Abstract
Oral contraceptive pills (OCP) contribute a major share in the current method‐mix in Bangladesh. However, multiple studies show high discontinuation rates of OCP. The present study examines the behavior and attitude towards OCP use, and investigates the determinants of its discontinuation among the rural married women of Bangladesh.
The present study is based on critical analyses of the data from 24 focus group discussions and 135 in‐depth‐interviews with women, their husbands and key informants conducted over the period of 1 year.
The present study shows that more than two‐thirds of married women have at one time or another used OCP as a method of family planning. However, many women did not take the pills regularly and about one‐quarter of ever users had taken, at one stage or another, a ‘short break’ from OCP use. Although nearly half of them took a break because of side effects, interestingly, 16% took a break as the result of fear of health problems that were related to ‘folk stories’ and other misconceptions. The individual assessment by users of the national family planning service delivery, perceived side effects, misconceptions about continuous use of pills, quality of counseling and information, and contraceptive behavior of the OCP users considerably influenced the decisions on contraceptive use or non‐use. (Reprod Med Biol 2006; 5: 111–121)
Keywords: Bangladesh, discontinuation, family planning, oral contraceptive pills, pills use
INTRODUCTION
WITH A POPULATION of 125 million within an area of 150 000 km2, Bangladesh is one of the most densely populated countries in the world. 1 , 2 , 3 Since independence in 1971, the Government of Bangladesh (GOB) has viewed rapid population growth as a high priority problem, and decided to launch the national family planning (FP) program in the mid 1970s. Since then, GOB has attempted to strengthen the FP program through increased resource allocation, multisectoral collaboration, use of mass media campaigns, the introduction of field staff to provide domiciliary FP services, and the promotion of involvement of voluntary and private agencies. 4 , 5 , 6 , 7 , 8 These efforts have enabled Bangladesh to achieve remarkable increases in use of contraceptive methods, resulting in a dramatic decline in the Total Fertility Rates (TFR). The contraceptive prevalence rate (CPR) has increased from 9.6% of married couples in 1975 to 54% in 2000, and the TFR has declined in this same period from 6.3 children per woman to 3.3. 6 , 9 , 10 , 11 , 12
Although a major cause of declining fertility has been the steady rise in contraceptive use over the past two decades, the pace of fertility decline has slowed in the past 10 years, creating a major challenge for the GOB in its goal of achieving replacement‐level fertility by 2005. 5 , 13 The TFR has remained almost constant since 1991, even though the contraceptive use rate increased at almost two percentage points per year. 5 , 14 A number of authors have argued that fertility in south Asian countries might well stagnate at a TFR of about 3 for some time as a result of son preference, a shift towards adoption of a less effective method mix and high discontinuation rates of contraceptive methods resulting in many unwanted pregnancies. 14 , 15 , 16 , 17 A recent Demographic and Health Survey (DHS) shows that 31% of births are unwanted in Bangladesh. 11 , 18
Contraceptives play an important role in improving women's health by avoiding unwanted or mistimed pregnancies, reducing the risks of unsafe abortion, increasing birth intervals, and allowing women to recover from the strain of pregnancy. 5 , 6 , 12 , 19 It is argued that use of family planning also decreases women's exposure to the risk of maternal mortality and is unique in providing a range of non‐contraceptive health benefits including protection against endometrial and ovarian cancers. 20
During the mid 1970s and early 1980s, the FP program was dominated by semipermanent and permanent methods such as intrauterine devices (IUD), tubectomy and vasectomy. The most significant change since the late 1980s has been a shift away from permanent methods to modern temporary methods. There has been a rapid rise in the use rates of oral contraceptive pills (OCP), increasing CPR from 5% in 1985 to 21% in 1997. 14 , 21 In Bangladesh, OCP are a widely used contraceptive method, currently constituting 55% of the ‘method‐mix’ (for modern methods). Almost two‐thirds of ever‐married women have used a modern method of family planning at some point in their lifetime. However, a key concern for the FP program is the rate at which users discontinue contraceptives and the reasons for such discontinuation. 11 , 12 , 13 , 22 The present estimated overall cumulative (all reasons) one‐year discontinuation rate for OCP is 46.7%, meaning that nearly half of users discontinue pills within 12 months of starting. The proportion of first year pill users who discontinued has increased from 44.4% to 46.7% since 1996–1997. 11 The first generation of OCP contained larger doses of hormones (known as ‘standard dose pills’), but the new generation pills have a much lower dose of hormones (known as ‘low‐dose oral contraceptive pills’). In 1991, the National Technical Committee approved the introduction of low‐dose oral contraceptive pills into the national FP program in Bangladesh. Although a lower level of hormones has fewer side‐effects, a substantial proportion of women in developed countries still discontinue low‐dose OCP within the first few months of use. In the USA, the dis‐ continuation rate is 29% among OCP users. 23 Comparable evidence from developing countries also suggests higher discontinuation rates. 19 , 24 , 25 Moreover, one‐third of the unwanted pregnancies in south Asian countries are because of OCP misuse, failure or discontinuation. Thus, discontinuation of OCP use has been considered as a main factor hindering further decline in fertility. 6 , 12 , 25
Several studies have cited the experience of side‐effects or other health problems as the main reason for early discontinuation of OCP. 12 , 19 , 24 , 25 , 26 Half of Bangladeshi women who discontinue pill use attribute their decisions to side‐effects. 11 , 12 In Niger and Gambia, nearly 30% of new FP users discontinued use within the first 8 months of acceptance primarily because of side‐effects. 19 Others argued that behavioral and cultural factors also influence the contraceptive use dynamics and method choice. 5 , 18 , 23 , 27 , 28 In Indonesia, women who were given the method they desired had a discontinuation rate of 9%, compared with 72% for women who were not given their chosen method. 28 , 29 Evidence from several countries suggests that the rates of discontinuation were lower among women who received high quality FP services in terms of more counseling or information from reliable sources, and early management of side‐effects. 28 , 30 , 31 , 32 Furthermore, social and economical variables also affect the decision‐making process for method choice and use pattern of contraceptives. 5 , 6 , 12 Some studies showed that misconceptions about continued use of OCP, pregnancy resulting from missing pills and poor counseling of providers also influenced discontinuation of OCP. 18 The big challenge for the family planning program is to reduce the high levels of contraceptive discontinuation as a strategy for health promotion and maternal mortality reduction, and in order to reach national demographic goals.
The purpose of the present study was, therefore, to examine the behavior, attitudes and practice of rural women towards OCP with special attention to the dynamics of use and discontinuation of OCP.
METHODS
THIS WAS AN in‐depth, analytical study. The data were collected through focus group discussions (FGD) and in‐depth interviews with OCP ever users, never users, husbands, key informants and service providers. A comprehensive literature review and analysis of relevant secondary data were also carried out to put the study into perspective.
A structured questionnaire was used to collect information from service providers and a semistructured questionnaire was used for the in‐depth interviews. An instruction guide was also prepared for conducting the FGD. These research instruments were reviewed by a group of leading Bangladeshi researchers and were pretested before being applied. The data collectors were trained on the interview techniques and instruments.
For the present research, Kalihati Upazila (subdistrict) – a rural Upazila of Tangail district was selected on the basis of prevalence of OCP use. Three villages were then selected purposively from three different wards (union is the lowest administrative unit, and 3–5 wards constitute one union). To begin the process, each village was enumerated. 136 respondents were selected for interviews through systematic random sampling method, out of which 121 in‐depth interviews were conducted with current users, former users, and never‐users of OCP. These interviews were mostly one‐to‐one and informal, which allowed collection of in‐depth information and personal insights. In total, 24 FGD were conducted with three groups of respondents; women, husbands and key informants. In addition, all service providers of MCH and family planning (total 14) from the Upazila Health Complex, Union Health and Family Welfare Centers and the field were interviewed.
The in‐depth interviews explored issues of decision making around contraceptive use and non‐use, including: why contraceptives (and in particular OCP) are used or not, who plays a role in the decision making process, who provides advice to women, what actual experience of contraceptive use has been and why women stop or discontinue OCP. The interview protocol also asked questions to explore the influence of folk stories about OCP on women's family planning practice, in particular the often‐cited myth that long‐term use of OCP causes sterility. A separate questionnaire was designed for interviews with service providers and a FGD guide was produced to enable additional exploration of the study themes and collection of more qualitative information.
Data were analyzed by using statistical software, spss, and by applying qualitative analytical techniques. For the analysis, inconsistent OCP use referred to missing one or more pills per cycle while taking OCP. Discontinuation was defined as using OCP for a period of less than 2 years, excluding women who stopped using OCP because of desired pregnancy or because they were no longer in a sexual relationship. 33 A ‘short break’ was defined as a limited period of non‐use of OCP, usually less than 6 months, during which a woman still does not plan or desire to become pregnant but is not actively using another method and where she has the intention to return to OCP use following the break.
RESULTS
Study area and population characteristics
A TOTAL OF 568 households, with a population of roughly 2600 were enumerated. Average family size was 4.65 (median 4.0), with the smallest households consisting of one person and the largest household of 20.
The study area has benefited from years of construction‐related work (particularly bridge and road‐related) and an associated increase in commerce. Consequently, a higher proportion (70%) of the houses was ‘semipucca’, meaning they had both tin walls and tin roofs.
Table 1 presents a range of characteristics of the study sample. Respondents were between 16 and 46 years old, with a mean age of 29 years. Nearly one third of the respondents could write Bangla. The number of living children among interviewees ranged from 0 to 7, with the mean being 2.2 and the median being 2.0 children. Thirty‐eight percent had also had one or more stillbirths (with one women having four and another five stillbirths).
Table 1.
Study sample characteristics
| Selected variables | % (n = 121) |
|---|---|
| Can read Bangla | 44 |
| Can write Bangla | 32 |
| Highest school class completed (self) | |
| no school attended | 55 |
| between 1 and 5 | 18 |
| between 6 and 9 | 18 |
| SSC completed (class 10) | 8 |
| Highest class completed (husbands) | |
| No school attended | 46 |
| Between 1 and 5 | 14 |
| Between 6 and 9 | 17 |
| SSC completed (class 10) | 17 |
| HSC completed (class 12) | 4 |
| College degree completed | 3 |
| Religion | |
| Islam | 95 |
| Hindu | 5 |
| House construction | |
| Semi‐pucca | 71 |
| Katcha‐1 | 17 |
| Katcha‐2 | 3 |
| Involved in NGO programs (credit, income generating activities, other) | 47 |
| Ever pregnant | 94 |
| Ever used family planning | 84 |
| Currently using family planning | 65 |
| Ever used oral contraceptive pill | 70 |
| Currently using oral contraceptive pill | 36 |
NGO, non‐government organization.
Reasons for use of family planning methods
Figure 1 shows currently used family planning methods among the respondents.
Figure 1.
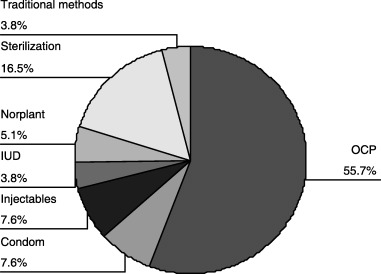
Currently used family planning methods.
About two‐thirds (59%) of women said they used FP methods for the first time because they did not want any more children. The next more common responses were stated as a desire to space the next child (40%) and economic reasons or poverty (22%). Exploration of different contraceptive methods is fairly common practice for women in the study area. Table 2 presents the proportion of women who had tried different FP methods and the percentage who had multiple separate periods of use by method, showing the figures in total and by OCP use category. In total, 71% of study participants who had ever used FP methods (or 46.3% of all women in the study) tried more than one (maximum four) method. Use of multiple methods over their reproductive lifetime was highest among former OCP users and lowest among OCP never‐users (P < 0.001).
Table 2.
Proportion of women who tried different family planning methods and the percentage of multiplicity of use by methods amongst study groups
| FP methods and multiplicity of use | Respondent groups | OCP never users % (n = 36) | Total % for all groups (n = 121) | |
|---|---|---|---|---|
| Current OCP users % (n = 44) | Former OCP users % (n = 41) | |||
| Used OCP | 100 | 100 | 0 | 70 |
| Used OCP more than once | 73 | 44 | 0 | 41 |
| Used condoms | 21 | 39 | 6 | 22 |
| Used condoms more than once | 9 | 10 | 3 | 7 |
| Used injectables | 18 | 24 | 6 | 17 |
| Used injectables more than once | 2 | 10 | 3 | 5 |
| Used Norplant | 0 | 7 | 3 | 3 |
| Used Norplant more than once | 0 | 0 | 0 | 0 |
| Used IUD | 9 | 15 | 8 | 10 |
| Used IUD more than once | 2 | 2 | 0 | 2 |
| Used traditional methods | 9 | 15 | 3 | 9 |
| Used traditional methods more than once | 5 | 7 | 0 | 4 |
| Used other methods | 0 | 7 | 22 | 9 |
| Used other methods more than once | 0 | 0 | 0 | 0 |
Dynamics of OCP Use
Seventy percent of the study sample had at one time or another used OCP as a method of family planning and 61% used OCP as their first method. For these first‐time OCP users, 28% indicated that they chose OCP because it was easy or convenient to use, 11% mentioned that it was reversible, 9.5% mentioned that it was delivered to the home and 9.5% that it was believed to have fewer side‐effects than other methods. The largest influence on the choice of OCP as the FP method for first‐time users, however, came from family, friends or neighbors with only 11% mentioning the influence of health workers.
Half of the current OCP users were using government supplied OCP (named ‘Shukhi’), others were using pills bought from shops or pharmacies (Social Marketing Company [SMC] or other brand pills). This is a slightly lower proportion of Shukhi users than the national average. A higher than expected proportion of our sample indicated that they collected their current FP method from a pharmacy or shop (26.6%), which is consistent with the high use of SMC and private brand pills noted above.
Among OCP current users and ever‐users, 40% said they had not experienced side‐effects from taking the pill. Of those who experienced side‐effects, the common side‐effects were dizziness (50.6%), nausea (24.1%), blurring of vision (12%) and weakness (10.8%). There were clear differences in side‐effect experience between current users and former users (see Fig. 2). Current users were more likely to have fewer side‐effects complaints than women who no longer used OCP.
Figure 2.
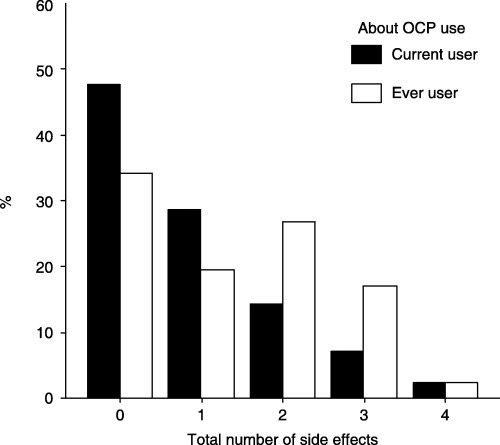
Percentage of respondents experiencing multiple side‐effects by use group.
Another dynamic of OCP use was the pill users taking a ‘short break’. Among ever‐users of OCP, more than one‐fifth (22%) indicated that they had at one stage or another taken one or more short breaks from OCP use.
Women were asked to indicate who made decisions about family planning use (starting, method choice, stopping). A large majority of decisions about OCP use were made jointly between husband and wife. Only on decisions about taking a short break from OCP use were women as likely to make their own decision independent of their husbands.
Women were also asked whom they turned to for advice about family planning and OCP issues, including who advised them on side‐effects or on contraindications to OCP use. Table 3 summarizes findings on advice questions. For general family planning advice, including advice about which method to take, women tended to consult female relatives, friends or neighbors most often. This was particularly true for women just starting family planning use. Government FP workers were supposed to recommend a particular method, explain methods and their use, and give advice on what to do for missed pills, but they were not the most common source of advice in the study area, and women still consulted ‘others’ more frequently. For instance, women in the present study were as likely to consult their husbands on what to do about side‐effects and nearly twice more likely to consult female friends and relatives than to consult any FP workers (government or non‐government organization).
Table 3.
Sources of family planning information and advice
| Information Sources | Husband (%) | Female friend/ relative (%) | GOB FP worker (%) | NGO health worker (%) | Doctor (%) | Printed material/ leaflet (%) | Other (%) | Not applicable (%) |
|---|---|---|---|---|---|---|---|---|
| About FP methods | 13 | 41 | 16 | 3 | 2 | 8 | 17 | |
| Recommending first method | 14 | 27 | 17 | 3 | 3 | 20 | 17 | |
| Advice on first method | 3 | 8 | 7 | 2 | 3 | 2 | 1 | 74 |
| Advice before using current methods | 2 | 3 | 7 | 2 | 3 | 2 | 7 | 84 |
| Advice on missed pill | 5 | 22 | 12 | 4 | 1 | 4 | 7 | 46 |
| With whom discussed about side‐effects | 7 | 13 | 5 | 3 | 1 | 1 | 3 | 69 |
| About contraindications | 2 | 1 | 4 | 3 | 1 | 90 |
FP, family planning; GOB, Government of Bangladesh; NGO, non‐government organization.
The interviews explored women's actual practice of OCP use. Thirty‐seven percent of current and ever‐users said they ‘always’ took their birth control pills everyday and 58% said they ‘usually’ did. For taking the pill at the same time each day, as recommended by the providers, 40% said they ‘always’ took the pill at the same time and 54% indicated they ‘usually’ did. 62% of respondents indicated that they had, at one time or another, missed taking a daily pill, 55% said that this happened roughly once in 3 months and nearly 20% of women said they forgot a pill usually every month.
On the basis of responses, a 10‐point ‘correct use’ scale was derived on the basis of some popular methods to measure judgments, such as, Likert Scale, Guttman Scalogram and Rosenberg Self‐Esteem Scale. 34 The responses elicited were ordinal; they had an inherent order or sequence and were coded between 0 (zero) and 10 (ten). Women who ‘always’ took pills everyday and at the same time, and said they never forgot a pill scored a maximum of 10 points. Women who only ‘sometimes’ took pills everyday and at the same time, and indicated they forgot pills as frequently as once a month, scored a minimum of 2 points. Those who missed pills more than once a month were given 0 (zero). Thirty‐seven percent of respondents scored full 10 (ten) points, whereas the low score of 2 was registered by 3.6%. The mean score was 6.9 and the median 6.0. Mean scores were slightly higher among current users (7.21) than among those who had stopped taking OCP (6.54). The distribution of scores according to each group is shown in Figure 3.
Figure 3.
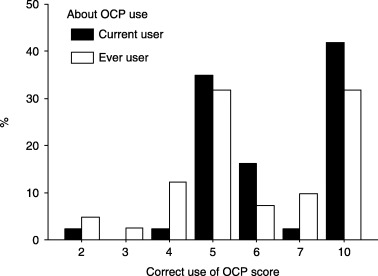
Correct use scores of oral contraceptive pill.
We tested for a possible relationship between higher correct use scores and accessing trained advice about FP use, source of method (expecting that those who collected contraceptives from trained sources might have more consistent correct use patterns), total number of side‐effects experienced and whether the decision to use family planning was made jointly with husbands, as well as for an inverse relationship with method failure. Two significant relationships were found. The first was between correct use and total number of side‐effects reported, where mean correct use scores were higher for women experiencing fewer side‐effects (P = 0.05). Interestingly, the relationship was not completely linear. The highest mean correct use scores were among women with no side‐effects, then with only one. Two and three side‐effects had roughly the same mean use score, but both were lower than for women with four side‐effects. Note that the cause and effect relationship is difficult to ascertain, as women with better patterns of use might experience fewer side‐effects, in part because they take pills correctly. Also, women with fewer side‐effects might find it easier to take pills correctly because they are not experiencing problems with taking them. The second noticeable relationship was between correct use scores and method failure, where women who had reported that they became pregnant while using OCP (n = 6) had lower mean correct use scores (4.7) than those who had not (7.0).
Reasons for discontinuation and taking a ‘short break’ from OCP use
Although 40% of the users did not experience any side‐effects while using OCP, women who discontinued OCP mentioned the experience of side‐effects as one of three major reasons for discontinuation. The other two factors were ‘trying to get pregnant’ and ‘fear of sterility’. A few of them also mentioned husband's or in‐laws’ disapproval including husband's dissatisfaction. It was observed that women who no longer used OCP were much more likely to have complained of multiple side‐effects.
The lack of consultation with trained FP workers about side‐effects and medical problems was another determinant of OCP discontinuation. From the FGD, it appeared that consultation with untrained sources failed to provide adequate explanations of side‐effects and were more likely to lead women to stop taking OCP when side‐effects occurred, without ensuring other forms of pregnancy protection. Trained workers could counsel women to give their bodies time to adjust to OCP use and only switch or stop if side‐effects did not disappear after continued use. The minimum period of first use of OCP among women who experienced side‐effects but did not consult a trained worker was under 1 month, whereas for women who had consulted a trained worker, the minimum period of use was 12 months. For example, one woman who had taken OCP for only one day and had felt dizzy the next day when out in the sun was advised by family to stop taking the pills right away. More than 8% of women used OCP for less than one month when they first started and an additional 13% used pills for about 2 months, and we found that the advice from local untrained contacts was one reason why they stopped. Other reasons also came into play, such as a woman finding out that she was already pregnant when she started OCP. Infrequent visits from FP field workers (3 months supply are commonly provided at one time) have made OCP less accessible for women in their village and have increased the reliance on family members and friends as a source of advice.
Providers’ poor knowledge and lack of counseling were another area of concern. For instance, only 38% of Family Welfare Assistants interviewed indicated that they would describe the range of different methods and their side‐effects if a client came to them. Thirty‐seven percent mentioned that they would explain how to take OCP and only 29% specified that they would provide information on possible side‐effects during the initial consultation. This was consistent with information from FGD where women noted that usually a FP field worker would only discuss side‐effects with them after they had a complaint. When asked about possible harmful effects of OCP, 43% said they believed that OCP might be harmful if taken consecutively for 3–5 years and one third agreed that long‐term use of OCP could cause sterility.
Figure 4 indicates the reasons reported for taking a ‘short break’ among the women of the study area. Although nearly half of them took a break because of side‐effects, interestingly, 16% took a break as a result of fears of health problems that were related to folk stories and misconceptions. Another 16% of women took a break because of inconvenience in terms of access, in‐house storage and intake of pills. Six percent of them took a short break as advised by others, most of whom were untrained sources, for example, friends, relatives and neighbors.
Figure 4.
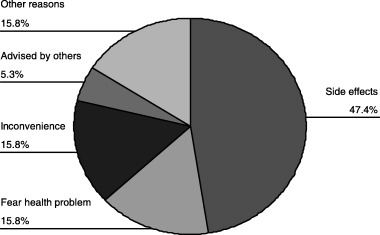
Reasons for taking a ‘short break’.
With closer examination, we did not find any significant correlation between taking a short break and age, level of education or household construction. There was an association between taking a short break and experience of side‐effects, with the average number of side‐effects reported being higher among women who had taken a short break and increasing again for those who had taken more than one short break (P = 0.05).
One of the interesting issues explored through both the questionnaire and FGD was women's attitudes towards certain stories or rumors about OCP use and its negative effects. These stories related either to OCP use causing sterility or other health problems or disease, or both. Examples of these beliefs and rumors include the following:
-
•
Pill will not dissolve in the stomach and will remain there as it is
-
•
Pills join together to form a mala or chora (these are local Bangla words meaning necklace) of snakes, scorpions or snails inside the stomach
-
•
Pills combine and harden to cause a stone in the stomach or uterus
At one FGD with women who had discontinued OCP, a participant volunteered her own experience, ‘I had a problem when I used oral pills for five years, my lower abdomen became hard. I went to a clinic and the doctor told me that this is because of oral pills’. Another respondent said, ‘If you don't use “expensive” oral pills, oil [fat] will store in the stomach and the door [for further children] may become closed’. Husbands were also aware of those stories. In another FGD, one man mentioned that he had heard that after a woman had an operation for a tumor, the doctor found 15 000–16 000 pills in her abdomen.
We were interested to see if knowledge of these stories affected women's behavior. Among ever‐users (current users and discontinuers), 54% said that they did not believe the stories or they did not affect their behavior. Twelve percent said they stopped taking OCP or took a short break. A few women reported that they started to chew pills or break them apart and other women started to take the pills with a large amount of water every night to ensure they would dissolve better (4.7% together).
We felt it was possible that immediately after discussing ‘folk stories’, women might be disinclined to admit to being influenced by them. Over the interview, we had asked several other open‐ended questions about why a woman had stopped using her first method of FP or had stopped OCP at different times (including taking a short break), as well as enquiring about her main reasons for stopping OCP and her feelings about what the main disadvantages of OCP were. In each of these other questions, some women's concerns about folk beliefs came through in the responses, and were coded either as fear of sterility or as fear of other health problems or disease from continuous use (where this appeared to be separate from side‐effects), depending on what was said. Fear of sterility from continuous OCP use came through as a strong theme. Table 4 summarizes the findings of the questions related to stopping OCP use.
Table 4.
Fears related to stopping oral contraceptive pill use
| Stated Reasons | Current users (n = 44) % | Discontinuers (n = 41) % | Never users (n = 36) % | Total (n = 121) % |
|---|---|---|---|---|
| Fear of sterility as reason | ||||
| To stop first method | 5 | 10 | – | 5 |
| To discontinue, take short break, or never using | 5 | 22 | 8 | 12 |
| To stop OCP (or belief as to why other women stop for never users) | 2 | 20 | 6 | 9 |
| As main disadvantage of OCP use | 5 | 20 | 6 | 10 |
| Fear of health problems as reason | ||||
| To stop first method | – | – | – | 0 |
| To discontinue, take short break or never using | – | 7 | 6 | 4 |
| To stop OCP (or belief as to why other women stop for never users) | 2 | 7 | 11 | 7 |
| As main disadvantage of OCP use | 2 | 17 | 6 | 8 |
OCP, oral contraceptive pill.
Fear of sterility and health effects was particularly noticeable among women in the former users group and appeared to play a large role in their decision to stop using OCP.
Besides these directly traceable relationships, we know folk stories also come into play in the information and advice provided to women by relatives, neighbors and others. All of the never‐users who knew of folk stories said they had heard of these from female relatives, friends and neighbors, as did 90% of ever users. However, from the present study, it was not possible to quantify the degree to which folk beliefs are a factor in advice given to women, particularly about stopping or switching from OCP.
For never‐users of OCP, Table 5 lists reasons women offered when asked why they had never tried this method. The seven women in the study who did not have children were among those who reported never using FP or OCP. Among ‘other reasons’ was current use of another FP method: eight never‐users of OCP had chosen a permanent method, two were using IUD, another two were using condoms, one each was using injectables, Norplant, and traditional methods.
Table 5.
Reasons for non‐use of oral contraceptive pill
| Reasons | Times mentioned | % Never‐users mentioned |
|---|---|---|
| Married recently | 1 | 3 |
| Trying to get pregnant | 17 | 47 |
| Heard about side‐effects | 4 | 11 |
| Fear of sterility | 3 | 8 |
| Fear of health problems/disease | 2 | 6 |
| Husband doe not approve | 4 | 11 |
| In‐laws do not approve | 2 | 6 |
| Insufficient knowledge about OCP | 7 | 19 |
| Other reasons mentioned | 4 | 11 |
OCP, oral contraceptive pill.
DISCUSSION
THE PRESENT STUDY involved a relatively small sample and was never intended to be representative of FP users in Bangladesh. However, this was a qualitative study to explore in‐depth OCP use dynamics and factors associated with its discontinuation among rural women. The findings are broadly consistent with previous studies on this issue and reaffirm the importance of improving the quality of FP services. Some of the findings, however, present completely new information, which is not available in DHS, or similar surveys. There are three such areas where the present study has provided compelling evidence and interesting insights, which would be worth exploring further in more detail, particularly to assess their potential contribution to the national level of OCP discontinuation and concerns surrounding TFR stagnation. Our discussion should therefore focus on these newly emerging issues, such as the incidence of ineffective use of OCP, the influence of folk stories on OCP behavior and the need to update service providers’ skills and knowledge.
Ineffective use of OCP
One interesting finding from the present study was about women's reported practice of taking OCP and the incidence of short breaks among OCP users. Many women do not take pills regularly. Looking at the correct use score calculated on the basis of responses to questions about the regularity and timing of OCP use and the frequency of missed pills, about half of the women were assigned scores beneath the median of 6.0 (minimum 2 and maximum 10). Some ever‐user women had scores low enough (4 or lower) to question the efficacy of their OCP use, which would expose them to the risk of unwanted pregnancy.
Nearly one quarter of ever‐users of OCP in our sample had at one or more times taken a short break from OCP use, where they were not being covered by another method, did not want to get pregnant and were intending to return to pill use in a few weeks or months. The most common reason mentioned for taking a short break was the experience of side‐effects, however, from other questions it is clear that issues raised by folk stories, in particular fear of sterility from continuous OCP use, were also affecting behavior. One key informant reported that she had taken a short break after using OCP for more than 4 years, even though she experienced no side‐effects and felt that taking OCP had contributed to her better health. She noted, ‘others say if you are taking pills for 4–5 years you won't get pregnant again. I have listened to this advice and decided to take a short break’. She also noted that her relatives had strongly influenced her to make this decision and that she did not use another FP method during the break, even though there was ‘no plan to give birth’. Despite both her own and her husband's high educational level, these stories influenced her to take action that could have had unwanted consequences (an unplanned pregnancy with its allied health risks).
Influence of folk stories
Another most interesting finding raised from the present study was the influence of folk stories or misconceptions about OCP use. Although the numbers were small and the survey sample is not representative, nevertheless, women had linked their own behavior to concerns that continued use of OCP would cause sterility in the long‐term. Taking short breaks most likely relates back to the first generation of OCP, where doctors and FP workers often recommended not taking pills continuously for more than 3–5 years without giving the body a ‘break’ from the high dose of hormones, which could be related to high blood pressure or other health risks. The break was meant to be long enough for a woman to regain her ‘normal’ cycle. From this pattern, a belief emerged that no OCP should be taken for more than 3–5 years, despite the fact that low‐dose pills do not have the same risks and that the practice of breaks is no longer medically recommended. This concern continues despite the very limited current use of high‐dose OCP in Bangladesh and despite huge communication campaigns undertaken a decade ago during the introduction of the low‐dose contraceptive into Bangladesh.
The role of folk stories in OCP discontinuation has not been widely studied. In the standard DHS framework, women indicating fear of sterility or fear of disease related to folk stories, as reasons for OCP discontinuation would probably be aggregated under ‘health concerns’ or ‘other’ reasons. Health concerns accounted for 7.5 of all OCP discontinuation in the past 5 years, according to the 1999–2000 DHS, whereas ‘other’ accounted for an additional 6.2%. Further exploration of the influence of folk stories among women in different parts of the country could be valuable, with a view towards designing information campaigns, which could reduce their impact. There is also a clear need to address the issue of folk stories in training for service providers, particularly those working at the community and union level, both because some of these providers themselves still hold these beliefs and because they need to know how to counsel women and their partners to reduce their fears and increase their comfort levels.
Concern over sterility is strongly interlinked with religion in the study area. In the FGD, various methods were raised as being problematic because they interfered too dramatically with fertility and as a result would be seen as wrongful acts under Islam. One discontinuer noted in a FGD that religious leaders say, ‘God gives food because he creates our children. If you take OCP, your stomach may fry, it is a sin to take OCP’. Although participants in key informants FGD said, ‘Religious leaders do not tell us anything [against OCP use] because they are also using [them]’. There is still a general discomfort in rural areas about whether FP use is really consistent with Islamic practice. But in the present study, one mullah (religious leader) mentioned that his wife was using OCP but he did not want anyone else in the village to know. Many women in the FGD mentioned that they did not use longer‐acting methods as this would displease Allah even more than using OCP; ‘Allah becomes dissatisfied with anyone who does the operation [sterilization]’. There is little doubt that women, who have inferior status because of their gender within their families as well as in the society, feel they must be careful not to displease Allah through their actions, which could have repercussions for them or other family members.
Together these two points deserve further exploration through a wider, more formal study, in that if significant numbers of OCP users around the country have similar patterns of ineffective use they call into question the link between CPR increase and TFR decrease.
Service provider beliefs and skills
The final analytical point that can be drawn from the present study is that service providers at all levels need periodic updating of knowledge and skills to ensure they are not providing outdated or inaccurate information that could create health risks for their clients and lead to underachievement of the FP program.
In the present study, almost half of the service providers said they believed that OCP should not be taken continuously for more than 5 years and one third agreed that long‐term use of OCP could cause sterility. These beliefs were not limited to lower‐level service providers, though they were slightly more common at the lowest level. Even the medical doctors in the present study felt that continued OCP use (in the absence of side‐effects or other problems) should not be recommended. For most providers at various levels, access to in‐service training after they are in their position is very limited. The average length of service in their professional designation for the service providers in the present study was roughly 20 years. Over this period, much has changed in regard to FP technology and products, knowledge of quality of care, and health promotion methodologies. It should not be surprising that medical and paramedical staff continue to hold onto outdated assumptions about first generation OCP, despite the introduction of third‐generation pills, if there is little or no access to retraining and professional development.
To the best of our knowledge, the issue of folk stories and how to address these fears with clients is not a topic that is being covered as part of the basic or refresher training of FP workers, nor is there much in the way of specific promotional media campaigns designed to address these concerns in the general population. Yet, reducing the influence of folk beliefs could have a positive influence on lowering rates of discontinuation of oral contraceptives, with significant associated health benefits for clients and faster progress towards achieving the policy goal of replacement‐level fertility for the Government of Bangladesh.
ACKNOWLEDGMENTS
THE PRESENT STUDY was funded by the Canadian International Development Agency (CIDA) through its Bangladesh Health and Population Reform Program (BHPRP). The opinions expressed herein are those of the authors and do not reflect the view of CIDA.
REFERENCES
- 1. Abedin MN. Health and Population Sector: An Overview and Vision. Paper for the Logical Framework (Log‐Frame) Workshop for the Fifth Health and Population Program (HAPP‐5) 23‐25 February 1997. Dhaka: Government of Bangladesh. [Google Scholar]
- 2. ESCAP . 1999 ESCAP Population Data Sheet. Bangkok: United Nations. [Google Scholar]
- 3. BBS. Statistical Handbook 2000 Bangladesh Bureau of Statistics (BBS). Dhaka: Government of Bangladesh. [Google Scholar]
- 4. Ullah MS, Chakraborty N. Factors affecting the use of contraception in Bangladesh: A multivariate analysis. Asia-Pacific Population J 1993; 8: 19–30. [PubMed] [Google Scholar]
- 5. Khan MA, Rahman M. Determinants of contraceptive method choice in rural Bangladesh. Asia-Pacific Population J 1997; 12: 65–82. [Google Scholar]
- 6. Islam MM, Al‐Mamun A, Bairagi R. Fertility and its proximate determinants in Bangladesh: Evidence from 1993/94 Demographic and Health Survey. Asia-Pacific Population J 1998; 13: 3–22. [PubMed] [Google Scholar]
- 7. Perry HB. Reaching ‘Health for All’ in Bangladesh: Lessons in primary health care for the twenty‐first century. Dhaka: University Press Ltd, 1999. [Google Scholar]
- 8. UNICEF. Country Experiences: Bangladesh (Part Two). 1999; 219–291.
- 9. The World Bank. Project Appraisal Document for Health and Population Program Project. Dhaka: The World Bank, 1998. [Google Scholar]
- 10. Khuda B, Roy NC, Rahman DMM. Family planning and fertility in Bangladesh. Asia-Pacific Population J 2000; 15: 41–54. [PubMed] [Google Scholar]
- 11. DHS. Bangladesh Demographic and Health Survey (DHS) 2000. Dhaka: Mitra and Associates and; Maryland USA: Macro International Inc, 2000. [Google Scholar]
- 12. Khan MA. Side effects and oral contraceptive discontinuation in rural Bangladesh. Contraception 2001; 64: 161–167. [DOI] [PubMed] [Google Scholar]
- 13. MOHFW. Health and Population Sector Programs: Program Implementation Plan (PIP) 1998–2003. Dhaka: Ministry of Health and Family Welfare (MOHFW), 1998. [Google Scholar]
- 14. DHS. Bangladesh Demographic and Health Survey (DHS) 1996–97. Dhaka: Mitra and Associates and; Maryland USA: Macro International Inc. [Google Scholar]
- 15. Islam A, Islam M, Chakraborty N. Plateauing of Fertility Level in Bangladesh: Exploring the Reality A Paper Presented at ‘Dialogue on Exploring Recent Fertility Behavior in Bangladesh’ in 2001. Dhaka: Centre for Policy Dialogue. [Google Scholar]
- 16. Dev SM, James KS, Sen B. Causes of Fertility Decline in India and Bangladesh – A Project Report – 2002. New Delhi: South Asia Network of Economic Research Institute. [Google Scholar]
- 17. Kamal N, Chaudhury RH. Plateauing TFR Bangladesh: An exploratory analysis. Asian Profile 2003; 31: 157–166. [Google Scholar]
- 18. Khan ME, D’Costa SM, Rahman M. Contraceptive use dynamics in Bangladesh: A case study of pills use. A Paper Presented in the 130th Annual Meeting of APHA, 9–13 November 2002. Philadelphia, USA: American Public Health Association (APHA). [Google Scholar]
- 19. Cotten N, Stanback J, Maidouka H, Taylor‐Thomas JT, Turk T. Early discontinuation of contraceptive use in Niger and Gambia. Int Family Planning Perspectives 1992; 18: 145–149. [Google Scholar]
- 20. Rosenberg M, Burnhill MS, Waugh MS, Grimes DA, Hillard PJA. Compliance and oral contraceptives: A review. Contraception 1995; 52: 137–141. [DOI] [PubMed] [Google Scholar]
- 21. Mannan HR. Factors in contraceptive method choice in Bangladesh: Goals, competence, evaluation and access. Contraception 2002; 65: 357–364. [DOI] [PubMed] [Google Scholar]
- 22. CIET Canada . Service Delivery Surveys 2000 – Health and Population Sector Program in Bangladesh. Dhaka: Ministry of Health and Family Welfare (MOHFW). [Google Scholar]
- 23. Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective study of the effects of oral contraceptives on sexuality and well‐being and their relationship to discontinuation. Contraception 2001; 64: 51–58. [DOI] [PubMed] [Google Scholar]
- 24. Ali M, Cleland J. Contraceptive discontinuation in six developing countries: A cause‐specific analysis. Int Family Planning Perspectives 1995; 21: 92–97. [Google Scholar]
- 25. Ali M, Cleland J. Determinants of contraceptive discontinuation in six developing countries. J Biosocial Sci 1999; 31: 343–360. [DOI] [PubMed] [Google Scholar]
- 26. Colli E, Tong D, Penhallegon R, Parazzini F. Reasons for contraceptive discontinuation in women 20–39 years old in New Zeland. Contraception 1999; 59: 227–231. [DOI] [PubMed] [Google Scholar]
- 27. Ross J, Hardee K, Mumford E, Eid S. Contraceptive method choice in developing countries. Int Family Planning Perspectives 2001; 28: 32–40. [Google Scholar]
- 28. RamaRao S, Laquesta M, Costello M, Pangolibay B, Jones H. The link between quality of care and contraceptive use. Int Family Planning Perspectives 2003; 29: 76–83. [DOI] [PubMed] [Google Scholar]
- 29. Pariani S, Heer DM, Van Arsdo MD Jr. Does choice make a difference to contraception use? Evidence form East Java. Studies Family Planning 1991; 22: 384–390. [PubMed] [Google Scholar]
- 30. Kamal N, Sloggett A. The effect of female family planning workers on the use of modern contraception in Bangladesh. Asia-Pacific Population J 1996; 11: 15–26. [PubMed] [Google Scholar]
- 31. Janowitz B, Holtman M, Johnson L, Trottier D. The importance of field workers in Bangladesh's family planning program. Asia-Pacific Population J 1999; 14: 23–36. [PubMed] [Google Scholar]
- 32. Koenig MA. The Impact of Quality of Care on Contraceptive Use: Evidence from Longitudinal Data from Rural Bangladesh. Baltimore: The John Hopkins University, 2003. [Google Scholar]
- 33. Rosenberg M, Waugh MS, Meehan TE. Use and Misuse of Oral Contraceptives: Risk Indicators for Poor Pill Taking and Discontinuation. Contraception 1995; 51: 283–288. [DOI] [PubMed] [Google Scholar]
- 34. Bailey KD. Methods of Social Research, 4th edn New York: The Free Press (A Division of Macmillan, Inc.), 1994. [Google Scholar]


