Abstract
Background
Structured physical activity interventions delay the onset of disability for at-risk older adults. However, it is not known if at-risk older adults continue to participate in physical activity or maintain mobility benefits after cessation of structured intervention.
Methods
One thousand six hundred and thirty-five sedentary men and women aged 70–89 years with Short Physical Performance Battery (SPPB) scores of 9 or less and able to walk 400 m were randomized to a structured, moderate-intensity physical activity (PA) program consisting of center-based (twice/week) and home-based (three to four times per week) aerobic, resistance, and flexibility training or a health education (HE) program combined with upper extremity stretching.
Results
Most of the participants (88% of HE and 87% of PA) returned for a follow-up visit (POST) 1 year after cessation of formal intervention. The HE group reported about 1-hour less activity per week than the PA group at end of intervention (LAST TRIAL; −68.9; 95% confidence interval [CI] = −86.5 to −51.3) but similar weekly activity at POST (−13.5; 95% CI = −29.5 to 2.47). SPPB did not differ between the two groups at LAST TRIAL (−0.06; 95% CI = −0.31 to 0.19) nor POST (−0.18; 95% CI = −0.45 to 0.088).
Conclusions
Although sedentary at-risk older adults increased their physical activity during a structured physical activity intervention, they did not continue at this level following the cessation of intervention. Future exercise interventions need to include novel methods to support older adults in continued physical activity following structured interventions.
Keywords: Exercise, Physical Function, Physical Activity
Older adults at risk for mobility disability experience improved functional outcomes, including delay of disability onset, with participation in a structured physical activity (PA) intervention (1). If the protective effects of a structured PA intervention persist following cessation, then implementing short-term PA interventions for at-risk older adults could be a cost-effective way to slow functional decline and decrease associated costs of care. However, it is unclear if these protective effects will persist after completion of the formal program. Cessation of physical activity slowly leads to a return of prior function; in frail older adults, it is not known how rapidly that decline occurs. If participants continue unstructured PA following an intervention, it is also not known if this is sufficient to slow or halt this decline. Furthermore, it is unclear if a long-term structured PA intervention will effect behavior change so that at-risk older adults will continue PA after cessation of the formal program. One recent study suggests that at-risk older adults do exhibit a functional improvement (trend toward higher function, as measured by Short Physical Performance Battery [SPPB] and gait speed) and a continued behavior change (greater time spent in PA) 2 years after completion of a PA intervention (2). Yet little other research into the long-term impact of PA interventions in at-risk older adults has been performed.
To better define the long-term impact of structured PA intervention on at-risk older adults, we used data from the main LIFE trial to evaluate if older adults at risk for mobility disability who participated in PA versus the health education (HE) intervention experienced continued functional behavioral change 1 year after completion of the intervention.
Methods
Trial Design and Participants
The methods, recruitment, intervention, and primary outcome for the LIFE study are detailed elsewhere (1,3,4). Briefly, the LIFE study was a 1,635-person multicenter single-blind randomized trial conducted between February 2010 and December 2013 at eight centers across the United States. The study protocol was approved by the institutional review board at all participating centers. The centers included suburban and urban communities (clinicaltrials.gov Identifier: NCT01072500).
Eligible participants were men and women aged 70–89 years who were sedentary (self-reported less than 20 min/wk of regular physical activity in the past month and less than 125 min/wk of moderate-intensity physical activity) and at high risk of mobility disability (SPPB score of 9 or less). Participants had to be able to walk 400 m in less than 15 minutes, could not use a walker, were not allowed to sit or receive help from another person during the test, had to be cognitively intact (Modified Mini-Mental State Examination score > 1.5 SD below education- and race-specific norms), and able to safely participate in the intervention. Final assessments were obtained in 2013 during the active intervention phase, between August and December of that year. All participants who were not deceased or lost to follow-up were approached to return for a post-trial visit (POST; between June and November 2014) scheduled approximately 1 year following their last scheduled assessment.
Intervention
Participants were randomized at baseline into a PA or an HE program (3). The PA intervention was focused on aerobic activity (walking) and also included strength, flexibility, and balance training. Participants attended two center-based sessions per week and were encouraged to perform home-based activity three to four times per week throughout the study. PA center-based sessions progressed to a goal of 30 minutes of walking at a moderate intensity, 10 minutes of lower extremity strength training (with ankle weights), and 10 minutes of balance training and large muscle flexibility exercises.
The HE program involved meeting weekly for the first 26 weeks and thereafter the meetings were offered twice monthly, with participants expected to attend at least once per month. The meetings addressed a variety of topics of interest to older adults, including travel safety, age-appropriate preventive services, legal and financial issues, and nutrition. Each session included 5–10 minutes of instructor-led gentle upper extremity stretching exercises. Both interventions ceased in November 2013.
Baseline Screening
Baseline demographics and medical history were obtained by self-report. Baseline biometrics and functional data obtained by study staff included body mass index, SPPB scores, and activity levels assessed with the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire to ensure that the participant met the entrance criteria (3). The SPPB is a three-part measure of lower extremity function including a static balance test, a 4-m walk at usual speed, and five timed repeated chair stands, each scored 0–4 and then summed with 0 indicating the worst performance and 12 the best (5). CHAMPS is a 41-item questionnaire of self-reported PA specifically designed for older adults, which is measured in minutes per week (6). For our analyses, we used a subset of the five items that focus on walking and weight training activities, referred to as the CHAMPS-5.
Outcomes
Participants were evaluated at baseline and every 6 months throughout the study. This article focuses on measurements obtained at baseline, during the final assessment visits following completion of the intervention (termed the “LAST TRIAL” measure from this point forward), and the measurements obtained during the postintervention visit (termed “POST” measure from this point forward), which was scheduled to be approximately 1 year following their LAST TRIAL visit. The primary outcomes for this analysis were the SPPB and gait speed obtained during the 400-m walk. At clinical assessments, participants were asked to complete both the SPPB and the 400-m usual paced walk. During the 400-m walk, participants were allowed to use a cane and rest for up to 1 minute due to fatigue. If a participant was unable to complete 400 m within 15 minutes, then gait speed was determined by dividing the distance actually walked by the elapsed time prior to stopping.
Statistical Considerations
Baseline demographic and health characteristics were summarized with means, SD, counts, and percentages by intervention group and the presence of a POST visit. Logistic regression was used to explore whether the presence of a POST measure was associated with the baseline characteristic, the intervention effect, and the interaction between these factors. Unadjusted means (SD) of both physical function (SPPB and gait speed) and minutes per week of five walking and weight training activities (CHAMPS) were calculated at each visit (baseline, LAST TRIAL, and POST) and changes between baseline to the POST, and the LAST TRIAL to the POST visit are also presented.
Comparisons of function and PA measures between intervention groups were made using constrained mixed-model repeated measures analysis of covariance with an unstructured covariance matrix to account for the fact that the multiple measurements (at baseline, LAST TRIAL, POST) from participants were not independent. The models contained terms for sex and clinical site (both used to stratify randomization) and intervention effects that were specific to each follow-up visit. For randomized trials, constrained mixed models can make use of observations with only baseline measurements and can provide more efficient estimates of postrandomization treatment differences when either baseline or postrandomization measures are missing (7,8). In addition, they are consistent with intent-to-treat, account for outcomes being missing at random, and can provide the same estimates of the intervention effect as mixed models analysis of covariance when complete data on outcomes are obtained. Contrasts were used to test the effect of the intervention at each visit. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). In additional supplemental analyses, similar models were used to analyze the subcomponents of the SPPB, in addition to 4-m gait speed.
To evaluate the effect of the intervention on continuous measures of SPPB and gait speed within subgroups of baseline function, the intervention groups were further subdivided into high and low for both baseline SPPB (low: ≤7 and high: 8–9) and baseline gait speed (low: <0.8 m/s; high: ≥0.8 m/s). Subgroups effects were evaluated by adding terms for the baseline subgroups and associated interactions into the above mixed models, using contrasts to evaluate for homogeneity of the intervention effects at each visit among levels of the baseline subgroups.
In addition to estimating change in SPPB on its original scale, change in SPPB from baseline to the LAST TRIAL visit and the LAST TRIAL visit to the POST were categorized into three group: (a) improved (>1 unit increase), (b) no to minimal change (≤1 unit change), and (c) decline (>1 unit decrease in SPPB), and intervention differences were evaluated using chi-square tests. Because analyses of these categorized outcomes are not intent-to-treat (ie, some participants have missing follow-up outcomes) and do not account for missing at random data, we used multiple imputation under two different sensitivity analysis assumptions to determine how robust the conclusions were to missing outcomes. These assumptions consisted of (a) sequentially imputing missing observations at each visit into the three categories based on ordinal logistic regression models that included clinical site, gender, age, and prior observed SPPB values and (b) adding the intervention term and the intervention by prior SPPB value interaction into the first imputation model. All analyses were carried out in SAS 9.4.
Results
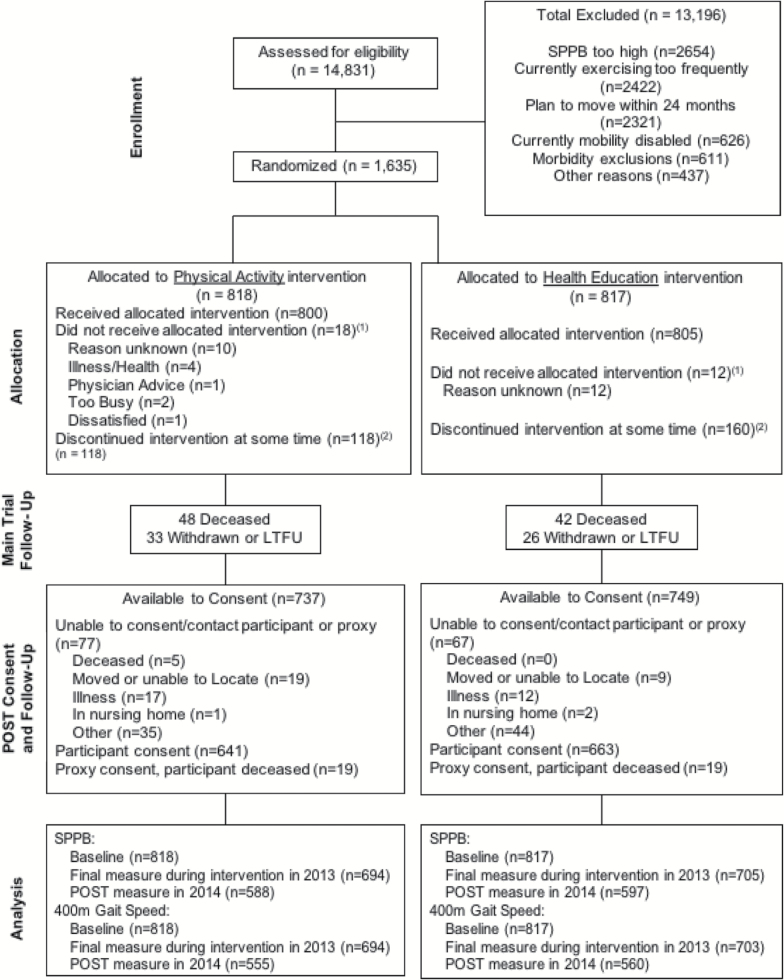
Following the end of the active intervention, 737 (90%) PA and 749 (92%) HE participants were available to consent for the POST visit. Consent was obtained from 641 (87%) PA and 663 (88%) HE participants. Main reasons for inability to consent are provided in the CONSORT diagram (Figure 1). The outcome measures obtained at the POST visit were, on average, 3.6 years postrandomization in both intervention groups and 1.05 years after the LAST TRIAL assessment. Based on the tests of interaction (Table 1), we could not conclude that the associations between baseline factors and the presence of a POST measure were different between intervention groups. Across intervention groups combined, those who returned were demographically similar at baseline from those who did not return for a POST; however, those who returned for the POST were healthier, with fewer baseline comorbidities, had higher SPPB scores, and faster 400-m walk gait speeds.
Figure 1.
Consort diagram of participants who had a POST versus those who did not.
Table 1.
Baseline Data With PA and HE Subdivided by POST and No POST
| Baseline Characteristics | Health Education | Physical Activity | p Values (for Prediction of POST Measure)a | ||||
|---|---|---|---|---|---|---|---|
| POST (n = 597) | No POST (n = 220) | POST (n = 590) | No POST (n = 228) | Baseline Characteristic | Intervention | Interaction | |
| Age (y); mean (SD) | 78.8 (5.2) | 79.8 (5.4) | 78.7 (5.1) | 78.7 (5.5) | .09 | .62 | .07 |
| Female N (%) | 134 (60.9) | 417 (69.8) | 153 (67.1) | 394 (66.8) | .10 | .68 | .08 |
| White N (%) | 172 (78.2) | 463 (77.6) | 176 (77.2) | 428 (72.5) | .28 | .66 | .38 |
| Height (cm); mean (SD) | 163.9 (9.5) | 165.0 (10.0) | 164.9 (9.9) | 164.1 (9.6) | .81 | .67 | .07 |
| Weight (kg); mean (SD) | 81.8 (19.0) | 82.3 (20.0) | 82.7 (18.4) | 79.7 (18.4) | .23 | .67 | .09 |
| BMI; mean (SD) | 30.3 (6.1) | 30.2 (6.6) | 30.3 (5.7) | 29.5 (5.8) | .14 | .69 | .31 |
| Education N (%) | .89 | .66 | .81 | ||||
| < High school | 16 (2.7) | 6 (2.7) | 16 (2.7) | 6 (2.6) | |||
| High School | 180 (30.2) | 61 (27.7) | 180 (30.5) | 69 (30.3) | |||
| College | 242 (40.5) | 96 (43.6) | 254 (43.1) | 91 (39.9) | |||
| Postgraduate | 156 (26.1) | 56 (25.5) | 137 (23.2) | 62 (27.2) | |||
| Other | 3 (0.5) | 1 (0.5) | 3 (0.5) | 0 (0.0) | |||
| Number of chronic conditions N (%)b | .006 | .68 | .91 | ||||
| 0 | 266 (44.6) | 90 (40.9) | 291 (49.3) | 110 (48.2) | |||
| 1 | 244 (40.9) | 88 (40.0) | 221 (37.5) | 75 (32.9) | |||
| 2 | 75 (12.6) | 31 (14.1) | 65 (11.0) | 30 (13.2) | |||
| 3–5 | 12 (2.0) | 11 (5.0) | 13 (2.2) | 13 (5.7) | |||
| Arthritis N (%) | 115 (19.3) | 50 (22.7) | 111 (18.8) | 42 (18.4) | .49 | .68 | .40 |
| Diabetes N (%) | 156 (26.3) | 60 (27.4) | 137 (23.3) | 62 (27.2) | .30 | .62 | .56 |
| Heart failure N (%) | 30 (5.0) | 15 (7.0) | 18 (3.1) | 8 (3.5) | .29 | .47 | .70 |
| Lung disease N (%) | 88 (14.8) | 35 (16.1) | 85 (14.5) | 45 (19.7) | .10 | .62 | .35 |
| Heart attack N (%) | 43 (7.2) | 26 (11.9) | 40 (6.8) | 20 (8.8) | .03 | .58 | .47 |
| SPPB score (total) | 7.3 (1.6) | 7.2 (1.7) | 7.5 (1.6) | 7.3 (1.7) | .04 | .61 | .81 |
| 400-m walk (m/s) | 0.83 (0.16) | 0.79 (0.17) | 0.84 (0.16) | 0.80 (0.17) | .05 | .61 | .95 |
Note: BMI = body mass index. Individuals were defined as having a POST visit if either an SPPB or a 400-m walk gait speed was obtained at a clinical assessment after stopping the LIFE intervention. Individuals who had neither an SPPB nor a 400-m walk time obtained following stopping the LIFE intervention were categorized as No POST.
aNo significant interactions were found between ARM and baseline characteristic; main effect p values are after removing the interaction effects. A backward selection procedure that included intervention group, age, BMI, gender, race, education, number of chronic conditions, SPPB score, and gait speed resulted in the following characteristics predicting POST measure status: BMI (p = .01), gender (p = .01), number of chronic conditions (p = .01), and gait speed (p < .001) being retained. There was no evidence of interactions between intervention group and these baseline characteristics in a multivariable model.
bNumber of chronic conditions based on the five conditions.
At the end of intervention, self-reported activity was slightly more than an hour per week greater among participants in the PA group relative to those in the HE group (Table 2; difference in means = −69 minutes; 95% confidence interval [CI] = −86 to −51). At the POST, there was a substantial decrease in activity in the PA group (−62 minutes; 95% CI = −76 to −48) in comparison (p < .001) to the HE group (−7 minutes; 95% CI = −21 to 7), resulting in PA levels at the POST visit that were comparable between the two groups.
Table 2.
CHAMPS-5 Scores for PA and HE From LAST TRIAL and POST
| Physical Function | N, Adjusted Meana (95% CI) | Difference (95% CI) | p Value on Difference | |
|---|---|---|---|---|
| Health Education | Physical Activity | |||
| CHAMPS 5 (min/wk) | ||||
| Baseline measureb | 80.90 (74.62, 87.18) | n/a | ||
| Last on trial measure | 119.7 (107.2, 132.2) | 188.6 (175.9, 201.3) | −68.9 (−86.5, −51.3) | <.001 |
| Post-trial measure | 112.8 (101.4, 124.2) | 126.3 (114.7, 137.9) | −13.5 (−29.5, 2.47) | .097 |
| Post-trial change from baseline | 31.87 (19.92, 43.81) | 45.40 (33.25, 57.55) | −13.5 (−29.5, 2.47)c | |
| Post-trial change from last on trial measure | −6.90 (−20.7, 6.928) | −62.3 (−76.3, −48.2) | 55.36 (35.63, 75.09) | <.001 |
Note: CI = confidence interval; n/a = not applicable. aAdjusted for gender and clinical site (both used to stratify randomization). bConstrained to be equal between groups prior to randomization. cEqual to the post-trial difference because baseline means are constrained to be equal between groups.
At the LAST TRIAL visit, the SPPB scores did not differ significantly between the two groups (Table 3; HE minus PA difference −0.06; 95% CI = −0.31 to 0.19), nor did the change in SPPB scores differ significantly at POST. When compared with baseline scores, within the PA group, SPPB scores returned to baseline levels (change from baseline = −0.045; 95% CI = −0.24 to 0.15), whereas in the HE group, the scores fell below baseline levels (change from baseline −0.23; 95% CI = −0.42 to −0.04). Supplementary Tables 1 and 2 illustrate that between baseline and POST trial, balance and gait speed scores fell, on average, in both intervention groups, whereas chair stand scores increased. For 400-m walk gait speed, there was not a significant difference between groups at any of the time points, and gait speed in both groups decreased a similar amount from baseline speeds by the POST assessment.
Table 3.
SPPB Score From PA and HE Groups POST Versus BASELINE and Versus LAST TRIAL
| Physical Function | N, Adjusted Meana (95% CI) | Difference (95% CI) | p Value on Difference | |
|---|---|---|---|---|
| Health Education | Physical Activity | |||
| SPPB | ||||
| Baseline measureb | 7.4 (7.3, 7.4) | n/a | ||
| Last on trial measure | 7.7 (7.5, 7.9) | 7.8 (7.6, 8.0) | −0.062 (−0.31, 0.19) | .625 |
| Post-trial measure | 7.1 (6.9, 7.3) | 7.3 (7.1, 7.5) | −0.18 (−0.45, 0.088) | .186 |
| Post-trial change from baseline | −0.23 (−0.42, −0.036) | −0.045 (−0.24, 0.15) | −0.18 (−0.45, 0.088)‡ | |
| Post-trial change from last on trial measure | −0.59 (−0.44, −0.74) | −0.47 (−0.32, −0.62) | −0.12 (−0.33, 0.092) | .266 |
| 400-m walk gait speed (m/s) | ||||
| Baseline measureb | 0.82 (0.81, 0.83) | n/a | ||
| Last on trial measure | 0.74 (0.73, 0.76) | 0.75 (0.74, 0.76) | −0.006 (−0.022, 0.011) | .50 |
| Post-trial measure | 0.71 (0.70, 0.73) | 0.71 (0.70, 0.73) | −0.002 (−0.020, 0.015) | .755 |
| Post-trial change from baseline | −0.11 (−0.12, −0.10) | −0.11 (−0.12, −0.10) | −0.002 (−0.020, 0.015)c | |
| Post-trial change from last on trial measure | −0.034 (−0.043, −0.025) | −0.037 (−0.046, −0.028) | 0.003 (−0.009, 0.015) | .662 |
Note: CI = confidence interval; n/a = not applicable. aAdjusted for gender and clinical site (both used to stratify randomization). bConstrained to be equal between groups prior to randomization. cEqual to the post-trial difference because baseline means are constrained to be equal between groups.
The effect of the intervention on the SPPB outcome was evaluated within groups defined by baseline function: high versus low SPPB or gait speed. No differences were found for the effect of the intervention at either the LAST TRIAL visit (interaction p = .15 for SPPB subgroups; interaction p = .72 for gait speed subgroups) or POST visit (interaction p = .43 for SPPB subgroups; interaction p = .91 for gait speed subgroups) based on baseline levels of function.
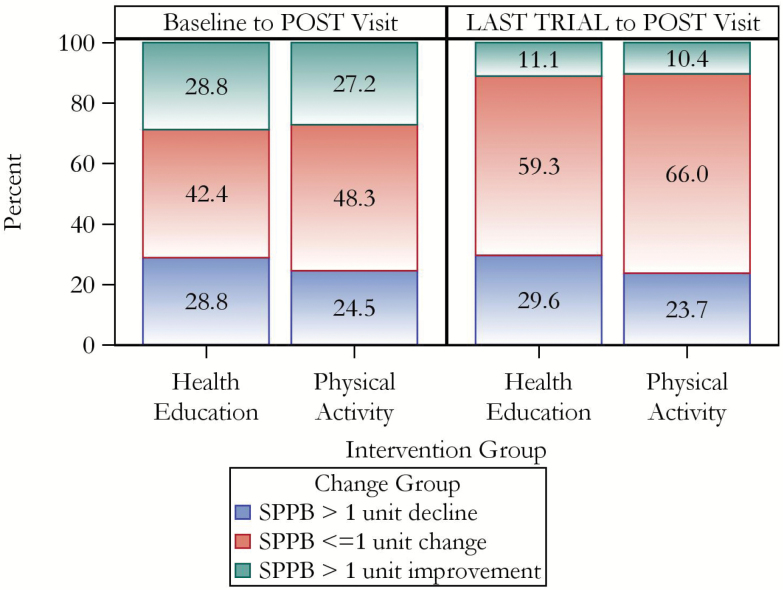
Finally, we evaluated the extent of categorized change: improved, no to minimal change, and decline, in SPPB at the POST. There were no differences by intervention in the proportion of participants in any of the three groups for change from BASELINE to POST visit (p = .098, chi-square 2 df); however, a slightly larger proportion of participants (p = .049, chi-square 2 df) maintained function (no to minimal change) in the PA group relative to HE group for change from LAST TRIAL to POST visits. These results were nonsignificant under both multiple imputation models (Assumption 1: BASELINE to POST p = .20; LAST TRIAL to POST p = .11; Assumption 2: BASELINE to POST p = .07; LAST TRIAL to POST p = .12; Figure 2).
Figure 2.
Percentage of participants with change in SPPB from baseline or LAST TRIAL at POST.
Discussion
Participants from the PA intervention of the LIFE trial who had a 1-year postintervention (POST) visit did not exhibit either a continued behavioral change or functional improvement. Based on observed data at the POST, a larger percentage of PA participants maintained LAST TRIAL SPPB scores than did HE participants; however, this result was not sustained under the two imputation models. In addition, a participant’s baseline functional status, defined as high versus low, did not moderate the effect of the PA intervention on SPPB scores at either LAST TRIAL or POST.
Our results differ from and expand on previous reports in several respects. First, most previous studies address prolonged behavioral change, but not functional improvement, following cessation of an intervention (9). Of those reviewed by Fjeldsoe and colleagues (9), 70% did report a continued behavioral change. However, these studies focused mainly on young- to middle-aged adults or healthy older adults and had shorter follow-up (average follow-up was 9 months with less than 1/3 reporting 12-month or longer follow-up). In addition, Fjeldsoe found one strong predictor of reporting continued behavioral change in the reviewed studies was a low rate of return for follow-up evaluation (<70%); we had greater than 75% of the initial participants return for follow-up. Although baseline differences between participants who did or did not return for follow-up were not specifically reported in previous studies, low rates of return at follow-up probably biased the results of previous studies by under-representing less active or sicker participants because, as we observed, those who returned for follow-up were healthier than those who did not return.
A few recent studies have evaluated both continued functional improvement and behavioral change following exercise interventions. First, in LIFE-P, which recruited frail, sedentary older adults (70–85 years), there was both continued behavioral and functional impact between the PA and HE groups at the one site studied 2 years after cessation of the formal intervention (2). Similarly, Gudlaugsson and colleagues (10) found both continued behavioral and functional effects at 6 or 12 months after cessation of a 6-month walking and resistance training intervention. Half of the participants continued to walk daily or perform resistance training twice weekly and, on average, participants retained end-of-intervention levels of function (measured by 8 foot timed up and go and 6-minute walk distance). Unlike the LIFE participants, these individuals (average age 79) were not recruited to be sedentary nor were they frail (average baseline SPPB was 10). Prolonged functional improvement has also been reported from a shorter intervention. Geirsdottir and colleagues (11) followed participants (average age 74) who completed a 12-week resistance training intervention for 6–18 months after cessation of formal intervention. One quarter still participated in strength training three times weekly and two thirds in recommended levels of physical activity with consequent retention of functional gains (as measured by timed up and go). Again unlike LIFE participants, these participants were not recruited to be sedentary and 87% reported being physically active prior to the study. Similarly, a DVD-based exercise program for older adults (average age 70) was found to have both prolonged behavioral and functional effects 6 months after cessation of the formal intervention with 70% of participants maintaining or increasing end-of-intervention activity levels and retaining functional gains in both SPPB and upper extremity strength (12). At follow-up, most of the participants (>80%) continued to use the intervention DVDs at least weekly. These prior studies, with the exception of LIFE-P, did not recruit frail or sedentary older adults and started with younger, healthier, and more active study participants. The baseline health of the participants may have influenced both their willingness to continue physical activity following the end of intervention and their ability to maintain functional improvements. Furthermore, in keeping with the Fjeldsoe’s review (9), the studies that exhibited the strongest prolonged effects also had the lowest retention rates at follow-up (Geirsdottir and colleagues retained only 63%).
Finally, differences in the study design between LIFE-P and LIFE may have influenced the post intervention effects. LIFE-P participants had to complete a 1-week behavioral run-in of recording dietary intake and physical activity participation, prior to randomization. More important, the behavioral intervention differed in LIFE-P with 10 group sessions focused on development of motivation and skills to promote physical activity adherence within the home environment. Beginning at Week 4 of intervention, a transition toward home-based intervention was expected, with the last half of the intervention having only optional once weekly center-based sessions. Rejeski and colleagues have shown that interventions that promote behavioral skills and the development of resources to sustain home-based physical activity yield stronger long-term effects than traditional structured exercise programs (13). Interestingly, by the end of formal intervention in LIFE-P, there was a much larger difference in time spent in moderate PA between the intervention groups (103 min/wk vs. 234 min/wk in LIFE-P and 120 min/wk vs. 189 min/wk in LIFE) (1,2). Although these activity levels cannot be compared directly because LIFE-P reported all moderate-intensity activities and LIFE reported a subset of five walking and weight training activities, this greater difference between groups may partially be explained by the longer duration of the LIFE intervention, LIFE-P lasted 12 months, and LIFE lasted at least 24 months. LIFE participants may have been losing interest in the intervention and returning to their prior sedentary habits, as noted by the progressive decrease in PA, even during the trial (1).
Given the return to sedentary habits by LIFE participants, the fall to baseline SPPB scores at POST is consistent with previous work. Geirsdottir and colleagues found that following an intervention, the individual’s postintervention activity level determined the time required to return to baseline status, from 11 months if sedentary to 27 months if highly active (11). Hars and colleagues also support this (14). They found that 3 years after cessation of a 6-month music-based physical activity intervention for older adults (average 75 years), about half of participants had remained active and had better functional status than those who had not.
Using the LIFE study, data to evaluate the long-term effect of PA have many strengths: it is a large randomized trial, had high retention (>75%) at follow-up, evaluated both behavioral and functional measures, and studied participants at high risk of developing mobility disability. Most of these aspects have been missing from previous reports. Our data did have some limitations: those with a POST visit were healthier than those without, so this may over-represent any potential long-term functional impact.
Conclusion
Frail, at-risk older adults who were previously sedentary may not be able to independently continue in long-term behavior change following participation in structured physical activity intervention as currently designed. In this regard, future work is needed to explore behavioral methods that target sustaining the adoption of physically active lifestyles. For example, one direction could be the formation of peer groups with similar fitness levels to provide social support for continued physical activity. Another option would be to combine the success observed from group-mediated interventions (13), with mHealth methods that permit an ongoing awareness of physical activity behavior, create a sense of accountability, and provide an opportunity to intervene. Further work into characterizing the few “long-term responders” from the LIFE intervention is warranted. For example, it is currently unclear if any characteristics can predict who (about 10% of participants) retained their improved function following cessation of the intervention. This information could help future interventions target those most likely to benefit. As we observed in the LIFE study, older adults with compromised function experience disruptions in attempts to be physically active due to acute illness and symptoms that accompany chronic disease. In the absence of a system to help patients manage such events and to reinitiate activity, it may be unrealistic to expect long-term effects for structured PA interventions employed in studies such as LIFE.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences online.
Funding
This study was supported by National Institutes of Health, National Institute on Aging (UO1AG22376), National Heart, Lung, and Blood Institute (3U01AG022376-05A2S), Intramural Research Program, National Institute on Aging, National Institutes of Health and Claude D. Pepper Older Americans Independence Centers (1P30AG031679, 1P30AG028740, P30AG024827, 1P30AG21332, P30AG021342).
Conflict of Interest
None reported.
Acknowledgments
Several of the authors are members of the editorial board of the Journal.
Anne B Newman, Editor-in-chief.
Roger Fielding, Stephen B Kritchevsky, Associate Editors.
Thomas M Gill, Jack M Guralnik, Todd M Manini, Anthony Marsh, Mary M McDermott, Marco Pahor, Editorial Board.
References
- 1. Pahor M, Guralnik JM, Ambrosius WT et al. ; LIFE Study Investigators Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–2396. doi:10.1001/jama.2014.5616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rejeski WJ, Marsh AP, Chmelo E et al. The Lifestyle Interventions and Independence for Elders Pilot (LIFE-P): 2-year follow-up. J Gerontol A Biol Sci Med Sci. 2009;64:462–467. doi:10.1093/gerona/gln041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fielding RA, Rejeski WJ, Blair S et al. ; LIFE Research Group The Lifestyle Interventions and Independence for Elders Study: design and methods. J Gerontol A Biol Sci Med Sci. 2011;66:1226–1237. doi:10.1093/gerona/glr123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marsh AP, Lovato LC, Glynn NW et al. ; LIFE Study Research Group Lifestyle interventions and independence for elders study: recruitment and baseline characteristics. J Gerontol A Biol Sci Med Sci. 2013;68:1549–1558. doi:10.1093/gerona/glt064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guralnik JM, Simonsick EM, Ferrucci L et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- 6. Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. [DOI] [PubMed] [Google Scholar]
- 7. Lu K. On efficiency of constrained longitudinal data analysis versus longitudinal analysis of covariance. Biometrics. 2010;66:891–896. doi:10.1111/j.1541-0420.2009.01332.x [DOI] [PubMed] [Google Scholar]
- 8. Liang KY, Zeger SL. Longitudinal data analysis of continuous and discrete responses for pre-post design. Sankha: Indian J Stat B. 2000;62:134–148. [Google Scholar]
- 9. Fjeldsoe B, Neuhaus M, Winkler E, Eakin E. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol. 2011;30:99–109. doi:10.1037/a0021974 [DOI] [PubMed] [Google Scholar]
- 10. Gudlaugsson J, Gudnason V, Aspelund T et al. Effects of a 6-month multimodal training intervention on retention of functional fitness in older adults: a randomized-controlled cross-over design. Int J Behav Nutr Phys Act. 2012;9:107. doi:10.1186/1479-5868-9-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geirsdottir OG, Arnarson A, Ramel A, Briem K, Jonsson PV, Thorsdottir I. Muscular strength and physical function in elderly adults 6–18 months after a 12-week resistance exercise program. Scand J Public Health. 2015;43:76–82. doi:10.1177/1403494814560842 [DOI] [PubMed] [Google Scholar]
- 12. Wójcicki TR, Fanning J, Awick EA, Olson EA, Motl RW, McAuley E. Maintenance effects of a DVD-delivered exercise intervention on physical function in older adults. J Gerontol A Biol Sci Med Sci. 2015;70:785–789. doi:10.1093/gerona/glu188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rejeski WJ, Brawley LR, Ambrosius WT et al. Older adults with chronic disease: benefits of group-mediated counseling in the promotion of physically active lifestyles. Health Psychol. 2003;22:414–423. [DOI] [PubMed] [Google Scholar]
- 14. Hars M, Herrmann FR, Fielding RA, Reid KF, Rizzoli R, Trombetti A. Long-term exercise in older adults: 4-year outcomes of music-based multitask training. Calcif Tissue Int. 2014;95:393–404. doi:10.1007/s00223-014-9907-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.