Abstract
Background: Levothyroxine is the most commonly prescribed medication in the United States. Many foods and medications, including calcium supplements, can interfere with levothyroxine absorption. No studies have investigated the effect of cow's milk, a common breakfast staple, on the absorption of oral levothyroxine. Cow's milk contains approximately 450 mg of elemental calcium per 12 oz (355 mL) serving.
Methods: A pharmacokinetic study was conducted in healthy euthyroid subjects to assess levothyroxine absorption with and without concurrent cow's milk consumption. Following an overnight fast, serum total thyroxine (TT4) concentrations were measured at baseline and at one, two, four, and six hours after ingestion of 1000 μg of oral levothyroxine alone or when co-administered with 12 oz (355 mL) of 2% milk. There was a four-week washout period between the two assessments in each subject.
Results: Ten subjects (Mage ± SD = 33.7 ± 10.2 years; 60% male) completed the study. The area under the curve (AUC) of TT4 concentrations was significantly lower when levothyroxine was ingested along with 12 oz (355 mL) of 2% cow's milk (M ± SD = 67.3 ± 12.1) compared to that with levothyroxine alone (73.5 ± 17.0; p = 0.02). Also, peak serum TT4 concentrations were significantly lower when cow's milk was co-administered with levothyroxine (M ± SD = 14.1 ± 0.8 μg/dL) than with levothyroxine alone (13.0 ± 0.9 μg/dL; p = 0.04).
Conclusions: This is the first study to demonstrate that concurrent cow's milk ingestion reduces oral levothyroxine absorption. The findings support previous literature showing the interference of elemental calcium and food with thyroid hormone absorption. Patients managed with thyroid hormone should be advised to avoid taking their levothyroxine simultaneously with cow's milk.
Keywords: : milk, levothyroxine, LT4, thyroid, hypothyroidism, absorption
Introduction
Levothyroxine, as the sodium salt of the L-isomer of thyroxine, is a compound with a narrow therapeutic range that is used routinely in the clinical management of patients with hypothyroidism. It is an increasingly common medication, with levothyroxine prescriptions having risen by nearly 20% from 2007 to 2014 (1). Approximately 21.5 million patients are prescribed levothyroxine per month (2), and Synthroid-brand levothyroxine was the most commonly prescribed medication in the United States during 2015 (2).
It is advised that patients take levothyroxine 60 minutes before the first meal of the day or at least four hours apart from other medications or supplements (3), as thyroid hormone absorption can be reduced when it is co-administered with a variety of different substances, including calcium supplements. Cow's milk contains approximately 450 mg of elemental calcium per 12 oz (355 mL) serving. Milk is a popular breakfast staple. In 2010, the U.S. per capita consumption of milk was 20.4 gallons per year (4).
The objective of this study was to assess whether cow's milk decreases bioavailability of levothyroxine using a pharmacokinetic protocol among healthy euthyroid adult volunteers.
Methods
Fifteen healthy volunteers were screened to participate in the study from January to November 2016. Inclusion criteria were age >18 years and ability to read and understand English. All volunteers underwent initial screening and were found to be healthy without significant past medical history. Specifically, they did not have any gastrointestinal symptoms or digestive issues. Exclusion criteria were: history of thyroid, liver, renal, or cardiovascular disease; pregnancy or breastfeeding; allergy to levothyroxine; lactose intolerance; and use of oral contraceptives. Subjects were excluded if a urine pregnancy test was positive or indeterminate, or if a screening serum thyrotropin (TSH) was abnormal. Study and consent procedures were approved by the Institutional Review Board at the VA Greater Los Angeles Healthcare System.
Ten subjects met study eligibility criteria and completed the full protocol. The study followed a modified protocol for assessing levothyroxine bioequivalence as utilized by the U.S. Food and Drug Administration (FDA) (5). Following an overnight fast of at least eight hours, serum was obtained for the baseline measurement of serum total thyroxine (TT4). Subjects were then administered 1000 μg of oral levothyroxine (as five 200 μg Synthroid-branded tablets) with 12 oz (355 mL) of water. Serum was again obtained at one, two, four, and six hours following levothyroxine administration for the measurement of TT4. Subjects remained fasting until after sera for the one-hour time point had been collected. Following a four-week washout period, subjects then repeated the same pharmacokinetic protocol, except that subjects received 12 oz (355 mL) of 2% fat cow's milk co-administered with their 1000 μg levothyroxine dose.
Serum TSH and TT4 measurements were performed by the University of Southern California Endocrine Laboratory using an electrochemiluminescence immunoassay. All Synthroid tablets utilized for the study were of the same manufactured lot. Area under the curve values (AUCs) were constructed for serum TT4 concentrations against time. Statistical analyses were performed using paired t-tests to test for mean differences in the AUC of the serum TT4 concentrations associated with and without milk ingestion, and p-values <0.05 were considered significant.
Results
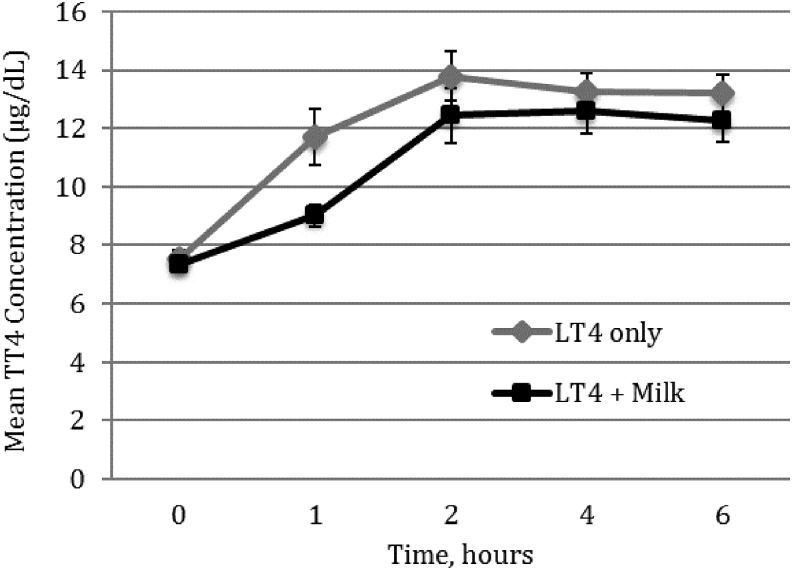
Ten subjects (Mage ± SD = 33.7 ± 10.2 years; 60% male) completed the study. The serum TT4 absorption over six hours, calculated as AUC, was significantly lower when subjects consumed 12 oz (355 mL) of 2% fat cow's milk concurrently with levothyroxine (M ± SD = 67.3 ± 12.1) compared to the AUC when they took levothyroxine alone with water (M ± SD = 73.5 ± 17.0; p = 0.02; Fig. 1). In addition, mean peak serum TT4 concentrations were significantly lower when cow's milk was co-administered with levothyroxine (13.0 ± 0.9 μg/dL) than with levothyroxine alone with water (14.1 ± 0.8 μg/dL; p = 0.04).
FIG. 1.
Serum total thyroxine absorption after ingestion of 1000 μg of oral levothyroxine alone or 1000 μg of oral levothyroxine concurrently with 12 oz of 2% cow's milk.
Discussion
This study demonstrates that oral levothyroxine absorption is impaired by co-ingestion of cow's milk. Early experiments showed that levothyroxine absorption in a fasting state was significantly higher than absorption calculated when levothyroxine was ingested simultaneously with food (6). It is now routine clinical practice to instruct patients to take their levothyroxine on an empty stomach to optimize gastrointestinal absorption of their thyroid hormone medication (3). This is the first study to show that cow's milk specifically impairs levothyroxine absorption, likely attributable to the effects of its calcium and protein content.
The present findings support those of other studies showing similar interfering effects of several foods, beverages, supplements, and medications. Decreased thyroid hormone absorption has been reported when levothyroxine is taken concurrently with substances that include coffee (7), soy products (8), calcium carbonate (9,10), iron (11), aluminum hydroxide (12), sucralfate (13,14), cholestyramine (15), colesevalam (16), raloxifene (17), orlistat (18), and phosphate binders (19) compared to when levothyroxine is taken alone (20,21).
One mechanism of interference is thought to result from nonspecific adsorption (complexing) between the aforementioned substances with levothyroxine in the gastrointestinal tract. A series of in vitro experiments by Liel et al. demonstrated that incubation of aluminum hydroxide with 125I-thyroxine and varying amounts of unlabeled T4 for two hours resulted in a positive linear association between the aluminum hydroxide concentration and T4 adsorption (12). Singh et al. later reported a similar effect from calcium carbonate in experiments at pH 2.0 (to simulate gastric acidity), while no interference was seen at pH 7.4 (10). Finally, the various formulations of calcium are all thought to interfere similarly with levothyroxine absorption. In a pharmacokinetic study of eight healthy euthyroid adults, serum TT4 concentrations were decreased whether the levothyroxine was co-administered with calcium carbonate, calcium citrate, or calcium acetate (22). There is approximately 450 mg of calcium in a 12 oz (355 mL) serving of 2% cow's milk; this calcium content likely has an effect on levothyroxine absorption.
There may also be interference related to the macronutrient content within milk. Twelve ounces (355 mL) of 2% cow's fat milk contains approximately 12 g of protein (casein and whey proteins), 7 g of fat, and 17 g of carbohydrate (lactose). Many foods that do not contain a significant amount of calcium have also been shown to affect levothyroxine absorption. Wenzel et al. found that a mixed meal containing no appreciable calcium content resulted in the decreased intestinal absorption of co-administered levothyroxine (6). Other studies have shown that co-ingestion of soy protein (8) and human serum albumin (23) with levothyroxine also affects the absorption of thyroid hormone. Thus, the macronutrient content within the foods, particularly proteins, may also be directly interfering with levothyroxine absorption.
A potential limitation to the study is the inclusion of only healthy euthyroid participants, although it is postulated that the interference by cow's milk of levothyroxine absorption would be similar in hypothyroid patients managed on long-term thyroid hormone replacement. The current study utilized a similar protocol to those of multiple previous studies examining the effects of substances interfering with levothyroxine absorption (7,9,10,22), although a more ideal but less practical design would have been to fast subjects for the entire duration of each absorption study. Also, it is important to note that the study utilized 2% cow's milk, and that there is a range of commercially available cow's milk with varying fat content; that is, skim milk contains 0% milk fat, and whole milk contains 4% milk fat, but both contain approximately 450 mg of calcium per 12 oz (355 mL) serving. Given the specific fat and nutritional makeup of 2% fat cow's milk, the results of this study may not be applicable to other types of milk, including other sources of calcium-containing milk, such as fortified soy milk (which contains approximately 300–600 mg of calcium per 12 oz [355 mL] serving) and the various popular nut milks (such as fortified almond milk, which contains approximately 375–675 mg calcium per 12 oz [355 mL] serving) (24–26). The specific time interval threshold between which the levothyroxine dose and milk can be consumed without interfering effects was also not studied in the protocol and remains unknown.
Another consideration of this study is that tablet levothyroxine was not compared to the newer liquid and soft gel capsule formulations of thyroid hormone. In several recent studies, switching from levothyroxine tablets to the oral liquid formulation in patients with levothyroxine malabsorption due to calcium supplementation, iron supplementation, sevelamer, or proton-pump inhibitors caused a significant decrease in serum TSH concentrations (27–29). Another study showed that the soft gel capsule formulation of levothyroxine, Tirosint, consistently had the highest dissolution compared to tablet levothyroxine and was less affected by pH or presence of surfactant (30). The effect of milk on these new liquid and soft gel capsule levothyroxine formulations was not studied in the current report. In the protocol, participants remained fasting until at least the sera for the one-hour time point had been collected to isolate the effect of the concurrent milk ingestion. In addition, all Synthroid-branded tablets used in the study were of the same manufactured lot, thus minimizing the variability of actual thyroid hormone content between pills.
Finally, both prescription levothyroxine use and cow's milk ingestion are common. Thus, these findings are generalizable to a substantial proportion of patients in the general population. In a recent study, most patients taking levothyroxine monotherapy routinely also use medications or eat foods/beverages that have the potential to interfere with thyroid hormone absorption (31). Potentially unnecessary frequent changes of levothyroxine dose, based on fluctuating serum TSH concentrations, are associated with increased utilization of healthcare costs and resources (32).
In conclusion, this study supports the recommendation that patients should be cautioned to take their levothyroxine apart from cow's milk, likely due to the interfering effects of the calcium and protein content in milk.
Acknowledgments
This study was supported by NIH K23HD068552 (A.M.L.).
Author Disclosure Statement
The authors report no conflicts of interest in this work.
References
- 1.Rodriguez-Gutierrez R, Maraka S, Ospina NS, Montori VM, Brito JP. 2017. Levothyroxine overuse: time for an about face? Lancet Diabetes Endocrinol 5:246–248 [DOI] [PubMed] [Google Scholar]
- 2.Brown T. The 10 most-prescribed and top-selling medications through March 2015. Available at: www.medscape.com/viewarticle/844317 (accessed June2, 2017)
- 3.Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, Cooper DS, Kim BW, Peeters RP, Rosenthal MS, Sawka AM. 2014. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid 24:1670–1751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Polis C. By the numbers: what Americans drink in a year. Available at: www.huffingtonpost.com/2011/06/27/americans-soda-beer_n_885340.html (accessed June2, 2017)
- 5.U.S. Food and Drug Administration Department of Health and Human Services, Center for Drug Evaluation and Research 2000 Guidance for industry: levothyroxine sodium tablets—in vivo pharmacokinetic and bioavailability studies and in vitro dissolution testing. Available at: https://www.fda.gov/OHRMS/DOCKETS/98fr/991149gd.pdf (accessed March22, 2018)
- 6.Wenzel KW, Kirschsieper HE. 1977. Aspects of the absorption of oral L-thyroxine in normal man. Metabolism 26:1–8 [DOI] [PubMed] [Google Scholar]
- 7.Benvenga S, Bartolone L, Pappalardo MA, Russo A, Lapa D, Giorgianni G, Saraceno G, Trimarchi F. 2008. Altered intestinal absorption of L-thyroxine caused by coffee. Thyroid 18:293–301 [DOI] [PubMed] [Google Scholar]
- 8.Bell DS, Ovalle F. 2001. Use of soy protein supplement and resultant need for increased dose of levothyroxine. Endocr Pract 7:193–194 [DOI] [PubMed] [Google Scholar]
- 9.Singh N, Weisler SL, Hershman JM. 2001. The acute effect of calcium carbonate on the intestinal absorption of levothyroxine. Thyroid 11:967–971 [DOI] [PubMed] [Google Scholar]
- 10.Singh N, Singh PN, Hershman JM. 2000. Effect of calcium carbonate on the absorption of levothyroxine. JAMA 283:2822–2825 [DOI] [PubMed] [Google Scholar]
- 11.Shakir KM, Chute JP, Aprill BS, Lazarus AA. 1997. Ferrous sulfate-induced increase in requirement for thyroxine in a patient with primary hypothyroidism. South Med J 90:637–639 [DOI] [PubMed] [Google Scholar]
- 12.Liel Y, Sperber AD, Shany S. 1994. Nonspecific intestinal adsorption of levothyroxine by aluminum hydroxide. Am J Med 97:363–365 [DOI] [PubMed] [Google Scholar]
- 13.Sherman SI, Tielens ET, Ladenson PW. 1994. Sucralfate causes malabsorption of L-thyroxine. Am J Med 96:531–535 [DOI] [PubMed] [Google Scholar]
- 14.Campbell JA, Schmidt BA, Bantle JP. 1994. Sucralfate and the absorption of L-thyroxine. Ann Intern Med 121:152. [DOI] [PubMed] [Google Scholar]
- 15.Northcutt RC, Stiel JN, Hollifield JW, Stant EG. 1969. The influence of cholestyramine on thyroxine absorption. JAMA 208:1857–1861 [PubMed] [Google Scholar]
- 16.Weitzman SP, Ginsburg KC, Carlson HE. 2009. Colesevelam hydrochloride and lanthanum carbonate interfere with the absorption of levothyroxine. Thyroid 19:77–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siraj ES, Gupta MK, Reddy SS. 2003. Raloxifene causing malabsorption of levothyroxine. Arch Intern Med 163:1367–1370 [DOI] [PubMed] [Google Scholar]
- 18.Madhava K, Hartley A. 2005. Hypothyroidism in thyroid carcinoma follow-up: orlistat may inhibit the absorption of thyroxine. Clin Oncol (R Coll Radiol) 17:492. [DOI] [PubMed] [Google Scholar]
- 19.Diskin CJ, Stokes TJ, Dansby LM, Radcliff L, Carter TB. 2007. Effect of phosphate binders upon TSH and L-thyroxine dose in patients on thyroid replacement. Int Urol Nephrol 39:599–602 [DOI] [PubMed] [Google Scholar]
- 20.Liwanpo L, Hershman JM. 2009. Conditions and drugs interfering with thyroxine absorption. Best Pract Res Clinical Endocrinol Metab 23:781. [DOI] [PubMed] [Google Scholar]
- 21.Skelin M, Lucijanić T, Amidžić Klarić D, Rešić A, Bakula M, Liberati-Čizmek AM, Gharib H, Rahelić D. 2017. Factors affecting gastrointestinal absorption of levothyroxine: a review. Clin Ther 39:378–403 [DOI] [PubMed] [Google Scholar]
- 22.Zamfirescu I, Carlson HE. 2011. Absorption of levothyroxine when coadministered with various calcium formulations. Thyroid 21:483–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hays MT1968 Absorption of oral levothyroxine in man. J Clin Endocrinol Metab 28:749–756 [DOI] [PubMed] [Google Scholar]
- 24.NIH Office of Dietary Supplements. Calcium: Fact Sheet for Health Professionals. Available at: https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/ (accessed June2, 2017)
- 25.Almond Breeze original almond milk. Available at: www.almondbreeze.com (accessed June2, 2017)
- 26.Silk original almond milk. Available at: www.silk.com (accessed June2, 2017)
- 27.Benvenga S, Di Bari F, Vita R. 2017. Undertreated hypothyroidism due to calcium or iron supplementation corrected by oral liquid levothyroxine. Endocrine 56:138–145 [DOI] [PubMed] [Google Scholar]
- 28.Vita R, Saraceno G, Trimarchi F, Benvenga S. 2014. Switching levothyroxine from the tablet to the oral solution formulation corrects the impaired absorption of levothyroxine induced by proton-pump inhibitors. J Clin Endocrinol Metab 99:4481–4486 [DOI] [PubMed] [Google Scholar]
- 29.Vita R, Di Bari F, Benvenga S. 2017. Oral liquid levothyroxine solves the problem of tablet levothyroxine malabsorption due to concomitant intake of multiple drugs. Expert Opin Drug Deliv 14:467–472 [DOI] [PubMed] [Google Scholar]
- 30.Pabla D, Akhlaghi F, Zia H. 2009. A comparative pH-dissolution profile study of selected commercial levothyroxine products using inductive coupled plasma mass spectometry. Eur J Pharm Biopharm 72:105–110 [DOI] [PubMed] [Google Scholar]
- 31.McMillan M, Rotenberg KS, Vora K, Sterman AB, Thevathasan L, Ryan MF, Mehra M, Sandulli W. 2016. Comorbidities, concomitant medications, and diet as factors affecting levothyroxine therapy: results of the CONTROL surveillance Project. Drugs R D 16:53–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ernst FR, Barr P, Elmor R, Sandulli W, Thevathasan L, Sterman AB, Goldenberg J, Vora K. 2017. The economic impact of levothyroxine dose adjustments: the CONTROL HE Study. Clin Drug Investig 37:71–83 [DOI] [PMC free article] [PubMed] [Google Scholar]