Abstract
Objective
Evidence of physical function difficulties, such as difficulty rising from a chair, may limit daily walking for people with knee osteoarthritis (OA). The purpose of this study was to identify minimum performance thresholds on clinical tests of physical function predictive to walk ≥6000 steps/day. This benchmark is known to discriminate people with knee OA who develop functional limitation over time from those who do not.
Methods
Using data from the Osteoarthritis Initiative, we quantified daily walking as average steps/day from an accelerometer (Actigraph GTM1) worn for ≥10 hours/day over one week. Physical function was quantified using three performance-based clinical tests: five times sit to stand test, walking speed (tested over 20 meters) and 400-meter walk test. To identify minimum performance thresholds for daily walking, we calculated physical function values corresponding to high specificity (80 to 95%) to predict walking ≥6000 steps/day.
Results
Among 1925 participants (age [mean±sd] 65.1±9.1 years, BMI 28.4±4.8 kg/m2, 55% female) with valid accelerometer data, 54.9% walked ≥6000 steps/day. High specificity thresholds of physical function for walking ≥6000 steps/day ranged from 11.4 to 14.0 sec on the five times sit to stand test, 1.13 to 1.26 meters/sec for walking speed, or 315 to 349 sec on the 400-meter walk test.
Conclusion
Not meeting these minimum performance thresholds on clinical tests of physical function may indicate inadequate physical ability to walk ≥6000 steps/day for people with knee OA. Rehabilitation may be indicated to address underlying impairments limiting physical function.
Keywords: physical function, walking, osteoarthritis
Introduction
Knee osteoarthritis (OA) is the 11th highest contributor to global disability (1) and the most common cause of functional limitation in older adults (2). People with knee OA often have low levels of physical activity (3). Physical activity is defined as any energy expenditure above a resting level (3, 4). Low levels of physical activity are a major problem since regular participation in physical activity lowers the risk of developing future comorbidities, such as cardiovascular disease, diabetes, and cancer (5, 6). Daily walking is a most common type of unstructured physical activity in older adults (7) and is recommended for people with knee OA (8). Evidence suggests that aerobic walking program reduces knee pain and improve physical function for people with knee OA (9–11).
For people with knee OA, a potential barrier to daily walking is difficulty with physical function.(12) For example, difficulty getting out of a chair or limited walking endurance may hinder how often one walks in the real world. However, it is not known whether reduced physical function is associated with less daily walking, i.e., taking fewer steps/day. If so, this would enable the investigation of minimum values of physical function that may be necessary in order to walk at a meaningful level. Little is known regarding the minimum level of physical function predictive for an active lifestyle. In particular, we are interested in identifying levels of physical function predictive to walk ≥ 6000 steps/day. We chose this threshold because we previously found walking ≥ 6000 steps/day better discriminates between those who did versus those who did not develop functional limitation two years later people with or at high risk of knee OA more so than walking 10,000 steps/day or 3,000 steps/day (13). Identifying the minimal physical function predictive to walk ≥ 6,000 steps/day may help healthcare providers gauge when limitations in physical function may be a barrier to daily walking in the real world for people with or at high risk of knee OA.
The purpose of this study was to evaluate minimum performance thresholds on standardized clinical tests of physical function predictive of walking ≥ 6000 steps/day. We first evaluated the association of physical function with daily walking, then identified levels of physical function that have a high degree of specificity to predict walking ≥ 6,000 steps/day. We chose high specificity values to conservatively identify physical function levels that do not support walking ≥ 6,000 steps/day by reducing the number of false positives, i.e., people who have poor physical function yet walk ≥ 6,000 steps/day.
Methods
Study participants
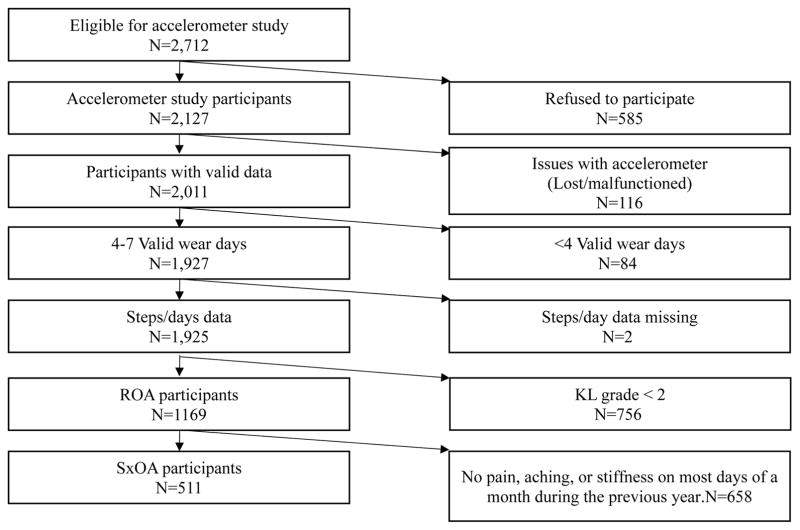
We used publicly available data from the Osteoarthritis Initiative (OAI), a large observational prospective cohort of people with or at risk of knee OA. The OAI examines the development and progression of OA in adults with or at high risk of knee OA. Study participants were recruited from clinical sites located in Maryland, Pennsylvania, Rhode Island and Ohio. Excluded were people with rheumatoid or inflammatory arthritis, a bilateral end-stage disease defined as severe joint space narrowing or total knee replacements in both knees, and those who used ambulatory aids other than a cane. Institutional review board approval was obtained from all OAI sites. The current analysis used accelerometer data collected on a sub-cohort of participants at the 48-month follow-up visit (13). Figure 1 provides a summary of the number of accelerometer records at the 48-month follow-up visit and reasons for exclusion from our analytical sample. Of the 2,127 OAI participants who participated in the accelerometer study, 1,925 participants wore the accelerometer for ≥ 4 valid days and had steps/day data at the 48-month follow-up visit. Those who participated in the accelerometer study but were not included in the analytic dataset (n=202) had a higher BMI, were less educated, and had worse physical function compared to those included in the analytic dataset (n=1925) (Supplemental table 1).
Figure 1.
Data reduction from full OAI sample to the eligible sub-cohort of accelerometer study participants (n=2,712) at 48-month follow-up.
Study Outcome
Daily walking was quantified as steps/day measured using a uniaxial accelerometer (Actigraph GT1M, Pensacola, FL, USA). The Actigraph GT1M is a valid device to quantify physical activity in free-living conditions (14, 15). Subjects were fitted with the accelerometer above the right hip and were instructed to wear the accelerometer during waking hours for 7 consecutive days. We employed previously published methods to determine valid physical activity records.(16) Briefly, we defined a valid wear day as ≥ 10 hours of wear time and included participants with ≥4 valid wear days, as this is the minimum time predictive for a reliable estimate of physical activity behavior (17). Steps/day were averaged across the available valid days. We categorized people as walking < 6000 steps/day and ≥ 6000 steps/day (13).
Study Exposures
Physical function
We used three performance-based clinical tests to measure physical function.
Five times sit to stand test. Five times sit to stand test was used as a correlate for lower extremity functional strength. Participants were instructed to stand from a chair (straight back, flat, level firm seat and seat height of 45cm in front) and return to sitting five times as quickly as possible with arms folded across the chest. Total time (sec) was measured with a digital stopwatch, and started with initial movement to stand on the first repetition and ended after returning to sitting on the fifth repetition. The five times sit to stand was recorded as the average of two trials. Longer time to perform the test was indicative of worse physical function. The five times sit to stand test has high test–retest reliability (intraclass correlation coefficients > 0.9) in older adults with symptomatic hip or knee OA (18, 19).
Walking speed. The 20-meter walk test was used to calculate self-selected walking speed. Participants were instructed to walk at their usual speed over a marked 20-meter course in an unobstructed and dedicated corridor. Timing with a digital stopwatch began at the initial movement from standing at the start and stopped when they crossed the 20-meter mark. Time to complete the walk (sec) was divided by distance (20 meters) to obtain walking speed in meters/second (meters/sec). The average of two trials was recorded, with slower walking speed indicating worse physical function (20). Measuring walking speed in a walkway has high test–retest reliability (intraclass correlation coefficients > 0.9) in older adults (21, 22).
400-meter walk test. The 400-meter walk test was administered to quantify walking endurance. Participants who did not complete the 20-meter walk test, or had a resting heart rate > 110 or < 40 bpm, or blood pressure systolic > 180 mmHg and diastolic > 100 mmHg were not allowed to perform the test. The test was conducted on the same course as the 20-meter walk test. Subjects were instructed to complete 10 laps in a clockwise direction at their usual walking pace. Timing using a digital stopwatch began from the initial movement from standing at the start until 10 laps were completed. Total time (sec) was recorded, with longer time indicating worse physical function. The 400-meter walk test has high test–retest reliability (intraclass correlation coefficients > 0.9) in healthy middle-aged adults (23).
Potential Confounders
We considered the following factors as potential confounders based on their association with daily walking and physical function (24–26) : age, sex (female versus male), race/ethnicity (white versus non-white), education (no college versus at least some college), body mass index (BMI, kg/m2) computed from weight and height assessment, comorbidity using the modified Charlson comorbidity index (>1 versus none), and intensity of knee pain (0–10 on a visual analog scale (VAS) where the participant pointed to a whole number on the card that best describes the pain at its worst ranging from “0” meaning “No pain” and “10” meaning “Pain as bad as you can imagine.”). These factors were ascertained at the 48-month visit by interview, questionnaire, and/or direct measurement, as appropriate.
Statistical Analysis
We described the study sample using means and standard deviations for continuous variables and percentages for categorical variables. To examine the association of steps/day with physical function, we calculated effect estimates using multiple linear regression adjusted for potential confounders, i.e., age, sex, BMI, race, education, knee pain intensity and comorbidity. Next, we calculated minimum performance thresholds on clinical tests of physical function corresponding to 80%, 85%, 90%, and 95% specificity values to predict walking ≥ 6000 steps/day (13). Specificity was defined as the proportion of participants whose test performance was above (better than) an identified threshold and walked ≥ 6000 step/day divided by the entire analytic sample who walked ≥ 6000 steps/day (footnote table 1 and equation). We chose high specificity cut points in order to minimize false-positives, i.e., minimize the number of people below minimum performance thresholds on clinical tests of physical function who walk ≥ 6,000 steps/day. Hence, we identified inadequate performance on clinical tests of physical function that predicted the inability to walk > 6000 steps/day daily walking. Lastly, we repeated the analyses restricting our sample to people with radiographic OA (ROA) defined Kellgren–Lawrence (KL) grade ≥ 2 on x-ray in one or both knees, and people with symptomatic OA (SxOA) defined by the presence of ROA and pain, aching, or stiffness on most days of a month during the previous year. Our intention with these sub-analyses was to investigate the stability of our findings across samples of people with ROA and SxOA because the presence of knee OA and/or symptoms may affect the participation in daily walking and physical functioning (12)
Footnote Table 1.
Example 2 × 2 contingency table to illustrate how groups were identified to calculate specificity. The italicized qualifiers for poor and good physical function were changed iteratively to determine the specificity over a range of performance on the clinical tests of physical function.
| Inactive (< 6000 steps/day) | Active (≥ 6000 steps/day) | |
|---|---|---|
| Poor physical function (five times sit to stand test in > 10 sec) | a | b |
| Good physical function (five times sit to stand test in < 10 sec) | c | d |
Results
The analytic study sample included 1925 people who were 65.1 ± 9.1 years of age (mean ± sd) with a BMI 28.4 ± 4.8 kg/m2. Over half were women (55%), the majority (84%) were white, and 66% graduated from high school (Table 1). On average, the participants walked 6166 ± 2924 steps/day, with 54% of the study sample walking ≥ 6000 steps/day. Average performance on the clinical tests of physical function were 10.5 ± 2.9 sec on the five times sit to stand test, 1.33 ± 0.21 meters/sec for walking speed over 20-meter walk test, or 306 ± 54 sec on the 400-meter walk test.
Table 1.
Characteristics of study participants
| All (N=1925) 100% of sample |
ROA (N=1169) 60.7% of sample |
SxOA (N=511) 26.5% of sample |
|
|---|---|---|---|
| Age, years [Mean±sd (n)] | 65.1±9.1 (1925) | 66.1±9.1 (1169) | 65.6±8.9 (511) |
| Women [% (n)] | 55 (1065) | 55 (641) | 54 (274) |
| Race, white [% (n)] | 84 (1601) | 81 (937) | 78 (394) |
| Education, more than college [% (n)] | 66 (1266) | 64 (746) | 62 (318) |
| BMI (kg/m2) [Mean±sd (n)] | 28.4±4.8 (1920) | 29.1±4.8 (1166) | 29.7±4.7 (510) |
| VAS pain [Mean±sd (n)] | |||
| Right | 2.4±2.6 (1915) | 2.7±2.7 (1163) | 3.9±2.9 (507) |
| Left | 2.3±2.6 (1916) | 2.6±2.7 (1162) | 4.0±2.8 (506) |
| Comorbidity [% (n)] | 30 (565) | 31 (364) | 35 (177) |
| Steps/day [Mean±sd (n)] | 6166±2924 (1925) | 5883±2821 (1169) | 5564±2778 (511) |
| Walked ≥ 6000 steps/day [% (n)] | 45 (868) | 42 (491) | 40 (203) |
| Five times sit to stand test (sec) [Mean±sd (n)] | 10.5±2.9 (1773) | 10.8±3.0 (1058) | 11.4±3.4 (439) |
| Walking speed (meters/sec) [Mean±sd (n)] | 1.33±0.21 (1876) | 1.31±0.21 (1139) | 1.28±0.21 (494) |
| 400-meter walk test (sec) [Mean±sd (n)] | 306±53 (1707) | 310±55 (1039) | 319±60 (446) |
ROA= radiographic OA SxOA= Symptomatic OA, BMI = body mass index, VAS = visual analog scale
Worse performance on clinical tests of physical function was associated with taking fewer steps/day after adjustment for potential confounders (Table 2). Each additional 1 sec to complete the five sit to stand test was associated with walking 130 fewer steps/day (95% CI [−178, −83]). Walking 0.1 meters/sec slower during the 20-meter walk test was associated with walking 342 fewer steps/day (95% CI [−276, −408]). Lastly, each additional 10 sec to complete 400-meter walk test was associated with walking 125 fewer steps/day (95% CI [−151, −98]).
Table 2.
Unadjusted and adjusted performance of physical function tests with steps/day using linear regression models.*
| Physical function | Steps/day (95% CI) | Adjusted Steps/day (95%CI)* |
|---|---|---|
| Five times sit to stand test (1 sec longer) | −261 (−307, −215) | −130 (−178, −83) |
| Walking speed (0.1 meters/sec slower) | −569 (−510, −628) | −342 (−276, −408) |
| 400-meter walk test (10 sec longer) | −211 (−235, −186) | −125 (−151, −98) |
Adjusted for age, sex, education, race, BMI, pain and Charlson comorbidity index.
Performance on the clinical tests of physical function corresponding to 80% to 95% specificity to identify those who walked ≥ 6000 steps/day ranged from 11.4 to 14.0 sec on the five times sit to stand, 1.13 to 1.26 meters/sec for walking speed, or 315 to 349 sec on the 400-meter walk test. (Figure 2) After restricting our study sample to participants with ROA, we observed that the thresholds for performance on the clinical tests of physical function to identify those who walked ≥ 6000 steps/day were almost identical to the full sample (Figure 2). When restricted to participants with SxOA, we observed that 80 to 95% specificity thresholds of performance on physical function tests ranged from 12.4 to 15.0 sec on the five times sit to stand test, 1.10 to 1.22 meters/sec for walking speed or 322 to 353 sec on the 400-meter walk test (Figure 2).
Figure 2. Physical function measures that reflect 80, 85, 90 and 95% specificity* in all, ROA and SxOA participants.
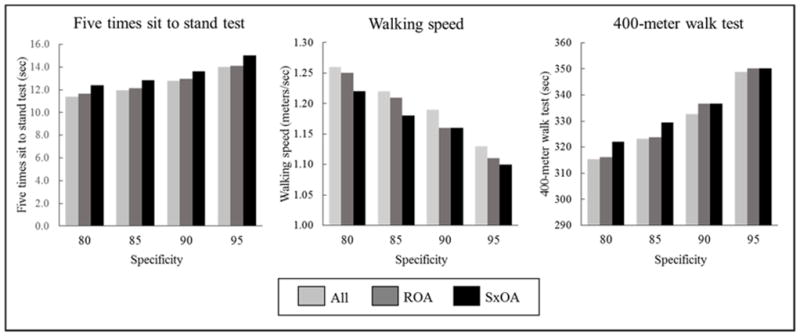
* Specificity was defined as the proportion of people who had less than threshold values of physical function and who walked ≥ 6000 steps/day divided by the proportion of people who walked ≥ 6000 steps/day.
Discussion
In general, we identified preliminary performance thresholds on clinical tests of physical function predictive to walk ≥ 6,000 steps/day for people with or at high risk of knee OA. Specifically, completing the five times sit to stand test in less than 11.4 to 14 sec, walking more than 1.13 to 1.26 meters/sec, or completing the 400-meter walk test in less than 315 to 349 sec corresponds to 80–95% specificity values to predict walking ≥ 6,000 steps/day. Study subjects who are unable to meet any one of these thresholds may have insufficient physical function to participate in walking more than 6,000 steps/day. We found these thresholds to be similar when analyses were restricted to those with ROA and SxOA. Previous work by White and his colleagues has found similar physical activity cut points across all, ROA and SxOA participants when predicting functional limitation (13). This indicates that people with or at high risk of knee OA can be similarly screened for insufficient physical function to walk 6000 steps/day.
The five times sit to stand test is a practical objective assessment of functional lower extremity strength that is feasible for use by health professionals. The test requires a chair and stopwatch, can be done in a doctor’s office and has minimal risk of injury as patients simply stand from a chair. 80% specificity thresholds for the sit-to-stand test were 11.4, 11.6 and 12.4 sec for all, ROA and SxOA participants respectively. There was variability of approximately 1 sec among all and SxOA participants, which is not a clinically meaningful difference (i.e. 2.3 sec) (27). Therefore, taking longer than 12 sec to complete the five times sit to stand test, a general heuristic (i.e., guiding) value that can be used in clinical practice, may indicate inadequate physical function to walk ≥ 6000 steps/day. Similar thresholds have been reported in the literature in other populations (18, 28–31). For instance, community-dwelling older adults who took more than 12 sec to complete the five times sit to stand test had double (OR = 2.0, 95%CI (1.3, 3.0)) the risk for multiple falls compared with those who took < 12 sec to complete the test (29). This test requires the use of lower body muscle groups, including knee and hip extensors, hip, knee and ankle range of motion and maintaining balance transitioning from sitting to stand (32). Poor performance, i.e., requiring greater time to complete the test, may reflect the presence of impairments including lower body pain, inadequate lower body muscle strength, poor balance or coordination deficits, which also can limit daily walking.
Walking speed is a well-established marker of health, a predictor of morbidity and mortality in older adults (33), and feasible to test in the clinic (34). 80% specificity thresholds for the 20-meter walk test were 1.26, 1.25 and 1.22 meters/sec for all, ROA and SxOA participants respectively. There was variability of approximately 0.04 meters/sec among all and SxOA participants, which is not a clinically meaningful difference (i.e., 0.08 meters/sec) (35). Therefore, walking slower than 1.22 meters/sec during the 20-meter walk test, a general heuristic value that can be used in clinical practice, may identify people without the capacity to walk ≥ 6,000 steps/day. This particular speed threshold is known to be important for community ambulation, as timed crosswalks are set to require a minimum speed of 1.22 meters/sec (20, 36). Hence, the inability to walk at this speed may represent the inability to safely walk in the community. Impairments in several body systems can slow walking speed (37), including vision, lower extremity strength (38, 39), aerobic capacity(40), postural control and proprioception (39), and can also restrict daily walking (33).
Walking endurance, like walking speed, is a well-known predictor of future health outcomes, including mobility limitations, disability, and mortality (23, 41, 42). 80% specificity thresholds for the 400-meter walk test were 315, 314 and 322 sec for all, ROA and SxOA participants respectively. There was variability of approximately 7 sec among all and SxOA participants, which is not a clinically meaningful difference (i.e. 20–30 sec) (43). Therefore, taking longer than 322 sec or 5.22 minutes to complete the 400-meter walk test, a general heuristic value that can be used in clinical practice, may have inadequate walking endurance to walk ≥ 6,000 steps/day. This benchmark is similar to that reported by Newman et al., who found community-dwelling older adults who completed the 400-meter walk test in >365 sec had three times greater risk of mortality compared with those who complete the walk in < 290 sec (41). Impairments in peak aerobic capacity (44) and cardiorespiratory changes (41) can limit walking endurance and daily walking (41, 44–46).
One possible implication of our study is referral to rehabilitation, such as physical therapy, may be of benefit to those with or at risk of knee OA not meeting one or more of these physical function thresholds. Physical therapists assess underlying modifiable impairments that limit physical function, including pain, muscular strength, range of motion, limited cardiorespiratory fitness, and coordination, then use therapeutic exercise and manual techniques to target underlying impairments(47). These interventions that are employed by physical therapists are effective to improve physical function in people with knee OA (48, 49).
Our study has several limitations. First, we employed only one definition of daily walking, i.e. 6000 steps/day, and did not examine thresholds of different intensities of physical activity, such as time spent in light, moderate or vigorous intensity activity. Future studies should consider intensity-based outcomes to confirm the extent to which our physical function thresholds also apply to time spent in moderate or vigorous intensity activity. Second, most of our sample was white, well educated, had a low BMI, and performed better on the physical function tests compared to those who participated in the accelerometer study but did not provide sufficient valid data (supplemental table 1). Thus, caution should be taken when generalizing these results to other populations. Third, the cross-sectional design allowed us to identify a relationship between physical function and physical activity, but not to draw conclusions about causation. Fourth, the 400-meter walk test was only administered to people who cleared a cardiovascular screen (heart rate 40–110 bpm, blood pressure systolic < 180 mmHg and diastolic < 100 mmHg, could complete 20-m walk test, did not report shortness of breath/angina or did not have recent hospitalization or surgery), which may affect the 400-meter walk test threshold. In our analytic sample, 60 participants did not clear the cardiovascular screen. Thus, it is likely that participants with compromised cardiovascular symptoms, who may perform worst on a test of endurance, were excluded. Lastly, there is a possibility study subjects chose to not participate in daily walking irrespective of their physical function ability possibly due to psychosocial barriers, hence the physical function threshold values should be viewed as estimates that have some variability.
Despite these limitations, our study has several strengths. First, we used a large analytic sample with objectively measured physical activity from a well-established cohort. Second, we selected thresholds of physical function that minimized false positives, i.e., people with knee OA who did not meet performance thresholds were highly unlikely to walk ≥ 6000 steps/day. Third, we established performance thresholds using clinically feasible measures of physical function that clinicians can employ in the real world.
Conclusions
We identified preliminary thresholds for performance on clinical tests of physical function that may indicate inadequate physical ability to walk at least 6,000 steps/day, which is an important benchmark we previously found to be associated with protection against the development of future functional limitation. Clinicians may consider prioritizing referral to rehabilitation to improve physical function for people with knee OA that are unable to meet these minimum thresholds.
Supplementary Material
Significance and Innovation.
The results from our study provide preliminary minimal performance thresholds on clinical tests of physical function that may be predictive to walk ≥ 6,000 steps/day, an important benchmark of daily walking for people with knee OA.
Based on our results, we identified general heuristic values that can be used in clinical practice. Taking longer than 12 sec on the five times sit to stand test, walking slower than 1.22 meters/sec, or taking longer than 323 sec to walk 400-meters may signal inadequate physical function predictive to walk ≥ 6,000 steps/day.
Acknowledgments
Funding: NIH U54 GM104941 and R21AR071079
Footnotes
Potential conflict of interest: None
Footnote: To calculate the specificity.
To illustrate this process, consider a test value of 10 sec to complete the five times sit to stand test. Since a slower time is indicative of worse physical function on this test, those who performed the five times sit to stand test in > 10 sec were identified as poor physical function. Likewise, those who performed the test in < 10 sec were identified as good physical function. We constructed a 2×2 contingency table (Table 1), and calculated specificity as shown in Equation 1. This process was repeated to determine the specificity over a range of possible performance on the clinical tests of physical function.
| Equation 1 |
References
- 1.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 2.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Physical Activity Guidelines Advisory Committee Report. US Dept of Health and Human Services; Washington, DC: 2008. [Google Scholar]
- 4.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public health reports. 1985;100(2):126. [PMC free article] [PubMed] [Google Scholar]
- 5.O’Grady M, Fletcher J, Ortiz S. Therapeutic and physical fitness exercise prescription for older adults with joint disease: an evidence-based approach. Rheumatic Disease Clinics of North America. 2000;26(3):617–46. doi: 10.1016/s0889-857x(05)70159-9. [DOI] [PubMed] [Google Scholar]
- 6.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Jama. 1995;273(5):402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 7.Mota J, Esculcas C. Leisure-time physical activity behavior: structured and unstructured choices according to sex, age, and level of physical activity. International journal of behavioral medicine. 2002;9(2):111–21. doi: 10.1207/s15327558ijbm0902_03. [DOI] [PubMed] [Google Scholar]
- 8.Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the Fitness Arthritis and Seniors Trial (FAST) Jama. 1997;277(1):25–31. [PubMed] [Google Scholar]
- 9.Messier SP, DeVita P, Cowan RE, Seay J, Young HC, Marsh AP. Do older adults with knee osteoarthritis place greater loads on the knee during gait? A preliminary study. Arch Phys Med Rehabil. 2005;86(4):703–9. doi: 10.1016/j.apmr.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50(5):1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 11.Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–73. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86(5):726–34. [PubMed] [Google Scholar]
- 13.White DK, Tudor-Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res (Hoboken) 2014;66(9):1328–36. doi: 10.1002/acr.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Medicine and science in sports and exercise. 2005;37(11):S531. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 15.Berlin JE, Storti KL, Brach JS. Using activity monitors to measure physical activity in free-living conditions. Physical Therapy. 2006;86(8):1137–45. [PubMed] [Google Scholar]
- 16.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40(1):181. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 17.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis & Rheumatism. 2011;63(11):3372–82. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Perceptual and motor skills. 2006;103(1):215–22. doi: 10.2466/pms.103.1.215-222. [DOI] [PubMed] [Google Scholar]
- 19.Lin YC, Davey R, Cochrane T. Tests for physical function of the elderly with knee and hip osteoarthritis. Scandinavian journal of medicine & science in sports. 2001;11(5):280–6. doi: 10.1034/j.1600-0838.2001.110505.x. [DOI] [PubMed] [Google Scholar]
- 20.Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have difficulty crossing the street. American journal of public health. 1997;87(3):393–7. doi: 10.2105/ajph.87.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fransen M, Crosbie J, Edmonds J. Reliability of gait measurements in people with osteoarthritis of the knee. Physical therapy. 1997;77(9):944–53. doi: 10.1093/ptj/77.9.944. [DOI] [PubMed] [Google Scholar]
- 22.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55(4):M221–M31. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gabriel KP, Rankin RL, Lee C, Charlton ME, Swan PD, Ainsworth BE. Test–retest reliability and validity of the 400-meter walk test in healthy, middle-aged women. J Phys Act Health. 2010;7(5):649–57. doi: 10.1123/jpah.7.5.649. [DOI] [PubMed] [Google Scholar]
- 24.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Sharma L, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis & Rheumatism. 2003;48(12):3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 26.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. American Journal of Public Health. 1990;80(8):945–9. doi: 10.2105/ajph.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meretta BM, Whitney SL, Marchetti GF, Sparto PJ, Muirhead RJ. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. Journal of Vestibular Research. 2006;16(4, 5):233–43. [PubMed] [Google Scholar]
- 28.Bohannon RW, Shove ME, Barreca SR, Masters LM, Sigouin CS. Five-repetition sit-to-stand test performance by community-dwelling adults: A preliminary investigation of times, determinants, and relationship with self-reported physical performance. Isokinetics and exercise science. 2007;15(2):77–81. [Google Scholar]
- 29.Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age and ageing. 2008;37(4):430–5. doi: 10.1093/ageing/afn100. [DOI] [PubMed] [Google Scholar]
- 30.Mong Y, Teo TW, Ng SS. 5-repetition sit-to-stand test in subjects with chronic stroke: reliability and validity. Archives of physical medicine and rehabilitation. 2010;91(3):407–13. doi: 10.1016/j.apmr.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 31.Schaubert KL, Bohannon RW. Reliability and validity of three strength measures obtained from community-dwelling elderly persons. The Journal of Strength & Conditioning Research. 2005;19(3):717–20. doi: 10.1519/R-15954.1. [DOI] [PubMed] [Google Scholar]
- 32.Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical Measurement of Sit-to-Stand Performance in People With Balance Disorders: Validity of Data for the Five-Times-Sit-to-Stand Test. Physical Therapy. 2005;85(10):1034–45. [PubMed] [Google Scholar]
- 33.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. Jama. 2011;305(1):50–8. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign”. Journal of geriatric physical therapy. 2009;32(2):2–5. [PubMed] [Google Scholar]
- 35.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society. 2006;54(5):743–9. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 36.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic Value of Usual Gait Speed in Well-Functioning Older People—Results from the Health, Aging and Body Composition Study. Journal of the American Geriatrics Society. 2005;53(10):1675–80. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 37.Park Y-H, Kim Y-m, Lee B-H. An ankle proprioceptive control program improves balance, gait ability of chronic stroke patients. Journal of physical therapy science. 2013;25(10):1321–4. doi: 10.1589/jpts.25.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age and ageing. 1997;26(1):15–9. doi: 10.1093/ageing/26.1.15. [DOI] [PubMed] [Google Scholar]
- 39.Clark DJ, Manini TM, Fielding RA, Patten C. Neuromuscular determinants of maximum walking speed in well-functioning older adults. Experimental gerontology. 2013;48(3):358–63. doi: 10.1016/j.exger.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fiser WM, Hays NP, Rogers SC, Kajkenova O, Williams AE, Evans CM, et al. Energetics of walking in elderly people: factors related to gait speed. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2010;65(12):1332–7. doi: 10.1093/gerona/glq137. [DOI] [PubMed] [Google Scholar]
- 41.Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. Jama. 2006;295(17):2018–26. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 42.Rolland YM, Cesari M, Miller ME, Penninx BW, Atkinson HH, Pahor M. Reliability of the 400-M Usual-Pace Walk Test as an Assessment of Mobility Limitation in Older Adults. Journal of the American Geriatrics Society. 2004;52(6):972–6. doi: 10.1111/j.1532-5415.2004.52267.x. [DOI] [PubMed] [Google Scholar]
- 43.Kwon S, Perera S, Pahor M, Katula J, King A, Groessl E, et al. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study) JNHA-The Journal of Nutrition, Health and Aging. 2009;13(6):538–44. doi: 10.1007/s12603-009-0104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: the Health ABC Long Distance Corridor Walk. J Am Geriatr Soc. 2001;49(11):1544–8. doi: 10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- 45.Simonsick EM, Newman AB, Visser M, Goodpaster B, Kritchevsky SB, Rubin S, et al. Mobility limitation in self-described well-functioning older adults: importance of endurance walk testing. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2008;63(8):841–7. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lange-Maia BS, Strotmeyer ES, Harris TB, Glynn NW, Simonsick EM, Brach JS, et al. Physical activity and change in long distance corridor walk performance in the health, aging, and body composition study. Journal of the American Geriatrics Society. 2015;63(7):1348–54. doi: 10.1111/jgs.13487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guide to Physical Therapist Practice. American Physical Therapy Association; 2016. [cited 2017 7/31/2017]. Available from: http://guidetoptpractice.apta.org/ [Google Scholar]
- 48.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. The Cochrane database of systematic reviews. 2015;1:Cd004376. doi: 10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Annals of internal medicine. 2000;132(3):173–81. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.