Abstract
Congenital heart disease is a significant cause of infant mortality. Epidemiology and social context play a crucial role in conditioning disease burden and modulating outcomes, while diagnosis and treatment remain resource intensive. This review will address the role of social demographics, environmental exposure, epigenetics and nutrition in the aetiology of congenital heart disease. We then discuss the determinant effect of social factors on the provision and outcomes of care for congenital heart disease and implications for practice. It is our hope that enhanced knowledge of the intersection of social determinants of health and congenital heart disease will facilitate effective preventative strategies at the individual and population levels to optimize heart health outcomes across the life course.
Keywords: Child, Heart diseases, Life course, Risk factors, Social environment, Socioeconomic factors
The impact of fetal and early life experiences on health and developmental outcomes across the life course are increasingly well mapped (1). Physical and social exposures during sensitive periods of development are now understood to shape the development and host response to a broad array of chronic diseases, of both childhood and adult onset (2). The mounting acceptance of a life course approach to human health and well-being is conditioned by accruing biological and epidemiological evidence of gene–environment interactions in the propagation and evolution of chronic diseases (3).
Heart disease is a quintessential case in point highlighting an opportunity to incorporate the role of social determinants of health, the social and economic factors that influence people’s health. The aetiology of congenital heart disease (CHD) has been considered to be multifactorial, due to both genetic predisposition and environmental influences (4), profoundly influenced by conditions in fetal and early life. Recent research has shown that gene expression can be altered by chemical modifications to the Deoxyribonucleic acid (DNA) and DNA-associated proteins in the nucleus, the epigenome. These modifications occur as a natural process during development and tissue differentiation, are heritable and can be altered in response to environmental exposures or disease (4). The insight that cardiovascular health in children and adults—once viewed as the province of genetic lottery or lifestyle choice—might hinge on the milieu of early life is transformative, to both science and policy (5). It challenges received notions of the determinants of heart disease and of the emphasis placed on strategies for prevention and treatment. A life course approach has far-reaching implications for both clinical and health system approaches to congenital heart disease (6).
FACTORS THAT AFFECT THE INTRAUTERINE LIFE STAGE
Heart malformations are the most common birth defects, affecting at least 2% of all newborns (approximately 1.35 million infants) each year worldwide (7). CHD affects both high and low income countries, with attendant burden on health systems with disparate resources and capacities. While the overall prevalence of birth defects has remained constant over time, since the 1970’s there has been an almost twofold increase in the prevalence of CHD, which may be due to changes in ascertainment and the availability of ultrasound (8). The highest overall rates of congenital heart disease are found in Asia (9.3 per 1000 live births), significantly more than in Europe (8.2 per 1000 live births) or North America (6.9 per 1000 live births) (7). The prevalence of major congenital heart disease, including hypoplastic left heart syndrome, transposition of the great arteries, truncus arteriosus, total anomalous pulmonary venous return and Tetralogy of Fallot has been reported as 1.1 per 1000 live births (9). Differential genetic and environmental risks—including disparities in social determinants of health may play formative roles in the observed geographic variation of CHD prevalence. A recent analysis of Canadian data with universal health care access revealed that children born in low income neighbourhoods had significantly higher rates of CHD (10).
The concept of childhood disease and adversity beginning in utero implicates the emerging field of epigenetics in developmental science (4). The role of epigenetics in the development of CHD is now the focus of extensive research. Most of the inherited forms of congenital heart disease are a result of mutations in cardiovascular transcription factor genes, which are regulated at the chromatin level and potentially modified by epigenetic mechanisms including environmental factors (11). Although of limited access to families of low socioeconomic status, pregnancies assisted by reproductive technology are associated with an overall increase in congenital anomalies and specific cardiac defects. Intracytoplasmic sperm injection is associated with a two- to fourfold increase in TOF occurrence (12).
It is well recognized that exposure to medications, such as antiepileptic drugs, lithium and alcohol are associated with an increased risk of developing CHD in the fetus. Although evidence is limited, there is growing concern that environmental exposures may contribute to the development of CHD. Observational studies have demonstrated increased incidence in ventricular septal defects in parents exposed to pesticides and an increase in the incidence of transposition of great arteries in maternal exposure to herbicides (13). Maternal cigarette smoking in the first trimester has also been linked to an increased incidence of CHD, and some studies have linked ambient air pollution to CHD after adjusting for socioeconomic status (14,15).
In addition to maternal environmental exposures, associations between maternal nutritional status and the development of CHD in offspring have been observed. The introduction of folate to reduce the prevalence of neural tube defects has been associated with reductions in CHD prevalence, particularly transposition of the great arteries (16). However, poor socioeconomic status may decrease the availability of folate containing foods and result in suboptimal folate levels to prevent defects. In addition, interactions between maternal lifestyle factors that alter folate metabolism, such as obesity and carrier rates of certain genetic polymorphisms, have been associated with increased rates of CHD (17). Similarly, studies have documented associations between maternal hyperglycemia and hyperlipidemia and increased risk of CHD (18). Maternal diabetes is strongly associated with certain cardiac defects and the increasing prevalence of glucose intolerance seen with maternal obesity and elevated body mass index is linked to socioeconomic status (4).
Due to advances in cardiac surgery and interventional techniques, there are now more adults than children with congenital heart disease, with corollary repercussions across the life trajectory (19). In many cases, the impact of CHD extends far beyond the patient’s diagnosis into their preoperative care, surgical management and medical therapies and follow-up, affecting the child’s and their family’s interaction and integration with their community. The social determinants of health have a bidirectional relationship with CHD, both contributing to aetiology and outcomes and in turn being influenced by the experience of living with congenital heart disease.
FACTORS THAT AFFECT THE CHILD LIFE STAGE
Adverse early childhood exposure is an important determinant of lifetime health setting children on a trajectory of increased risk for development of cardiometabolic risk. Children with congenital heart disease are equally susceptible.
Cardiometabolic disease is a leading cause of morbidity and mortality in chronic noncommunicable disease worldwide. Stressors and toxic exposures during sensitive and critical periods of early development play critical roles in determining cardiometabolic risk over the life-course (20). This is of particular relevance as metabolic syndrome is more common in adults with CHD than in the general population (21). Barker’s seminal epidemiological study demonstrated the detrimental effect of nutritional insults to the fetus and influence on later-life cardiovascular disease (20). In particular, the association of low birth weight secondary to intrauterine growth restriction, has significant association with later risk of hypertension and cardiovascular disease (4,20). Similarly, the Life Course Health Developmental Model posits that health outcomes are defined by continuous interactions between biology and developmental experiences, such as genetic, psychological, socioeconomic and cultural over the lifetime (6).
Optimal health outcomes can be obtained by promoting protective factors and reducing stress (6). Psychological stressors, negative life events and low family income are associated with childhood overweight and obesity (22). Similarly, socioeconomic disadvantage at individual to neighbourhood levels and childhood obesity and cardiometabolic risk are linked (23). Time spent in low socioeconomic position, including poor hygiene, unhealthy lifestyle habits and limited access to health care, predicts cardiovascular disease and related mortality (4). Importantly, early-life cardiovascular disease risk factors, particularly childhood obesity, independently predict adult cardiovascular disease (21).
IMPLICATIONS FOR PAEDIATRIC PRACTICE
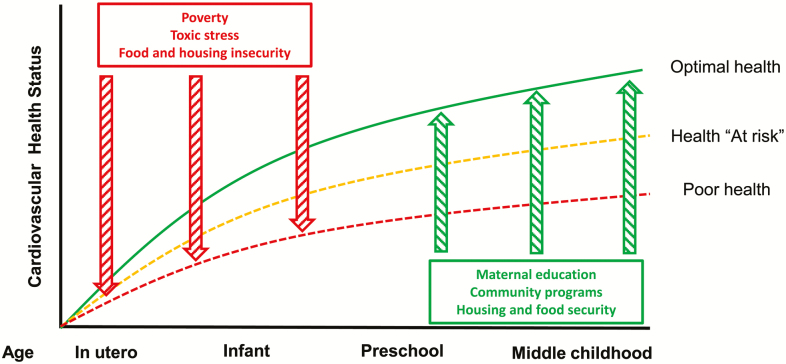
Paediatricians will need to consider a public health paradigm of preventing and promoting cardiac health across the lifespan (Figure 1). First, we will need to recognize that economic and social drivers, such as income, food security, education and access to comprehensive health care, have profound influence (24). Second, we will need to implement universal screening for social factors that identify children at risk for heart disease and connect to community resources (25,26). Finally, we will need to detect early and intervene for developmental delay in children with CHD to optimize long-term child potential (27).
Figure 1.
Effect of social determinants of health on cardiac health across childhood. Adapted from ref. (10).
KEY MESSAGES
• Cardiovascular health in children and adults is profoundly affected by the milieu of early life.
• Social antecedents play a significant role in conditioning disease burden and modulating outcomes of congenital heart disease.
• Wider introduction of universal screening for social factors that impact on cardiac health will help identify children and families at risk.
Funding sources: There are no financial relationships relevant to this article to disclose from all identified authors.
Conflict of Interest: There are no conflicts of interest or financial relationships relevant to this article to disclose from all identified authors.
References
- 1. Szilagyi M, Halfon N.. Pediatric Adverse Childhood Experiences: Implications for Life Course Health Trajectories. New York: Elsevier Science Inc, 2015. [DOI] [PubMed] [Google Scholar]
- 2. Schickedanz A, Dreyer BP, Halfon N. Childhood poverty: Understanding and preventing the adverse impacts of a most-prevalent risk to pediatric health and well-being. Pediatr Clin North Am 2015;62(5):1111–35. [DOI] [PubMed] [Google Scholar]
- 3. Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 2002;31(2):285–93. [PubMed] [Google Scholar]
- 4. Kelishadi R, Poursafa P. A review on the genetic, environmental, and lifestyle aspects of the early-life origins of cardiovascular disease. Curr Probl Pediatr Adolesc Health Care 2014;44(3):54–72. [DOI] [PubMed] [Google Scholar]
- 5. Almond D, Currie J. Killing me softly: The fetal origins hypothesis. J Econ Perspect 2011;25(3):153–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Halfon N. Socioeconomic influences on child health: Building new ladders of social opportunity. Jama 2014;311(9):915–7. [DOI] [PubMed] [Google Scholar]
- 7. van der Linde D, Konings EE, Slager MA et al. . Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J Am Coll Cardiol 2011;58(21):2241–7. [DOI] [PubMed] [Google Scholar]
- 8. Lin AE, Herring AH, Amstutz KS et al. . Cardiovascular malformations: Changes in prevalence and birth status, 1972-1990. Am J Med Genet 1999;84(2):102–10. [PubMed] [Google Scholar]
- 9. Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics 2001;107(3):E32. [DOI] [PubMed] [Google Scholar]
- 10. Agha MM, Glazier RH, Moineddin R, Moore AM, Guttmann A. Socioeconomic status and prevalence of congenital heart defects: Does universal access to health care system eliminate the gap?Birth Defects Res A Clin Mol Teratol 2011;91(12):1011–8. [DOI] [PubMed] [Google Scholar]
- 11. Chang CP, Bruneau BG. Epigenetics and cardiovascular development. Annu Rev Physiol 2012;74:41–68. [DOI] [PubMed] [Google Scholar]
- 12. Tararbit K, Houyel L, Bonnet D et al. . Risk of congenital heart defects associated with assisted reproductive technologies: A population-based evaluation. Eur Heart J 2011;32(4):500–8. [DOI] [PubMed] [Google Scholar]
- 13. Gorini F, Chiappa E, Gargani L, Picano E. Potential effects of environmental chemical contamination in congenital heart disease. Pediatr Cardiol 2014;35(4):559–68. [DOI] [PubMed] [Google Scholar]
- 14. Alverson CJ, Strickland MJ, Gilboa SM, Correa A. Maternal smoking and congenital heart defects in the Baltimore-Washington infant study. Pediatrics 2011;127(3):e647–53. [DOI] [PubMed] [Google Scholar]
- 15. Dadvand P, Rankin J, Rushton S, Pless-Mulloli T. Ambient air pollution and congenital heart disease: A register-based study. Environ Res 2011;111(3):435–41. [DOI] [PubMed] [Google Scholar]
- 16. Goh YI, Bollano E, Einarson TR, Koren G. Prenatal multivitamin supplementation and rates of congenital anomalies: A meta-analysis. J Obstet Gynaecol Can 2006;28(8):680–9. [DOI] [PubMed] [Google Scholar]
- 17. Hobbs CA, Cleves MA, Karim MA, Zhao W, MacLeod SL. Maternal folate-related gene environment interactions and congenital heart defects. Obstet Gynecol 2010;116(2 Pt 1):316–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smedts HP, van Uitert EM, Valkenburg O et al. . A derangement of the maternal lipid profile is associated with an elevated risk of congenital heart disease in the offspring. Nutr Metab Cardiovasc Dis 2012;22(6):477–85. [DOI] [PubMed] [Google Scholar]
- 19. Gilboa SM,Devine OJ,Kucik JE,et al. . Congenital heart defects in the United States. Estimating the magnitude of the affected population in 2010.Circulation 2016;134;101:–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barker DJ. Fetal nutrition and cardiovascular disease in later life. Br Med Bull 1997;53(1):96–108. [DOI] [PubMed] [Google Scholar]
- 21. Deen JF,Krieger EV,Slee AE et al.. Metabolic syndrome in adults with congenital heart disease.J Am Heart Assoc 2016;5:e001132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lumeng JC,Wendorf K,Pesch MH,et al.. Overweight adolescents and life events in childhood.Pediatrics 2013;132:e1506–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carter MA, Dubois L. Neighbourhoods and child adiposity: A critical appraisal of the literature.Health Place 2010;16(3):616–28. [DOI] [PubMed] [Google Scholar]
- 24. Botto LD, Krikov S, Carmichael SL, Munger RG, Shaw GM, Feldkamp ML. Lower rates of selected congenital heart defects with better maternal diet quality: A population-based study. Arch Dis Child Fetal Neonatal Ed 2016;101(1):F43–9. [DOI] [PubMed] [Google Scholar]
- 25. Poverty and child health in the United States. AAP Statement. Pediatrics 2016;137(4):e20160339. [DOI] [PubMed] [Google Scholar]
- 26. Fazalullasha F, Taras J, Morinis J et al. . From office tools to community supports: The need for infrastructure to address the social determinants of health in paediatric practice. Paediatr Child Health 2014;19(4):195–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tabbutt S, Gaynor JW, Newburger JW. Neurodevelopmental outcomes after congenital heart surgery and strategies for improvement. Curr Opin Cardiol 2012;27(2):82–91. [DOI] [PubMed] [Google Scholar]