Abstract
Background
Total daily physical activity is associated with a wide range of adverse health outcomes. We examined the extent to which quantitative measures of gait and balance abilities were associated with total daily physical activity, controlling for a variety of potential covariates.
Methods
Participants (n = 608) were older adults participating in the Rush Memory and Aging Project, a community-based cohort study of aging. Objective measures of total daily physical activity were derived from a wearable device. Gait and balance abilities were objectively quantified using a body-fixed sensor. We also collected measures of other motor functions, cognitive and psychosocial factors, and chronic health. We employed linear regression models to identify facets of mobility significantly associated with total daily physical activity, and tested for independence of these associations when all significant covariates were considered together in a final model.
Results
Three gait and balance measures were independently associated with total daily physical activity (p < .01), together accounting for approximately 16% of its variance. Other motor measures, cognitive and psychosocial factors, and chronic health accounted for 8.8%, 4.9%, and 6.4% of the variance, respectively, when considered in isolation. Considered together in a single model, all significant covariates accounted for approximately 21% of the variance in physical activity.
Conclusions
Gait and balance measures from a body-fixed sensor are strongly associated with objectively measured total daily physical activity in older adults. However, given the importance of physical activity to many health outcomes, further work is needed to more completely characterize the factors that may influence physical activity.
Keywords: Actigraphy, Mobility, Motor, Inertial sensors
Physical activity is a modifiable behavior with a wide range of potential health benefits (1). Therefore, public health efforts have focused on promoting a more active lifestyle or, alternatively, reducing sedentariness as a means of improving the health of older adults (2). Traditionally, community-based studies have relied on self-report, questionnaire-derived measures of physical activity (3). In recent years, however, technologic advances have led to the availability of unobtrusive, wearable devices that can capture movement continuously over the course of several days by means of a small accelerometer, thereby yielding a measure of total daily physical activity that is free from recall bias and other sources of subjectivity (4). Previous work has shown that measures of total daily physical activity from these devices are associated with important health-related outcomes such as mortality (5), incident disability (6), cognitive decline (7), mild cognitive impairment (8), and incident Alzheimer’s disease (7).
Continuous recordings of total daily physical activity include contributions from both exercise and nonexercise movements that are dependent on a wide range of motor abilities, especially the ability to ambulate. Therefore, poor gait and balance abilities that degrade or limit the capacity to move (ie, mobility limitations) are likely to be important determinants of total daily physical activity, the extent to which older adults actually move in their everyday environment. In prior work in this cohort, we found that a body-fixed sensor comprising small electronic accelerometers and gyroscopes can be used to quantify diverse facets of mobility in the community setting (9). These novel measurements complement traditional timed gait performance measures and allow clinicians and investigators to assess a wider range of gait and balance abilities without additional testing burden for participants. However, the extent to which the quantified gait and balance abilities are independently associated with an actigraphic measure of total daily physical activity is unknown.
This study examines the extent to which quantitative measures of gait and balance are associated with total daily physical activity, controlling for a wide range of clinical covariates that may potentially affect physical activity level. We quantified total daily physical activity in 608 nondemented, community-dwelling older individuals from recordings made with an omnidirectional accelerometer (Actical; Mini Mitter, Bend, OR) worn on the wrist continuously for up to ten days. Gait and balance abilities were quantified from recordings obtained during structured mobility testing in the community setting using a second device, a body-fixed sensor (DynaPort Hybrid, McRoberts B.V.). Additional covariates collected during the same testing cycle included traditional motor performance measures as well as non-motor features, namely cognitive factors and chronic health. Via a series of regression models and employing variable selection techniques, we identified the gait and balance measures that were associated with total daily physical activity, independent of a diverse range of other clinical covariates. We also quantified the portion of cross-sectional variance in total daily physical activity accounted for by these gait and balance measures as well as the clinical covariates.
Methods
Participants
Participants were from the Rush Memory and Aging Project (MAP), an ongoing longitudinal clinical-pathological study of aging that began in 1997 (10). MAP participants provide informed consent at enrollment, and the study is administered in accordance with the Declaration of Helsinki and the protocols approved by the Institutional Review Board of Rush University Medical Center. While collection of actigraphic physical activity recordings began in 2005, instrumentation of the annual mobility testing with a body-fixed sensor occurred later, in 2011. At the time of these analyses, there were 608 participants with valid actigraphic and instrumented mobility recordings available from the same testing cycle.
Total Daily Physical Activity
Participants wore the actigraphy device on the nondominant wrist continuously for up to 10 days. The mean activity count for each 15-second epoch was written to the device’s onboard memory. Mean total daily physical activity was computed based on all available full days of recording as described in the Supplementary Methods and in prior publications (7).
Body-fixed Sensor Gait and Balance Quantification
During an instrumented gait and balance testing protocol, additional details of which can be found in the Supplementary Methods, participants who could ambulate independently wore a body-fixed sensor (DynaPort) positioned on the lower back. The sensor records acceleration along and rotation rate around each of three orthogonal axes at 100 samples per second. Further details of the pipeline through which gait data are collected and ultimately integrated with available clinical data are conveyed in Supplementary Figure S1. The current study analyzed gait and balance metrics derived from recordings of three tests: a 32-foot walk, the Timed Up and Go (TUG), and a 20-second period of standing with eyes closed. Measures derived from these recordings (see Supplementary Table S1 for raw measures) were summarized into scores representing five different mobility subtasks as described in a prior publication (9).
Other Covariates
Three additional groups of covariates that have the potential to confound the associations of motor abilities with total daily physical activity by degrading motor capacity or affecting an individual’s propensity to engage in physical activity were examined in these analyses. These included: (i) other nongait motor measures, (ii) cognitive and psychosocial factors, and (iii) chronic health status. Supplementary Table S2 provides a list of the covariates included in these three categories. A description of the methods by which they are collected and computed is included in the Supplementary Methods.
Statistical Analyses
All analyses were carried out using SAS/STAT software, version 9.3 (SAS Institute Inc., Cary, NC). We assessed correlations among the 13 device-derived gait and balance scores using Pearson’s r presented as a graphical heat map. We then performed 13 separate linear regressions, with each gait score taking on the role of explanatory variable of interest and age- and sex-adjusted total daily physical activity as the outcome. For each of the five mobility subtasks contained within the three main tasks (ie, walking, transitioning from sitting to standing, turning 180 degrees, transitioning from standing to sitting, and standing with eyes closed), the scores for which p was less than .05 were entered in a backward elimination routine, which proceeded until all remaining terms had p less than .1. We then extracted a summary score for each subtask by calculating each participant’s expected value of total daily physical activity based on the estimated model parameters. These summary subtask scores were entered together in a combined regression model along with traditional timed measures of mobility performances, and elimination proceeded until all terms had p less than .1. In this way, we identified the gait and balance abilities and their constituent measures that were independently associated with total daily physical activity and quantified the percentage of its cross-sectional variation for which they accounted.
We employed the same approach to examine the relation of three additional categories of covariates to total daily physical activity. Briefly, after computing correlations among all variables, we performed backward elimination within each subcategory of covariates and computed a summary score for the subcategory based on its remaining terms. Summary scores within the same overarching category were subjected to another backward elimination step to identify those scores that were independently associated with total daily physical activity. We then carried out a series of regression models to determine whether the associations of gait and balance scores with total daily physical activity were attenuated after controlling for the three categories of clinical covariates.
In analyses involving many covariates, as in the current work, there exists potential for genuine associations to be obscured due to, for example, instability in the results of the backward elimination of variables. Such a problem may stem from the a priori categorization of variables as well as the deterministic order of their removal from the models. To guard against this and further validate key findings, we repeated the analyses using an alternative variable selection approach, a penalized likelihood technique with a smoothly clipped absolute deviation (SCAD) penalty, which in comparison to traditional variable selection methods has advantages such as unbiasedness, sparsity, and continuity (11). In addition, SCAD accomplishes simultaneous rather than stepwise variable selection and parameter estimation, thereby easing the multiple testing burden that might have inflated the family-wise error rate in the backward elimination approach.
Results
Metric Properties of Total Daily Physical Activity
As shown in Table 1, the mean value of total daily physical activity after adjustment for age and sex was about 3.5 counts/day (×105), with a range of 1.2–7.0 and lower and upper quartiles at 2.9 and 4.0, based on an average of 9.6 days of actigraphy recordings (SD = 1.3). The mean total daily physical activity was slightly higher than in previous studies in the same cohort (6,12,13) due to the exclusion of individuals who were unable to complete the structured mobility exam. Total daily physical activity was lower with increasing age (0.022-unit decrease per year, F1,606 = 125.3, R2 = .17, p < .0001) and was higher in females (0.09 unit difference, t606 = 2.47, p = .014). Correlations among total daily physical activity and gait and balance abilities as well as other covariates are illustrated in Supplementary Figure S2.
Table 1.
Demographic, Actigraphic, and Gait/Balance Characteristics of the Sample (n = 608)
| Variable | Mean (SD) or N (%) |
|---|---|
| Demographics | |
| Age (years) | 82.1 (7.5) |
| Sex (females) | 470 (77.3%) |
| Education (years) | 15.3 (2.9) |
| Activity | |
| Total Daily Physical Activity (105 counts/day) | 3.50 (0.91) |
| Gait and Balance (z-scores) | |
| Walking | |
| Speed | 0.26 (0.97) |
| Cadence | 0.11 (0.97) |
| Stride Variability | −0.21 (0.96) |
| Regularity | 0.01 (0.54) |
| Sit-to-Stand Transition (S1) | |
| Anterior-Posterior | −0.10 (1.01) |
| Range | −0.02 (0.28) |
| Posterior | 0.15 (1.07) |
| Stand-to-Sit Transition (S2) | |
| Jerk | 0.12 (0.88) |
| Range | 0.26 (0.84) |
| Median | 0.08 (1.09) |
| Turn 180° | |
| Yaw | −0.02 (0.66) |
| Frequency | −0.33 (0.92) |
| Standing Posture (Eyes Closed) | |
| Sway | −0.12 (0.97) |
Gait and Balance Abilities and Total Daily Physical Activity
Descriptive statistics for 13 measures of gait and balance ability derived from the body-fixed sensor recordings appear in Table 1. As shown in Table 2, nine of these gait and balance scores were associated with total daily physical activity (p < .05) when considered individually. Of these, six scores spanning four of the five mobility subtasks remained in the model after backward elimination within the subtasks (Table 2). The final model retained the summary scores for the walking, sit-to-stand transition, and 180-degree turn subtasks, which together accounted for about 16% of the variation in the age- and sex-adjusted total daily physical activity (Table 2).
Table 2.
Association of Individual and Summary Gait and Balance Scores with Total Daily Physical Activity
| Gait and Balance Mobility Subtasks and Scores | Stage 1: Associations of Gait and Balance Measures with Physical Activity | Stage 2: Associations of Subtask Summary Scores with Physical Activity | ||
|---|---|---|---|---|
| Individual Associations β (SE, p value) | After Backward Elimination within Subtasks β (SE, p value) | Initial Combined Model β (SE, p value) | Final Model after Backward Elimination β (SE, p value) | |
| Walking | 0.635 (0.131, <.0001) | 0.637 (0.129, <.0001) | ||
| Speed | 0.372 (0.038, <.0001) | 0.372 (0.038, <.0001) | ||
| Cadence | −0.017 (0.037, .64) | - | ||
| Stride Variability | −0.117 (0.037, .0018) | - | ||
| Regularity | 0.187 (0.038, <.0001) | - | ||
| Sit-to-Stand Transition (S1) | 0.437 (0.164, .0081) | 0.440 (0.160, .0061) | ||
| Anterior-Posterior | −0.170 (0.037, <.0001) | −0.074 (0.041, .074) | ||
| Range | 0.053 (0.037, .16) | - | ||
| Posterior | 0.261 (0.037, <.0001) | 0.227 (0.042, <.0001) | ||
| Turn 180° | 0.408 (0.151, .0073) | 0.411 (0.149, .0060) | ||
| Yaw | 0.304 (0.040, <.0001) | 0.311 (0.039, <.0001) | ||
| Frequency | −0.117 (0.038, .0020) | −0.134 (0.036, .0002) | ||
| Stand-to-Sit Transition (S2) | 0.019 (0.214, .93) | - | ||
| Jerk | 0.193 (0.037, <.0001) | 0.193 (0.037, <.0001) | ||
| Range | 0.105 (0.037, .0047) | - | ||
| Median | 0.012 (0.037, .76) | - | ||
| Standing Posture (Eyes Closed) | - | - | ||
| Sway | 0.041 (0.037, .272) | - | ||
| Adjusted R-Squared | .159 | .159 | ||
Note: Stage 1 relates to backward elimination of individual gait scores within each subtask. Stage 2 relates to the backward elimination of subtask summary scores in a combined model.
Other Covariates and Total Daily Physical Activity
Descriptive statistics for additional covariates included in the analyses are given in Supplementary Table S2. Covariates associated with total daily physical activity were identified within all three categories, and the within-category backward elimination of summary scores for those subcategories is presented in Supplementary Table S3. Within the category of other motor-related factors, parkinsonian signs and body composition retained significant association with total daily physical activity and accounted for about 9% of its variance when considered in isolation from other factors. Within the category of cognitive and psychosocial factors, self-reported engagement in social and physical activities accounted for about 5% of the variance. Within the chronic health category, medical conditions and lab measures accounted for about 6% of the variance.
Gait and Balance Abilities, Other Covariates, and Total Daily Physical Activity
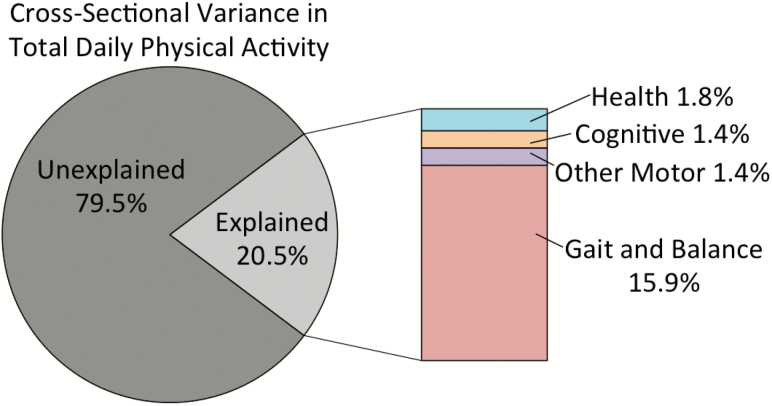
We carried out a final series of linear regression models designed to clarify the relative association of each subtask’s or subcategory’s summary score with total daily physical activity. The base model included summary scores for the three gait and balance motor subtasks that remained after the backward elimination routine (walking, sit-to-stand transition, 180-degree turn), which together accounted for about 16% of the variance in total daily physical activity, as shown in Table 3. The addition of parkinsonian signs and body composition (other motor category) increased the explained variance of total daily physical activity by 1.4%. Next, we added the summary score for self-reported participation in social and physical activities (cognitive and psychosocial factors), which accounted for an additional 1.4%. Finally, we included summary scores for chronic medical conditions and lab measures (chronic health), which explained an additional 1.8 percentage points, for a total of more than 20% of the variance of total daily physical activity, as illustrated in Figure 1. Gait and balance summary scores remained associated with total daily physical activity after controlling for all three additional categories of covariates.
Table 3.
Joint Contributions of Gait/Balance Abilities and Other Covariates to Variance in Total Daily Physical Activity
| Performance or Category | Subtask or Subcategory | Model A β (SE, p value) | Model B β (SE, p value) | Model C β (SE, p value) | Model D β (SE, p value) |
|---|---|---|---|---|---|
| Gait and Balance | Walking | 0.637 (0.129, <.0001) | 0.584 (0.140, <.0001) | 0.534 (0.139, .0001) | 0.519 (0.136, .0002) |
| Sit-to-Stand (S1) | 0.440 (0.160, .0061) | 0.421 (0.177, .018) | 0.383 (0.175, .029) | 0.297 (0.174, .088) | |
| Turn 180° | 0.411 (0.149, .0060) | 0.315 (0.162, .052) | 0.320 (0.160, .046) | 0.335 (0.157, .034) | |
| Other Motor | Parkinsonian Signs | 0.397 (0.171, .021) | 0.282 (0.172, .10) | 0.255 (0.171, .14) | |
| Body Composition | 0.348 (0.313, .266) | 0.335 (0.310, .28) | 0.177 (0.310, .57) | ||
| Cognitive Resources | Late-Life Participation in Activities | 0.584 (0.180, .0012) | 0.419 (0.178, .019) | ||
| Chronic Health | Medical Conditions | 0.488 (0.204, .017) | |||
| Laboratory Measures | 0.551 (0.234, .019) | ||||
| Adjusted R-Squared | .159 | .173 | .187 | .205 | |
| R-Squared Increase from Preceding Model | - | .014 | .014 | .018 | |
| R-Squared Increase from Model A | - | .014 | .028 | .046 |
Figure 1.
The majority of the variance in total daily physical activity was unexplained by variables included in these analyses. Of the explained variance, most was accounted for by measures of gait and balance abilities, while smaller portions were accounted for by three other categories of variables.
In further analyses, we examined whether the association between objective gait and balance metrics and total daily physical activity differed in participants who reported low levels of exercise-related activity compared to those who reported high levels. We stratified participants based on their self-reported time spent per week engaging in five specific types of exercise-related activities (see Supplementary Methods). Gait and balance metrics accounted for 33.0% of the variance of total daily physical activity in the lowest quintile of self-reported activity, versus 10.3% in the highest quintile.
Alternative Variable Selection Method
We employed an alternative statistical technique, SCAD, to further validate key findings. As shown in Supplementary Table S4, the final model according to SCAD included gait and balance scores from the same three mobility subtasks as in the backward elimination approach. SCAD also identified parkinsonian gait as a relatively strong correlate of total daily activity, in agreement with results of the backward elimination strategy. Within the category of cognitive factors, SCAD and backward elimination both identified late life participation in physical activities as a contributor to total daily physical activity. Only within the chronic health category did the results of the SCAD technique substantially diverge from the backward elimination results.
Discussion
In the current work, we examined the extent to which quantitative measures of gait and balance were associated with an objective measure of total daily physical activity in more than 600 older adults. Gait and balance abilities quantified using a body-fixed sensor worn during structured mobility testing accounted for 16% of the total variation in total daily physical activity. A wide range of diverse covariates including other motor abilities, cognitive factors and resources, and chronic health conditions and laboratory measures were independently associated with total daily physical activity and accounted for an additional 5% of its variation when considered in the same model with measures of gait and balance. Thus, gait and balance accounted for the largest portion of explained variance in total daily physical activity. Nonetheless, most of the variance remained unexplained. Further work is needed to explicate the potentially complex relation of other biologic, psychosocial, and environmental factors underlying total daily physical activity, which may be leveraged to promote higher levels of physical activity in community-dwelling older adults.
A growing literature implicates the total daily physical activity metric as an important correlate—and in many cases a likely determinant—of a variety of health outcomes that impact heavily on successful aging, including mortality (5), incident disability (14), cognition (15) and cognitive decline, and incident Alzheimer’s disease (7). Walking is a prominent feature of mobility related to many of the exercise and non-exercise movements encompassed by measures of physical activity. Studies have revealed an association of walking speed, one of the most salient and easily measured parameters of gait, with self-reported habitual physical activity level in late life (16,17), consistent with raw correlations observed in the current work (Supplementary Figure S2). Activity monitors employed for prolonged recordings demonstrated stronger association of physical activity level with gait speed and other facets of mobility derived from timed tests (18). Now, technologic advances permit more detailed assessment of mobility beyond measurement of gait speed in the community setting. A recent study employing instrumented gait testing reported on the associations that physical activity has with variability in step length and stance time (19), which may not be visually discernible to trained research personnel. Overall, however, there are few data to elucidate the joint contributions of speed and other facets of mobility with objective measures of total daily physical activity. Instrumented gait and balance testing for enhanced quantification of these abilities represents a promising avenue for expanding this area of research.
In the current work, diverse gait and balance measures showed differential associations with total daily physical activity. These findings have potential to be of particular importance in efforts to individualize interventions for complex phenotypes such as physical activity in older adults. The summary score for speed remained the only measure from the walking subtask that was independently associated with total daily physical activity. Outside of the walking subtask, the sit-to-stand transition (S1) of the TUG performance, specifically the rate at which participants gathered forward momentum during S1, was also associated with total daily physical activity. Those who accelerated forward more rapidly tended to be more physically active. In this regard, the association of the S1 transition with total daily physical activity dovetails with the idea that the ease with which an individual rises from a chair effectively summarizes motor abilities including planning, balance, and lower extremity strength, which also influence physical activity level. The 180-degree turning subtask was also associated with total daily physical activity. Individuals who turned more rapidly, but with less frequent (and therefore fewer) steps were more likely to have higher levels of total daily physical activity. The opposite pattern of turning (slower turning with more steps) resembles that observed in association with Parkinson’s disease, representing one plausible pathway by which poorer performance in the 180-degree turn subtask could be linked to lower levels of total daily physical activity (20).
An important finding in this study was that body-fixed sensory mobility metrics accounted for about 16% of the variance of total daily physical activity. The modest association of these metrics suggests that they may measure separate but related constructs (21). Instrumented gait testing provides a snapshot of diverse gait and balance abilities that underlie an individual’s capacity to move during a short structured mobility testing session. Conversely, total daily physical activity was derived from continuous actigraphic recordings and conveys the extent to which an individual actually moved over the course of several days. Since physical activity is a volitional behavior, an individual with above average mobility capacity might nonetheless choose to sit on a couch or remain in bed, leading to a low value for total daily physical activity. Alternatively, an individual in a supportive environment might find ways to remain physically active despite poor gait and balance capacity. These results underscore the complexity of late-life motor impairment and the importance of developing strategies to improve both motor capacity and motor function. The availability of unobtrusive devices that measure both motor capacity and function in the same individual has potential to facilitate investigations that could help to elucidate the extent to which these distinct constructs differ and may be amenable to targeted interventions.
Quantitative mobility measures were independently associated with total daily physical activity when controlling for a wide range of clinical covariates thought to potentially influence physical activity. When considered together in a single model, these non-gait clinical covariates explained an additional 5% of the variation in total daily physical activity. While this percentage may seem small, converging evidence from recent genetic and autopsy studies underscores that complex clinical phenotypes are not driven by single genes or pathologies. Even when a significant association is identified, single factors may only account for a small percentage of the phenotype’s variance (22,23). Thus, at a population level, the explanation of 5% of the variation of a complex construct such as total daily physical activity is an important finding.
Nonetheless, despite considering quantitative mobility metrics and many common clinical covariates, the majority of the variance of total daily physical activity remained unexplained. Since physical activity is a complex construct that depends on multiple physiologic systems (24), had we employed analogously detailed metrics for cardiopulmonary function, bioenergetics (25), body composition (26), and musculoskeletal function (27), we might have accounted for a larger proportion of the variance of total daily physical activity. Several other important factors were not accounted for in the current work and could more fully characterize the keys to a physically active lifestyle in later life. For example, sleep quantity and quality, recognized as important influences on cognitive performance (28), might also contribute to variation in motor performances and physical activity level (29). Pain is another likely factor that may reduce total daily physical activity in older adults with otherwise good gait abilities (30). The volitional hurdle to be physically active in daily life may also be profoundly affected by environmental factors. For instance, the “walkability” of the local environment (31) and sources of social support (32) may raise or lower barriers to physical activity in the community setting. Further work is needed to integrate measures such as sleep, pain, and barriers to physical activity in future investigations of total daily physical activity.
This study has strengths as well as certain limitations. First, we designed analyses of the current study with the total daily physical activity metric serving as the outcome, taking the simplified viewpoint that activity level is the output of a multitude of biologic systems and factors, each of which might be intervened upon to counteract late life declines in physical activity level. In actuality, reverse or circular causality must also be considered and may in fact figure prominently in the associations of total daily physical activity with several of the gait and nongait factors included in the current work (33,34). Given that our data were cross-sectional and originated from a selected observational cohort, our results need to be replicated in more diverse cohorts, and future longitudinal studies will be necessary to provide an empiric approach to disentangling direction of causality. Moreover, as suggested by results of the stratified analysis, it will be important to determine whether associations between mobility metrics and total daily physical activity identified in the current cohort vary between sedentary and more active older adults. A notable strength of the current study is the wide range of covariates included in the analyses and the relatively large number of well-characterized subjects. Despite this wealth of data, most of the variation in total daily physical activity went unaccounted for, an apparent reflection of the complexity of the activity construct. A corresponding opportunity exists for future work to quantify and examine additional dimensions of gait and balance, as well as biologic, psychosocial, motivational, and environmental factors that may contribute to total daily physical activity and, conversely, to sedentariness.
In conclusion, the current work extends the growing efforts to leverage available technology to quantify mobility and physical activity among older adults. The feasibility of employing instrumented mobility testing with an unobtrusive body-fixed sensor in a large number of older adults in the community-setting lends support to the notion that similar techniques could one day be used to quickly and easily assess mobility outside of specialized labs or via telemedicine. This study also provides evidence that combinations of devices can be employed in the same individuals to capture both motor capacity as well as the extent to which individuals actually move in their everyday environment. This emphasizes that distinct risk factors and targeted interventions may be necessary to improve both aspects of physical function in older adults. Finally, our results underscore the complexity of total daily physical activity and the need for further studies to more fully elucidate its underlying biology to guide public health efforts to reduce sedentariness and increase physical activity in older adults.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences online.
Funding
This work was supported by the National Institute on Aging (R01 AG22018, R01 AG17917, R01 AG443379, R01 AG47976, R01 AG052488); the National Institute of Neurological Disorders and Stroke (R01 NS78009); and the Illinois Department of Public Health.
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
We are grateful to the participants of the Rush Memory and Aging Project and faculty and staff of the Rush Alzheimer’s Disease Center. More information regarding obtaining MAP data for research use can be found at the RADC Research Resource Sharing Hub (www.radc.rush.edu).
References
- 1. Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health. 2013;13:813. doi:10.1186/1471-2458-13-813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Haskell WL, Lee IM, Pate RR et al. ; American College of Sports Medicine; American Heart Association Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi:10.1161/CIRCULATIONAHA.107.185649 [DOI] [PubMed] [Google Scholar]
- 3. Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi:10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Murphy SL. Review of physical activity measurement using accelerometers in older adults: considerations for research design and conduct. Prev Med. 2009;48:108–114. doi:10.1016/j.ypmed.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buchman AS, Yu L, Boyle PA, Shah RC, Bennett DA. Total daily physical activity and longevity in old age. Arch Intern Med. 2012;172:444–446. doi:10.1001/archinternmed.2011.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shah RC, Buchman AS, Leurgans S, Boyle PA, Bennett DA. Association of total daily physical activity with disability in community-dwelling older persons: a prospective cohort study. BMC Geriatr. 2012;12:63. doi:10.1186/1471-2318-12-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buchman AS, Boyle PA, Yu L, Shah RC, Wilson RS, Bennett DA. Total daily physical activity and the risk of AD and cognitive decline in older adults. Neurology. 2012;78:1323–1329. doi:10.1212/WNL.0b013e3182535d35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Middleton LE, Manini TM, Simonsick EM et al. Activity energy expenditure and incident cognitive impairment in older adults. Arch Intern Med. 2011;171:1251–1257. doi:10.1001/archinternmed.2011.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buchman AS, Leurgans SE, Weiss A et al. Associations between quantitative mobility measures derived from components of conventional mobility testing and Parkinsonian gait in older adults. PLoS One. 2014;9:e86262. doi:10.1371/journal.pone.0086262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bennett DA, Schneider JA, Buchman AS, Barnes LL, Boyle PA, Wilson RS. Overview and findings from the rush Memory and Aging Project. Curr Alzheimer Res. 2012;9:646–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fan J, Li R. Variable selection via nonconcave penalized likelihood and its oracle properties. J Am Stat Assoc. 2001;96:1348–1360. [Google Scholar]
- 12. James BD, Boyle PA, Bennett DA, Buchman AS. Total daily activity measured with actigraphy and motor function in community-dwelling older persons with and without dementia. Alzheimer Dis Assoc Disord. 2012;26:238–245. doi:10.1097/WAD.0b013e31822fc3cb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Buchman AS, Wilson RS, Yu L, James BD, Boyle PA, Bennett DA. Total daily activity declines more rapidly with increasing age in older adults. Arch Gerontol Geriatr. 2014;58:74–79. doi:10.1016/j.archger.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shah RC, Wilson RS, Bienias JL, Arvanitakis Z, Evans DA, Bennett DA. Relation of blood pressure to risk of incident Alzheimer’s disease and change in global cognitive function in older persons. Neuroepidemiology. 2006;26:30–36. doi:10.1159/000089235 [DOI] [PubMed] [Google Scholar]
- 15. Buchman AS, Wilson RS, Bennett DA. Total daily activity is associated with cognition in older persons. Am J Geriatr Psychiatry. 2008;16:697–701. [DOI] [PubMed] [Google Scholar]
- 16. Busch Tde A, Duarte YA, Pires Nunes D et al. Factors associated with lower gait speed among the elderly living in a developing country: a cross-sectional population-based study. BMC Geriatr. 2015;15:35. doi:10.1186/s12877-015-0031-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Talkowski JB, Brach JS, Studenski S, Newman AB. Impact of health perception, balance perception, fall history, balance performance, and gait speed on walking activity in older adults. Phys Ther. 2008;88:1474–1481. doi:10.2522/ptj.20080036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morie M, Reid KF, Miciek R et al. Habitual physical activity levels are associated with performance in measures of physical function and mobility in older men. J Am Geriatr Soc. 2010;58:1727–1733. doi:10.1111/j.1532-5415.2010.03012.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brach JS, Perera S, Studenski S, Newman AB. The reliability and validity of measures of gait variability in community-dwelling older adults. Arch Phys Med Rehabil. 2008;89:2293–2296. doi:10.1016/j.apmr.2008.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stack E, Ashburn A. Dysfunctional turning in Parkinson’s disease. Disabil Rehabil. 2008;30:1222–1229. doi:10.1080/09638280701829938 [DOI] [PubMed] [Google Scholar]
- 21. van Lummel RC, Walgaard S, Pijnappels M et al. Physical performance and physical activity in older adults: associated but separate domains of physical function in old age. PLoS One. 2015;10:e0144048. doi:10.1371/journal.pone.0144048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Buchman AS, Yu L, Boyle PA et al. Microvascular brain pathology and late-life motor impairment. Neurology. 2013;80:712–718. doi:10.1212/WNL.0b013e3182825116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Buchman AS, Yu L, Boyle PA, Schneider JA, De Jager PL, Bennett DA. Higher brain BDNF gene expression is associated with slower cognitive decline in older adults. Neurology. 2016;86:735–741. doi:10.1212/WNL.0000000000002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34:1996–2001. doi:10.1249/01.MSS.0000038974.76900.92 [DOI] [PubMed] [Google Scholar]
- 25. Wert DM, Brach JS, Perera S, VanSwearingen J. The association between energy cost of walking and physical function in older adults. Arch Gerontol Geriatr. 2013;57:198–203. doi:10.1016/j.archger.2013.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goodpaster BH, Park SW, Harris TB et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–1064. [DOI] [PubMed] [Google Scholar]
- 27. Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Rheum. 2003;49:129–135. doi:10.1002/art.10911 [DOI] [PubMed] [Google Scholar]
- 28. Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci. 2015;10:97–137. doi:10.1177/1745691614556680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tang NK, Sanborn AN. Better quality sleep promotes daytime physical activity in patients with chronic pain? A multilevel analysis of the within-person relationship. PLoS One. 2014;9:e92158. doi:10.1371/journal.pone.0092158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cohen-Mansfield J, Marx MS, Guralnik JM. Motivators and barriers to exercise in an older community-dwelling population. J Aging Phys Act. 2003;11:242–253. [Google Scholar]
- 31. Van Holle V, Van Cauwenberg J, Gheysen F et al. The association between belgian older adults’ physical functioning and physical activity: what is the moderating role of the physical environment?PLoS One. 2016;11:e0148398. doi:10.1371/journal.pone.0148398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Prev Med. 2003;37:110–118. [DOI] [PubMed] [Google Scholar]
- 33. Brach JS, FitzGerald S, Newman AB et al. Physical activity and functional status in community-dwelling older women: a 14-year prospective study. Arch Intern Med. 2003;163:2565–2571. doi:10.1001/archinte.163.21.2565 [DOI] [PubMed] [Google Scholar]
- 34. Leblanc A, Pescatello LS, Taylor BA et al. Relationships between physical activity and muscular strength among healthy adults across the lifespan. Springerplus. 2015;4:557. doi:10.1186/s40064-015-1357-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.