Abstract
Background
Vertebral compression fracture is common in osteoporosis, but can also occur due to bone metastases, for which current treatment options are limited and include bone-strengthening with cement and supportive care. Kyphoplasty is a surgical method of bone augmentation that can reduce pain, stabilize vertebral bone, and restore some or all of the vertebral body height. The aim of this study was to investigate the clinical results of balloon kyphoplasty in the correction of vertebral deformity due to metastatic vertebral compression fracture.
Material/Methods
A retrospective clinical study included 72 patients (82 vertebral bodies) with metastases resulting in vertebral compression fracture, treated by percutaneous balloon kyphoplasty; 9 patients were found incidentally to have vertebral metastases. Bone mineral density (BMD) levels were measured. Patient responses from questionnaires, including the visual analog scale (VAS) for pain intensity, and the Oswestry Disability Index (ODI) for disability, were scored. The local kyphosis angle (KA) and the vertebral height ratio (VHR) were measured. All patients were followed up for 12 months. The initial postoperative and 12-month postoperative values, and the preoperative and postoperative values were compared.
Results
Following balloon kyphoplasty, the KA, VHR, VAS, and ODI scores significantly improved at the final 12-month follow-up compared with preoperative levels (p<0.05, and p<0.001). There was cement leakage in 6 procedures (8.3%) and adjacent segment fracture in 11 procedures (15.2%).
Conclusions
Balloon kyphoplasty was an effective method to reduce pain, reduce disability, and improve quality of life by eliminating kyphotic deformity in pathological vertebral compression fractures due to vertebral metastases.
MeSH Keywords: Kyphoplasty, Neoplasm Metastasis, Spinal Fractures
Background
Worldwide, the average lifespan is increasing, and the prevalence of vertebral compression fracture has become more common. Vertebral compression fracture, as a result of weakening of the bone, mainly occurs due to osteoporosis, but malignant tumors can metastasize to the vertebral bone, resulting in compression fractures. In some patients, the initial diagnosis of malignancy is found incidentally by imaging findings and from a biopsy of the tumor metastasis in the vertebral body in patients presenting with vertebral deformity.
Bone metastases from primary solid tumors are common, with a reported rate of 30–95% from primary breast, lung, bladder, and thyroid cancers [1,2]. In patients with multiple myeloma, vertebral fractures can be due to osteolytic lesions in the course of the disease or from generalized osteoporosis [1].
Spontaneous vertebral compression fractures can cause severe pain, kyphotic deformity, impaired respiratory function, and deterioration of quality of life. The main goals of the treatment of vertebral compression fracture are to reduce pain, improve functional ability, and reduce future risk of fracture [2–4]. Bed rest, analgesics, and the use of braces or corsets can be used in the conservative management of vertebral compression fractures. While non-surgical treatment may have limited effects, prolonged immobilization can also exacerbate osteoporosis and increase the risk of thromboembolic events.
Despite poor bone quality in fractured vertebrae, open surgery can be performed in patients with neurological deficit and also when intracanalicular bone fragments are present, but these methods carry a high risk, particularly in patients with co-morbidities [5]. The method of balloon kyphoplasty was introduced by Garfin and colleagues in 2015, who described the percutaneous approach to the vertebral body via the pedicle percutaneously to correct the vertebral height and kyphotic deformity [6]. Balloon kyphoplasty, which is a minimally invasive technique compared with open surgery, is effective in correcting pain and deformity. In this percutaneous procedure, the balloon is inflated and polymethyl methacrylate (PMMA) is injected into the corrected vertebra to fill the gap. Recent randomized controlled clinical trials have shown that in patients with vertebral compression fractures due to tumor metastases, percutaneous kyphoplasty, when compared with open surgery, reduces pain and improves patient functional ability and quality of life [5,7].
The aim of this retrospective clinical study was to investigate the clinical results of balloon kyphoplasty, a surgical method of bone augmentation, in the correction of vertebral deformity due to vertebral compression fracture associated with tumor metastases, in a single center. The initial postoperative and 12-month postoperative values and the preoperative and postoperative values were compared.
Material and Methods
Ethics approval and patient consents
This was a retrospective clinical study that compared patient symptoms and imaging findings before and after treatment. The study was conducted according to the principles of the World Medical Association Declaration of Helsinki, ‘Ethical Principles for Medical Research Involving Human Subjects’ (amended in October 2013). Informed consent was obtained from all patients who participated in the study.
Patients studied
This retrospective clinical review included 72 patients (82 vertebrae) who consecutively underwent balloon kyphoplasty for vertebral compression fractures due to metastases between 2013 and 2016 at our hospital. Seventeen (23.6%) of the patients were men and 55 (76.4%) were women; the mean age was 78.93±8.77 years. The demographic characteristics of the patients are shown in Table 1.
Table 1.
Clinical and demographic factors in the patients in the study.
| Patients (n=72) | |
|---|---|
| Age (years, mean ±SD) | 78.93±8.77 |
| Gender (n,%) | |
| Male | 17 (23.6%) |
| Female | 55 (76.4%) |
| Follow-up (month, mean ±SD) | 18.91±3.71 |
| Bone mineral density (BMD, mean ±SD) | 3.19±0.46 |
| Polymethyl methacrylate (PMMA) volume (ml, mean ±SD) | 5.21±0.91 |
| Incidental metastatic tumours (n) | |
| Breast cancer | 1 |
| Chronic lymphocytic leukemia | 1 |
| Multipl myeloma | 4 |
| Adenocarcinoma metastasis (lung) | 2 |
| Gastric cancer | 1 (postoperative 7 month exitus) |
SD – standard deviation.
Study design
Patients with severe pain due to acute (<2 weeks) or subacute (2–8 weeks) vertebral compression fractures and with >30° kyphotic deformity who did not respond to conservative treatment methods, including 2 weeks of bed rest, treatment with non-steroidal anti-inflammatory drugs (NSAIDs), or with supporting corsets or braces were included in the study. Patients with previous vertebroplasty, kyphoplasty, vertebral collapse of more than 90%, patients with neurological deficit, urinary or fecal incontinence, or unstable vertebral fractures associated with involvement of the posterior vertebral elements were excluded from the study. Patients with incidentally discovered vertebral metastasis were referred to the local medical oncology clinical team.
Imaging, bone mineral density (BMD), visual analog scale (VAS), and the Oswestry Disability Index (ODI) scores
Vertebral radiographs and magnetic resonance imaging (MRI) examinations of affected vertebrae were evaluated in all patients. Preoperative and postoperative visual analog scale (VAS) score questionnaires were used to assess pain intensity. According to the requirements of the VAS, the patients were asked to rate their pain from 0 to 10, with 0 being the lowest score with no pain, and 10 being the highest score with the worst pain ever experienced.
The functional ability status of all patients in the study was assessed using the Oswestry Disability Index (ODI) scale [8]. The ODI consists of a self-completed questionnaire that contains 10 topics concerning the intensity of pain, the ability to lift, the ability to care for oneself, the ability to walk, the ability to sit, sexual function, the ability to stand, social life, sleep quality, and the ability to travel. Each topic category was followed by 6 statements describing different potential scenarios in the patient’s life relating to the topic. In the standard ODI questionnaire, each patient checked the statement that most closely matched their situation.
Each question in the ODI questionnaire was scored on a scale of 0–5, with 0 being the lowest score with no disability and 5 being the highest score with the most severe disability. The scores for all questions answered were added together and then multiplied by 2 to obtain the ODI score (range 0–100). For the ODI score, a score of 0 indicated no disability and a score of 100 indicated the maximum disability possible. The patients were followed-up at 1, 6, and 12 months. VAS and ODI evaluations of the patients were done postoperatively, and again at 1-month, 6-month, and 12-month follow-up examinations of all patients, including radiography and vertebral MRI.
Local kyphosis angle (KA), and vertebral height ratio (VHR)
Local kyphosis angle (KA) and vertebral height ratio (VHR) were measured via direct radiography. The local kyphosis angle was measured by the Cobb method. The VHR is the ratio of the height of the frontal edges of the lower and upper adjacent vertebrae to the height of the anterior margin of the fractured vertebra. Bone edema in acute fractures was shown by MRI with short tau inversion recovery sequences (STIR) (Figure 1). Intravenous contrast series were also evaluated in all patients. KA and VHR were recorded preoperatively and postoperatively at 1 and 12 months. The difference in KA at 1 and 12 months postoperatively was recorded as loss of correction.
Figure 1.
Magnetic resonance imaging (MRI) in a patient with a vertebral body compression fracture at T6. Preoperative T2-weighted (A) and T1-weighted (B) magnetic resonance imaging (MRI) sequences of the patient before kyphoplasty. After kyphoplasty procedure (C) MRI appearance following kyphoplasty.
Bone mineral density (BMD) measurements
Bone mineral density (BMD) measurements and the levels of the vertebral fractures were noted. BMD was measured preoperatively using bone densitometry, also called dual-energy x-ray absorptiometry (DEXA), in the lumbar spine (L1–L4) and the proximal femur. The mean BMD value was calculated as the mean value of the vertebrae in each patient from L1 to L4, the previous vertebral strengthened level value was subtracted from this mean, and the T-score of the patients (their BMD compared with a healthy adult) before the operation were recorded.
Surgical technique: Percutaneous balloon kyphoplasty
All procedures were performed in the operating room under sedation and local anesthesia. Cephazolin sodium (1 gm) was administered intravenously and all patients were placed in the prone position. The vertebral fracture level was centered with anteroposterior (AP) and lateral radiographic views, assisted by a mobile C-arm scope and monitor. Two 11-gauge Jamshidi biopsy needles were inserted percutaneously on AP imaging, entering the upper outer margin of the pedicle ring, with a transpedicular approach into the fractured vertebra corpus. Two guided Kirschner wires were used to place a cannula into the posterior half of the vertebral body. As in routine practice, each patient had a biopsy from the cannula in this area. Two balloons were simultaneously inflated, guided by the C-arm scope lateral view until the restoration of the vertebral height was observed. The balloons were deflated and 4–6 cc of polymethyl methacrylate (PMMA) was injected into the vertebrae via the pedicle. Postoperative AP and direct lateral radiographs were evaluated to detect any leakage of PMMA following kyphoplasty.
Statistical analysis
In this study, the initial postoperative and 12-month postoperative values were compared, and the preoperative and postoperative values were compared. Statistical analysis was performed using SPSS for Windows© software, version 21.0 (Armonk, NY, USA). Variables were analyzed using visual analysis, including histograms and probability plots. Analytical methods were investigated using the Kolmogorov-Smirnov and Shapiro-Wilk tests, to determine whether they were normally distributed. Descriptive data are presented using the mean and standard deviation (SD) for normally distributed variables. Since bone mineral density and kyphotic angle values were normally distributed, the t test was used to compare these parameters between the postoperative and the 12-month values. The VAS and ODI scores were not normally distributed, so the Wilcoxon test was used to compare the preoperative and postoperative values. A P-value <0.05 was considered to represent a statistically significant result.
Results
There were 72 patients (82 intervertebral bodies) who underwent percutaneous balloon kyphoplasty between 2013 and 2016. The mean follow-up period was 18.91±3.71 months and the mean bone mineral density (BMD) values of the patients were 3.19±0.46. Simultaneous kyphoplasty was performed in 8 patients in 2 levels and in 1 patient in 3 levels (Table 1).
The preoperative local kyphosis angle (KA) measured in the patients in the study decreased from 13.45±6.73 to 7.67±1.67 in the first postoperative month and the vertebral height ratio (VHR) improved by 55.75±12.82% preoperatively to 75.33±10.21 in the first postoperative month (p <0.05). At the 12th postoperative month, these values declined to 8.55±1.55 for the KA and 74.27±10.54 for the VHR, suggesting minimal and non-significant deterioration (Figure 2). The mean loss of correction was 0.88° at 12 months.
Figure 2.
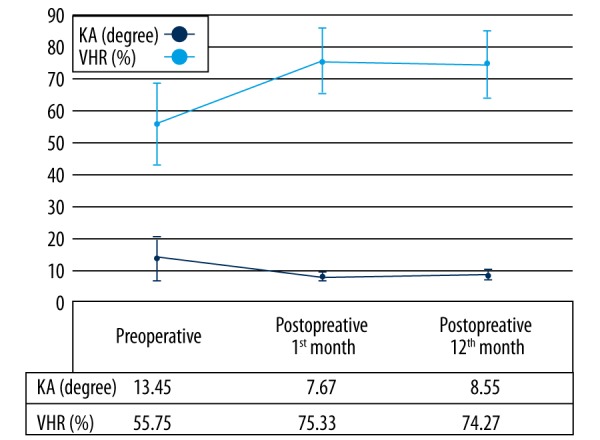
Preoperative, postoperative, 6-month, and 12-month kyphotic angle (KA) and vertebral height ratio (VHR) values.
Preoperative VAS and ODI scores 8.11±0.83 and 65.51±7.32, respectively, which significantly declined by 6 months postoperatively to 2.01±0.77 and 25.67±5.28, respectively (p<0.001). The VAS and ODI scores by 12 months postoperatively significantly declined to 2.55±1.16 and 25.18±4.37, respectively (P<0.001) (Figure 3).
Figure 3.
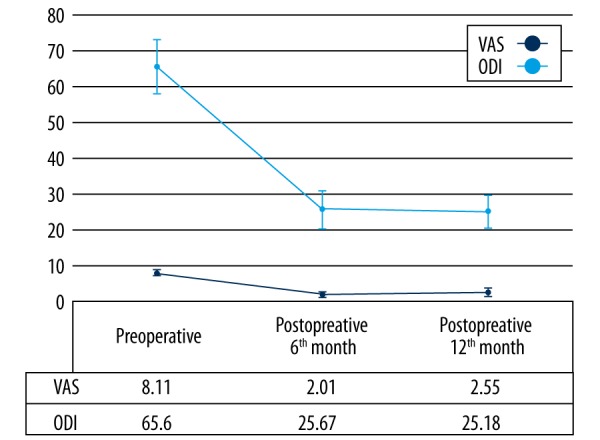
Preoperative, postoperative, 6-month, and 12-month Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) scores.
The mean polymethyl methacrylate (PMMA) volume was 5.21±0.91 ml. In 6 cases (8.3%) there was post-procedural cement leakage, associated with upper endplate fracture. No neurological complications were associated with cement leakage. Neighboring segment fractures were observed in 11 patients (15.2%) on follow-up.
Vertebral involvement with multiple myeloma was found in 4 patients who underwent kyphoplasty; 1 patient was found to have metastatic breast cancer; 1 patient had metastatic renal cancer; and 2 patients had metastatic adenocarcinoma of the lung. No tumor recurrence was observed at 12-month follow-up. However, 1 patient with metastatic gastric cancer died at 7 months postoperatively. Complications such as neurological deficit or cardiopulmonary embolism due to treatment were not observed in any patients.
Discussion
The main goals in the treatment of symptomatic vertebral fracture are pain relief, correction of vertebral height, and correction of kyphotic angulation [9]. Early intervention is important in this group of patients, who are usually elderly, to reduce morbidity and mortality. Vertebral compression fractures are most commonly seen in osteoporotic patients. However, in 10–15% of patients with vertebral fracture, an incidental malignant tumor metastasis is reported to be the cause [10]. In the present study, the rate of incidental malignancy was 12.5% (9/72), which is comparable with the previously published literature.
The aim of this study was to investigate the clinical results of balloon kyphoplasty in the correction of vertebral deformity due to a metastatic vertebral compression fracture. All patients were followed up for 12 months. The initial postoperative and 12-month postoperative values and the preoperative and postoperative values were compared. The main findings were that the preoperative vertebral height ratio (VHR) of the patients was 53.6±13.4% and the mean VHR was increased by 21.1% to 74.7±11.3% (p<0.005). The local kyphosis angle (KA) was 15.3±11.4 before the procedure and 8.02±2.9 after the procedure (P<0.005). In previously published studies, restoration of VHR with kyphoplasty was reported to be 12.8–31.7% and the KA correlation was 3.9–16.5° [11–13]. In these previous studies, the lowest KA cure rate was reported in patients with rheumatoid arthritis [14].
In the present study, 1 patient died of gastric cancer 7 months postoperatively and was removed from the study. No tumor recurrence was found in the 12-month controls of the other patients with tumors, and no significant deterioration was found in the KA correction and VHR. Falco and Bochetti found a slight variation of deformation of VHR and KA only in 3 patients between the 5-year and immediate postoperative surgery follow-up [15]. In a previously published study, mid-thoracic and transition zone vertebral compression fractures showed significant improvement in VHR with balloon kyphoplasty [16]. Kyphoplasty has been proposed to be an effective method of improving KA and vertebral compression fractures [17].
One of the alternative treatments for vertebral compression fracture is vertebroplasty and radiotherapy. In the vertebroplasty procedure, similar to kyphoplasty, only cement is given via a cannula placed in the vertebra corpus, but vertebra height restoration is not possible. Vertebroplasty has a high risk of symptomatic or asymptomatic cement leakage from procedural complications. The literature contains no non-randomized clinical trials on vertebroplasty in the pain treatment of vertebral compression fractures associated with cancer metastasis. Two randomized studies of vertebroplasty in osteoporosis patients compared non-surgical treatment with vertebroplasty [5,18]. The first of these trials reported that there was no significant change in pain intensity at 3 and 12 months, but in a small group of patients. In the present study, with a larger number of patients, the decrease in pain intensity at the end of the 12th month was more obvious.
In pathological analysis, due to vertebral metastasis, or osteoporotic vertebral compression fractures, balloon kyphoplasty has been shown to provide a significant reduction in pain intensity, and improved mobilization scores, including in a randomized controlled study of kyphoplasty in cancer patients that used the Roland Morris Disability Questionnaire (RDQ) [16]. However, a further randomized controlled clinical trial compared patients with balloon kyphoplasty with non-surgical osteoporotic patients with vertebral compression fractures, and showed that pain intensity and functional status improved significantly in the first month [19]. However, similar results were seen in the control group at the end of 12 months [19]. The findings of the present study also showed significant improvement in these scores (p<0.001), which might be due to effective VHR and KA correction, and that the 12-month loss of correction does not show any significant change. When patients with osteoporotic and pathologic vertebral compression fractures were compared, no significant difference was found in terms of KA, VHR, VAS, and ODI scores (P>0.05).
Another factor in this study that might have contributed to the decrease in pain intensity was the amount of cement used in the vertebrae. This view is supported by a previously published study that showed that the pain relief effect in patients with vertebroplasty was related to the amount of cement applied to the vertebrae [20]. In this previous study, the authors argued that cement amounts of 4–8 ml gave adequate restoration and rigidity to the bones [20].
However, excessive segmental polymethyl methacrylate (PMMA) augmentation can result in adjacent segment fractures. Kyphoplasty provides homogenous cement augmentation in spaces opened by the balloons on both sides of the spine while being effective in maintaining height restoration. In the present study, post-procedural pain decreased significantly, and mean cement volume was around 4.6±1.3 ml. Several previous authors have reported cement leakage of 4–45%. In a previously reported vertebroplasty series that included 37 patients, 29 patients had metastases and 8 patients had multiple myeloma [21]. Despite the patients showing excellent pain relief, in this previous study, surgery was required for 72.5% of patients with cement leakage and for 2 symptomatic patients who required neurological decompression [21].
In the present study, 6 cases (8.3%) had cement leakage, and all of them were due to upper endplate fracture. In these patients, no neurological deficit due to cement leakage was observed and no additional surgical procedure was performed. In 2015, Zapałowicz et al. [22] reported 17% of patients with balloon kyphoplasty had cement leakage, while in the same year, Bouza et al. reported 27% of cases had cement leakage [13]. Therefore, kyphoplasty might be a more reliable method in terms of cement leakage than vertebroplasty.
The balloon kyphoplasty method is effective in KA and VHR correction and was found in the present study to reduce pain. Pain treatment and supportive care in metastatic spinal disease might extend the average lifespan for patients, and cement strengthening techniques have previously been used to facilitate early patient mobilization in the treatment of metastatic fractures due to lung adenocarcinoma, eosinophilic granuloma, and vertebral hemangioma. The use of PMMA to fill the gap formed when the deformity is corrected by balloon kyphoplasty is effective in forming a solid structure. This method makes early mobilization possible and provides increased functional capability by reducing pain.
A disadvantage of the percutaneous balloon kyphoplasty method is its high cost, but due to pain relief and shorter duration of hospital stay, the use of kyphoplasty may lead to long-term healthcare cost savings.
This study had several limitations. This was a retrospective study performed in a single center with a relatively small patient population eligible for inclusion in the study. The involvement of the same surgeon in performing the kyphoplasty technique each time may be a strength of the study, but the participation of a single surgeon might be criticized as introducing bias regarding patient selection or outcome. This study did not contain a control population of patients and we did not compare KA and VHR with operated pedicle screw patients. Therefore, a prospective, large-scale, multicenter, randomized, controlled study is needed to provide the evidence required to evaluate any future roles or recommendations for the use of percutaneous balloon kyphoplasty in the management of patients with vertebral metastases.
Conclusions
Percutaneous balloon kyphoplasty is an effective method to reduce pain and improve quality of life by eliminating kyphotic deformity in pathological vertebral fractures. In particular, a biopsy is recommended for the detection of incidental tumors during treatment of osteoporotic vertebral fractures.
Acknowledgements
None.
Footnotes
Source of support: Departmental sources
References
- 1.Kaloostian PE, Yurter A, Zadnik PL, et al. Current paradigms for metastatic spinal disease: An evidence-based review. Ann Surg Oncol. 2014;21:248–62. doi: 10.1245/s10434-013-3324-8. [DOI] [PubMed] [Google Scholar]
- 2.Smith M, Coleman R, Klotz L, et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: Comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol. 2014;26:368–74. doi: 10.1093/annonc/mdu519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X, Yang KH, Wanyan P, Tian JH. Comparison of the efficacy and safety of denosumab versus bisphosphonates in breast cancer and bone metastases treatment: A meta-analysis of randomized controlled trials. Oncol Lett. 2014;7:1997–2002. doi: 10.3892/ol.2014.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guckenberger M, Mantel F, Gerszten PC, et al. Safety and efficacy of stereotactic body radiotherapy as primary treatment for vertebral metastases: A multi-institutional analysis. Radiat Oncol. 2014;9:226. doi: 10.1186/s13014-014-0226-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dohm M, Black C, Dacre A, et al. A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis. Am J Neuroradiol. 2014;35:2227–36. doi: 10.3174/ajnr.A4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tutton SM, Pflugmacher R, Davidian M, et al. KAST study: The Kiva system as a vertebral augmentation treatment – a safety and effectiveness trial: A randomized, noninferiority trial comparing the Kiva system with balloon kyphoplasty in treatment of osteoporotic vertebral compression fractures. Spine. 2015;40:865–75. doi: 10.1097/BRS.0000000000000906. [DOI] [PubMed] [Google Scholar]
- 7.Terpos E, Berenson J, Raje N, Roodman GD. Management of bone disease in multiple myeloma. Expert Rev Hematol. 2014;7:113–25. doi: 10.1586/17474086.2013.874943. [DOI] [PubMed] [Google Scholar]
- 8.Fairbank JC. Why are there different versions of the Oswestry Disability Index? A review. J Neurosurg Spine. 2014;20:83–86. doi: 10.3171/2013.9.SPINE13344. [DOI] [PubMed] [Google Scholar]
- 9.Saxena BP, Shah BV, Joshi SP. Outcome of percutaneous balloon kyphoplasty in vertebral compression fractures. Indian J Orthop. 2015;49:458–64. doi: 10.4103/0019-5413.159673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendler D, Bauer DC, Davison K, et al. Vertebral fractures: Clinical importance and management. Am J Med. 2016;129:221.e1–10. doi: 10.1016/j.amjmed.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 11.Ateş A, Gemalmaz HC, Deveci MA, et al. Comparison of effectiveness of kyphoplasty and vertebroplasty in patients with osteoporotic vertebra fractures. Acta Orthop Traumatol Turc. 2016;50(6):619–22. doi: 10.1016/j.aott.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshii T, Ueki H, Kato T, et al. Severe kyphotic deformity resulting from collapses of cemented and adjacent vertebrae following percutaneous vertebroplasty using calcium phosphate cement. A case report. Skelet Radiol. 2014;43:1477–80. doi: 10.1007/s00256-014-1912-8. [DOI] [PubMed] [Google Scholar]
- 13.Bouza C, López-Cuadrado T, Almendro N, Amate JM. Safety of balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures in Europe: A meta-analysis of randomized controlled trials. Eur Spine J. 2015;24:715–23. doi: 10.1007/s00586-014-3581-7. [DOI] [PubMed] [Google Scholar]
- 14.Shim J, Lee K, Kim H, et al. Outcome of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fracture in patients with rheumatoid arthritis. BMC Musculoskel Disord. 2016;17:365. doi: 10.1186/s12891-016-1215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Falco R, Bocchetti A. Balloon kyphoplasty for pure traumatic thoracolumbar fractures: Retrospective analysis of 61 cases focusing on restoration of vertebral height. Eur Spine J. 2014;23:664–70. doi: 10.1007/s00586-014-3548-8. [DOI] [PubMed] [Google Scholar]
- 16.Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: A multicentre, randomised controlled trial. Lancet Oncol. 2011;12:225–35. doi: 10.1016/S1470-2045(11)70008-0. [DOI] [PubMed] [Google Scholar]
- 17.Yaltirik K, Ashour AM, Reis CR, et al. Vertebral augmentation by kyphoplasty and vertebroplasty: 8 years experience outcomes and complications. J Craniovertebral Junction Spine. 2016;7:153–60. doi: 10.4103/0974-8237.188413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao H, Yang J, Feng X, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: A meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol. 2015;25:77–85. doi: 10.1007/s00590-014-1502-4. [DOI] [PubMed] [Google Scholar]
- 19.Wang H, Sribastav SS, Ye F, et al. Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: A meta-analysis of the literature. Pain Physician. 2015;18:209–22. [PubMed] [Google Scholar]
- 20.Ioannis P, Andreas B, Panagiotis K. Calcium phosphate cement leakage during balloon kyphoplasty causing incomplete paraplegia: Case report and review of the literature. Journal of Orthopedic and Spine Trauma. :2016. [in Press] [Google Scholar]
- 21.Gu Y-F, Tian Q-H, Li Y-D, et al. Percutaneous vertebroplasty and interventional tumor removal for malignant vertebral compression fractures and/or spinal metastatic tumor with epidural involvement: A prospective pilot study. J Pain Res. 2017;10:211–18. doi: 10.2147/JPR.S122211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zapałowicz K, Radek M. Percutaneous balloon kyphoplasty in the treatment of painful vertebral compression fractures: Effect on local kyphosis and one-year outcomes in pain and disability. Neurol Neurochir Pol. 2015;49:11–15. doi: 10.1016/j.pjnns.2014.11.005. [DOI] [PubMed] [Google Scholar]



