Abstract
An inability to recover lateral balance with a single step is predictive of future falls in older adults. This study investigated if balance stability at first step lift-off (FSLO) would be different between multiple and single stepping responses to lateral perturbations. 54 healthy older adults received left and right waist-pulls at 5 different intensities (levels 1–5). Crossover stepping responses at and above intensity level 3 that induced both single and multiple steps were analyzed. Whole-body center of mass (COM) and center of pressure (COP) positions in the medio-lateral direction with respect to the base of support were calculated. An inverted pendulum model was used to define the lateral stability boundary, which was also adjusted using the COP position at FSLO (functional boundary). No significant differences were detected in the COP positions between the responses at FSLO (p ≥ 0.075), indicating no difference in the functional boundaries between the responses. Significantly smaller stability margins were observed at first step landing for multiple steps at all levels (p ≤ 0.024), while stability margins were also significantly smaller at FSLO for level 3 and 4 (p ≤0.048). These findings indicate that although reduced stability at first foot contact would be associated with taking additional steps, stepping responses could also be attributable to the COM motion state as early as first step lift-off, preceding foot contact. Perturbation-based training interventions aimed at improving the reactive control of stability would reduce initial balance instability at first step lift-off and possibly the consequent need for multiple steps in response to balance perturbations.
Keywords: Falls, Lateral stability, Perturbation, Stepping, Inverted pendulum model
1. Introduction
An impaired ability to control lateral balance is one of the important balance problems relevant to falls (Maki and McIlroy, 1996, 2006; O’Neill et al., 1994; Robinovitch et al., 2013; Rogers and Mille, 2003). In response to lateral perturbations of standing balance, older adults are much more likely than younger adults to take multiple balance recovery steps with a crossover or medial step strategy, which increases the potential for inter-limb collisions and subsequent falls (Bair et al., 2016; Maki et al., 2000; Mille et al., 2013, 2005). Use of multiple recovery steps has been a consistent finding that distinguishes older adults from younger adults and older fallers from non-fallers (Hilliard et al., 2008; Luchies et al., 1994; Maki and McIlroy, 2006; Mille et al., 2005; Patton et al., 2006). An inability to recover lateral balance with a single step is predictive of future falls (Hilliard et al., 2008). As protective responses with multiple steps have been shown to be a sensitive predictor of fall risk, it is important to identify underlying factors that lead to multiple steps to recover lateral balance.
When balance is disturbed by external means, the central nervous system (CNS) appears to estimate the current and future states of motion of the whole-body center of mass (COM) in relation to the base of support (BOS) on the basis of ongoing sensory information (Maki and Mcilroy, 1999; Rogers and Mille, 2016), which may determine the number of steps used to prevent falling. The CNS appears to monitor the evolving state of balance stability and modify the triggered response in an online manner to safe-guard stability. Such an estimation of dynamic stability may underlie the choices for recovery step strategies (i.e., type of step and single versus multiple steps).
Dynamic balance stability has been quantified based on the position-velocity relationship between the COM and BOS (Carty et al., 2011; Hof et al., 2005; Pai and Patton, 1997; Pai et al., 1998). The tendency for older adults to step more often than younger subjects has been well predicted by a reduced margin of stability for forward or backward steps, where the level of instability of the initial step, indicated by the reduced margin of stability at first foot contact, has been reported to be strongly predictive of the recovery strategies employed (Carty et al., 2011; Hsiao and Robinovitch, 2001; Maki and Mcilroy, 1999). These studies indicate that instability at foot contact would be a determinant of the use of multiple stepping.
Although reduced stability at foot contact has been linked with the use of additional steps, stepping strategies for balance recovery may also be determined by factors preceding foot contact. For example, older adults may preplan to take a series of small steps to gain a greater opportunity to make corrective adjustments in the response (Luchies et al., 1994; Maki et al., 2000). Since more adjustments can be made to correct for any ill-chosen responses, multiple stepping by older adults may be a more conservative response to ensure stability to disturbances that fully stress their balance capacity (Luchies et al., 1994). Thus, even earlier than the first step ground contact, the CNS might estimate the evolving level of instability and select to make different protective stepping responses. In doing so, stepping strategies can be enacted in a pre-determined manner and the use of multiple steps may be attributable to the level of stability as early as the instant of first step lift-off (FSLO).
To further examine these issues, the objective of this study was to compare balance stability at FSLO between single and multiple step recoveries in response to lateral perturbations of standing balance in older adults. An inverted pendulum model was used to define the BOS lateral stability boundary at FSLO, which was also adjusted using the COP position at FSLO (functional boundary). It was hypothesized that reduced balance stability would be observed for multiple step recovery responses at FSLO.
2. Methods
2.1. Subjects
A total of 54 healthy, community dwelling older adults [25 males/29 females; mean age: 73.6 ± 6.7 years; mean height: 1.67 ± 0.10 m, mean body mass: 77.3 ± 15.9 kg] participated in this study. 6 male and 10 female participants had a history of falls during the year prior to testing as indicated by self-report. The exclusion criteria were the same as those reported in our previous studies (Bair et al., 2016; Fujimoto et al., 2015; Young et al., 2013; Yungher et al., 2012). All participants provided written, informed consent prior to participation, and the study was approved by the Institutional Review Board at the University of Maryland School of Medicine and the Baltimore Veteran’s Administration Medical Center.
2.2. Data collection
Participants received a total of 60 randomly applied, position-controlled, motor-driven waist-pull lateral perturbations at five different intensities (Levels 1–5) in the left and right directions (L and R pulls). The system has been previously described (Pidcoe and Rogers, 1998) and used in prior studies (Bair et al., 2016; Fujimoto et al., 2015; Hilliard et al., 2008; Mille et al., 2013, 2005; Young et al., 2013; Yungher et al., 2012). Six trials were conducted for each of 5 different pull intensities to the left and to the right (2 directions × 5 intensities × 6 repetitions). The order in which the trials were presented was randomized to prevent anticipatory and sequence learning effects. Wearing a safety harness, participants stood in a self-selected, comfortable standing position with each foot on a separate force platform (Advanced Mechanical Technology Inc., Newton, MA, USA) and held a light cylindrical rod with both hands in front of the body at the start of each trial. The foot locations were traced to ensure consistent initial foot placement. They were instructed to “relax and react naturally to prevent themselves from falling.”
Whole body motion was captured with a six-camera motion analysis system (Vicon 460, Oxford, UK). 28 reflective markers were placed according to Eames et al. with additional markers on the medial malleoli and 5th metatarsophalangeal (MP) joints (Eames et al., 1999). Three-dimensional marker trajectories were collected at 120 Hz and smoothed using a fourth-order Butterworth filter with a cut-off frequency of 8 Hz. Ground reaction forces (GRFs) were collected by two force plates located under each foot at 600 Hz and filtered with a 10 Hz cut-off frequency (Hernandez et al., 2012; Maki et al., 1994).
2.3. Data analysis
Since crossover stepping with the limb that was passively unloaded by the lateral perturbation is a common maneuver used by older adults (Maki and McIlroy, 2006; Mille et al., 2005), crossover stepping responses with single and multiple steps were compared. To ensure that subjects responded with both single and multiple step recovery responses, the balance tolerance limit (BTL), the minimum intensity level where multiple steps (mean number of steps greater than 1) occurred, was determined (Yungher et al., 2012). Crossover stepping responses to the perturbations above the average BTL, which induced both single and multiple step responses, were analyzed.
The whole-body COM was calculated as the weighted sum of 13 body segments (Eames et al., 1999). The COM and stance foot center of pressure (COP) positions in the medio-lateral (ML) directions at FSLO were referenced to the medial malleolus and normalized to the BOS width. The BOS width was the ML distance between the medial malleolus and the 5th MP joint of the stance foot (Fig. 1). FSLO timing was determined as the instant when the vertical GRF of the stepping foot was reduced to less than 10 N (Brauer et al., 2002). The onset latency of the first step was calculated as the time interval between the perturbation onset and FSLO.
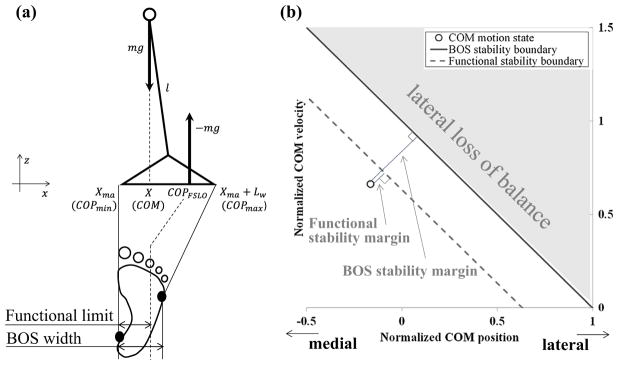
Fig. 1.
(a) A single-link-plus-foot inverted pendulum model in the frontal plane. X indicates the COM position in the ML direction. m and l are the whole body mass and pendulum length (distance from the ankle to the COM). Lw and Xma are the BOS width and medial ankle marker position. The lateral stability boundaries were defined in two ways: one based on the actual BOS width (BOS stability boundary), and the other adjusted according to the COP position at FSLO (COPFSLO), considering it as a functional limit for COP movement (functional stability boundary). (b) COM motion state with respect to the lateral stability boundaries. Stability margins were calculated as the shortest distance from the location of the COM position-velocity combination (○) to the respective lateral stability boundaries.
A single-link-plus-foot inverted pendulum model for the stance foot was used to define the lateral stability boundary (Fig. 1). Since previous studies have shown that the area functionally used for COP movement is smaller than the actual BOS (Fujimoto et al., 2015, 2013; King et al., 1994), the lateral stability boundary was adjusted based on the COP position at FSLO, considering it as a functional limit for COP movement to control the COM (Fig. 1). Thus, the lateral stability boundaries were defined in two ways: one based on the actual BOS width (BOS stability boundary), and the other adjusted according to the functional limit (functional stability boundary). These boundaries were defined using the following equation based on the work of Hof et al. (Hof et al., 2005):
where X̃FSLO, are normalized COM position and velocity at FSLO in the ML direction, defined as X̃FSLO = (XFSLO − Xma)/Lw, (where , Lw: BOS width, Xma: position of the medial ankle marker, l: pendulum length). COPFSLO is the COP position at FSLO referenced to the medial ankle. The stability margins for both the BOS and functional boundaries were defined as the shortest distance from the location of the COM position-velocity combination to the respective lateral stability boundaries (Yang et al., 2008).
Step length, COM-to-ankle distance (COM-ankle distance), COM velocity (COMv), and stability margins at first step ground contact (FSGC) in the ML direction were also calculated to assess first step characteristics. FSGC was identified from the vertical velocity of the step side lateral ankle marker (Hilliard et al., 2008; Mille et al., 2013, 2005; Patton et al., 2006; Yungher et al., 2012). The FSGC timing was determined as the instant when the vertical velocity became less than 10 mm/s in the downward direction. Step length was calculated as the ML displacement of the stepping ankle joint center between FSLO and FSGC. COM-ankle distance was the distance between the COM and ankle joint center at FSGC. COMv was the COM velocity at FSGC. Step length was normalized to the subjects’ leg length, calculated as the distance between the greater trochanter and lateral malleolus (Yungher et al., 2012). COM-ankle distance and COMv were also normalized by the leg length. To assess the stability margins at FSGC, the ML distance between the left and right ankle joint centers was considered as the BOS width and the mean distance from the COM to the left and right ankle joint centers at FSGC was used as the pendulum length.
A paired t-test was performed to examine differences between single and multiple stepping responses for step characteristics at first step lift-off (first step onset latency, COP position, COM position and velocity, and stability margins at FSLO), as well as the first step characteristics (step length, COM-ankle distance, COM velocity, and stability margin at FSGC). Since our previous study did not identify any differences in outcome measures between the perturbation directions (Young et al., 2013), responses to the left and right perturbations were combined at each perturbation level. Analyses were performed independently for each perturbation level since the subjects who responded with both single and multiple steps were different depending on the perturbation level. A one sample t-test was also performed to determine if the stability margins at FSLO were significantly different from zero. Statistical analyses were performed using SPSS (Chicago, IL). Significance level was set at α = 0.05.
3. Results
The average BTL was 2.93 and 2.98 for the L and R pulls, respectively, and thereby single and multiple crossover stepping responses for perturbation magnitude levels 3, 4, and 5 were analyzed (Table 1).
Table 1.
Number of subjects who responded with both single and multiple crossover steps at each perturbation level.
| Perturbation level | # of subjects |
|---|---|
| Level 3 | 24 (9 men/15 women) |
| Level 4 | 24 (13 men/11 women) |
| Level 5 | 7 (3 men/4 women) |
There were no significant differences in the step onset latency between the single and multiple stepping responses (p ≥ 0.513, Table 2). No significant differences were also detected for the normalized COP position at FSLO between the single and multiple stepping responses (p ≥ 0.075, Table 2).
Table 2.
Step onset latency and normalized COP position for single and multiple step responses (mean ± SD) at each perturbation level.
| n | Single | Multiple | p | |
|---|---|---|---|---|
| Step onset latency [ms] | ||||
| Level 3 | 24 | 365 ± 93 | 369 ± 97 | 0.513 |
| Level 4 | 24 | 369 ± 94 | 367 ± 102 | 0.817 |
| Level 5 | 7 | 325 ± 62 | 330 ± 65 | 0.599 |
| Normalized COP position | ||||
| Level 3 | 24 | 0.61 ± 0.09 | 0.60 ± 0.08 | 0.371 |
| Level 4 | 24 | 0.63 ± 0.07 | 0.61 ± 0.07 | 0.075 |
| Level 5 | 7 | 0.62 ± 0.06 | 0.62 ± 0.06 | 0.607 |
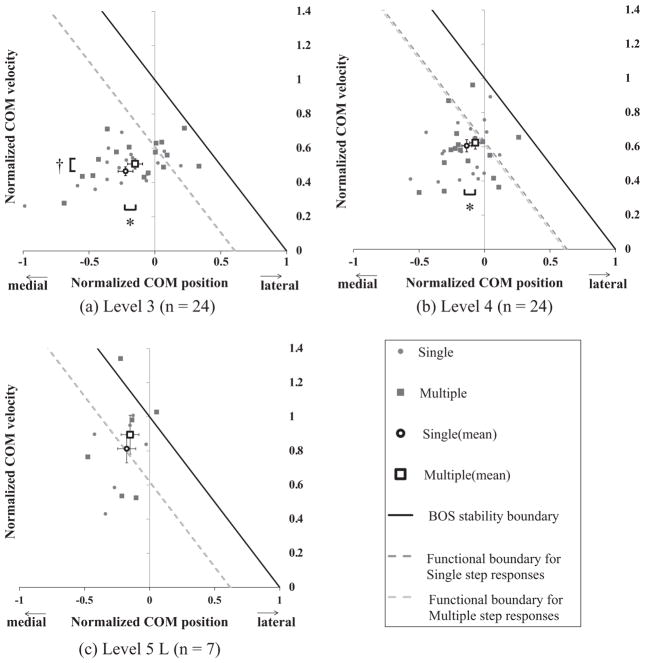
The COM at FSLO for multiple steps was located more lateral to that for single steps with significant differences found at level 3 and 4 (p ≤ 0.045, Fig. 2). Larger COM velocities at FSLO were also observed for multiple steps with significance found at level 3 (p = 0.004). Accordingly, stability margins at FSLO for both the BOS and functional boundaries were smaller for multiple steps with significance found for level 3 and 4 (p ≤ 0.048, Fig. 3). In addition, the functional stability margins were not significantly different from zero for multiple steps (p ≥ 0.263) except for level 3 (p = 0.006), indicating that they closely reached the functional stability limits, while the margins were significantly different from zero for single steps (p ≤ 0.034), except for level 5 (p = 0.894).
Fig. 2.
Normalized COM velocity vs. normalized COM position at FSLO in the ML direction for single (●) and multiple (■) step responses at (a) perturbation level 3, (b) level 4, and (c) level 5. Mean for each group (○ and □) are also indicated. Error bars are SEM. The solid line indicates the BOS stability boundary based on the actual BOS width. The two dashed lines indicate the functional stability boundaries for single and multiple step responses. Since the functional boundaries vary between subjects, the average for all subjects within the group was shown here. (a) *p = 0.013, †p = 0.004; (b) *p = 0.045.
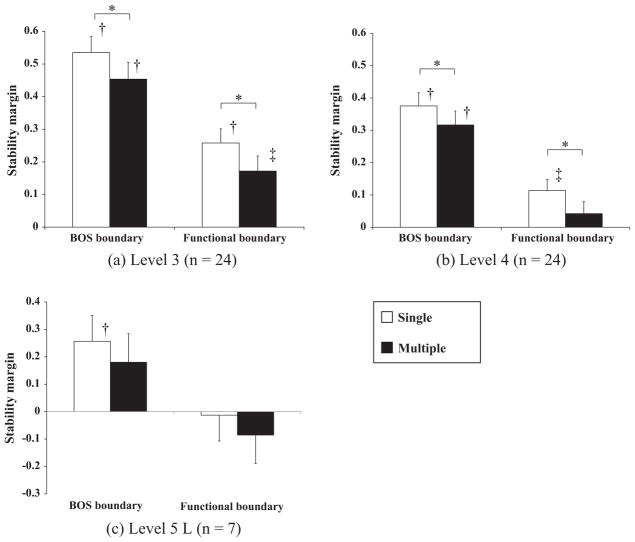
Fig. 3.
Stability margins (unitless) at first step lift-off based on the BOS and functional stability boundaries at (a) perturbation level 3, (b) level 4, and (c) level 5. Values and error bars are mean and SEM. *Indicate a significant difference between single and multiple responses. †and ‡indicate that the stability margin is significantly different from zero. (a) *p = 0.003, †p < 0.001, ‡p = 0.006; (b) *p = 0.003, †p < 0.001, ‡p = 0.004; (c) †p = 0.034.
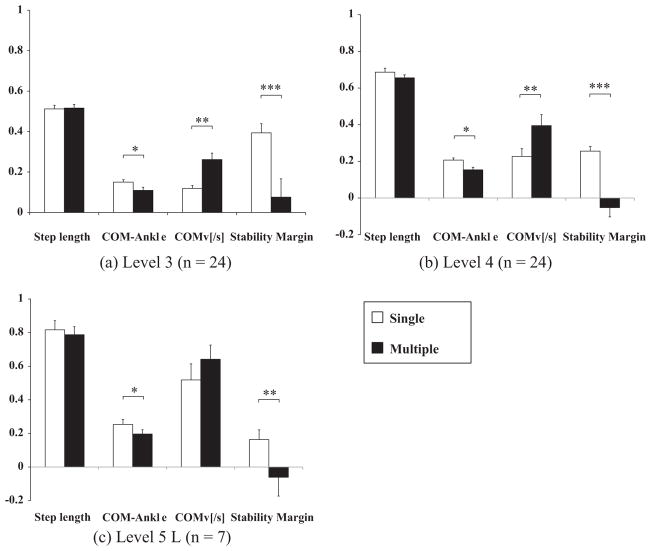
At FSGC, no significant differences were detected in the step length between the responses (p ≥ 0.063, Fig. 4). The COM-ankle distance was significantly smaller for multiple steps (p ≤ 0.041). The COMv was larger for multiple steps with significance found at levels 3 and 4 (p ≤ 0.018). Furthermore, the stability margins at FSGC were significantly smaller for multiple steps at all levels (p ≤ 0.024, Fig. 4).
Fig. 4.
First step characteristics: Step length, COM-to-ankle distance (COM-Ankle), COM velocity (COMv), and Stability margin at first step contact in the ML direction, normalized by leg length at (a) perturbation level 3, (b) level 4, and (c) level 5. Values and error bars are mean and SEM. (a) *p = 0.017, **p < 0.001, ***p = 0.002; (b) *p = 0.001, **p = 0.018, ***p < 0.001; (c) *p = 0.041, **p = 0.024.
4. Discussion
The objective of this study was to compare balance stability at first step lift-off between single and multiple step recoveries in response to lateral perturbations of standing balance in older adults. Crossover stepping responses at and above intensity level 3 that induced both single and multiple steps were analyzed. The main findings were that significantly smaller stability margins were observed at first step landing for the multiple steps at all levels, while stability margins were also significantly smaller at first step lift-off for level 3 and 4. These findings indicate that the use of multiple steps could be attributable to the COM motion state as early as the time of first step lift-off.
Our previous study found a reduced functional limit of stability for COP movement in older fallers, who took multiple steps more often, compared with older non-fallers, which indicated a functional deficit in stabilizing lateral balance related to a limitation in actively controlling the COP (Fujimoto et al., 2015). In contrast, the COP positions at first step lift-off were similar between the responses in the present study (Table 2), indicating no differences in the functional stability boundaries. These results suggested that even when different protective stepping responses were used, the area functionally used for COP movement was utilized comparably within the same individuals. Thus, the use of a multiple versus single stepping responses would not appear to entirely reflect differences in the functional limit for COP movement.
Smaller stability margins at first step lift-off were observed for multiple steps with significance found at level 3 and 4 (Fig. 3). Such reduced stability at first step lift-off has been identified in the forward direction for older multiple steppers compared with older single steppers (Carty et al., 2012). In that report, they compared single versus multiple “steppers”, i.e., individuals with low and high risk of falls, considering that older fallers more often use multiple steps than non-fallers (Hilliard et al., 2008; Maki and McIlroy, 2006; Mille et al., 2005). However, it was unclear if such reduced stability was directly associated with the use of multiple steps since they compared the different groups rather than directly comparing single versus multiple stepping performances. Comparing the responses within the same individuals in the present study allowed us to determine if the use of different stepping responses reflected differences in balance stability. Our results demonstrated that even within the same individuals, reduced stability was observed when multiple steps were used.
Consistent with previous findings, reduced stability margins were observed at the first step ground contact for multiple steps at all levels (Fig. 4), indicating that stability at landing may be a determinant of taking multiple steps (Carty et al., 2012, 2011). We have further demonstrated that such reduced stability could result from the initial state of instability (level 3 and 4, Fig. 3). There were no significant differences in step length between the responses, but smaller stability margins were observed at first step lift-off for the multiple steps for level 3 and 4 pulls, which appears to result in smaller stability margins at landing. An estimation of the mechanical state conditions for stability as early as first step lift-off based on a forward internal model, may have been used to determine the use of single or multiple step recoveries (Rogers and Mille, 2016). It should also be noted that the COM motion state for the multiple stepping responses was closer to the functional boundary, rather than the BOS boundary. Except for the level 3 pulls, the stability margin for multiple steps was not significantly different from zero for the functional boundary (Fig. 3), i.e. approximating the functional stability limit at first step lift-off. The combined results imply that an initial state of balance instability, reaching the functional stability limit, increased the subsequent need for online correction with multiple steps even though a similar first step length was used.
Among the limitations of this study, was the smaller number of subjects for level 5. This is because the perturbation was strong enough to induce multiple steps in most of the trials. A loss of significance at level 5 appears to have resulted from this smaller sample size. However, the same trend found for the other pulling magnitudes was seen whereby stability margins were smaller or more negative for the multiple steps. It should also be noted that some of the participants had a history of falls, and may have responded differently than non-fallers and influenced our results. However, when only the subjects without a history of falls were analyzed, the main findings were unaffected whereby the stability margins were smaller for the multiple steps at FLSO (Level 3: n = 20, p < 0.001; Level 4: n = 21, p = 0.055; Level 5: n = 6, p = 0.364). Another limitation was that the subjects analyzed were different depending on the perturbation level, which prevented us from comparing the results of the same individuals across different perturbation levels. However, at least for the subjects who responded with both single and multiple steps for perturbation level 3 and 4 (n = 14), a two-way repeated measures ANOVA, with level (level 3 and 4) and step type (single and multiple steps) as factors, indicated significant main effects of step type on the BOS and functional stability margins at FSLO (p ≤ 0.009) and on the stability margins at landing (p < 0.001), consistent with our main findings.
In conclusion, no significant difference was detected in the COP positions at FSLO, indicating no difference in functional boundaries between the single and multiple stepping responses. Overall, the findings indicated that although reduced stability at first foot contact could be a determinant of taking additional steps, stepping responses could also be attributable to the COM motion state as early as first step lift-off, preceding foot contact. Since perturbation training has been reported to improve the reactive control of balance stability (Barrett et al., 2012; Dijkstra et al., 2015; Kurz et al., 2016; Mansfield et al., 2015; Pai et al., 2014; Rosenblatt et al., 2013), which increased balance stability at the instant of step lift-off (Lee et al., 2016; Liu et al., 2016), perturbation-based training interventions aimed at improving the reactive control of stability would reduce initial balance instability at first step lift-off and possibly the consequent need for multiple steps in response to balance perturbations.
Acknowledgments
This study was supported by NIH grant RO1AG029510, the University of Maryland Claude D. Pepper - Older Americans Independence Center Grant (OAIC) NIH/NIA grant P30 AG028747, NIDRR UMANRRT grant H133P100014, and the Baltimore VA Medical Center, Geriatric Research, Education and Clinical Center (GRECC).
Footnotes
Conflict of interest
The authors have no conflicts of interest in relation to the work reported here.
References
- Bair WN, Prettyman MG, Beamer BA, Rogers MW. Kinematic and behavioral analyses of protective stepping strategies and risk for falls among community living older adults. Clin Biomech. 2016;36:74–82. doi: 10.1016/j.clinbiomech.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett RS, Cronin NJ, Lichtwark GA, Mills PM, Carty CP. Adaptive recovery responses to repeated forward loss of balance in older adults. J Biomech. 2012;45:183–187. doi: 10.1016/j.jbiomech.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Brauer SG, Woollacott M, Shumway-Cook A. The influence of a concurrent cognitive task on the compensatory stepping response to a perturbation in balance-impaired and healthy elders. Gait Posture. 2002;15:83–93. doi: 10.1016/s0966-6362(01)00163-1. [DOI] [PubMed] [Google Scholar]
- Carty CP, Cronin NJ, Lichtwark GA, Mills PM, Barrett RS. Mechanisms of adaptation from a multiple to a single step recovery strategy following repeated exposure to forward loss of balance in older adults. PLoS ONE. 2012;7:e33591. doi: 10.1371/journal.pone.0033591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carty CP, Mills P, Barrett R. Recovery from forward loss of balance in young and older adults using the stepping strategy. Gait Posture. 2011;33:261–267. doi: 10.1016/j.gaitpost.2010.11.017. [DOI] [PubMed] [Google Scholar]
- Dijkstra BW, Horak FB, Kamsma YP, Peterson DS. Older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci. 2015;7:201. doi: 10.3389/fnagi.2015.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eames MHA, Cosgrove A, Baker R. Comparing methods of estimating the total body centre of mass in three-dimensions in normal and pathological gaits. Hum Mov Sci. 1999;18:637–646. [Google Scholar]
- Fujimoto M, Bair WN, Rogers MW. Center of pressure control for balance maintenance during lateral waist-pull perturbations in older adults. J Biomech. 2015;48:963–968. doi: 10.1016/j.jbiomech.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto M, Hsu WL, Woollacott MH, Chou LS. Ankle dorsiflexor strength relates to the ability to restore balance during a backward support surface translation. Gait Posture. 2013;38:812–817. doi: 10.1016/j.gaitpost.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez ME, Ashton-Miller JA, Alexander NB. Age-related changes in speed and accuracy during rapid targeted center of pressure movements near the posterior limit of the base of support. Clin Biomech. 2012;27:910–916. doi: 10.1016/j.clinbiomech.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard MJ, Martinez KM, Janssen I, Edwards B, Mille ML, Zhang Y, Rogers MW. Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil. 2008;89:1708–1713. doi: 10.1016/j.apmr.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hof AL, Gazendam MG, Sinke WE. The condition for dynamic stability. J Biomech. 2005;38:1–8. doi: 10.1016/j.jbiomech.2004.03.025. [DOI] [PubMed] [Google Scholar]
- Hsiao ET, Robinovitch SN. Elderly subjects’ ability to recover balance with a single backward step associates with body configuration at step contact. J Gerontol Series A, Biol Sci Med Sci. 2001;56:M42–M47. doi: 10.1093/gerona/56.1.m42. [DOI] [PubMed] [Google Scholar]
- King MB, Judge JO, Wolfson L. Functional base of support decreases with age. J Gerontol. 1994;49:M258–M263. doi: 10.1093/geronj/49.6.m258. [DOI] [PubMed] [Google Scholar]
- Kurz I, Gimmon Y, Shapiro A, Debi R, Snir Y, Melzer I. Unexpected perturbations training improves balance control and voluntary stepping times in older adults – a double blind randomized control trial. BMC Geriatr. 2016;16:58. doi: 10.1186/s12877-016-0223-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A, Bhatt T, Pai YC. Generalization of treadmill perturbation to overground slip during gait: effect of different perturbation distances on slip recovery. J Biomech. 2016;49:149–154. doi: 10.1016/j.jbiomech.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Bhatt T, Pai YC. Intensity and generalization of treadmill slip training: high or low, progressive increase or decrease? J Biomech. 2016;49:135–140. doi: 10.1016/j.jbiomech.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchies CW, Alexander NB, Schultz AB, Ashton-Miller J. Stepping responses of young and old adults to postural disturbances: kinematics. J Am Geriatr Soc. 1994;42:506–512. doi: 10.1111/j.1532-5415.1994.tb04972.x. [DOI] [PubMed] [Google Scholar]
- Maki BE, Edmondstone MA, McIlroy WE. Age-related differences in laterally directed compensatory stepping behavior. J Gerontol Series A, Biol Sci Med Sci. 2000;55:M270–M277. doi: 10.1093/gerona/55.5.m270. [DOI] [PubMed] [Google Scholar]
- Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994;49:M72–M84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE. Postural control in the older adult. Clin Geriatr Med. 1996;12:635–658. [PubMed] [Google Scholar]
- Maki BE, Mcilroy WE. Control of compensatory stepping reactions: age-related impairment and the potential for remedial intervention. Physiother Theory Practice. 1999;15:69–90. [Google Scholar]
- Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35(Suppl 2):ii12–ii18. doi: 10.1093/ageing/afl078. [DOI] [PubMed] [Google Scholar]
- Mansfield A, Wong JS, Bryce J, Knorr S, Patterson KK. Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Phys Ther. 2015;95:700–709. doi: 10.2522/ptj.20140090. [DOI] [PubMed] [Google Scholar]
- Mille ML, Johnson-Hilliard M, Martinez KM, Zhang Y, Edwards BJ, Rogers MW. One step, two steps, three steps more ellipsis directional vulnerability to falls in community-dwelling older people. J Gerontol Series A, Biol Sci Med Sci. 2013;68:1540–1548. doi: 10.1093/gerona/glt062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mille ML, Johnson ME, Martinez KM, Rogers MW. Age-dependent differences in lateral balance recovery through protective stepping. Clin Biomech. 2005;20:607–616. doi: 10.1016/j.clinbiomech.2005.03.004. [DOI] [PubMed] [Google Scholar]
- O’Neill TW, Varlow J, Silman AJ, Reeve J, Reid DM, Todd C, Woolf AD. Age and sex influences on fall characteristics. Ann Rheum Dis. 1994;53:773–775. doi: 10.1136/ard.53.11.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J Gerontol Series A, Biol Sci Med Sci. 2014;69:1586–1594. doi: 10.1093/gerona/glu087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Patton J. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30:347–354. doi: 10.1016/s0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- Pai YC, Rogers MW, Patton J, Cain TD, Hanke TA. Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults. J Biomech. 1998;31:1111–1118. doi: 10.1016/s0021-9290(98)00124-9. [DOI] [PubMed] [Google Scholar]
- Patton JL, Hilliard MJ, Martinez K, Mille ML, Rogers MW. A simple model of stability limits applied to sidestepping in young, elderly and elderly fallers. Conf Proc IEEE Eng Med Biol Soc. 2006;1:3305–3308. doi: 10.1109/IEMBS.2006.260199. [DOI] [PubMed] [Google Scholar]
- Pidcoe PE, Rogers MW. A closed-loop stepper motor waist-pull system for inducing protective stepping in humans. J Biomech. 1998;31:377–381. doi: 10.1016/s0021-9290(98)00017-7. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, Loughin M. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013;381:47–54. doi: 10.1016/S0140-6736(12)61263-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MW, Mille ML. Lateral stability and falls in older people. Exerc Sport Sci Rev. 2003;31:182–187. doi: 10.1097/00003677-200310000-00005. [DOI] [PubMed] [Google Scholar]
- Rogers MW, Mille ML. Timing paradox of stepping and falls in ageing: not so quick and quick(er) on the trigger. J Physiol. 2016;594:4537–4547. doi: 10.1113/JP271167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. J Am Geriatr Soc. 2013;61:1629–1631. doi: 10.1111/jgs.12428. [DOI] [PubMed] [Google Scholar]
- Yang F, Passariello F, Pai YC. Determination of instantaneous stability against backward balance loss: two computational approaches. J Biomech. 2008;41:1818–1822. doi: 10.1016/j.jbiomech.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young PM, Whitall J, Bair WN, Rogers MW. Leg preference associated with protective stepping responses in older adults. Clin Biomech. 2013;28:927–932. doi: 10.1016/j.clinbiomech.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yungher DA, Morgia J, Bair WN, Inacio M, Beamer BA, Prettyman MG, Rogers MW. Short-term changes in protective stepping for lateral balance recovery in older adults. Clin Biomech. 2012;27:151–157. doi: 10.1016/j.clinbiomech.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]