Abstract
Skin manifestations can herald, co-exist, or follow the evolution of inflammatory bowel disease (IBD). We report a middle-aged man with recent onset alopecia universalis and a history of intermittent diarrheal attacks for 6 years. Colonscopy and biopsy sampling confirmed ulcerative colitis. Regrowth of hair was achieved by treating the patient with azathioprine and mesalamine. Clinicians have to be aware that a multitude of skin manifestations with history of diarrhea can be an extraintestinal manifestation of IBD such as ulcerative colitis and this warrants further investigation.
Keywords: Ulcerative colitis, Alopecia universalis, Azathioprine
INTRODUCTION
The prevalence of inflammatory bowel disease (IBD) is variable among studies depending mainly on geographic regions. Europe has the highest prevalence, that is for ulcerative colitis (UC) 505 per 100,000 populations and for Crohn’s disease (CD) 322 per 100,000 populations. Meanwhile, the annual incidence rate was estimated in Europe to range from 0.6 to 24.3 per 100,000 and in Asia and Middle East 0.1 to 6.3 per 100,000.1 Extraintestinal manifestations of IBD tend to occur at higher rates ranging from 21% to 41%.2
The cutaneous manifestations are considered the most diverse and they may be the presenting manifestation in some occasions. Of these, hair loss was thought to be less prevalent.3 However, a recent cross sectional study,4 revealed that the frequency of hair loss in 210 patients with IBD was 33%. The hair loss associated with IBD is of three varieties i) telogen effluvium (TE); possibly exacerbated by nutritional deficiencies, chronic inflammatory state, and adverse effects of the treatment, ii) alopecia areata (AA); related directly to the autoimmunity of the disease, and iii) primary cicatricial alopecia (PCA) for which a recent retrospective study,5 from the UK reports this condition in 12 patients with IBD that signifies a higher than expected co-existence. Moreover the pathogenesis of both conditions implicates T-helper cell (Th-1) based cell-mediated cytotoxicity and similar pro-inflammatory cytokines profile. Furthermore, peroxisome proliferator-activated receptors (PPARγ) were shown to be deficient in both cells of hair follicles in PCA and in intestinal mucosa of patients with UC. This was the basis for the use of PPARγ agonists in the treatment of both conditions.6,7 No prior reports of AA universalis and nail dystrophy with UC that responded to azathioprine exist in PubMed.
CASE REPORT
A 40-year-old, North African man working as a plumber came presenting with diffuse hair loss for 4 months. It started by the falling of the beard, followed by scalp hair (figure 1) then progressed to loss of pubic hair and the extremities. Finally, it was followed by the loss of eyebrows (figure 1). He also reported nail changes in the form of discoloration and nail dystrophy affecting fingers and toenails (figure 2). On questioning, the patient admitted intermittent diarrhea of 6 years duration, which in the last 4 months reached a frequency of 6 motions per day. The attacks of watery diarrhea lasted for 2 days and were characterized by tenesmus, not associated with hematochezia, pus, or worms. Stool analysis was insignificant. The patient denied the intake of any drugs known to cause hair loss or receiving treatment for any other medical conditions except for over-the-counter anti-diarrheal medications. His history was significant for surgery for hemorrhoids. He had a 30 pack-year history of smoking. He was married and had two offspring. His sister was diagnosed as having Behcet’s disease. Possibly related to his condition, he reported low back pain associated with limitation of movement and inability to walk with stiffness increased by rest and decreased by movement. This pain was relieved by non-steroidal anti-inflammatory drugs (NSAIDs) and well tolerated by the patient. On physical examination he was of average built with generalized alopecia with sparse grey hair on his scalp and his genitals associated with dystrophy of all nails. System review was unremarkable for any other abnormality. Total colonoscopy with ileoscopy was done and multiple biopsy samples were taken from the terminal ileum and rectum. The histopathological examination confirmed a picture of UC with mild to moderate activity (figure 3). Capilloroscopy revealed scanty capillaries and veiling of the capillary nail bed. His laboratory examination was remarkable for elevated ESR. The virology screening included Epstein Barr virus (EBV) and Cytomegalovirus (CMV) was negative. Anticardiolipin IgM, anti-nuclear (ANA), anti-dsDNA, and anti-neutrophil cytoplasmic antibodies were negative. The micronutrient levels including iron and zinc were assessed to exclude nutritional causes of hair loss. The patient received the following regimen; Azathioprine 2mg/kg/day, prednisone 40 mg/day, mesalamine 500mg/8hrs with good compliance. On follow-up, there is improvement in the bowel condition as well as observed re-growth of scalp, beard, and other body hair.
Fig.1.
1a Loss of beard hair and eyebrows. 1b Loss of scalp hair
Fig.2.

a,b. Dystrophic nail changes; pitting, onychorrhxis and leukonychia
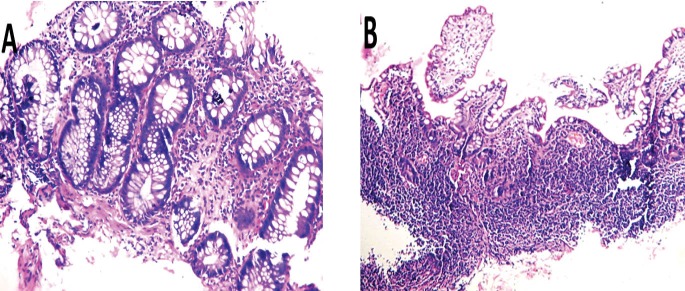
Fig.3.
3A. Backwash ileitis with grade II villous atrophy: Ileal biopsy with surface erosions, villi showing broadening and shortening. The glands showing regenerative changes, the lamina propria infiltrated by mild to moderate chronic inflammatory cells. 3B. Rectal biopsy: mucosal damage, glandular distortion, missing crypts and cryptitis. Lamina propria infiltrated by moderate chronic inflammatory cells. No evident dysplastic or neoplastic changes.
DISCUSSION
Careful history taking was behind the link between recent onset dermatological presentations to unsettled old bowel complaints. The patient had accommodated to his bowel complaints for six years and what urged him to seek medical advice was his recent onset skin manifestations namely alopecia universalis along with increasing severity of original complaints. Upon receiving azathioprine and mesalamine, his skin manifestations started to resolve. We believe that the association of diffuse hair loss with UC is under-reported8–13 and was thought in most cases to be attributed mainly to side effects of the treatment. Patel and colleagues3 , reviewed 11 case reports of AA associated with IBD. Seven of these cases had developed other autoimmune diseases. Occasionally, the activity of IBD is quiescent at the time of hair loss. The regrowth of hair after azathioprine prescription is reported only in two cases with CD.14,15
It is important to notice that azathioprine has a therapeutic effect on AA, which is not associated with IBD. One pilot study14 assessed the effect of azathioprine 2 mg/kg/day for 6 months on 20 patients with moderate to severe AA. It was found that there was considerable improvement in hair condition. On the other hand, a recent study16 showed the development of AA in 5 out of 146 patients with IBD while they were receiving azathioprine. Our case may be the first to document the response of alopecia universalis to azathioprine in a patient with UC. Meanwhile another case report15 documented the response of alopecia totalis to azathioprine in a patient with CD. Farshi and others14 have encountered the same positive response of alopecia universalis to azathioprine. This may be what urges them to conduct the previously discussed pilot study.
It is interesting that most reported cases of AA and UC have a co-associated autoimmune conditions such as vitiligo,8,9,17 autoimmune thyroiditis,12 myasthenia gravis,8 and scleroderma.9 The autoimmune nature of AA is well established. The hair follicle is an immune-privileged site and when its integrity is compromised it is identified as an autoantigen by T-lymphocytes and an immune reaction ensues. Clinically, AA uncommonly presents as chronic diffuse hair loss and in such cases, has to be distinguished from telogen effluvium.18 It is noteworthy that nail changes with AA include pitting, trachyonchia, onychorrhxis, koilonychia, and leukonychia. In one case-control study19 designed to assess the association between AA and other autoimmune disorders among 70 patients with AA, the frequency of associated diseases were found as follows: thyroid disorder (18.3%), Diabetes Mellitus (7.1%), allergic rhinitis and bronchial asthma (4.2%), ulcerative colitis (2.8%) and Systemic lupus erythematosus (1.4%). Moreover nail changes were observed in 16.8% of patients with AA.
To date, there are around 47 loci/genes implicated in the susceptibility to UC.20 Genetic overlap between UC and AA has been verified through genome-wide association study at IL2/IL21 locus.21,22 Celiac disease also shows strong association with this locus and there are some case reports of AA that developed in patients with celiac disease.23 In conclusion, patients with UC can develop AA years before or after the onset of bowel disease as the two conditions are related in their genetic susceptibility and their autoimmune pathogenic processes.
Please cite this paper as:
Shohdy S K, Rashad W, Elmeligui A. Alopecia Universalis Associated with Ulcerative Colitis and The Role of Azathioprine. Middle East J Dig Dis 2018;10:50-54. doi: 10.15171/mejdd.2017.91.
Footnotes
ETHICAL APPROVAL There is nothing to be declared.
CONFLICT OF INTEREST The authors declare no conflict of interest related to this work.
References
- 1.Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G. et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review Gastroenterology. 2012;142:46–54 e42. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Marzano AV, Borghi A, Stadnicki A, Crosti C, Cugno M. Cutaneous Manifestations in Patients With Inflammatory Bowel Diseases. Inflamm Bowel Dis. 2014;20:213–27. doi: 10.1097/01.MIB.0000436959.62286.f9. [DOI] [PubMed] [Google Scholar]
- 3.Patel K V, Farrant P, Sanderson JD, Irving PM. Hair loss in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1753–63. doi: 10.1097/MIB.0b013e31828132de. [DOI] [PubMed] [Google Scholar]
- 4.Shah R, Abraham B, Hou J, Sellin J. Frequency and associated factors of hair loss among patients with inflammatory bowel disease. World J Gastroenterol. 2015;21:229–32. doi: 10.3748/wjg.v21.i1.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massa AF, Chiang YZ, Tosti A, Harries M. Primary cicatricial alopecia and inflammatory bowel disease - is there a link? J Eur Acad Dermatol Venereol. 2016;30:1198–9. doi: 10.1111/jdv.13119. [DOI] [PubMed] [Google Scholar]
- 6.Baibergenova A, Walsh S. Use of pioglitazone in patients with lichen planopilaris. J Cutan Med Surg. 2012;16:97–100. doi: 10.2310/7750.2011.11008. [DOI] [PubMed] [Google Scholar]
- 7.Lewis JD, Lichtenstein GR, Deren JJ, Sands BE, Hanauer SB, Katz JA. et al. Rosiglitazone for active ulcerative colitis: a randomized placebo-controlled trial. Gastroenterology. 2008;134:688–95. doi: 10.1053/j.gastro.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan RS. Ulcerative colitis, myasthenia gravis, atypical lichen planus, alopecia areata, vitiligo. Proc R Soc Med. 1974;67:195–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson D. Alopecia areata, vitiligo, scleroderma, ulcerative colitis. Proc Roy Soc Med. 1974;67:48–50. [PMC free article] [PubMed] [Google Scholar]
- 10.Treem WR, Veligati LN, Rotter JI, Targan SR, Hyams JS. Ulcerative colitis and total alopecia in a mother and her son. Gastroenterology. 1993;104:1187–91. doi: 10.1016/0016-5085(93)90291-j. [DOI] [PubMed] [Google Scholar]
- 11.Katsinelos P, Kountouras J, Paroutoglou G, Zavos C. Alopecia Areata, Primary Sclerosing Cholangitis, and Ulcerative Colitis: Autoimmunity and Apoptosis as Common Links? Apoptosis. 2007;80:1288–92. doi: 10.1007/s10620-006-9265-3. [DOI] [PubMed] [Google Scholar]
- 12.Sheehan M, Islam R. Silent thyroiditis, isolated corticotropin deficiency, and alopecia universalis in a patient with ulcerative colitis and elevated levels of plasma factor viii: an unusual case of autoimmune polyglandular syndrome type 3. Endocr Pract. 2009;15:138–42. doi: 10.4158/EP.15.2.138. [DOI] [PubMed] [Google Scholar]
- 13.Safina D, Abdulkhakov R, Abdulkhakov S, Odintsova A, Cheremina N. Clinical case of a combination of ulcerative colitis and alopecia areata. Eksp Klin Gastroenterol. 2013;12:92–6. [PubMed] [Google Scholar]
- 14.Farshi S, Mansouri P, Safar F, Khiabanloo SR. Could azathioprine be considered as a therapeutic alternative in the treatment of alopecia areata? A pilot study. Int J Dermatol. 2010;49:1188–93. doi: 10.1111/j.1365-4632.2010.04576.x. [DOI] [PubMed] [Google Scholar]
- 15.Goddard CJ, August PJ, Whorwell PJ. Alopecia totalis in a patient with Crohn’s disease and its treatment with azathioprine. Postgrad Med J. 1989;65:188–9. doi: 10.1136/pgmj.65.761.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer L, Simian D, Lubascher J. Eventos adversos en la terapia farmacológica de la enfermedad inflamatoria intestinal. Rev Med Chile. 2015;143:7–13. doi: 10.4067/S0034-98872015000100001. [DOI] [PubMed] [Google Scholar]
- 17.Okan G, Vural P, Peker O, Colakoglu E, Saruc M. Azathioprine-induced liver injury in a patient with multiple autoimmune syndrome. J Dermatolog Treat. 2010;21:357–360. doi: 10.3109/09546630903410174. [DOI] [PubMed] [Google Scholar]
- 18.Sehgal VN, Jain S. Alopecia areata: clinical perspective and an insight into pathogenesis. J Dermatol. 2003;30:271–89. doi: 10.1111/j.1346-8138.2003.tb00389.x. [DOI] [PubMed] [Google Scholar]
- 19.Thomas E, Kadyan R. Alopecia areata and autoimmunity: A clinical study. Indian J Dermatol. 2008;53:70–4. doi: 10.4103/0019-5154.41650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lees CW, Barrett JC, Parkes M, Satsangi J. New IBD genetics: common pathways with other diseases. Gut. 2011;60:1739–53. doi: 10.1136/gut.2009.199679. [DOI] [PubMed] [Google Scholar]
- 21.Festen E A M, Goyette P, Scott R, Annese V, Zhernakova A, Lian J. et al. Genetic variants in the region harbouring IL2/IL21 associated with ulcerative colitis. Gut. 2009;58:799–804. doi: 10.1136/gut.2008.166918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petukhova L, Duvic M, Hordinsky M, Norris D, Price V, Shimomura Y. et al. Genome-wide association study in alopecia areata implicates both innate and adaptive immunity. Nature. 2010;466:113–7. doi: 10.1038/nature09114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fessatou S, Kostaki M, Karpathios T. Coeliac disease and alopecia areata in childhood. J Paediatr Child Health. 2003;39:152–4. doi: 10.1046/j.1440-1754.2003.00116.x. [DOI] [PubMed] [Google Scholar]