Abstract
Background
We aimed to investigate the prevalence of unrecognized depression in patients with chronic pain, but with no history of psychiatric diseases.
Methods
Patients with chronic pain who did not have a history of psychiatric disease were selected for this study. The Beck Depression Index (BDI) was used to evaluate depression. Participants' socio-demographic characteristics and pain-related characteristics were also recorded.
Results
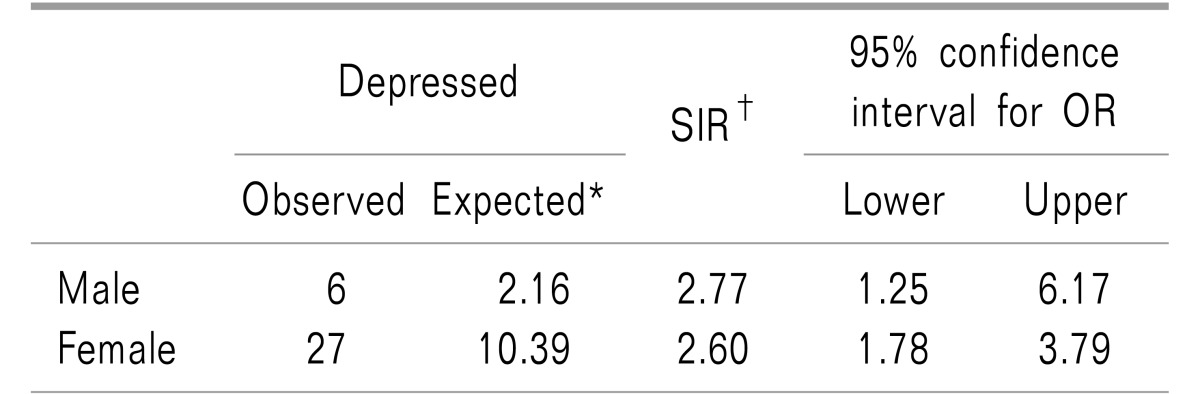
The study included 94 consecutive patients with chronic pain (28 men and 66 women). Based on the BDI scores, 33/94 (35.1%) patients with chronic pain had comorbid depression. The prevalence of depression was significantly higher in our cohort than it was in the general population (P < 0.001). The standardized incidence ratio, adjusted for age and sex, was 2.77 in men and 2.60 in women. Patients who were unmarried (odds ratio [OR] = 3.714, P = 0.044), and who had subjective sleep disturbance (OR = 8.885, P < 0.001), were more likely to have moderate to severe depression. Patients with high education levels (OR = 0.244, P = 0.016), and who were economically active (OR = 0.284, P = 0.023), were less likely to have moderate to severe depression.
Conclusions
Our results indicate that unrecognized depression in patients with chronic pain is common. Therefore, pain physicians should actively seek to identify these problems rather than relying on the patient to volunteer such information.
Keywords: Age factors, Chronic pain, Delayed diagnosis, Depression, Marital status, Mental disorders, Outpatient clinics, Pain clinics
INTRODUCTION
Pain physicians focus primarily on the etiologic cause of a patient's pain. However, pain is a subjective experience, which is greatly influenced by emotional states. The International Association for the Study of Pain has defined pain as, “an unpleasant sensation and emotional experience associated with a real or potential damage to tissue, or the equivalent of such damage” [1]. Several studies have reported that negative emotional states such as depression, anxiety, and anger are particularly associated with chronic pain [2,3,4] and that patients with chronic pain have a greater prevalence of psychiatric disorders compared with the general population [5].
Depression is one of the most common psychiatric diseases associated with chronic pain, and the incidence of depression is higher in patients with chronic pain than in the general population [6]. The mean prevalence of comorbid major depression in pain clinics is reportedly 52% [7]. There are few Korean studies on the association between chronic pain and depression. Kim et al. [8] assessed 97 Korean patients with spinal stenosis using the Beck Depression Index (BDI) and found that 54 of the patients (55.7%) had scores that were above the threshold for depression (> 14 points). Although the prevalence of depression in chronic pain patients varies across countries and cultures, many chronic pain patients are likely to have comorbid depression.
Not only do depression and chronic pain commonly occur together, they also share many common neurobiological pathways and can affect one another [9]. A number of studies have investigated the effects of depression on the outcomes of chronic pain patients [10,11,12]. These studies found that patients with chronic pain and comorbid depression experienced more intense pain and longer durations of pain than chronic pain patients without depression [10,12]. It was also reported that comorbid depression was a significant predictor of the onset of persistent pain [6] and that depression had an adverse effect on treatment outcomes by decreasing a patient's ability to cope with pain [12]. Additionally, depression itself can cause pain [13]. Thus, it is important to identify and treat depression in patients with chronic pain.
Although many studies have investigated the relationship between depression and chronic pain, the results of these studies do not benefit patients unless these conditions are properly identified and treated. Pain physicians must be able to identify patients with depression even if these patients have never been treated and do not complain of depressive symptoms. There has been no study specifically investigating pain physicians' ability to recognize depression, however, evidence suggests that many cases of depression go undetected by non-psychiatric physicians [14,15,16].
Psychiatric diseases such as depression do not have specific markers for diagnosis and there are no objective tests that can be easily performed by non-psychiatric physicians. Evaluations for comorbidities also depend on patients self-reporting their history and symptoms. However, unlike other comorbidities, patients are often reluctant to reveal a history of depression or seek professional help due to the stigma [17,18]. Therefore, the absence of a psychiatric medical history or self-reported symptoms does not exclude the possibility of depression. As a result, depression is often not identified at pain clinics even though it can greatly affect the prognosis of these patients.
Therefore, the present study aimed to determine the prevalence of unrecognized depression (not detected through medical histories) in patients with chronic pain. In addition, we investigated how chronic pain patients, with comorbid depression, express their depressive symptoms to pain physicians. We also investigated the characteristics of chronic pain patients at risk for moderate-to-severe depression.
MATERIALS AND METHODS
The study population consisted of consecutive outpatients who visited our pain center from November 2015 to August 2016. Patients with chronic pain (defined by a duration of six months or longer) without a history of psychiatric disease were included in the study. Patients who did not agree to participate, or who had difficulty understanding the questionnaires, were excluded. In all, 109 participants completed the Beck Depression Index (BDI) prior to meeting with a pain physician. Three pain specialists helped perform the study, all of whom had at least 5 years of experience in pain management. We also collected patient sociodemographic information (gender, age, education level, marital status, employment status, monthly income, residential area, and other medical conditions) and pain-related information (numeric rating scale and duration of pain) to characterize the patients with depression. This study was approved by our hospital's Institutional Review Board, and written informed consent was obtained from all participants.
We used the BDI to evaluate depression. The BDI is widely used, and its efficiency has been demonstrated in clinical studies [19,20]. Moreover, the validity of the BDI in assessing depression among patients with chronic pain has been confirmed in a previous study [21]. The BDI consists of 21 self-rated questions that evaluate the patient's mood during the last week. Each question is rated on a scale of 0–3, with the total score ranging from 0 to 63. Based on the results of a national BDI standardization study, patients in the present study were considered to have depression if the BDI total score was ≥ 16 in men or ≥ 17 in women [19]. The severity of depression was also assessed. In men, scores of 16–19, 20–23, and > 24 were considered mild, moderate, and severe, respectively; in women, scores of 17–20, 21–24, and > 25 were considered mild, moderate, and severe, respectively [19]. The pain physicians in this study were blinded to the results.
Participants were followed for at least one year after completion of the survey to determine if they received further psychiatric evaluation or treatment during this period. We reviewed the patients' electronic medical records to determine whether they had complained to their doctors about depressive symptoms. Pain physicians recorded when patients complained of emotional distress, such as depressed mood, as well as their suspicion of depression in the medical records. Phrases related to an emotional state were also investigated in the medical records.
We calculated that 60 was the number of patients required for the detection of a difference of 15% in the prevalence of depression between the general population and chronic pain patients, including a 20% dropout rate, using a single proportion two-sided exact test at a significance level of 5% and 80% power using PASS 15.0.1 (NCSS statistical software, Kaysville, UT).
All statistical analyses were performed using the R statistical software (version 3.2.3; R Foundation for Statistical Computing, Vienna, Austria) and indirect standardization for the epidemiological analysis was performed using Epitools version 0.5–7 [22]. Data are presented as the mean ± standard deviation or as the number and percentage. Comparisons were conducted using Student's t-test and Pearson's chi-squared test.
To assess whether the prevalence of depression in this study was significantly different from that of the general population, we used an indirect standardization to the general population using data from the Korea National Health and Nutrition Examination Survey (KNHANES VI-1) [23].
The factors associated with moderate-to-severe depression were examined using a logistic regression analysis. Moderate-to-severe depression was defined as a BDI score ≥ 20 in men or ≥ 21 in women based on cutoff values reported in a previous standardization study [20]. In the study comparing the BDI and DSM-IV criteria, the optimal cut-off value for depression on the BDI scale was 21 or greater [21]. Therefore, we used the cutoff value for moderate depression (a BDI score ≥ 20 in men or ≥ 21 in women) as a dependent variable in the univariate logistic regression analysis to evaluate the odds ratios and 95% confidence intervals (CIs) of related factors. P values < 0.05 were considered statistically significant.
RESULTS
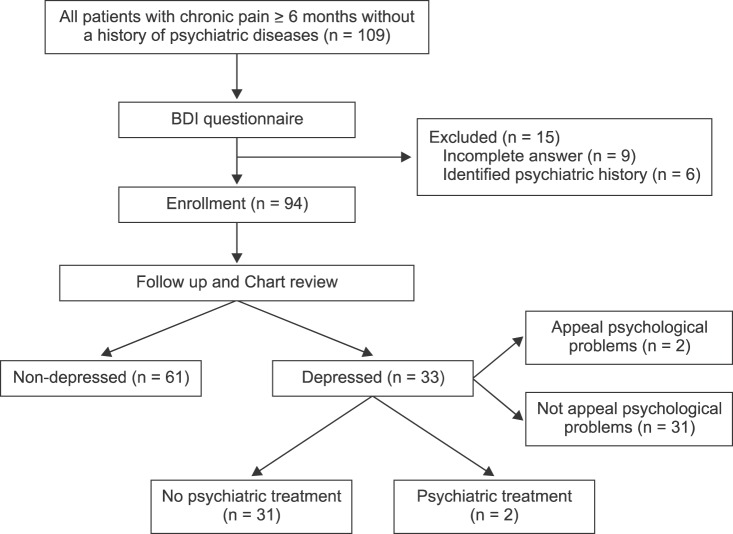
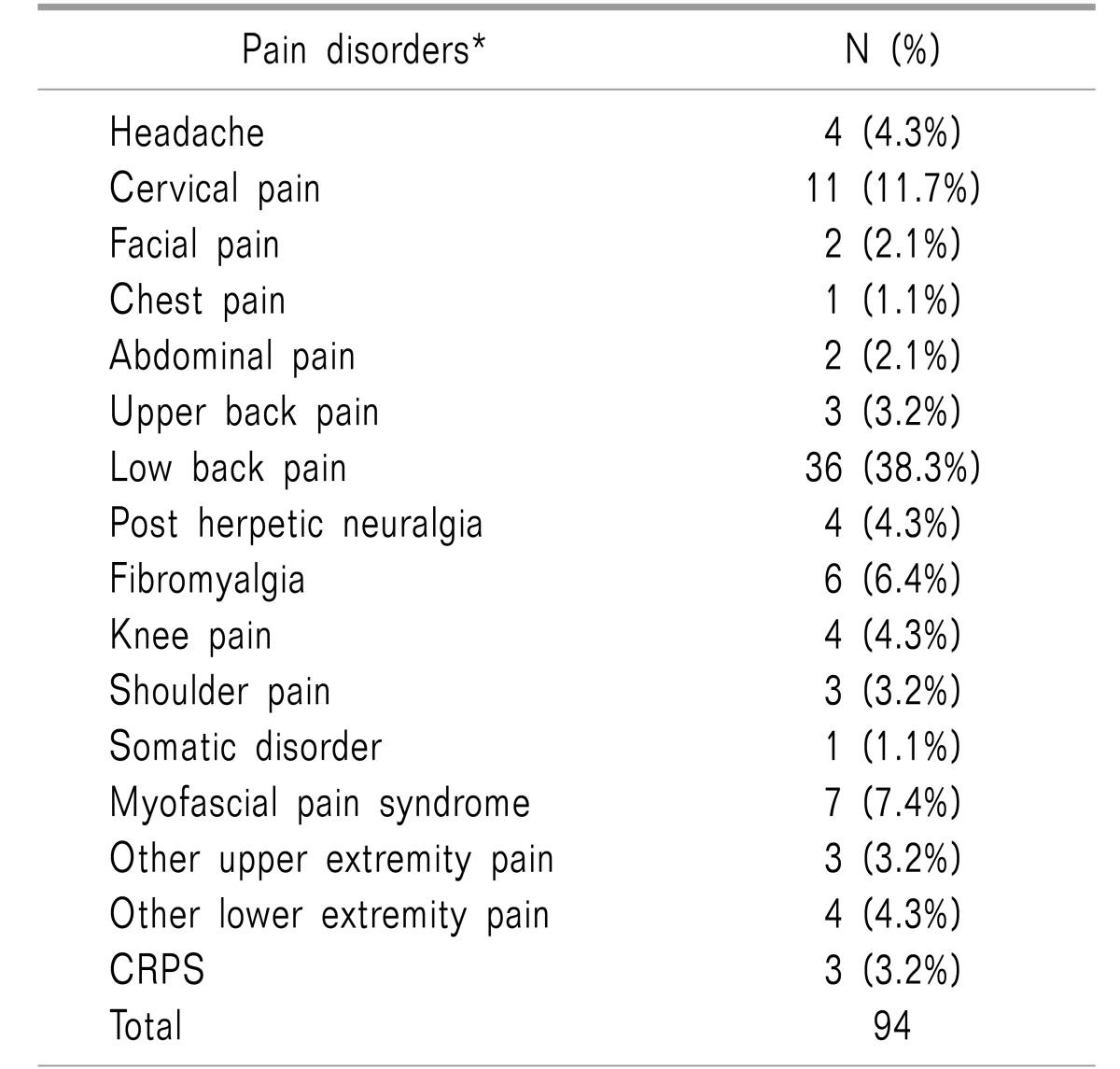
The data from 94 participants (28 men and 66 women) were included in the final analysis, following the exclusion of participants with incomplete responses (n = 9) or a confirmed history of a psychiatric disorder upon further investigation (n = 6) (Fig. 1). In order to investigate the relationships of various variables, the final number of patients included more than the number of subjects originally planned. However, this study was very low-risk since it used questionnaires. Patients had a variety of pain disorders (Table 1), however, the most frequent was low back pain (n = 36, 37.5%) followed by cervical pain (n = 11, 11.5%). Because our hospital has a separate cancer pain clinic, none of the patients in this study had cancer-related pain.
Fig. 1. Flow diagram showing the inclusion process of subjects in the study. BDI: Beck depression index.
Table 1. Various Types of Chronic Pain in the Study.
*If there is a more specific diagnosis, this is the priority.
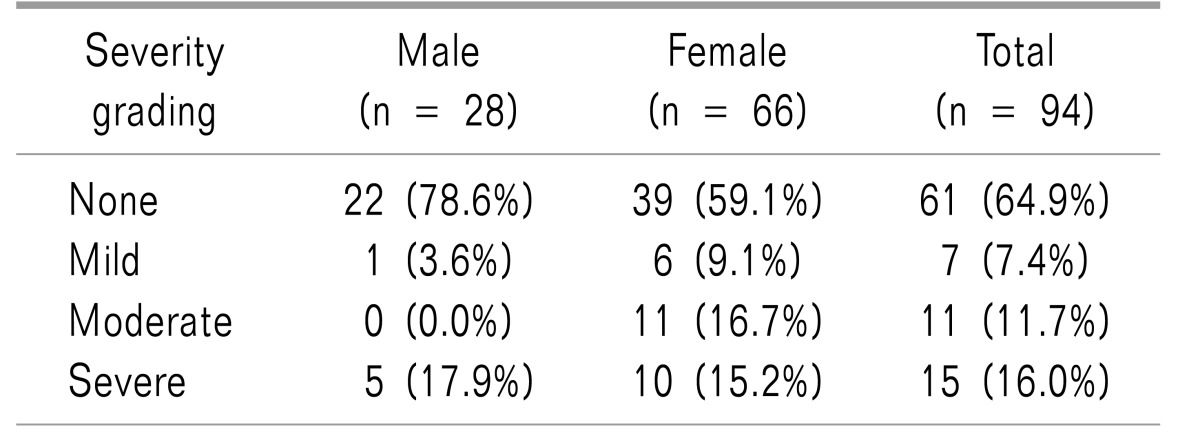
The mean BDI scores for the total study population were 14.84 ± 10.9 (12.7 ± 14.0 in men and 15.7 ± 9.3 in women). The prevalence of depression across the entire study population, as defined by a BDI score ≥ 16 in men or ≥ 17 in women, was 35.1% (21.4% in men and 40.9% in women). The patients considered to have depression were graded according to severity as shown in Table 2.
Table 2. Severity Grading of Patients with Depressive Symptoms.
Based on BDI score, in men, scores of 16.19, 20.23, and > 24 were considered mild, moderate, and severe, respectively, while in women, scores of 17.20, 21.24, and > 25 were considered mild, moderate, and severe, respectively.
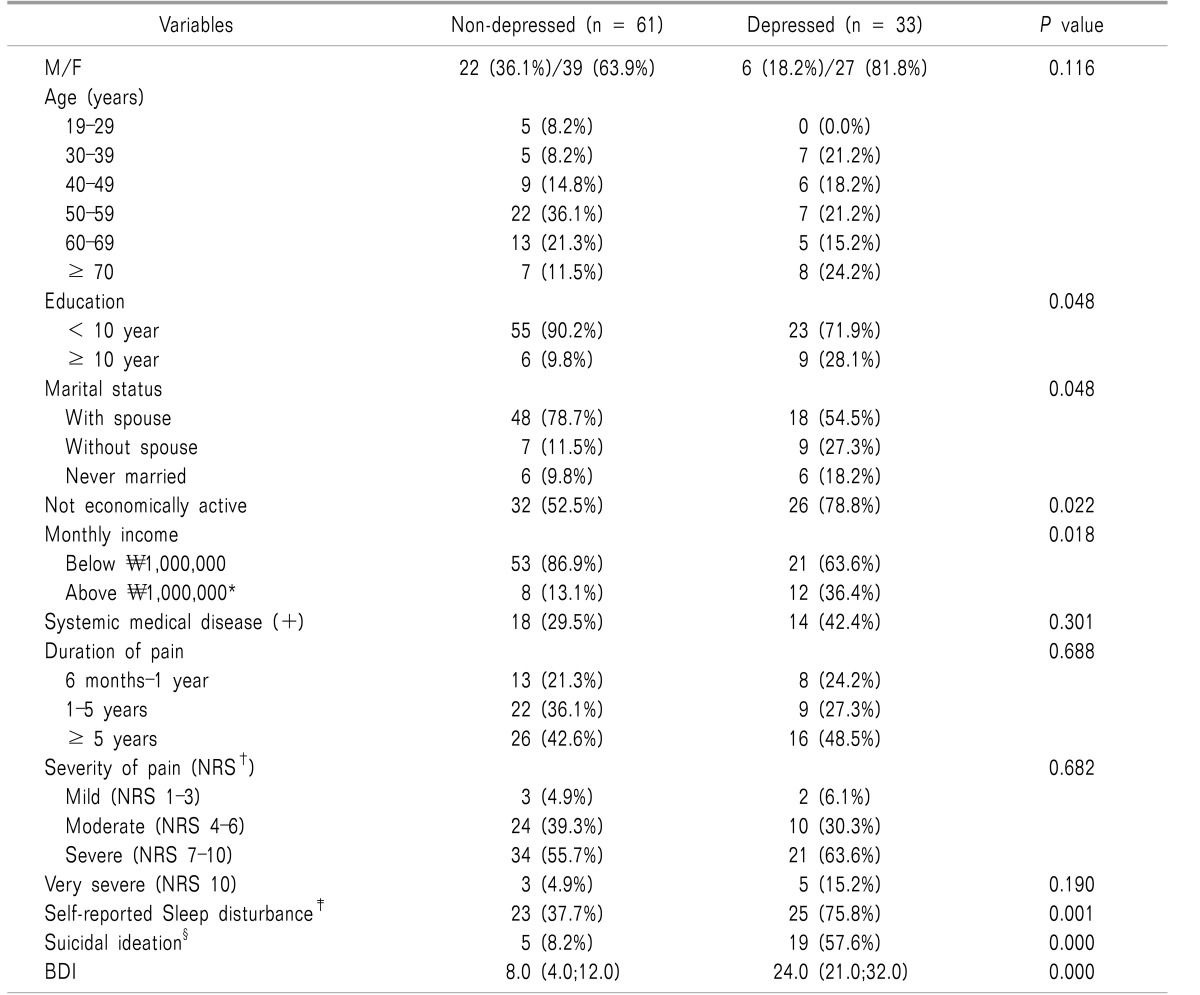
Education level, marital status, occupation, monthly income, and the incidence of self-reported sleep disturbances were significantly different between patients with and without depression (Table 3).
Table 3. Sociodemographic and Pain-frelated Characteristics between the Depressed and the Non-depressed Patients.
*The lower 10th percentile of income, †NRS: numeric rating scale, ‡Sleep disturbance that patients complain when they are interviewed, §More than one point on the question of suicidal ideation in BDI.
Patients with a pain numerical rating scale (NRS) rating of 10, the most severe pain, were classified according to the presence of depression because other factors are likely to affect pain severity. A higher proportion of patients with depression had an NRS rating of 10 compared to those without depression, but this difference was not statistically significant.
Because the prevalence of depression varies with age and sex, we adjusted for age and sex through indirect standardization to compare our finding with the prevalence of depression identified in the general population using data from the KNHANES VI-1 study [23] (Table 4). The standardized incidence ratios for depression in men and women were 2.77 (95% CI: 1.78–6.17) and 2.60 (95% CI: 1.25–3.79), respectively.
Table 4. Results of Indirect Standardization by Sex and Age.
*The prevalence was based on Korea National Health and Nutrition Examination Survey (KNHANES) VI, 2013 [23], †Standardized Incidence Ratio.
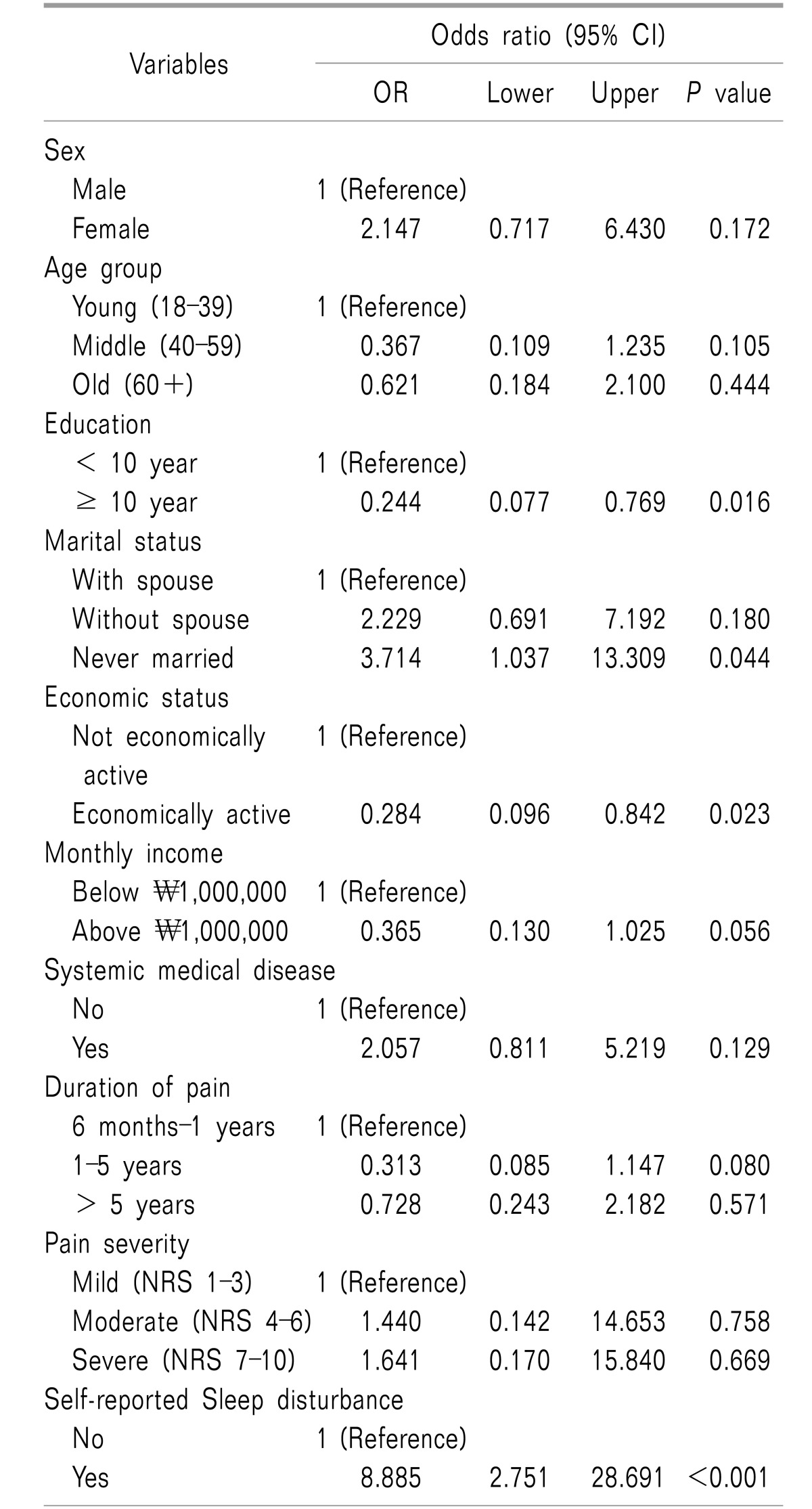
Table 5 shows the results of the univariate logistic regression analysis in which the relationships between the presence or absence of moderate-to-severe depression and sociodemographic and pain-related characteristics were analyzed. The analysis revealed that patients who were never married, were not economically active, and who had subjective sleep disturbance, had significantly higher frequencies of moderate-to-severe depression compared with their counterparts in each of these categories. Patients who had a higher level of education (≥ 10 year), and who were economically active, had significantly lower frequencies of moderate-to-severe depression compared with their counterparts in each of these categories.
Table 5. Univariate Logistic Regression Analysis for Factors Associated with Moderate to Severe Depressive Symptoms.
Patients in this study were followed for at least one year after completing the survey. During this period, we found that only two patients received psychiatric treatment (Fig. 1). One patient was suspected to have a somatoform disorder and was referred to a psychiatrist by a pain physician; that patient is currently being treated for a major depressive disorder by a psychiatrist. The other patient voluntarily visited a psychiatrist and was diagnosed with a major depressive disorder; this patient is also currently receiving treatment for depression. The BDI scores of these two patients were 28 and 40, respectively. During the follow-up period, only two patients voluntarily discussed their psychiatric problems with their pain physicians (Fig. 1). One of these two patients was the one who voluntarily visited a psychiatrist as mentioned above; the other patient did not receive any additional treatment for depressive symptoms. Additionally, in the BDI question about suicide, 5 patients answered, ‘I would like to kill myself’ (score 2), and one patient answered, ‘I would kill myself if I had the chance’ (score 3); their average BDI was 32.2 ± 8.3. Only one of these patients received psychiatric treatment; the other five patients received no further psychiatric evaluation or treatment.
DISCUSSION
This study aimed to investigate the prevalence of unrecognized depression in chronic pain patients without a history of psychiatric disease. Because non-psychiatrists often fail to accurately recognize depression [14], we hypothesized that many chronic pain patients have undiagnosed depression. Our results showed that the prevalence of depression in patients with chronic pain, but without a history of psychiatric disease, was 35.1%, which is similar to the prevalence identified in prior epidemiologic studies [7]. However, unlike previous studies, the present study only evaluated chronic pain patients without a history of psychiatric disease, which provides important clues about patients' depression in a busy clinical setting. Despite excluding patients with a psychiatric history, the prevalence of depression in this study (35.1%) was still significantly higher than that of the general population (10.3%) [23].
Considering the negative perceptions about depression [17,18] and the low utilization rate of psychiatric services in Korea [24], depression is unlikely to be recognized in patients with chronic pain. Moreover, depression will affect the clinical outcomes of patients with chronic pain by the interactions between the chronic pain and their other conditions.
There are many potential explanations for the under-recognition of depression in patients with chronic pain, including physicians' lack of knowledge about depression, limited time to evaluate patients, and the lack of available treatment providers [25].
Among the many potential reasons for why depression goes unrecognized, we focused on the specific characteristics of patients who visit pain clinics. First, pain clinic patients often discuss their physical symptoms with their physician but not their psychiatric problems [26]. In this study, only two patients voluntarily mentioned their depressive symptoms to their doctor. Patients may be unaware that they are depressed or may minimize their depressive symptoms for fear of being further stigmatized. Many patients are reportedly afraid of using psychiatric services or of being labeled with a psychiatric illness in Korea [27]. The stigmatization and shame that are associated with mental illness have been suggested as barriers to the use of psychiatric services [28]. As a result, the utilization rate of psychiatric services in Korea is much lower than that of other developed countries. According to an epidemiologic investigation, only 15.3% of individuals with psychiatric diseases discuss their mental health with a psychiatrist, other physician, or mental health professional [24].
Second, if a patient chiefly complains of pain, this can interfere with a physician's recognition of psychiatric problems. Menchetti et al. [29] reported that depression often goes unrecognized if patients complain of physical pain. To explain this phenomenon, the authors suggested that physicians likely focus on various diagnostic procedures to identify an organic cause of pain. Similarly, another study reported that patients' pain affects the physicians' behaviors [30]. If patients complain about pain, then physicians tended to spend more time performing technical procedures, such as physical examinations, or discussing diagnostic and therapeutic strategies [30]. Because patients who visit pain clinics characteristically focus on pain complaints, pain physicians may fail to identify comorbid psychiatric problems.
The results of the present study demonstrate that detecting depression through medical history and/or voluntary self-reporting is insufficient. Considering the high prevalence of depression in chronic pain patients and the effects of depression on chronic pain, pain physicians must be more proactive in assessing depression in this population. Self-report depression questionnaires are known to improve the accuracy of detecting depression in patients when used by non-psychiatric physicians.
Among the various screening tests for depression, we recommend the Patient Health Questionnaire-2 (PHQ-2) in busy clinical settings, which the United States Preventive Services Task Force Recommendation Guidelines proposed using in the general adult population [31]. The PHQ-2 only utilizes two of the nine questions from the PHQ-9, namely those on depressive mood and anhedonia; thus, this test can be performed quickly and easily without increasing the consultation time. An answer of “yes” to either of the two PSQ-2 questions can detect depression with a sensitivity of 85–90%; answering “yes” to both questions yields a sensitivity of 95% [32].
As chronic pain itself is a strong risk factor for depression, it is reasonable to conduct depression screenings in all patients who visit a pain clinic. Pain physicians should also discuss with patients the relationship between chronic pain and depression. By doing so, patients who visit pain clinics may more freely discuss their emotional problems.
Finally, the role of pain specialists does not end with the diagnosis of depression. If there is moderate depression that may affect the prognosis and the treatment of chronic pain, close coordination with a psychiatrist is required. In addition, pain specialists will need a basic understanding of various psychiatric disorders, including depression.
The current study also revealed that chronic pain patients with a low education level (middle school or below), who were never married, and who were not economically active were more likely to have comorbid depression. These results are consistent with the known risk factors of depression in the general population [33]. Although the prevalence of depression increased with the severity of pain (NRS), there was no statistically significant correlation. However, previous studies have reported that depression increases with severity of pain [34,35]. In addition, no statistically significant relationship was identified between the duration of pain and the presence of moderate-to-severe depression. Likewise, a previous study reported that the duration of pain was not associated with the onset of depression [35]. These findings suggest that pain physicians should not exclude the possibility of psychiatric problems in patients with short pain durations or mild pain (NRS 1–3).
Finally, chronic pain patients with subjective sleep disturbances were more likely to have comorbid depression. Sleep disorders are closely related to chronic pain and depression, which interact with each other and affect the prognosis of the patient [36]. Therefore, sleep evaluation is very important in the management of chronic pain.
This study has several limitations. First, although the reliability and validity of the BDI have been well demonstrated, the ability to diagnose major depressive disorders is limited using only questionnaire scores. Second, because this is a single-center study involving only three pain specialists, it is difficult to generalize these results to all pain physicians. Third, this study does not reflect differences in clinical practice across different countries. In Korea, physicians have a limited amount of time to spend with patients, which may have affected the results of this study. In addition, studies on the relationship between chronic pain and depression have not yet been actively conducted in Korea. Since, the development of depression varies according to country, culture, and race, it is necessary to conduct research that reflects domestic circumstances. In addition, since this study is a cross-sectional study, it was not possible to determine whether the depression of the patient existed before the chronic pain or the if depression occurred following the onset of chronic pain. Fishbain et al. [37], in a literature review of the temporal relationship between depression and chronic pain, suggested that depression occurred as a result of chronic pain. Further researches are needed to determine what mechanism is associated with the development of depression in patients with chronic pain and how this affects the prognosis of treatment in patients with chronic pain. Finally, because this study included patients with various types of chronic pain, the prevalence of depressive symptoms according to each pain condition could not be determined.
In conclusion, this study evaluated the prevalence of unrecognized depression in patients with chronic pain using valid screening tools. The results of this study indicate that many chronic pain patients without a psychiatric history do in fact have depression. Chronic pain and depression are frequently comorbid and may impair patients' quality of life and reduce the effectiveness of pain treatment. However, depression in patients with chronic pain often goes undiagnosed and untreated.
Although many studies have investigated the relationship between depression and chronic pain, the results of these studies do not benefit patients unless these conditions are properly identified and treated. Pain physicians need to be aware that many patients with chronic pain have unrecognized depression; thus, more proactive measures should be taken to identify patients with depression rather than relying on medical history and voluntary self-reporting of depressive symptoms. Based on the results of this and previous studies, we believe that depression screening questionnaires should become the standard of care for patients with chronic pain.
ACKNOWLEDGEMENTS
The authors declare no potential conflicts of interests with respect to the research, authorship, and/or publication of this article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors thank the Division of Statistics in the Medical Research Collaborating Center at Seoul National University Bundang Hospital for assistance with the statistical analyses.
Footnotes
Previous presentation at conferences: The 63rd Korean Pain Society Scientific Meeting & Training Course, 19th Nov. 2016, Venue Grand Hilton Hotel Convention Center, Seoul, Korea.
References
- 1.Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain. 1979;6:249. [PubMed] [Google Scholar]
- 2.Keogh E, Cochrane M. Anxiety sensitivity, cognitive biases, and the experience of pain. J Pain. 2002;3:320–329. doi: 10.1054/jpai.2002.125182. [DOI] [PubMed] [Google Scholar]
- 3.Gatchel RJ, Turk DC. New York (NY): Guilford Press; 1999. Psychosocial factors in pain: critical perspectives. [Google Scholar]
- 4.Gaskin ME, Greene AF, Robinson ME, Geisser ME. Negative affect and the experience of chronic pain. J Psychosom Res. 1992;36:707–713. doi: 10.1016/0022-3999(92)90128-o. [DOI] [PubMed] [Google Scholar]
- 5.Benjamin S, Morris S, McBeth J, Macfarlane GJ, Silman AJ. The association between chronic widespread pain and mental disorder: a population-based study. Arthritis Rheum. 2000;43:561–567. doi: 10.1002/1529-0131(200003)43:3<561::AID-ANR12>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 6.Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 7.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 8.Kim AR, Seo BB, Kim JM, Bae JI, Jang YH, Lee YC, et al. Beck depression inventory score and associated factors in Korean patients with lumbar spinal stenosis. Korean J Pain. 2007;20:138–142. [Google Scholar]
- 9.Boakye PA, Olechowski C, Rashiq S, Verrier MJ, Kerr B, Witmans M, et al. A critical review of neurobiological factors involved in the interactions between chronic pain, depression, and sleep disruption. Clin J Pain. 2016;32:327–336. doi: 10.1097/AJP.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 10.Lamb SE, Guralnik JM, Buchner DM, Ferrucci LM, Hochberg MC, Simonsick EM, et al. Factors that modify the association between knee pain and mobility limitation in older women: the Women's Health and Aging Study. Ann Rheum Dis. 2000;59:331–337. doi: 10.1136/ard.59.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Croft PR, Papageorgiou AC, Ferry S, Thomas E, Jayson MI, Silman AJ. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine (Phila Pa 1976) 1995;20:2731–2737. doi: 10.1097/00007632-199512150-00015. [DOI] [PubMed] [Google Scholar]
- 12.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine (Phila Pa 1976) 1995;20:722–728. doi: 10.1097/00007632-199503150-00014. [DOI] [PubMed] [Google Scholar]
- 13.Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262–268. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- 14.Cepoiu M, McCusker J, Cole MG, Sewitch M, Belzile E, Ciampi A. Recognition of depression by non-psychiatric physicians: a systematic literature review and meta-analysis. J Gen Intern Med. 2008;23:25–36. doi: 10.1007/s11606-007-0428-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wancata J, Windhaber J, Bach M, Meise U. Recognition of psychiatric disorders in nonpsychiatric hospital wards. J Psychosom Res. 2000;48:149–155. doi: 10.1016/s0022-3999(99)00098-7. [DOI] [PubMed] [Google Scholar]
- 16.Kohli C, Kishore J, Agarwal P, Singh SV. Prevalence of unrecognised depression among outpatient department attendees of a rural hospital in delhi, India. J Clin Diagn Res. 2013;7:1921–1925. doi: 10.7860/JCDR/2013/6449.3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. 2006;40:51–54. doi: 10.1080/j.1440-1614.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- 18.Roeloffs C, Sherbourne C, Unützer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiatry. 2003;25:311–315. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- 19.Rhee M, Lee Y, Park S, Shon C, Jeong Y, Hong S, et al. A standardization study of beck depression inventory I-Korean version (K-BDI): reliability and factor analysis. Korean J Psychopathol. 1995;4:77–95. [Google Scholar]
- 20.Love AW. Depression in chronic low back pain patients: diagnostic efficiency of three self-report questionnaires. J Clin Psychol. 1987;43:84–89. [PubMed] [Google Scholar]
- 21.Geisser ME, Roth RS, Robinson ME. Assessing depression among persons with chronic pain using the Center for Epidemiological Studies-Depression Scale and the Beck Depression Inventory: a comparative analysis. Clin J Pain. 1997;13:163–170. doi: 10.1097/00002508-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Aragon T, Fay M, Wollschlaeger D. Vienna: Comprehensive R Archive Network; 2010. EpiTools: R package for epidemiologic data and graphics. [Google Scholar]
- 23.Ministry of Health and Welfare. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANESVI-1) Cheongju: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 24.Cho M, Sung S, Shin S, Kim J, Jeon S, Kim M. The epidemiological survey of mental disorders in Korea. Seoul: Ministry of Health and Welfare; [Google Scholar]
- 25.Goldman LS, Nielsen NH, Champion HC. Awareness, diagnosis, and treatment of depression. J Gen Intern Med. 1999;14:569–580. doi: 10.1046/j.1525-1497.1999.03478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Connor DW, Rosewarne R, Bruce A. Depression in primary care. 1: elderly patients' disclosure of depressive symptoms to their doctors. Int Psychogeriatr. 2001;13:359–365. doi: 10.1017/s1041610201007748. [DOI] [PubMed] [Google Scholar]
- 27.Cho SJ, Lee JY, Hong JP, Lee HB, Cho MJ, Hahm BJ. Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2009;44:943–951. doi: 10.1007/s00127-009-0015-7. [DOI] [PubMed] [Google Scholar]
- 28.Jang Y, Kim G, Hansen L, Chiriboga DA. Attitudes of older Korean Americans toward mental health services. J Am Geriatr Soc. 2007;55:616–620. doi: 10.1111/j.1532-5415.2007.01125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menchetti M, Belvederi Murri M, Bertakis K, Bortolotti B, Berardi D. Recognition and treatment of depression in primary care: effect of patients' presentation and frequency of consultation. J Psychosom Res. 2009;66:335–341. doi: 10.1016/j.jpsychores.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Bertakis KD, Azari R, Callahan EJ. Patient pain: its influence on primary care physician-patient interaction. Fam Med. 2003;35:119–123. [PubMed] [Google Scholar]
- 31.Whooley MA. Screening for depression—A tale of two questions. JAMA Intern Med. 2016;176:436–438. doi: 10.1001/jamainternmed.2015.8493. [DOI] [PubMed] [Google Scholar]
- 32.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hahm BJ, Kim JK, Cho MJ. Prevalence, incidence, and risk factors of dementia and depressive disorders of the elderly residing in the community: a two stage one-year follow-up study. J Korean Geriatr Psychiatry. 1999;3:140–148. [Google Scholar]
- 34.Wilson KG, Eriksson MY, D'Eon JL, Mikail SF, Emery PC. Major depression and insomnia in chronic pain. Clin J Pain. 2002;18:77–83. doi: 10.1097/00002508-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Gerrits MM, van Oppen P, van Marwijk HW, Penninx BW, van der Horst HE. Pain and the onset of depressive and anxiety disorders. Pain. 2014;155:53–59. doi: 10.1016/j.pain.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Nicassio PM, Wallston KA. Longitudinal relationships among pain, sleep problems, and depression in rheumatoid arthritis. J Abnorm Psychol. 1992;101:514–520. doi: 10.1037//0021-843x.101.3.514. [DOI] [PubMed] [Google Scholar]
- 37.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]