Abstract
Infections of the orbit and periorbita are relatively frequent, and can cause significant local and systemic morbidity. Loss of vision occurs in more than 10% of patients, and systemic sequelae can include meningitis, intracranial abscess, and death. Numerous organisms infect the orbit, but the most common are bacteria. There are many methods through which orbital infections occur, with infection from the neighboring ethmoid sinuses the most likely cause for all age groups. Prompt management is essential in suspected orbital cellulitis, and involves urgent intravenous antibiotics, rehydration, and treatment of any co-existent underlying systemic disease, e.g., diabetes, renal failure. This review summarizes the common infectious processes of the orbit in both pediatric and adult groups. We review pathophysiology, symptoms, signs, and treatment for infectious orbital processes.
Keywords: Bacterial Orbital Infections, Common Orbital Infections, Orbital Infections
INTRODUCTION
Infections of the orbit and periorbita are relatively frequent and can lead to significant local and systemic morbidity. Loss of vision occurs in more than 10% of patients [Table 1], and possible systemic sequelae include meningitis, intracranial abscess, and death [Table 2].[1,2] As such, in patients with suspected orbital infection, while a reliable history and examination are important, prompt treatment is essential, as it may be both sight- and life-saving.
Table 1.
Reasons for visual loss in orbital infections
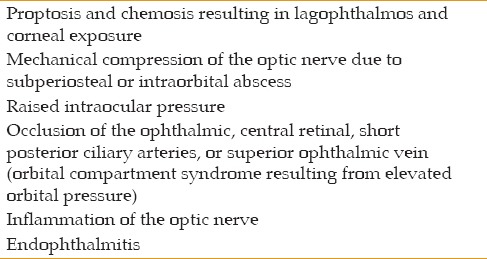
Table 2.
Systemic complications of orbital infection
Numerous organisms infect the orbit, including bacteria, viruses, fungi, and parasites; the etiologies of these infections are given in Table 3. Predisposing factors include a history of immunosuppression including diabetes, sinus or dental disease, recent facial trauma [Figure 1], and patients with systemic disease.
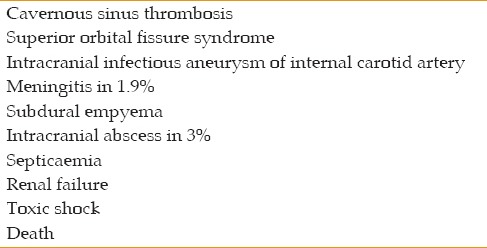
Table 3.
Orbital infections: Aetiology
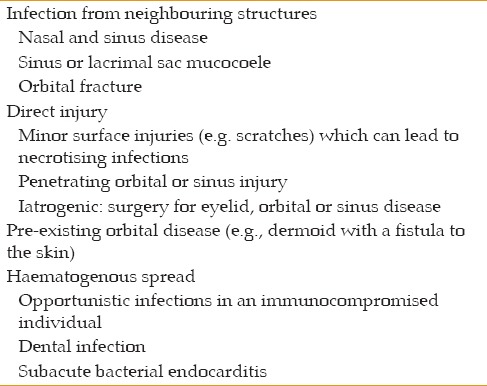
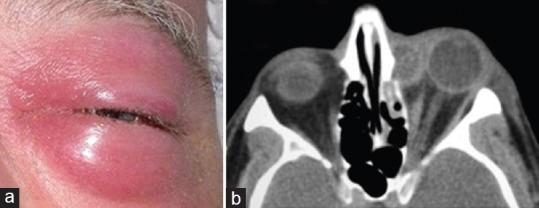
Figure 1.
(a) Injury of the orbit from penetration by a pencil. Clinical features include proptosis, chemosis, and loss of vision due to raised intraorbital pressure. (b) CT scan identifies gas within the orbit, which together with the soft tissue swelling, accounts for the rise in orbital pressure.
Bacterial Orbital Infections
Key points
In all age groups, the most common infectious organisms are bacteria; these are frequently staphylococci and streptococci
At any age, infection from the neighboring ethmoid sinuses is the most likely cause [Figure 2]
Extension of infection from the sinuses to the orbit is thought to result from septic thrombophlebitis of the valveless veins that are between the two structures
The septum is a natural barrier to the passage of microorganisms, with infections described as pre-septal (periorbital) and post-septal (orbital)
Five “stages” of post-septal infection have been described (Chandler's classification), each with increasing risk of sight loss and systemic morbidity*: (1) inflammatory edema, (2) orbital cellulitis, (3) subperiosteal abscess, (4) orbital abscess, (5) cavernous sinus thrombosis
Prompt management is essential in suspected orbital cellulitis, and involves urgent intravenous (IV) antibiotics, rehydration, and treatment of any co-existent underlying systemic disease, e.g., diabetes, renal failure
If a patient fails to respond to appropriate measures for any presumed infection, the diagnosis should be reconsidered.
Figure 2.
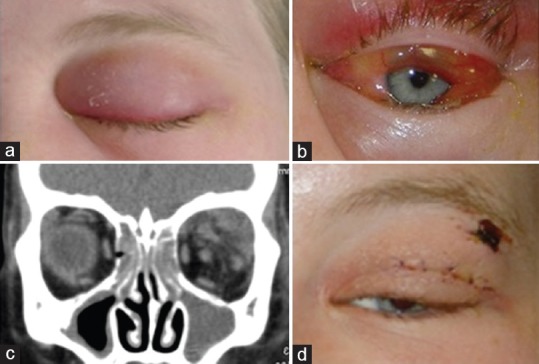
(a and b) A ten-year-old female presented with a short history of orbital ache, chemosis, and reduced eye movements. (c) CT imaging identifies a collection in the superotemporal quadrant of the orbit, as well as ethmoid and maxillary sinusitis. (d) Drainage of the orbital collection via skin crease approach precipitated rapid recovery.
Orbital Infections – Origins
Bacteria can reach the orbit by implantation, local extension, or hematogenous spread. The paper-thin bone of the lamina papyracea and the valveless veins of the midface and orbit predispose this area to infection. Implantation results from trauma to the periorbital area or sinuses.[3,4,5,6] Local extension occurs through spread from contiguous sinusitis. Hematogenous spread occurs from a multiplicity of distant sites, and most often in a debilitated patient. Trauma, nasolacrimal, and odontogenic infections are also important factors that should be considered when locating the source of an orbital infection.
Orbital Infections in Children
Overview
Among children younger than 5 years of age, pre-septal cellulitis is more prevalent than post-septal infection, with ethmoid sinusitis being the most common underlying cause.[3] A wide spectrum of pathogenic organisms is recognized as being associated with these conditions, although, haemophilusinfections are less likely following H. influenzae type b vaccination.[7,8] Surgical intervention, either to drain an infected sinus or a subperiosteal abscess, should be undertaken where there is clinical deterioration, or an inadequate response to antibiotics (vide infra).
Clinical Features, Diagnosis, and Investigations
The average age for orbital infection in both boys and girls is 7 years, although, for reasons unknown, it is almost twice as common in boys.[9] This finding is in accordance with the trend of more serious childhood infections occurring in males. Presenting clinical features include pain, heat, redness, and swelling in the periorbital region. Any history of fever, sinusitis, upper respiratory tract infection and trauma should be ascertained. In pre-septal infection, there is lid edema and redness, but ocular examination is otherwise normal (Chandler stage 1). Early post-septal clinical features may be quite subtle, and include an inflammation demarcation line (which corresponds to the arcus marginalis; Figure 3), chemosis, proptosis, reduced eye movements, and loss of vision.[10] In more severe cases, particularly if there is visual loss, there must be consideration of orbital apex syndrome and cavernous sinus thrombosis. In the most severe cases, signs of meningitis indicate intracranial spread of an orbital infection. It is important to emphasize that examination is crucial in differentiating pre- and post-septal infections. Chemosis, proptosis, restriction of extraocular movements, positive relative afferent pupillary defect and visual loss are all indicative of post-septal infections.
Figure 3.
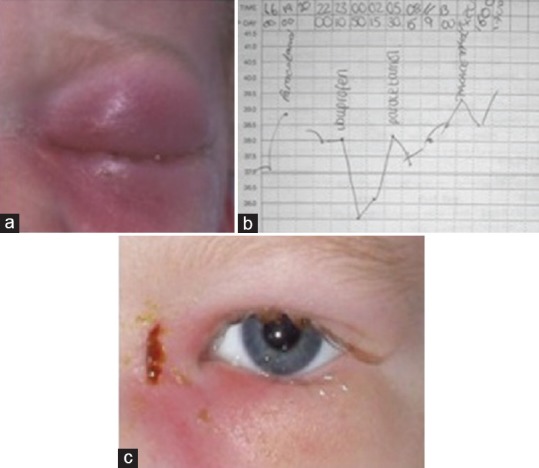
(a) A four-year-old boy presented with periorbital swelling and an upper respiratory tract infection. (b) His general condition deteriorated over the following 36 hours and he developed spiking pyrexia. (c) Rapid recovery followed drainage of the medial orbital collection via a Lynch-Howarth incision.
A reliable history and examination are of the utmost importance in reaching the correct diagnosis. Investigations, such as hematology, microbiology, and orbital ultrasonography are frequently non-contributory and delay the initiation of treatment.[11] Although contrast-enhanced computed tomography will identify sinus disease and the presence of a subperiosteal or orbital abscess, this too should not delay treatment of a suspected orbital infection. Magnetic resonance imaging (MRI), the secondary choice in orbital imaging, is valuable when cavernous sinus, intracranial extension, or radiolucent foreign bodies are suspected; lumbar puncture is reserved for children with features of meningitis.[12]
Bacteriology in Pediatric Infections
The most commonly isolated organisms in children with post-septal infection are α- or non-hemolytic streptococci, group A β-hemolytic streptococci, Staphylococcus aureus and Haemophilus influenzae.[9] Among those requiring drainage, positive cultures from abscess or sinus drainage specimens may be expected in two-thirds and polymicrobial infections occur in over a third. A variety of other aerobic organisms may be implicated in orbital infections, including group C β-hemolytic streptococci, Eikenella corrodens, Arcanobacterium haemolyticum, and Moraxella catarrhalis. Anaerobes are encountered less frequently than aerobes, but carry a higher morbidity than aerobic organisms; these include Peptostreptococcus, Bacteroides sp., and Fusobacterium necrophorum.[13]
The Management of Pediatric Orbital Cellulitis
Medical treatment
Active and early involvement of the oculoplastic surgeons, ophthalmologists, pediatricians and otorhinolaryngologists is essential in managing children with orbital cellulitis. Outpatient management with oral antibiotics and daily review is appropriate for those individuals with only mild pre-septal disease, and who are otherwise well. In all other cases, the patient should be admitted for IV antibiotics, with systemic and visual functioning monitored and recorded at least thrice daily, depending on the severity of the clinical signs.
Although sinusitis might be managed with appropriate antibiotics, where a child fails to respond to IV antibiotics, or deteriorates despite treatment, endoscopic sinus drainage should be performed. In one study by Nageswaran et al, 12 of 41 children (29%) responded to antibiotics alone. The remainder required surgical drainage, of which the majority also required ethmoidectomy.[9]
Since empirical treatment should cover pathogens associated with acute sinusitis (S. pneumoniae, H. influenzae, M. catarrhalis, S. pyogenes) in addition to S. aureus and anaerobes, the current first-line IV antibiotic is ampicillin. Where community-acquired methicillin-resistant S. aureus is prevalent, the advice of a microbiologist should be sought in order to re-evaluate treatment options. Although H. influenzae orbital cellulitis now occurs infrequently, treatment should include a second- or third generation cephalosporin in children younger than 5 years. This particular treatment is recommended because of the risk of meningitis from the organism.[14] There is an argument for the use of adjuvant oral or IV corticosteroids in addition to IV antibiotics as an anti-inflammatory treatment. Recently, Chen et al showed in a prospective comparative study that using IV steroids with IV antibiotics concurrently is safe and reduces the length of the hospital stay.[15]
Surgical Treatment
Previously, any development of a subperiosteal abscess per se required urgent drainage. However, now, medical treatment is deemed sufficient for those with normal visual function, fewer than 9 years of age, medially located abscesses, and no evidence for intracranial or frontal sinus involvement.[16,17] Indications for drainage include progression of the disease despite medical management, decrease in visual acuity, positive relative afferent pupillary defect or ophthalmoplegia, and a large, well-defined abscess.
Rudloe et al[18] presented an algorithm to stratify the risk factors for significant complications in those patients with orbital cellulitis, who presented without classic symptoms or clinical findings. They showed that an absolute neutrophil count of greater than 10,000 cells/ml, moderate to severe periorbital edema, absence of conjunctivitis as the presenting symptom, age of more than 3 years, and previous antibiotic use were all predictors of orbital abscess. An edema extending beyond the eyelid margins was thought to be a strong predictor of surgical intervention by Vu et al[19] Smithet al[20] found that risk factors associated with surgery included, age older than 9 years, proptosis, extraocular motility restriction, and elevated intraocular pressure.
Orbital Infections in Adults
Overview
Orbital infections in adults can have several origins [Table 3]. Sinus disease, typically of the ethmoid air cells, is reported in 60 to 70% of cases [Figures 4 and 5][5,21,22,23] Involvement of the more posterior sphenoid sinus may lead to orbital apex syndrome with early visual loss.[24] Posterior extension of any infectious process intracranially may lead to meningitis, abscess, or cavernous sinus thrombosis; these are particularly severe manifestations of orbital infection. Further important causes of infection include direct trauma to the eye, periocular tissues or bony orbit in which a foreign body might also be present, dental infections, and extension of infection posterior to the orbital septum from dacryocystitis [Figure 6].[21,23,25,26] Immediate management is vital in preventing visual and systemic co-morbidity in orbital infection.
Figure 4.
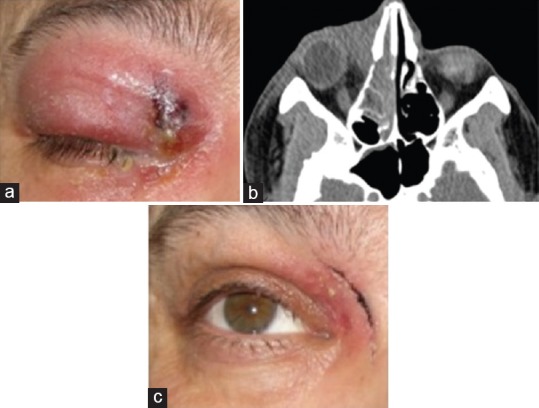
(a) A patient presented with a three-day history of ocular ache, ptosis, and discharge at the medial canthus. (b) CT imaging shows ipsilateral ethmoid sinusitis and a medial orbital collection. (c) Orbital and ethmoid abscesses were drained through a Lynch–Howarth incision.
Figure 5.
(a and b) CT imaging of young male with visual acuity of counting fingers and a left relative afferent pupillary defect. A subperiosteal abscess in the superolateral quadrant of the orbit and ipsilateral frontal, ethmoid and maxillary sinusitis are apparent. (c) CT bone windows confirm loss of the posterior table of the frontal sinus, although no intracranial abscess is present.
Figure 6.
(a) Diabetic 65-year-old male with a history of a left-sided mucocele, presented with pain, ptosis, double vision, and proptosis. (b) Imaging shows a large lacrimal mucocele extending into the orbit, which was then drained.
Bacteriology in Adult Orbital Cellulitis
Gram-positive bacteria, particularly staphylococcus and streptococcus species, are the most common organisms identified in adult orbital cellulitis.[3] In contrast to young children, individuals older than 15 years of age are significantly more likely to harbor polymicrobial infections with both aerobic and anaerobic species. This might reflect differences in sinus anatomy between the two groups; in children, the sinus ostia are relatively large in comparison to the sinus cavities and have higher drainage rates than adults. In adults the converse is true, they have well-developed frontal sinuses that are colonized by polymicrobial and anaerobic organisms. In a mixed microbial environment, a synergistic effect between aerobic and anaerobic organisms might occur. Aerobes reduce tissue oxygen pressure, toxic to anaerobic organisms, and anaerobes produce beta-lactamase, which confers a protective effect for aerobes against some antibiotics. Such synergism might explain the finding that the prognosis for a subperiosteal abscess is better in children younger than 9 years of age, in whom drainage cultures are usually negative.
Clinical Evaluation
Relevant features in the history of any patient with suspected orbital infection include soft tissue or bony injury to the midface, a history of antibiotic or steroid treatment, any otolaryngological past history, and systemic illness that indicates a distant infective cause, including upper respiratory tract infections. It is important to properly investigate and understand differences in preceding factors for children and adults. Sinusitis is the major preceding factor in children, while adults are more likely to have trauma and comorbidities.[27]
An astute clinician will obtain certain, key information regarding the nature of the infection. This includes the position, whether pre- or post-septal, and the severity, ranging between mild inflammatory periorbital edema to an intraorbital abscess or cavernous sinus thrombosis. Both pre- and post-septal disease can present with local inflammatory signs, such as pain, heat, redness and swelling, in addition to fever. Post-septal infections are often associated with a peripheral demarcation line corresponding to the arcus marginalis [Figures 4 and 6]. These infections are likely to cause general malaise, chemosis, reduced eye movement, exophthalmos and, in severe cases, visual loss.
The development of a subperiosteal abscess can occur in two ways, the first is due to direct extension from an infected sinus. The second, more common way is by local hematogenous spread through the valveless veins that cross from the sinuses into the orbit. The penetration of antibiotics into this space is poor, and visual loss can rapidly ensue with the expansion of an abscess.[28] Further to this, infection in the frontal sinus, with a corresponding subperiosteal orbital abscess, carries a worse prognosis due to the risk of intracranial spread. Should an early intracranial abscess be suspected, thin-slice MRI with fat suppression might enable visualization of any intracranial component.[29]
Diagnostic Studies
Ancillary studies, such as a white blood cell counts with differential and microbial cultures, are frequently unhelpful in elucidating either the cause or the extent of an infection. However, thin-slice CT imaging with contrast, the modality of choice in imaging the orbit, is helpful in defining the extent of disease [Figures 4–7] and identifying either a foreign body, with appropriate soft tissue windows, or the presence of a subperiosteal or intraperiosteal abscess.[21,30] The clinician should remember that, occasionally, a hematoma may be misinterpreted as an abscess, and that a surgically-identified abscess might not be evident on CT scanning.[31]
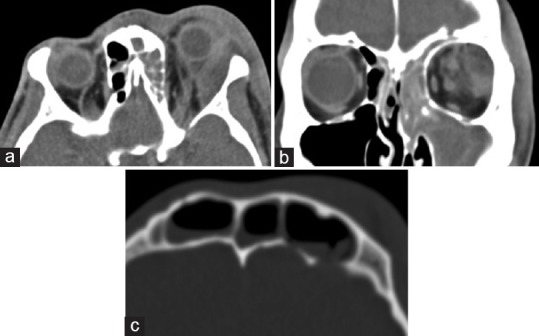
Figure 7.
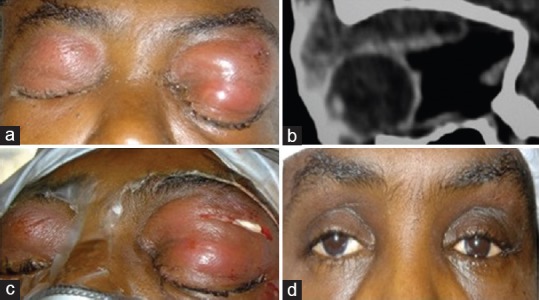
(a) A 32-year-old male with a history of sinusitis presented with bilateral subperiosteal orbital abscesses. (b) The sagittal CT image identified an abscess lying alongside the the orbital roof. (c) These were drained through the upper lid, and corrugated drains were left in situ for 48 hours. (d) Abscess cultures were negative and the patient made an excellent recovery.
Recently, Kang et al[32] reported a role for ocular ultrasound in stratifying the risk to vision for patients with more nonspecific symptoms, such as ocular pain, eyelid swelling, and erythema.
Management of Orbital Infections in Adults
Medical treatment
Patients with mild pre-septal cellulitis, and no evidence of orbital or systemic disease, may be managed as outpatients with oral antibiotics. Those with suspected post-septal infection should immediately commence high-dose, broad-spectrum IV antibiotics. Failure to treat these patients urgently carries a high risk of irreversible vision loss.[11] A combination of parenteral cefuroxime (1.5 g) and metronidazole (500 mg) every eight hours is a reasonable empirical approach until culture results, and the advice of a microbiologist, can be obtained. Where there is a high incidence of community-acquired methicillin-resistant staphylococcus infection, the initial treatment might include vancomycin, cefotaxime, and either metronidazole or clindamycin.[33] In addition, where there is co-existent sinus, ear or oral disease, management should be undertaken in consultation with the appropriate subspecialist. Since the majority of cases are associated with sinus inflammation, a nasal decongestant should also be administered. This can improve drainage of the sinuses and any adjacent subperiosteal intraorbital collection of pus.[34]
Most patients with orbital infections improve with medical measures alone; constitutional symptoms generally respond before the orbital signs, which can deteriorate before improving.[35] This unexpected observation might be due to the large volume of fluid administered with IV antibiotics. This is often in the context of systemic dehydration, and may be reflected in the CT signs, which also lag behind, or even worsen, relative to the clinical response.[26]
Surgical Treatment
The necessity and timing for surgical intervention depend on the patient's history and clinical signs. A subperiosteal abscess that does not respond to antibiotic therapy is one of several indications for drainage [Table 4]. Conversely, a patient with an orbital abscess diagnosed on imaging alone who is responding to oral antibiotics, may be managed medically.[36] Recently, Marchaino et al showed that older patients and males more commonly undergo surgical intervention for orbital cellulitis.[37] The approach for drainage of an orbital collection is determined by the location of the abscess [Table 5]. The periorbita is elevated until the anterior extent of the abscess is reached, and the contents are then released. Microbiological specimens should be obtained, the exposed subperiosteal space washed with saline, and a sutured corrugated drain is left in situ for 2-3 days to permit further drainage.
Table 4.
Subperiosteal abscess: Indications for drainage
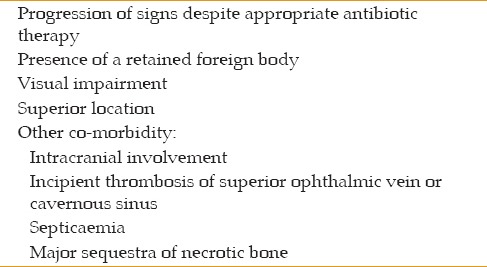
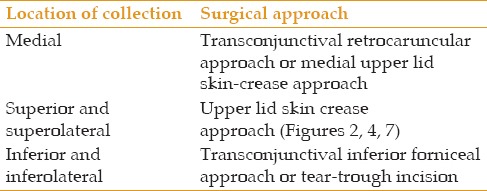
Table 5.
Drainage of an orbital collection: Approaches
The majority of orbital collections are subperiosteal; intraorbital abscesses (Chandler stage 4) are rare and usually result from ocular surgery, penetrating injury, or infected hematogenous emboli. An intraconal abscess frequently leads to significant proptosis with visual deterioration, and does not always respond to medical therapy.
No firm argument exists to support the use of glucocorticoids in orbital infections, since this treatment carries a small but significant risk of deterioration in patients with fungal disease, and in those who are immunosuppressed. Where there is clear clinical improvement on medical treatment, or where the bacterial sensitivities are known, their use may be considered on an individual basis.[38]
Necrotizing Fasciitis
Overview
Necrotizing fasciitis (NF) is an aggressive, rapidly progressive infection that spreads along subcutaneous fascial planes. Typically caused by group A β-hemolytic streptococcus, periocular NF is a true ophthalmic emergency, since early diagnosis and urgent treatment are paramount. Treatment requires high-dose IV penicillin and clindamycin, and debridement of any affected tissues.
Pathophysiology and Management
Features of periorbital NF include pain, violaceous skin discoloration with vesicle formation that is often apparent within 24 hours of symptom onset, presence of fluid-filled bullae, tense edema with crepitus, cutaneous anesthesia and frank necrosis. Histological findings show extensive subcutaneous and fascial necrosis [Figure 8].[39] NF has been associated with traumatic events in patients with compromised immune systems, diabetes, chronic steroid use and alcoholism.[40] Approximately two thirds of cases are associated with group A β-hemolytic streptococcus (GAS). This is a commensal organism that can also cause pharyngitis, pyoderma (impetigo), pneumonia, meningitis, and puerperal sepsis.[41] A wide variety of other bacteria have also been isolated in NF, including group G β-hemolytic streptococcus (GGS), Staphylococcus aureus, Escherichia coli, Pseudomonas, Enterobacter, Klebsiella, Proteus, Bacteroides, Clostridium, and Moraxella catarrhalis. Whether these are primary infections, or secondary to GAS, remains uncertain.[42,43,44] Infections spread into the fibrous septae within the orbit from fibrofatty-fascial tissue planes in the eyelid. This can lead to intense perivasculitis and potentially, loss of vision, when ophthalmic or central retinal artery thrombosis occurs.[45] CT and MRI may help in making an early diagnosis, through identification of soft tissue edema infiltrating the fascial planes and/or subcutaneous emphysema.
Figure 8.
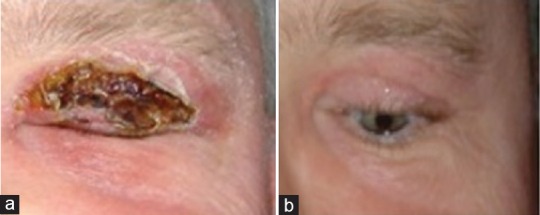
A healthy 50-year-old male presented with deteriorating periorbital swelling which had failed to respond to IV benzylpenicillin and flucloxacillin. Necrotic changes developed in the upper eyelid, and he became pyrexial. Investigations identified neutrophilia, raised CRP (417), and an ESR of 61 mm/hr. (a) Diagnosis of necrotizing fasciitis was made and he underwent immediate surgical debridement of the necrotic lid tissue. He improved rapidly following surgery. (b) Defect healed by granulation, resulting in a minor degree of lagophthalmos but no corneal exposure.
NF can progress rapidly, over the course of hours to days, leading to septicemia, multi-organ failure, and death for a quarter of patients [Figure 9].[43] Suspected NF of the periorbita and orbit is, therefore, a true ophthalmic emergency.[42,43,44,45] Effective management depends on timely diagnosis, immediate treatment, including high-dose parenteral penicillin and clindamycin, aggressive debridement of necrotic subcutaneous tissue, and repeated debridements if necessary.[46] It is important to note that all patients with suspected periorbital NF should be monitored extremely closely. Furthermore, the infectious diseases team should have active input, given the potentially destructive and rapidly progressive nature of this disease.[39]
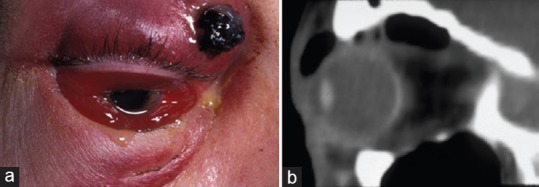
Figure 9.

An elderly diabetic patient presented with periocular necrotizing fasciitis. Septicemia developed rapidly and death ensued due to multiple organ failure. Necrotizing fasciitis is an ophthalmic emergency and should be treated immediately.
SUMMARY
Infection of the orbit is relatively common, and can be associated with significant morbidity including loss of vision, meningitis, intracranial abscess, and death. Therefore, clinicians should be aware of the clinical signs, etiology and appropriate management. A reliable history and examination are essential for any patient who is suspected of having an orbital infection in order to treat them promptly and preserve both sight and life. Orbital cellulitis management involves urgent IV antibiotics, rehydration and treatment of any co-existing underlying systemic disease. In addition, if a patient fails to respond to appropriate measures for a presumed infection, the diagnosis must be reconsidered.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Footnotes
N.B.: There may not be a sequential transition through each stage – for example, patients may present with an intraorbital abscess without pre-existing subperiosteal collection.
REFERENCES
- 1.Patt BS, Manning SC. Blindness resulting from orbital complications of sinusitis. Otolaryngol Head Neck Surg. 1991;104:789–795. doi: 10.1177/019459989110400604. [DOI] [PubMed] [Google Scholar]
- 2.Tomac S, Turgut S. Orbital cellulitis and irreversible visual loss owing to acute sinusitis. Ann Ophthalmol. 2006;38:131–133. doi: 10.1385/ao:38:2:131. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999;27:375–379. doi: 10.1046/j.1440-1606.1999.00242.x. [DOI] [PubMed] [Google Scholar]
- 4.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–1423. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Smith AT, Spencer JT. Orbital complications resulting from lesions of the sinuses. Ann Otol Rhinol Laryngol. 1948;57:5–27. doi: 10.1177/000348944805700101. [DOI] [PubMed] [Google Scholar]
- 6.Dhariwal DK, Kittur MA, Farrier JN, Sugar AW, Aird DW, Laws DE. Post-traumatic orbital cellulitis. Br J Oral Maxillofac Surg. 2003;41:21–28. doi: 10.1016/s0266-4356(02)00259-0. [DOI] [PubMed] [Google Scholar]
- 7.Barone SR, Aiuto LT. Periorbital and orbital cellulitis in the Haemophilus influenzae vaccine era. J Pediatr Ophthalmol Strabismus. 1997;34:293–296. doi: 10.3928/0191-3913-19970901-08. [DOI] [PubMed] [Google Scholar]
- 8.Ambati BK, Ambati J, Azar N, Stratton L, Schmidt EV. Periorbital and orbital cellulitis before and after the advent of Haemophilus influenzae type B vaccination. Ophthalmology. 2001;108:1514–1515. doi: 10.1016/s0161-6420(00)00178-0. [DOI] [PubMed] [Google Scholar]
- 9.Nageswaran S, Woods C, Benjamin D, Givner LB, Shetty A. Orbital Cellulitis in Children. Pediatr Infect Dis J. 2006;25:695–699. doi: 10.1097/01.inf.0000227820.36036.f1. [DOI] [PubMed] [Google Scholar]
- 10.Rubin SE, Slavin ML. Rubin LG: Eyelid swelling and erythema as the only signs of subperiosteal abscess. Br J Ophthalmol. 1989;73:576–578. doi: 10.1136/bjo.73.7.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rose GE. Suspicion, speed, sufficiency and surgery: Keys to the management of orbital infection. Orbit. 1998;17:223–226. doi: 10.1076/orbi.17.4.223.2735. [DOI] [PubMed] [Google Scholar]
- 12.Antoine GA, Grundfast KM. Periorbital cellulitis. Int J Pediatr Otorhinolaryngol. 1987;13:273–278. doi: 10.1016/0165-5876(87)90108-x. [DOI] [PubMed] [Google Scholar]
- 13.Partamian LG, Jay WM, Fritz KJ. Anaerobic orbital cellulitis. Ann Ophthalmol. 1983;15:123–126. [PubMed] [Google Scholar]
- 14.Weiss A, Friendly D, Eglin K, Chang M, Gold B. Bacterial periorbital and orbital cellulitis in childhood. Ophthalmology. 1983;90:195–203. doi: 10.1016/s0161-6420(83)34573-5. [DOI] [PubMed] [Google Scholar]
- 15.Chen L, Silverman N, Wu A, Shinder R. Intravenous steroids with antibiotics on admission for children with orbital cellulitis. Ophthal Plas Reconstr Surg. 2017 doi: 10.1097/IOP.0000000000000910. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Greenberg MF, Pollard ZF. Medical treatment of pediatric subperiosteal orbital abscess secondary to sinusitis. J AAPOS. 1998;2:351–355. doi: 10.1016/s1091-8531(98)90033-7. [DOI] [PubMed] [Google Scholar]
- 17.Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: Analysis of outcomes 1988-1998. Ophthalmology. 2000;107:1454–1456. doi: 10.1016/s0161-6420(00)00242-6. [DOI] [PubMed] [Google Scholar]
- 18.Rudloe TF, Harper MB, Prabhu SP, Rahbar R, Vanderveen D, Kimia AA. Acute periorbital infections: Who need emergent imaging? Pediatrics. 2010;125:e719–726. doi: 10.1542/peds.2009-1709. [DOI] [PubMed] [Google Scholar]
- 19.Vu BL, Dick PT, Levin AV, Pirie J. Development of a clinical severity score for preseptal cellulitis in children. Pediatr Emerg Care. 2003;19:302–307. [PubMed] [Google Scholar]
- 20.Smith JM, Bratton EM, Dewitt P, Davies BW, Hink EM, Durairaj VD. Predicting the need for surgical intervention in pediatric orbital cellulitis. Am J Ophthalmol. 2014;158:387–394. doi: 10.1016/j.ajo.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 21.Clary R, Weber AL, Eavey R, Oot RF. Orbital cellulitis with abscess formation caused by sinusitis. Ann Otol Rhinol Laryngol. 1988;97:211–212. doi: 10.1177/000348948809700222. [DOI] [PubMed] [Google Scholar]
- 22.Bergin DJ, Wright J. Orbital cellulitis. Br J Ophthalmol. 1986;70:174–178. doi: 10.1136/bjo.70.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson K, Baker SR. Periorbital cellulitis. Head Neck Surg. 1987;9:227–234. doi: 10.1002/hed.2890090406. [DOI] [PubMed] [Google Scholar]
- 24.Slavin ML, Glaser JS. Acute severe irreversible visual loss with sphenoethmoiditis “posterior” orbital cellulitis. Arch Ophthalmol. 1987;105:345–348. doi: 10.1001/archopht.1987.01060030065027. [DOI] [PubMed] [Google Scholar]
- 25.Bullock JD, Fleishman JA. Orbital cellulitis following dental extraction. Trans Am Ophthalmol Soc. 1984;87:111–133. [PMC free article] [PubMed] [Google Scholar]
- 26.Gatot A, Tovi F, Moshiashvili A. Periorbital cellulitis: Presenting feature of undiagnosed old maxillary fracture. Int J Pediatr Otorhinolaryngol. 1986;11:129–134. doi: 10.1016/s0165-5876(86)80007-6. [DOI] [PubMed] [Google Scholar]
- 27.Murphy C, Livingstone I, Foot B, Murgatroyd H, MacEwen CJ. Orbital cellulitis in Scotland: Current incidence, aetiology, management and outcomes. Br J Ophthalmol. 2014;98:1575–1578. doi: 10.1136/bjophthalmol-2014-305222. [DOI] [PubMed] [Google Scholar]
- 28.Harris GJ Subperiosteal inflammation of theorbit. A bacteriological analysis of 17 cases. Arch Ophthalmol. 1988;106:947–952. doi: 10.1001/archopht.1988.01060140093032. [DOI] [PubMed] [Google Scholar]
- 29.Hartstein ME, Steinvurzel MD, Cohen CP. Intracranial abscess as a complication of subperiosteal abscess of the orbit. Ophthal Plast Reconstr Surg. 2001;17:395–397. doi: 10.1097/00002341-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Weber AL, Mikulis DK. Inflammatory disorders of the periorbital sinuses and their complications. Radiol Clin North Am. 1987;25:615–630. [PubMed] [Google Scholar]
- 31.Hodges E, Tabbara KF. Orbital cellulitis: Review of 23 cases from Saudi Arabia. Br J Ophthalmol. 1989;73:205–208. doi: 10.1136/bjo.73.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang T, Seif D, Chilstrom M, Mailhot T. Ocular ultrasound identifies early orbital cellulitis. West J Emerg Med. 2014;15:394. doi: 10.5811/westjem.2014.4.22007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yen MT. Current Techniques for the Management of Orbital Cellulitis. Tech Ophthalmol. 2006;4:45–49. [Google Scholar]
- 34.Benninger MS, Anon J, Mabry RL. The medical management of rhinosinusitis. Otolaryngol Head Neck Surg. 1997;117:S41–49. doi: 10.1016/S0194-59989770006-8. [DOI] [PubMed] [Google Scholar]
- 35.Harris GJ. Subperiosteal abscess of the orbit: Computed tomography and the clinical course. Ophthal Plast Reconstr Surg. 1996;12:1–8. doi: 10.1097/00002341-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Gold SC, Arrigg PG, Hedges TR. Computerized tomography in the management of acute orbital cellulitis. Ophthalmic Surg. 1987;18:753–756. [PubMed] [Google Scholar]
- 37.Marchiano E, Raikundalia M D, Carnio E, Echanique KA, Kalyoussef E, Baredes S, et al. Characteristics of patients treated for orbital cellulitis: An analysis of inpatient data. Laryngoscope. 2016;126:554–559. doi: 10.1002/lary.25529. [DOI] [PubMed] [Google Scholar]
- 38.Yen MT, Yen KG. Effect of corticosteroids in the acute management of pediatric orbital cellulitis with subperiosteal abscess. Ophthal Plast Reconstr Surg. 2005;21:363–366. doi: 10.1097/01.iop.0000179973.44003.f7. [DOI] [PubMed] [Google Scholar]
- 39.Mehta R, Kumar A, Crock C, McNab A. Medical management of periorbital necrotising fasciitis. Orbit. 2013;32:253–255. doi: 10.3109/01676830.2013.788667. [DOI] [PubMed] [Google Scholar]
- 40.Casey K, Cudjoe P, Green III JM, Valerio IL. A recent case of periorabital necrotizing faciitis- presentation to definitive reconstruction within an In-Theater combat hospital setting. J Oral Maxillofac Surg. 2014;72:1320–1324. doi: 10.1016/j.joms.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 41.Currie BJ. Group A streptococcal infections of the skin: Molecular advances but limited therapeutic progress. Curr Opin Infect Dis. 2006;19:132–138. doi: 10.1097/01.qco.0000216623.82950.11. [DOI] [PubMed] [Google Scholar]
- 42.Headley AJ. Necrotizing soft tissue infections: A primary care review. Am Fam Phys. 2003;15(68):323–328. [PubMed] [Google Scholar]
- 43.Childers BJ, Potyondy LD, Nachreiner R, Rogers FR, Childers ER, Oberg KC, et al. Necrotizing fasciitis: A fourteen-year retrospective study of 163 consecutive patients. Am Surg. 2002;68:109–116. [PubMed] [Google Scholar]
- 44.Brittain CJ, Penwarden A, Mearza A, Verity D. Moraxella as a cause of necrotizing fasciitis of the eyelid. Eye. 2006;2006:1312–1314. doi: 10.1038/sj.eye.6702173. [DOI] [PubMed] [Google Scholar]
- 45.Elner VM, Demirci H, Nerad JA, Hassan AS. Periocular necrotizing fasciitis with visual loss Pathogenesis and treatment. Ophthalmology. 2006;113:2338–2345. doi: 10.1016/j.ophtha.2006.06.037. [DOI] [PubMed] [Google Scholar]
- 46.Costet-Fighiera C, Lagier J, Bastiani-Griffet F, Bernard E, Gastaud P. Necrotizing fasciitis of the eyelids and orbit: A life-threatening ophthalmological emergency. J Fr Ophtalmol. 2002;25:375–378. [PubMed] [Google Scholar]


