater than 0.001] to estimate county-specific numbers of deaths.
We performed a Monte Carlo simulation to construct an error distribution of estimated death counts using the standard error of risk coefficients reported in Krewski et al. (2009) and Nasari et al. (2016), respectively. We estimated total numbers of deaths in the continental United States for each year by summing the county-specific estimates, and reported the sums of the 2.5th and 97.5th percentiles of the Monte Carlo distributions as 95% CIs.
Estimating the Fraction of Deaths Attributable to
We calculated the fraction of all-cause deaths attributable to deaths in each county and year using the following function:
| [2] |
where is the estimated number of all-cause deaths, is the age-stratified baseline death rate, and is the age-stratified population, respectively, in county in year . Death rates for certain age strata were unavailable from the U.S. Census between 7 and 318 counties in 1980, either because data were missing or because the number of deaths were too small to report (e.g., in rural counties with small populations). For these counties, we imputed county-specific values using the median age-specific death rates for the United States as a whole. These imputed values represent about 3.2% of the total number of age-stratified county-level death rates. State-level estimates were derived by summing county-specific estimates.
Estimating Gains in Life Years and Life Expectancy at Birth Attributable to Declines in
We used a life table approach (Miller and Hurley 2003) to estimate national-level impacts on the number of years of life expected to remain at each age, and on life expectancy at birth, from 1980 to 2050. To estimate changes in life years and life expectancy values, we used the PopSim life table model, in the software BenMAP-CE (version 1.1; U.S. Environmental Protection Agency) as in a previous U.S. EPA analysis of changes in longevity associated with the provisions of the Clean Air Act (U.S. EPA 2011a). PopSim starts with a table reflecting the age-specific risk of death for a given starting year (i.e., 1980 here) and then adjusts the baseline hazard to account for the decrease (or increase) in air pollution-attributable risk of death, using national population-weighted changes in over time (Table 2) and a risk coefficient (Krewski et al 2009).
Table 2.
Summary statistics of county-specific annual average predictions and nationwide population-weighted annual average predictions (in ) in 1980, 1990, 2000, and 2010.
| Year | County-specific annual average | National population-weighted annual average | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Min | 10% | 25% | 50% | 75% | 90% | Max | Mean | SD | |||
| 1980 | 3,109 | 3.21 | 7.79 | 11.33 | 14.63 | 16.97 | 18.66 | 25.53 | 14.01 | 4.07 | 15.4 |
| 1990 | 3,111 | 2.95 | 6.93 | 9.72 | 12.43 | 14.30 | 15.81 | 21.80 | 11.92 | 3.34 | 15.1 |
| 2000 | 3,109 | 1.67 | 5.49 | 7.45 | 10.58 | 12.93 | 14.23 | 19.41 | 10.19 | 3.37 | 11.4 |
| 2010 | 3,109 | 1.32 | 4.81 | 6.48 | 8.25 | 9.36 | 10.38 | 13.36 | 7.90 | 2.10 | 8.8 |
Note: 10%, 25%, 50%, 75%, and 90% are percentiles. SD, standard deviation.
In brief, the model uses a Mortality Hazard Adjustment Factor (MHAF) to adjust gender-specific life table estimates of age-specific risks of death for a given baseline year (1980 in the present analysis) to account for the decrease (or increase) in air pollution–attributable risk of death. For the present analysis, the MHAF was derived for year (, 1981, 1982 through 2050) as
| [3] |
where is the fully adjusted risk coefficient for all-cause mortality in adults () in association with a increase in long-term exposure from Krewski et al. (2009), and is the national-scale population-weighted annual mean difference in concentration () in year (the start year to the year ) from the previous year.
We calculated the population-weighted annual mean concentration for all counties combined () in year as
| [4] |
where is the county-average concentration in county in year , is the population in county in year , and is the total population over all counties combined in year .
MHAF-adjusted survival estimates for each birth cohort in each year (through 2050) were compared with survival estimates for the same birth cohort if exposures were held constant at 1980 levels to estimate the years of life gained, and the change in overall life expectancy from birth, as a consequence of changes in exposures between 1980–2010. Our estimates assume a linear decrease in annual mean concentrations for intervening years between 1980, 1990, 2000, and 2010, and make the conservative assumption that there will be no further decline in mean concentrations from 2010 to 2050.
Results
Air Quality
The median estimated county-level annual mean concentration was in 1980, and decreased by during each decade through 2010 (Table 2). The estimated mean concentration at the 90th percentile decreased by almost half during 1980–2010 (from 18.66 to ). The standard deviation declined from 4 to 2 over this period, indicating reduced variation in county-level concentrations in the contiguous United States. Estimated mean population-weighted annual mean concentrations (over all counties combined) decreased from in 1980 to in 2010 (Table 2), though county-specific population-weighted concentration increased in some individual counties (such as Los Angeles County in California and Alleghany County in Pennsylvania) over this period (Figure S1).
Estimates of Premature Deaths, Life Years, and Life Expectancy
We estimated that there were 190,000 (95% CI: 130,000–240,000) premature deaths in 1980 using the risk coefficient from Krewski et al. (2009) and 280,000 (95% CI: 130,000–990,000) using the risk coefficients from Nasari et al. (2016). Corresponding estimates for 2010 were 120,000 (95% CI: 83,000–160,000) and 200,000 (95% CI: 43,000–1,100,000), respectively (Table 3). Proportional declines in the estimated numbers of deaths were less than declines in mean population-weighted concentrations because population sizes increased and baseline death rates decreased over the same time period. The estimated fraction of deaths for the contiguous United States were 8.6–12.7% in 1980 and 5.0–8.1% in 2010, depending on the risk coefficient used (Table 3).
Table 3.
Estimated numbers and fractions of deaths in adults in the continental United States in 1980, 1990, 2000, and 2010.
| Year | Estimated numbers of attributable deaths (95% confidence interval)a | Estimated percentage of total deaths attributable to | ||
|---|---|---|---|---|
| Krewski et al. (2009)b | Nasari et al. (2016)c | Krewski et al. (2009)b | Nasari et al. (2016)c | |
| 1980 | 190,000 (130,000–240,000) | 280,000 (130,000–990,000) | 8.63% | 12.74% |
| 1990 | 170,000 (110,000–220,000) | 260,000 (120,000–910,000) | 8.39% | 12.69% |
| 2000 | 140,000 (98,000–190,000) | 230,000 (79,000–990,000) | 6.40% | 10.21% |
| 2010 | 120,000 (83,000–160,000) | 200,000 (43,000–1,100,000) | 5.02% | 8.13% |
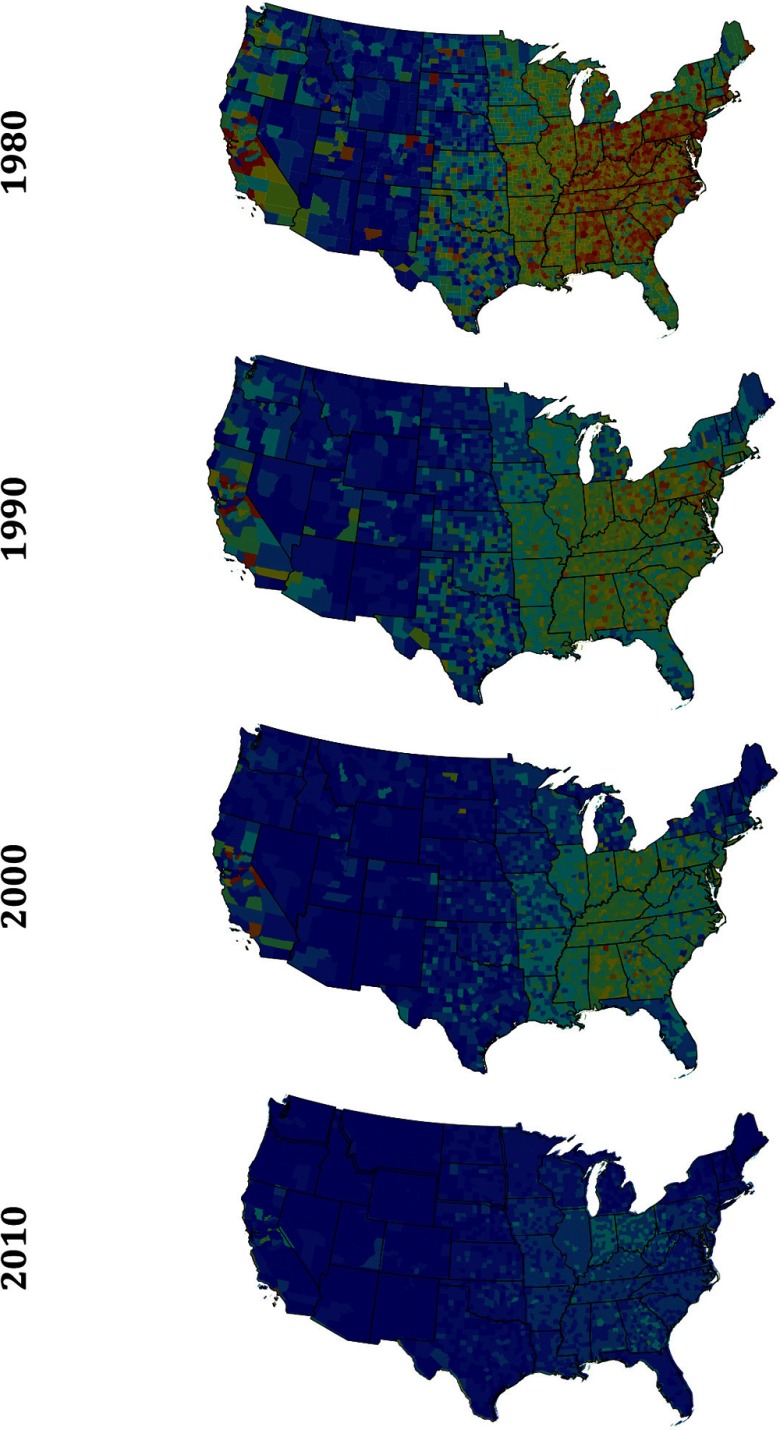
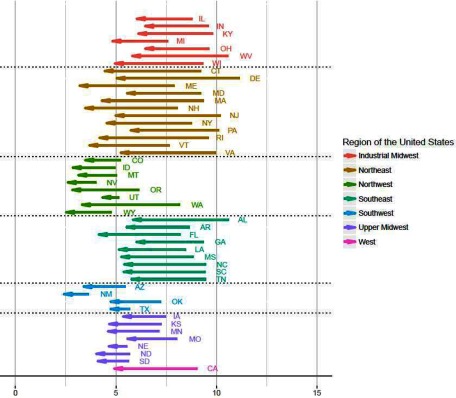
In 1980, the fraction of deaths, or mortality, was highest in the eastern United States and California, and in clusters of counties in western states, including Colorado, North Dakota, and Oregon (Figure 1). Statewide estimates of the mortality all indicated declines between 1980 and 2010, though the extent of the estimated decline varied among the states (Figure 2), and in a very small number of individual counties, mortality estimates increased over time (Figure S2). The average estimated reduction in mortality among states in the lowest quintile of mortality in 1980 () was low compared with the estimated reduction among the states in the highest quintile in 1980 () (Table S1).
Figure 1.
The fraction of total all-cause deaths attributable to in U.S. counties in the years 1980, 1990, 2000, and 2010 among adults ages 30 and older (calculated using risk coefficient from Krewski et al. 2009). State and county boundaries for each year drawn according to Census Topologically Integrated Geographic Encoding and Referencing (TIGER)/Line files as reported by the Minnesota Population Center National Historical Geographic Information System (NHGIS Database).
Figure 2.
Estimated reduction in Deaths in 48 U.S. states among adults Aged 30 and older between 1980 and 2010. Note: AL = Alabama; AR = Arkansas; AZ = Arizona; CA = California; CO = Colorado; CT = Connecticut; DE = Delaware; FL = Florida; GA = Georgia; IA = IOWA; ID = Idaho; IL = Illinois; IN = Indiana; KS = Kansas; KY = Kentucky; LA = Louisiana; MA = Massachusetts; MD = Maryland; ME = Maine; MI = Michigan; MN = Minnesota; MO = Missouri; MS = Mississippi; MT = Montana; NC = North Carolina; ND = North Dakota; NE = Nebraska; NH = New Hampshire; NJ = New Jersey; NM = New Mexico; NY = New York; OH = Ohio; OK = Oklahoma; OR = Oregon; PA = Pennsylvania; RH = Rhode Island; SC = South Carolina; SD = South Dakota; TN = Tennessee; TX = Texas; UT = Utah; VA = Virginia; VT = Vermont; WA = Washington; WI = Wisconsin; WV = West Virginia; WY = Wyoming. The region of the United States corresponds to seven clusters of states that are proximate to one another. The right-hand end of each arrow denotes the fraction of deaths due to in 1980, while the left-hand side of each arrow shows the fraction of deaths due to in 2010.
We estimate that the U.S. population will experience an increase in life expectancy due to reductions in annual mean concentrations from 1980–2010 (Table 4). Specifically, we estimate that because of declining concentrations between 1980 and 2010 (and resulting reductions in mortality), the life expectancy of U.S. residents born in 2050 will be almost 1 y longer than it would have been if had stayed constant at 1980 levels (0.94 and 0.87 additional y for men and women, respectively). In addition, we estimate that, as a group, U.S. adults who are born in 2050 will live 4.4 million more years than they would have lived if they had been exposed to at 1980 levels.
Table 4.
Estimated increase in life expectancy at birth and number of life years lived attributed to concentration reductions between 1980 and 2010 for individuals born in 1990, 2000, 2010, and 2050.
| Year of birth | Estimated increase in life expectancy at birtha,b,c | Cumulative number of life years gaineda,b,d | |
|---|---|---|---|
| Men | Women | ||
| 1990 | 0.01 | 0.01 | 7,800 |
| 2000 | 0.19 | 0.18 | 140,000 |
| 2010 | 0.43 | 0.61 | 640,000 |
| 2050 | 0.94 | 0.87 | 4,400,000 |
Estimates rounded to two significant figures.
The all-cause risk coefficient from Krewski et al. (2009) was used to estimate changes in life expectancy at birth and life years, under the assumption that has no effect on mortality prior to the age of 30.
Estimated increase in life expectancy at birth due to declines in from 1980–2010, relative to the estimated life expectancy for the same birth cohort if concentrations were fixed at 1980 concentrations.
Estimated cumulative increase in life years among adults of age in each birth cohort due to declines in concentrations from 1980–2010 compared with the estimated life years for the same birth cohort if concentrations were fixed at 1980 concentrations.
Discussion
To our knowledge, this is the first analysis to estimate national and local changes in ambient concentrations from 1980 to 2010, and subsequent changes in adult mortality, in the contiguous United States. We applied a new approach to estimate historical concentrations, including concentrations before the spatially extensive monitoring network was fully implemented in 1999. Using this approach, we estimated that annual average population-weighted exposures for the United States as a whole dropped by nearly half between 1980– 2010, while the U.S. population grew from 227 million to 309 million people (U.S. Census Bureau 2010).
Our estimates indicate that the human health burden of declined as exposures decreased between 1980 and 2010, with a 30–40% reduction in the estimated number of deaths depending on the mortality risk coefficient applied (Krewski et al. 2009 or Nasari et al. 2016). Our estimates of the number of deaths in 2000 and 2010 (140,000 and 120,000, respectively) are generally consistent with estimates reported by others (Anenberg et al. 2010; Caiazzo et al. 2013; Fann et al. 2011a, 2013). For example, Anenberg et al. (2010) estimated that exposures were responsible for approximately 124,000 cardiopulmonary deaths and 17,000 lung cancer deaths the United States and Canada in 2000, while Fann et al. (2011) estimated that exposures caused approximately 120,000 premature deaths in the United States in 2005.
Analyses using the pooled Nasari et al. (2016) all-cause risk coefficients yielded consistently larger estimates of deaths than analyses that used the all-cause risk coefficient from Krewski et al. (2009)—generally by a margin of about 90,000 deaths—and 95% CIs were much wider as well. However, regardless of the risk coefficient used, estimated numbers of premature deaths decreased between 1980 and 2010. Although we had anticipated that mortality estimates based on the Nasari et al. (2016) risk coefficients would decline at an increasing rate over time (given the slight sigmoidal shape of the concentration–response relationship), this did not occur, probably because the slope of the concentration–response curve was roughly constant over the range of estimated annual mean population-weighted concentrations during 1980–2010 (Table 2).
Air pollution health impact assessments for often report estimated numbers of individuals who die prematurely due to exposures, but not the degree to which exposure shortened their life spans. For this reason, we also estimated the additional life years gained and life expectancy at birth. Declining concentrations over the three-decade period were associated with a cumulative increase in the estimated number of life years gained over time, such that falling concentrations between 1980 and 1990 were estimated to result in thousands of additional life years by 1990, hundreds of thousands of additional life years by 2010, and millions of additional life years by 2050 (Table 3). Our estimates assumed that concentrations will remain constant from 2010–2050, but this may be a conservative assumption given the likelihood of further reductions in exposures due to local, state, and federal air quality policies implemented and promulgated after 2010 (U.S. EPA, 2010, 2011a, 2011b, 2011c, 2012a, 2012b, 2014a, 2014b).
It is not possible to directly compare our estimates with previous estimates given differences in analytic methods, baseline air quality data, and other inputs. Our estimate of an additional 0.2 y of life expectancy at birth for U.S. residents born in 2010 (relative to a counterfactual 2010 birth cohort with exposures fixed at 1980 levels) is smaller than previous estimates based on measured concentrations during a similar time frame. For example, using different methods than those employed here, Pope et al. (2009a) estimated an average additional 0.4 y of life expectancy at birth in the year 2000 among populations living in 211 counties from improved air quality between 1980 and 2000. Correia et al. (2013) estimated an additional 0.56 y of life expectancy at birth due to improved air quality between 1980 and 2007. Their longer years of life expectancy could be in part due to their approach using statistical models, while this analysis employed a life table approach.
Despite our conservative assumption holding future concentrations at 2010 levels, we estimate that reductions in exposures from 1980–2010 will increase the life expectancy of U.S. residents born in 2050 by almost 1 y relative to what their estimated life expectancy would have been if they had been exposed to concentrations at 1980 levels. If concentrations continue to decline as states implement provisions of the Clean Air Act, we would expect an even greater improvement in life expectancy due to declining exposures.
While our analysis clearly demonstrates that concentrations fell over this 30-y period, it is difficult to attribute this reduction to specific policy interventions. Although many factors are likely to have contributed to the decline in concentrations from 1980–2010, federal air quality policies are likely to have played an important role (Chestnut and Mills 2005; U.S. EPA 2011a). The Acid Rain program and the Clean Air Interstate and Cross-State Air Pollution rules each contributed to reductions in concentrations, which is a key precursor to forming (Hubbell et al. 2009b). Other rules contributed to reductions in precursor emissions from light duty, heavy duty, and nonroad vehicles (Fann et al. 2012; U.S. EPA 2014a).
Our estimates of PM-related mortality were calculated relative to a baseline rate of death in each decade. There is ample evidence that the life expectancy of the U.S. population has been increasing over time (Bell and Miller 2005; CDC 2011), and the Social Security Administration reported a particularly sharp decline in the number of cardiovascular deaths between 1981 and 2001. Other things being equal, a decline in the death rate will yield smaller estimates of air pollution related deaths in a health impact assessment, suggesting that some fraction of the reduced related deaths is partly a result of the population becoming healthier, more resilient, and less susceptible to the risk of death. On the other hand, previous studies using county-level data have reported that reductions in concentrations were associated with lower death rates, even after changes in demographic and socioeconomic characteristics were accounted for (Correia et al. 2013; Pope et al. 2009a).
Our estimates are subject to important uncertainties and limitations. We derived CIs for our estimates of mortality using an approach that incorporated uncertainty in the concentration–response estimates from previous studies due to random error, but we did not account for uncertainty due to other sources of error. For example, the model used to estimate historical levels of before the monitoring network was deployed had of 0.11–0.40 in 1980 and 1981, indicating poor predictive performance. Monitoring data from the Inhalable Particulate Network (IPN), which were used as the observed comparison data for validating our model predictions, were limited to data from only 6 and 12 IPN sites in 1980 and 1981, respectively (after we applied site inclusion criteria). Therefore, limitations of the measured data may have been partly responsible for the apparent deficits in model performance. However, we cannot rule out the possibility that our estimates of risks were less accurate for the early 1980s than more recent years, and these uncertainties are not reflected in our estimates.
In addition, our estimates of associations between exposures and mortality at the county level did not account for the potential influence of exposures that occurred outside of the county where each death occurred, including exposures resulting from activities outside of the county of residence, as well as changes in residence from one county to another. An analysis of MESA Air cohort data using the same exposure model indicated that model-based predictions of average concentrations over a 30-y period were more consistent with 1-y average predictions in 2000 among participants who did not move during the study period compared with participants who moved at least once ( vs. 0.86, respectively), suggesting an effect of residential mobility on the accuracy of exposure estimates (Kim et al. 2017).
We used age-stratified population counts and all-cause death rates matched to each year to account for changes in population characteristics between 1980 and 2010. However, all-cause death rates for 1980 were suppressed for counties with low death counts, and our use of national median values for missing age-specific mortality data in these counties may have reduced the accuracy of our estimates of attributable deaths in 1980.
We used concentration–response relationships from epidemiological studies to relate historical changes in fine particle concentrations to changes in the estimated risk of premature death, which implicitly assumed that the association between and mortality was stable over the 30-y study period. However, modification of the association by time-varying factors, such as the chemical composition of PM mass, population activity patterns, housing stock, medical care access and effectiveness, and the prevalence of comorbid conditions, would also affect the accuracy of our estimates. Moreover, we estimated PM-related deaths without assuming a no-risk concentration threshold or accounting for natural background exposures; if a minimum risk threshold exists, our estimates will be inflated. Finally, the maximum annual mean concentration experienced by the Krewski et al. (2016) study population was lower than the maximum concentration predicted by our model for the year 1980. This adds to uncertainty about the validity of the Krewski et al. (2009) concentration–response estimate for estimating PM-related deaths in 1980, though the potential consequences of this, if any, are unpredictable.
Conclusions
While subject to important limitations and uncertainties, our estimates suggest that the U.S. population has experienced significantly improved health, with fewer deaths and prolonged life expectancy at birth, as a result of declining exposures to fine particles in ambient air pollution between 1980 and 2010. In nearly all locations, estimated numbers of excess deaths and proportions of total deaths attributed to fine particles declined, consistent with a reduced public health burden. Future research might extend these findings by addressing whether the benefits of declining levels vary among different population groups, and by projecting exposure estimates further into the future.
Supplemental Material
Acknowledgments
This work was supported by the U.S. EPA (RD 831697, CR-834077101-0, and RD-83479601-0). Additional support was provided by the National Research Foundation of Korea (Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education: 2013R1A6A3A04059017).
References
- Anenberg SC, Horowitz LW, Tong DQ, West JJ. 2010. An Estimate of the Global Burden of Anthropogenic Ozone and Fine Particulate Matter on Premature Human Mortality Using Atmospheric Modeling. Environ Health Perspect 118(9):1189–1195, PMID: 20382579, 10.1289/ehp.0901220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anenberg SC, Talgo K, Arunachalam S, Dolwick P, Jang C, West JJ. 2011. Impacts of global, regional, and sectoral black carbon emission reductions on surface air quality and human mortality. Atmos Chem Phys 11:7253–7267, 10.5194/acp-11-7253-2011. [DOI] [Google Scholar]
- Bachmann J. 2007. Will the Circle Be Unbroken: A History of the U.S. National Ambient Air Quality Standards. J Air Waste Manag Assoc 57(6):652–697, 10.3155/1047-3289.57.6.652. [DOI] [PubMed] [Google Scholar]
- Bell FC, Miller ML. 2005. Life Tables for the United States Social Security Area 1900-2100. Social Security Administration. https://www.ssa.gov/oact/NOTES/as120/LifeTables_Body.html [accessed 15 August 2016].
- Brook RD, Rajagopalan S, Pope CA III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. 2010. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121(21):2331–2378, PMID: 20458016, 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Burnett RT, Pope CA, Ezzati M, Olives C, Lim SS, Mehta S, et al. 2014. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspec. 122(4):397–403, PMID: 24518036, 10.1289/ehp.1307049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byun D, Schere KL. 2006. Review of the governing equations, computational algorithms, and other components of the Models-3 Community Multiscale Air Quality (CMAQ) Modeling System. Appl Mech Rev 59(2):51–77, 10.1115/1.2128636. [DOI] [Google Scholar]
- Caiazzo F, Ashok A, Waitz IA, Yim SHL, Barrett SRH. 2013. Air pollution and early deaths in the United States. Part I: Quantifying the impact of major sectors in 2005. Atmos Environ 79:198–208, 10.1016/j.atmosenv.2013.05.081. [DOI] [Google Scholar]
- CDC. 2011. United States Life Tables, 2007. https://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_09.pdf [accessed 17 July 2017].
- CDC WONDER Database (Centers for Disease Control and Prevention). Wide-ranging OnLine Data Epidemiologic Research (CDC WONDER) Data from Years 1980–2010. https://wonder.cdc.gov/ [accessed 17 July 2017].
- Chestnut LG, Mills DM. 2005. A fresh look at the benefits and costs of the US acid rain program. J Environ Manage 77(3):252–266, PMID: 16171931, 10.1016/j.jenvman.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Correia AW, Pope CA, Dockery DW, Wang Y, Ezzati M, Dominici F. 2013. Effect of air pollution control on life expectancy in the United States: an analysis of 545 U.S. counties for the period from 2000 to 2007. Epidemiology 24(1):23–31, PMID: 23211349, 10.1097/EDE.0b013e3182770237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O, et al. 2012. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ Health Perspect 120(5):708–714, PMID: 22313724, 10.1289/ehp.1104049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann N, Lamson AD, Anenberg SC, Wesson K, Risley D, Hubbell BJ. 2011a. Estimating the national public health burden associated with exposure to ambient PM2.5 and ozone. Risk Anal 32(1):81–95, PMID: 21627672, 10.1111/j.1539-6924.2011.01630.x. [DOI] [PubMed] [Google Scholar]
- Fann N, Roman HA, Fulcher CM, Gentile MA, Hubbell BJ, Wesson K, et al. 2011b. Maximizing health benefits and minimizing inequality: incorporating local-scale data in the design and evaluation of air quality policies. Risk Anal 31(6):908–922, PMID: 21615761, 10.1111/j.1539-6924.2011.01629.x. [DOI] [PubMed] [Google Scholar]
- Fann N, Baker KR, Fulcher CM. 2012. Characterizing the PM2.5-related health benefits of emission reductions for 17 industrial, area and mobile emission sectors across the U.S. Environ Int 49:141–151, PMID: 23022875, 10.1016/j.envint.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Fann N, Fulcher CM, Baker K. 2013. The recent and future health burden of air pollution apportioned across U.S. sectors. Environ Sci Technol 47(8):3580–3589, PMID: 23506413, 10.1021/es304831q. [DOI] [PubMed] [Google Scholar]
- Hand J, Copeland S, Day D, Dillner A, Indresand H, Malm WC, et al. 2011. “Spatial and Seasonal Patterns and Temporal Variability of Haze and its Constituents in the United States Report V.” State Univ. Fort Collins. http://vista.cira.colostate.edu/Improve/spatial-and-seasonal-patterns-and-temporal-variability-of-haze-and-its-constituents-in-the-united-states-report-v-june-2011/ [accessed 17 July 2017].
- Health Effects Institute. 2003. Assessing Health Impact of Air Quality Regulations: Concepts and Methods for Accountability Research. https://www.healtheffects.org/publication/assessing-health-impact-air-quality-regulations-concepts-and-methods-accountability [accessed 17 July 2017].
- Hubbell B, Fann N, Levy J. 2009a. Methodological considerations in developing local-scale health impact assessments: balancing national, regional, and local data. Air Qual Atmos Health 2(2):99–110, 10.1007/s11869-009-0037-z. [DOI] [Google Scholar]
- Hubbell BJ, Crume RV, Evarts DM, Cohen JM. 2009b. Policy Monitor: Regulation and Progress under the 1990 Clean Air Act Amendments. Rev Environ. Econ. Policy 4(1):122–138, 10.1093/reep/rep019. [DOI] [Google Scholar]
- Kim SY, Olives C, Sheppard L, Sampson PD, Larson TV, Keller JP, et al. 2017. Historical prediction modeling approach for estimating long-term concentrations of PM2.5 in cohort studies before the 1999 implementation of widespread monitoring. Environ Health Perspect 125(1):38–46, PMID: 27340825, 10.1289/EHP131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, et al. 2009. “Extended Follow-Up and Spatial Analysis of the American Cancer Society Study Linking Particulate Air Pollution and Mortality.” 5-114–36. https://www.healtheffects.org/publication/extended-follow-and-spatial-analysis-american-cancer-society-study-linking-particulate [accessed 17 July 2017]. [PubMed]
- Levy JI, Greco SL, Spengler JD. 2002. The importance of population susceptibility for air pollution risk assessment: a case study of power plants near Washington, DC. Environ Health Perspect 110(12):1253–1260, PMID: 12460806, 10.1289/ehp.021101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. 2012. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2224–2260, PMID: 23245609, 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BG, Hurley JF. 2003. Life table methods for quantitative impact assessments in chronic mortality. J Epidemiol Community Health 57(3):200–206, PMID: 12594196, 10.1136/jech.57.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasari MM, Szyszkowicz M, Chen H, Crouse D, Turner MC, Jerrett M, et al. 2016. A class of non-linear exposure-response models suitable for health impact assessment applicable to large cohort studies of ambient air pollution. Air Qual Atmos Heal 9(8):961–972, 10.1007/s11869-016-0398-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHGIS Database. National Historical Geographic Informat ion System. Version2.0. http://www.nhgis.org [accessed 2 December 2015].
- Peters JM, Avol E, Gauderman WJ, Linn WS, Navidi W, London SJ, et al. 1999. A study of twelve Southern California communities with differing levels and types of air pollution: II. Effects on pulmonary function. Am J Respir Crit Care Med 159(3):768–775, PMID: 10051249, 10.1164/ajrccm.159.3.9804144. [DOI] [PubMed] [Google Scholar]
- Pope CA III, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, et al. 2009a. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation 120(11):941–948, PMID: 19720932, 10.1161/CIRCULATIONAHA.109.857888. [DOI] [PubMed] [Google Scholar]
- Pope CA III, Ezzati M, Dockery DW. 2009b. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med 360(4):376–386, PMID: 19164188, 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J, Coull B, Laden F, Ryan L. 2008. The effect of dose and timing of dose on the association between airborne particles and survival. Environ Health Perspect 116(1):64–69, PMID: 18197301, 10.1289/ehp.9955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisler JF, Malm WC. 2000. Interpretation of Trends of PM25 and Reconstructed Visibility from the IMPROVE Network. J. Air Waste Manage Assoc 50(5):775–789, PMID: 28080835, 10.1080/10473289.2000.10464127. [DOI] [PubMed] [Google Scholar]
- U.S. EPA (U.S. Environmental Protection Agency). 1997. “The Benefits and Costs of the Clean Air Act, 1970 to 1990.” https://www.epa.gov/clean-air-act-overview/benefits-and-costs-clean-air-act.
- U.S. EPA. 2009. “Integrated Science Assessment for Particulate Matter.” EPA/600/R-. http://ofmpub.epa.gov/eims/eimscomm.getfile?p_download_id=494959 [accessed 17 July 2017].
- U.S. EPA. 2010. “Regulatory Impact Analysis for the Proposed Federal Transport Rule.” Docket ID No. EPA-HQ-OAR-2009-0491. http://www.epa.gov/ttn/ecas/regdata/RIAs/proposaltrria_final.pdf [accessed 17 July 2017].
- U.S. EPA. 2011a. “Benefits and Costs of the Clean Air Act 1990-2020, the Second Prospective Study.” https://www.epa.gov/clean-air-act-overview/benefits-and-costs-clean-air-act-1990-2020-second-prospective-study [accessed 17 July 2017].
- U.S. EPA. 2011b. “Regulatory Impact Assessment for Final Transport Rule.” https://www3.epa.gov/ttn/ecas/docs/ria/transport_ria_final-csapr_2011-06.pdf [accessed 17 July 2017].
- U.S. EPA. 2011c. “Regulatory Impact Assessment for the Mercury and Air Toxics Standards.” https://www3.epa.gov/ttnecas1/regdata/RIAs/matsriafinal.pdf [accessed 17 July 2017].
- U.S. EPA. 2012a. Integrated Planning Model Analysis for Mercury and Air Toxics Standards. http://www.epa.gov/airmarkets/progsregs/epa-ipm/toxics.html [accessed 17 July 2017].
- U.S. EPA. 2012b. Regulatory Impact Assessment for the PM NAAQS RIA.
- U.S. EPA. 2014a. “Control of Air Pollution from Motor Vehicles: Tier 3 Motor Vehicle Emission and Fuel Standards Final Rule.” https://www.epa.gov/regulations-emissions-vehicles-and-engines/final-rule-control-air-pollution-motor-vehicles-tier-3 [accessed 17 July 2017].
- U.S. EPA. 2014b. “Regulatory Impact Analysis of the Proposed Revisions to the National Ambient Air Quality Standards for Ground-Level Ozone.” EPA-452/P-14-006. https://www3.epa.gov/ttnecas1/regdata/RIAs/20141125ria.pdf [accessed 17 July 2017].
- U.S. EPA. 2016. Air Trends Report. https://gispub.epa.gov/air/trendsreport/2016/ [accessed 17 July 2017].
- Voorhees AS, Fann N, Fulcher C, Dolwick P, Hubbell B, Bierwagen B, et al. 2011. Climate change-related temperature impacts on warm season heat mortality: a proof-of-concept methodology using BenMAP. Environ Sci Technol 45(4):1450–1457, PMID: 21247099, 10.1021/es102820y. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2013. Review of Evidence on Health Aspects of Air Pollution – REVIHAAP Project: Final Technical Report, PMID: http://www.euro.who.int/__data/assets/pdf_file/0004/193108/REVIHAAP-Final-technical-report-final-version.pdf?ua=1.27195369
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.