Abstract
Background
Patients with lumbar disc herniation are treated with physiotherapy/medication and some with surgery. However, even after technically successful surgery some develop a failed back syndrome with persistent pain. Our aim was to evaluate the efficacy of epiduroscopy in patients who suffer chronic low back pain and/or radicular pain with or without surgery and the gender difference in outcome.
Methods
A total of 88 patients were included with a mean age of 52 years (27-82), 54 women and 34 men. 66 of them were operated previously and 22 were non-operated. They all had persistent chronic back pain and radicular pain despite of medication and physical rehabilitation. Visual Analog Scale (VAS) for pain and Oswestry Disability Index (ODI) were evaluated preoperatively, after one month, six months and one-year after the epiduroscopy.
Results
All patients, and also the subgroups (gender and operated/non-operated) improved significantly in pain (VAS) and disability (ODI) at one month. A significant improvement was also seen at one year. No differences were found between men and woman at the different follow-up times. A slight worsening in VAS and ODI was noticed over time except for the non-operated group.
Conclusions
Epiduroscopy helps to improve the back and leg pain due to lumbar disc herniation in the early stage. At one year an improvement still exists, and the non-operated group seems to benefit most of the procedure.
Keywords: Disability evaluation, Endoscopy, Epidural space, Intervertebral disc displacement, Low back pain, Pain measurement, Radiating pain, Sex, Surgery
INTRODUCTION
Chronic low back pain and radicular pain denote pain in lumbosacral region together with the radiating pain along the affected nerve. One of several reasons for lumbosacral pain is lumber disc herniation. The first line of treatment for patients with lumbar disc herniation presenting with back pain is physiotherapy and medication [1].
Surgery is generally recommended in patients with MRI verified disc herniation, who are neurologically impaired or have intractable pain despite of nonsurgical treatment [2]. However, in some cases after successful surgery for lumbar disc herniation, as in in post-laminectomy syndrome, intractable pain occurs. Post-laminectomy syndrome is a major source of lumbosacral pain, which is defined as the presence of persistent pain even after technically and biomechanically successful spine surgery [3]. Postoperative inflammation and epidural fibrosis is known to cause intractable pain in post-laminectomy syndrome.
Recently, several studies have confirmed the effectiveness of epiduroscopy in the treatment of chronic back pain [4,5]. Epiduroscopy is a procedure which allows observation of the epidural space and the subsequent removal of adhesions and fibrosis using laser, the tip of the flexible catheter and saline flushing. In the final stage, steroids are administered to help cleanse the inflammatory agents in the epidural space. With this technique, the epidural space can easily be monitored, anatomic structures identified and pathologies detected.
We aimed to evaluate pain relief and disability in daily living after treatment with epiduroscopy in patients with chronic low back pain who had and had not been previously operated on for lumbar disc herniation and to investigate whether there were any gender differences in the outcome of the treatment.
MATERIALS AND METHODS
Medical records were reviewed retrospectively for 109 patients who were treated with epiduroscopy at the Department of Neurosurgery, Mugla, Turkey, between January 1, 2014 and May 1, 2016. All patients were followed up for one year, with a clinical examination on the day of the surgery, and then after one, six and twelve months. All the patients evaluated their pain on a Visual Analog Scale (VAS) and validated their disability using the Oswestry Disability Index (ODI) questionnaire on all visits.
Fifteen patients failed to keep the follow-up appointments and six were excluded from the study as they had lumbar surgery during the follow-up time. The study finally comprised 88 (34 [39%] male and 54 [61%] female) patients.
The inclusion criteria for the non-operated patients were: having chronic low back pain despite medical and physical rehabilitation therapy, with lumbar disc herniation at one level or more but with no indication of the need for surgery. The inclusion criteria for the operated patients were as for the non-operated patients, except for the operation. The operated patients had had one-level micro-discectomy.
Patients with spinal instability or with one or more levels of spinal stenosis were not included. Patients who had any lumbar surgery at any point during follow-up were not included. Patients with recurrent disc herniation, iatrogenic segmental instability, or one or multilevel spinal stenosis were excluded. Patients who received a second surgery, re-operation for disc herniation and or spinal stabilization were also excluded.
None of the patients received corticosteroids or narcotic analgesics before or after the epiduroscopy and none had any disease that could increase the pain (diabetes, polyneuropathy, or rheumatoid arthritis).
VAS is a continuous horizontal scale measuring 100 mm, with “no pain” at one end and “worst imaginable pain” at the other. A higher score indicates more severe pain. The following cut-off points on the pain VAS have been recommended: no pain (0–4 mm), mild pain (5–44 mm), moderate pain (45–74 mm) and severe pain (75–100 mm) [6].
ODI is the most commonly used outcome measure for low back pain [7,8]. It is a self-administered questionnaire with ten questions aimed at assessing limitations on various activities of daily living. The score is expressed as a percentage and the interpretations of the scores are: minimal disability (0–20%), moderate disability (21–40%), severe disability (41–60%) and crippled (61–80%). Patients with a score of between 81% and 100% are either bed-bound or exaggerating their symptoms.
The epiduroscopy is performed under local anesthesia, sedation and with cardiac monitoring. With the patient in prone position, an 18 G needle is introduced into the epidural space through the sacral hiatus. Fluoroscopy is used to identify the needle tip in the epidural space. Using the Seldinger technique, and with the aid of fluoroscopy, a 0.9 mm fiber optic endoscope (LD0028-12, Myelotec Inc., Roswell, GA) is introduced into the epidural space. The endoscope is directed cephalically in the epidural space by direct visual control. The epidural space is examined by distending it with a saline infusion. Adhesions are made visible and removed using the mechanical motion of the video-guided catheter tip and the forced injection of the saline into the epidural space. No laser was used during the procedure.
Analyses were made for the whole group, for women and men and for previously operated or non-operated patients and the groups were compared. Statistical analyses were performed using the SPSS-22 (IBM Corporation, Worldwide). Analyze of variance for repeated measurements was used to compare the whole group, gender and operated/non-operated patients and when applicable the Bonferroni's correction was done. Analyze of interaction between time and gender and time and operated/non-operated has been done. There were no missing data for any variable. A P value of < 0.05 was considered statistically significant.
The local ethics committee approved the study and all the patients included signed an informed consent form.
RESULTS
1. Patients
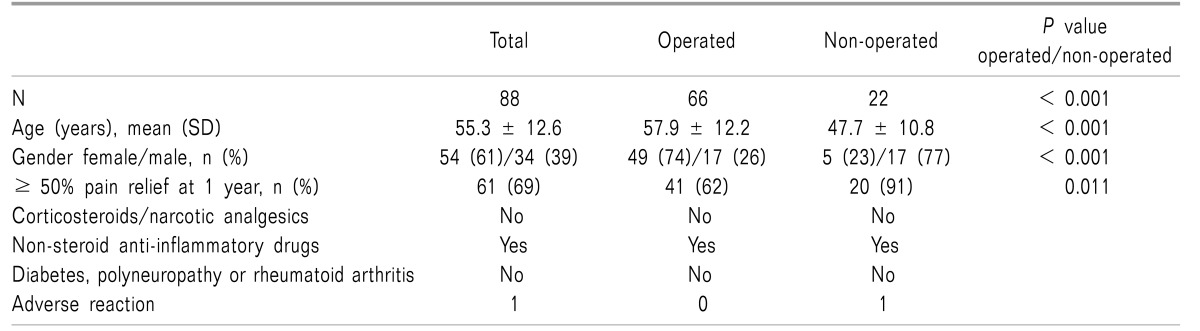
The mean age of the 88 patients was 55 ± 12.6 years, 34 (39%) were male and 54 (61%) were female. Sixty-six patients had previously been operated on with a technique of one-level one-sided micro discectomy. Twenty-two of the patients included had not had any kind of previous surgical intervention (Table 1).
Table 1. Demographic Data for the 88 Included Patients Treated with Epiduroscopy and Divided in Operated and Non-operated.
All patients were free to take non-steroid anti-inflammatory drugs. No information is available concerning the consumption of these drugs during follow-up.
One female patient in the non-operated group had atrial fibrillation during the epiduroscopy procedure. She was hospitalized overnight and discharged the following day with a normalized heart-beat and was not excluded from the study. No other patient experienced any adverse events (Table 1).
There was a significant decline in both VAS (P < 0.001) and ODI (P < 0.001) scores from pre-epiduroscopic values to values at one month, six months and the oneyear follow-up. After pairwise correction all remained significant.
Sixty-one (69%) patients had at least a 50% relief or more at the 1-year follow-up.
All patients responded to the treatment except one who had the same VAS and ODI scores at pre-epiduroscopy and at all the follow-ups.
2. Gender
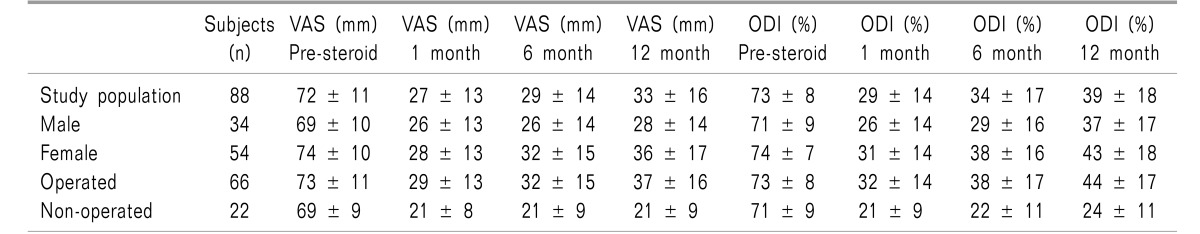
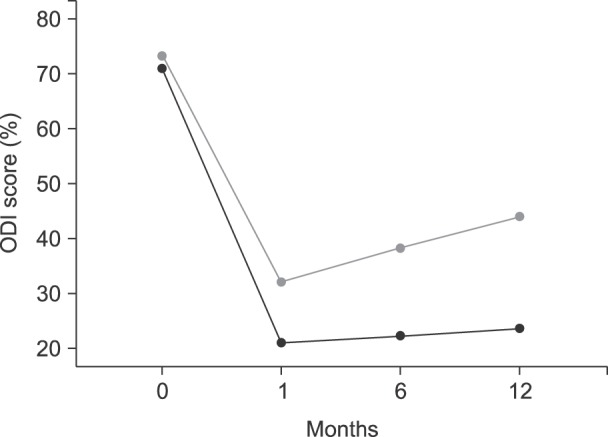
We found no difference between females and males before the epiduroscopy. There was a significant difference over time between gender and VAS (P = 0.026) and gender and ODI (P = 0.012). The interaction between time and gender was significant for ODI (P = 0.041) but not for VAS (P = 0.138) (Fig. 1 and 2, Table 2).
Fig. 1. Visual analogue scale (VAS) for male (black) and female (grey) patients at pre-epiduroscopy (0), 1 month, 6 months and one year. There was a significant difference over time between gender and VAS (P = 0.026). The interaction between time and gender was not significant for VAS (P = 0.138).
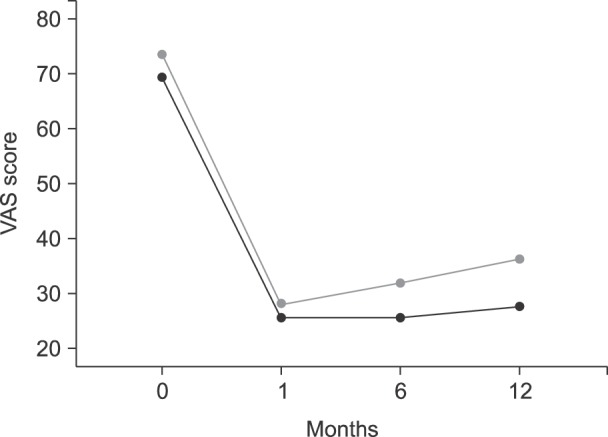
Fig. 2. Oswestry disability index (ODI) for male (black) and female (grey) patients at pre-epiduroscopy (0), 1 month, 6 months, and 1 year. There was a significant difference over time between gender and ODI (P = 0.012). The interaction between time and gender was significant for ODI (P = 0.041).
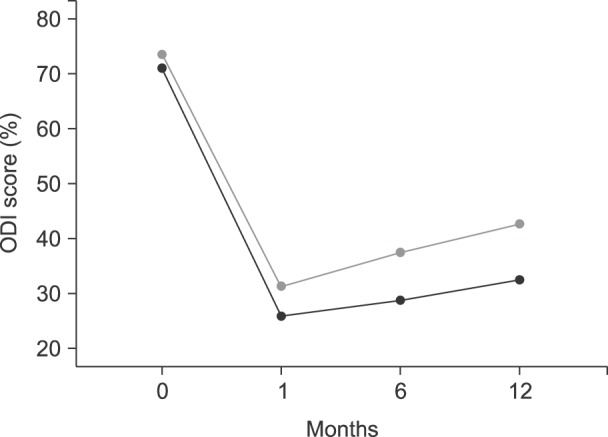
Table 2. VAS and ODI at the Different Follow-up Times for the Whole Study Population, for Gender and for the Previously Operated and Non-operated Groups.
All values are given as means and standard deviations. VAS: visual analogue scale, ODI: oswestry disability index.
3. Operated/Non operated
No significant difference was found for either VAS or ODI in the pre-epiduroscopy values between the operated and non-operated groups. However, there was a significant difference over time between the operated/non-operated and VAS (P < 0.001) and between operated/non-operated and ODI (P < 0.001).
Also the interaction between time and operated/nonoperated was significant for VAS (P < 0.001) and ODI (P = 0.002) (Fig. 3 and 4, Table 2).
Fig. 3. Visual analogue scale (VAS) scores for operated (grey) and non-operated (black) patients at pre-epiduroscopy (0), 1 month, 6 months, and 1 year. There was a significant difference over time between the operated/non-operated and VAS (P < 0.001). Also the interaction between time and operated/non-operated was significant for VAS (P < 0.001).
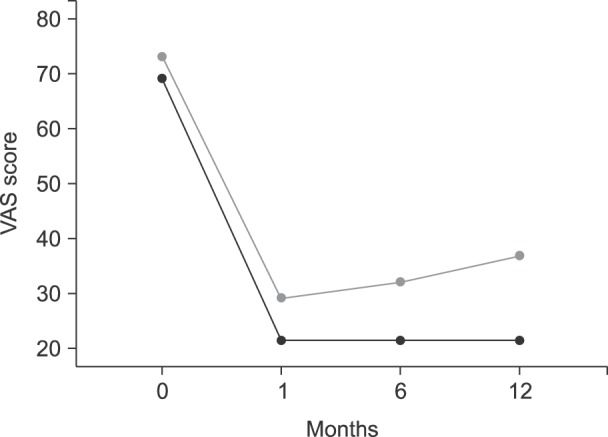
Fig. 4. Oswestry disability index (ODI) scores for operated (grey) and non-operated (black) patients at pre-epiduroscopy (0), 1 month, 6 months, and 1 year. There was a significant difference over time between the operated/non-operated and ODI (P < 0.001). Also the interaction between time and operated/non-operated was significant for ODI (P = 0.002).
DISCUSSION
Epiduroscopy with adhesiolysis and steroid injection helps to relieve pain and reduce disability in patients with back and leg pain due to lumbar disc herniation, regardless of gender. Patients who had not had previous surgery seemed to benefit more from the treatment. The improvement in pain relief and reduced disability seemed to last for at least 1 year.
Many studies have investigated the pathophysiology of lumber pain. In patients with disc degeneration an increase in prostaglandins, TNF, various interleukins and agents such as NO (Nitric Oxide) have been found [9]. These inflammatory agents are thought to cause the pain. Removing them from the epidural space may have positive effects on the pain. Therefore, many attempts have been made to remove these inflammatory agents from the epidural space. One of the most popular techniques for doing this is the epiduroscopy where the epidural space is washed with saline and mechanical adhesiolysis is performed by the catheter.
Our patients did indeed gain significant benefit in the first six months of our study, probably because the epidural space was washed with saline and the inflammatory agents were removed from the epidural space during the epiduroscopy procedure [10]. Additionally, the steroid injection into the epidural space at the end of the procedure is likely to increase the benefits to the patients. The steroid injection and the washing of the epidural space not only diluted the inflammatory agents in the environment but also reduced the edema in the nerve root and increased the blood circulation, thereby reducing the ischemia. All these factors help to decrease the chronic back pain and radicular pain [11].
All patients in our study graded their pre-epiduroscopy pain on the VAS as moderate, mean 72 mm, which is in the upper range and close to the severe pain level. The patients graded their limitations in daily living as being crippled, having serious problems in daily life.
However, a substantial improvement was already seen in both VAS and ODI values at the one-month follow-up with the patients then grading the pain as mild and their disability as moderate. Most other studies present results at three months and also show improvement in pain. In the long-term results after one year the pain was graded as mild and the disability still as moderate, which is in accordance with others. There seems to be a gradual but slow worsening of the patient's pain and disability from 6 months up to the 1-year follow-up. However, at the one-year follow-up there is still a significant improvement in pain and disability problems compared to pre-epiduroscopy levels. Others have reported higher number of patients with ≥ 50% improvement in both VAS and ODI [12]. However, in these studies they have had a high number of drop outs and crossover between groups which make it difficult to compare the results [12,13].
There were no gender differences in pre-epiduroscopy values. Men and women improved significantly both at the early and at the one-year follow-ups. An increase in VAS and ODI scores was also noted for men and women between the later follow-up times, indicating a slight worsening of the patients' problems. We have not found any studies comparing gender.
Both the operated and non-operated groups already had improved VAS and ODI scores after one month and an improvement was also seen after one year. During the follow-up a worsening in pain and disability was found in the operated group, but not in the non-operated group. The non-operated group seem to maintain the improvement over time, at least for the first year after treatment. Thus the effect of epiduroscopy treatment is better in the non-operated group with reduced pain and improvements in daily activities. We only had one complication and others have also found the complication rate to be low [12].
The advantage of the epiduroscopy procedure compared to other methods is that it is possible to determine the pain region more precisely. With the help of the rotatable camera, an increased hydrostatic pressure can be achieved in the pain region by mechanical compression or by washing with saline. The more precise identification of the troubled area means that the washing procedure and the steroid injection can be targeted on the exact site of the pain [9,10].
Epidural fibrosis has largely been held to be the cause of post-laminectomy syndrome [14,15]. The fibrous tissues surrounding the nerve root and the epidural space lead to pain. Cleaning the fibrosis from around the nerve root, with the help of the camera's mechanical movements and the washing procedure, gives the nerve root mobility. This situation provides another long-term benefit as it causes an increase in the blood flow in the nerve root and therefore reduces the pain [4,12].
In our study, there was a significant improvement up to the six-month follow-up, and then a slight worsening occurred in the VAS and ODI scores at the one-year follow-up. We do not know why the worsening occur. However, we may speculate that reformation of fibrosis and an inflammatory reaction may cause it [12]. This may be explained by the reformation of fibrosis. The epidural adhesions and fibrosis was found to be present after surgery, and most pronounced at the 3rd month after the surgery. Although it is the most important cause for pain after the surgery, ongoing degenerative process in spine triggers the pain, with repeated secretion of cytokines and eventually causing more adhesions. There have been cases that presented with epidural scarring after 7 years of intervention also [16,17].
Our study may have several potential biases. The number of patients included might be insufficient, even if there were 88. The number of patients included might be too few for comparisons concerning gender and non-operated versus operated patients. We had no control over the consumption of analgesics during the follow-up period but we know that no narcotics were used during the time of the study. We did not use laser technology in our study and therefore do not know whether that might have improved pain relief and daily living.
In conclusion, the epiduroscopy helps to relieve pain and reduce disability in patients with back and leg pain due to lumbar disc herniation, regardless of gender. It seems that the patients who had not had previous surgery benefitted more from the treatment. However, the epiduroscopy procedure can offer a good alternative treatment for all groups of patients with these symptoms with an estimated improvement lasting for at least one year.
References
- 1.Rabinovitch DL, Peliowski A, Furlan AD. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. 2009;9:509–517. doi: 10.1016/j.spinee.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Overdevest GM, Vleggeert Lankamp CL, Jacobs WC, Brand R, Koes BW, Peul WC. Recovery of motor deficit accompanying sciatica--subgroup analysis of a randomized controlled trial. Spine J. 2014;14:1817–1824. doi: 10.1016/j.spinee.2013.07.456. [DOI] [PubMed] [Google Scholar]
- 3.Leveque JC, Villavicencio AT, Bulsara KR, Rubin L, Gorecki JP. Spinal cord stimulation for failed back surgery syndrome. Neuromodulation. 2001;4:1–9. doi: 10.1046/j.1525-1403.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 4.Jo DH, Kim ED, Oh HJ. The comparison of the result of epiduroscopic laser neural decompression between FBSS or not. Korean J Pain. 2014;27:63–67. doi: 10.3344/kjp.2014.27.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutze G. Heidelberg: Springer; 2008. Epiduroscopy: spinal endoscopy; pp. 12–16. [Google Scholar]
- 6.Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4:407–414. doi: 10.1016/s1526-5900(03)00716-8. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 8.Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Miyamoto H, Saura R, Harada T, Doita M, Mizuno K. The role of cyclooxygenase-2 and inflammatory cytokines in pain induction of herniated lumbar intervertebral disc. Kobe J Med Sci. 2000;46:13–28. [PubMed] [Google Scholar]
- 10.Lee GW, Jang SJ, Kim JD. The efficacy of epiduroscopic neural decompression with Ho:YAG laser ablation in lumbar spinal stenosis. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):S231–S237. doi: 10.1007/s00590-013-1407-7. [DOI] [PubMed] [Google Scholar]
- 11.Di Donato A, Fontana C, Alemanno D, Di Giacomo A. Epiduroscopy in treatment of degenerative chronic low back pain: a prospective analysis and follow-up at 60 months. Clin Res Regul Aff. 2010;27:69–74. [Google Scholar]
- 12.Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014;27:3–15. doi: 10.3344/kjp.2014.27.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013;16:185–196. [PubMed] [Google Scholar]
- 14.Kallewaard JW, Vanelderen P, Richardson J, Van Zundert J, Heavner J, Groen GJ. Epiduroscopy for patients with lumbosacral radicular pain. Pain Pract. 2014;14:365–377. doi: 10.1111/papr.12104. [DOI] [PubMed] [Google Scholar]
- 15.Ryu KS, Rathi NK, Kim G, Park CK. Iatrogenic intradural lumbosacral cyst following epiduroscopy. J Korean Neurosurg Soc. 2012;52:491–494. doi: 10.3340/jkns.2012.52.5.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dullerud R, Graver V, Haakonsen M, Haaland AK, Loeb M, Magnaes B. Influence of fibrinolytic factors on scar formation after lumbar discectomy. A magnetic resonance imaging follow-up study with clinical correlation performed 7 years after surgery. Spine (Phila Pa 1976) 1998;23:1464–1469. doi: 10.1097/00007632-199807010-00007. [DOI] [PubMed] [Google Scholar]
- Mohi Eldin MM, Abdel Razek NM. Epidural fibrosis after lumbar disc surgery: prevention and outcome evaluation. Asian Spine J. 2015;9:370–385. doi: 10.4184/asj.2015.9.3.370. [DOI] [PMC free article] [PubMed] [Google Scholar]