Abstract
BACKGROUND
Using the data from 56,365 individuals, from 185 countries, and a Nokia Health Wireless blood pressure (BP) monitor, we investigated real-world characteristics of BP variability (BPV).
METHODS
All included individuals self-measured and uploaded their BP using Bluetooth at least 20 times over a period of ≥1 month at a frequency and duration of their choosing. In total, 16,904,844 BP measurements were analyzed, with a median of 146 measurements per person (interquartile range [IQR] 73–321) over a median of 14 months (IQR 7–31). SD, coefficient of variation, maximum BP, and maximum minus minimum BP difference were all calculated as measures of BPV.
RESULTS
BPV showed a distinct pattern, influenced by season of year, day of week, and time of day. BPV index was higher in females compared with males (P < 0.001) and increased with age (P < 0.001). Compared to the weekend, the weekday BPV index was significantly higher, and this finding was more prominent in females (P = 0.001). In multivariate analysis, BPV index were significantly associated with age, gender, geographic location, and mean BP values.
CONCLUSION
Using the largest BP data set we are aware of, with the benefits and limitations of real-world measurement, we could show the pattern of BPV and provide reference values that may be helpful in understanding the nature of BPV as self-measurement at home becomes more common, and help guide individualized management.
Keywords: blood pressure, blood pressure variability, big data, hypertension, mobile health
Blood pressure (BP)-related morbidity and mortality is one of our most pressing global health issues. Although, absolute BP values appear to be the most important factors determining prognosis, BP variability (BPV) has also been proven in a number of studies to be an independent and strong indicator of future coronary heart disease, heart failure, stroke, and cardiovascular or all-cause mortality.1–3
BPV had been thought of as random fluctuations or noise around a patient’s true basal BP. Accordingly, it was considered to be a limitation of measuring BP in the office setting. However, recent data showed that BPV including short-term (over 24 hours), mid-term (day-to-day), and long-term (visit-to-visit) is reproducible and not a random phenomenon.4
The vast majority of prior studies of BPV were based on BPs determined in the clinical setting.2,5 One of the largest studies of BPV included 6,312 community-dwelling participants, with BP measurements determined in a community setting, but only included morning BP measurements.6 The growing availability and use of reliable and accurate home BP devices with wireless connectivity and automated logging of BPs allows limitations of prior studies to potentially be overcome. Home BP monitoring makes it possible to collect a large amount of data, any time of day or day of week, which can more likely capture real-world influences on BPV, including environmental, temporal, emotional, or seasonal variations.7
In this study, we describe the characteristics and investigate the factors associated with BPV within the largest data set to date ever available of self-monitored BPs acquired from over 56,000 self-monitoring individuals using a wireless BP monitoring device in a real-world setting. Using these data, we will identify characteristics associated with BPV and to provide reference values of BPV in a self-monitored population.
METHODS AND PARTICIPANTS
Participants
From all the active user of Nokia Health’s wireless BP monitor, we included a total of 56,365 participants from 185 countries including United States, France, Germany, and United Kingdom who had ≥20 BP measurements with the earliest and latest separated by at least 1 month. We applied the same selection criteria for all the populations. No clinical information was available for participants, including medications or diagnoses.
All participants agreed to their data being used for research purposes as part of the Terms and Conditions when setting up a user account. The data are anonymous and were extracted for research purposes. The study was reviewed and exempted by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. X-1707-411-902). In addition, all methods were performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology Statement.
Data acquisition, management, and definition for analysis
All BP measurements were made using a Nokia Health BP-800 (Nokia Health, Paris, France) by individuals who obtained the device for self-monitoring purposes. This device has been validated according to European Society of Hypertension International Protocol.8 The device can be connected to an Apple iOS and fits an iPhone, iPad, or iPod. A specific Withings BP-800 free application can be downloaded from the App store, which also provides a set of instruction to measure BP properly. The device automatically saves systolic BP (SBP) and diastolic BP (DBP) data, pulse, and local date and time of measurement, sending those values to network servers. After excluding duplicated values and outlier (SBP < 50 mm Hg or > 300 mm Hg, DBP < 30 mm Hg or > 250 mm Hg), we analyzed 16,904,844 SBP measurements data (number of median BP measurements per person: 146, interquartile ranges [IQR] 73–321) (Supplementary Figure 1). All measurements were made purely at the discretion of the individual with no prompting.
For the analysis of the relationship between BPV and time dependent variation, we compared the BPV of weekdays (from Monday to Friday) and weekends (from Saturday to Sunday) among 55,028 participants who had more than 5 BP measurements on both weekdays and weekends. Finally, comparison between summer (from June to August) and winter (from November to February) BPV was done in 39,835 participants who had more than 5 BP measurements during both summer and winter period and lived in the Northern hemisphere.
Calculation of BPV
We quantified the variation of SBP or DBP within an individual over the course. We computed SD, coefficient of variation (CV), maximum BP, and the difference between the maximum and minimum BP as an intraindividual BPV index.5 CV is calculated as SD − SBP/mean SBP × 100.
Statistical analysis
We report means (SD) or medians with IQRs for continuous variables and counts with percentages for categorical variables. The differences in continuous variables were analyzed using Student’s t-tests and 1-way analysis of variance. Comparisons according to time and seasonal variation were done using paired t-test. Multiple linear regression analysis was performed to identify the independent factors associated with BPV. Differences were considered statistically significant at P <0.05, and all analyses were 2-tailed. We analyzed the data using R package (version 3.3.1, https://www.r-project.org/) and SPSS 21.0 for Window (IBM-SPSS, Chicago, IL). All data from the participants were de-identified and analyzed anonymously.
RESULTS
Demographic and BP characteristics of study population
A total of 56,365 participants had at least 20 BP measurements, spanning over greater than 1 month were included in this analysis. Their data included 16,904,844 individual BP measurements, with a median of 146 measurements per person (IQR 73–321), acquired over a median period of 14 months (IQR 7–31). Details of the participants were presented in Table 1. The majority were male (n = 44,844, 79.6%) and the mean (SD) age was 54.7 (12.6). US participants were most common (N = 19,963, 35.4%). The mean (SD) SBP/DBP were 131.0 (10.9)/80.1 (8.2) mm Hg and the mean (SD) pulse rate was 70.3 (9.6)/min. The population’s mean (SD) maximum SBP/DBP were 161.2 (18.0)/100.2 (11.7) mm Hg and minimum SBP/DBP were 103.1 (12.3)/61.6 (9.0) mm Hg.
Table 1.
Characteristics of study participants
| Number of participants (N = 56,365) | |
|---|---|
| Gender | |
| Male | 44,844 (79.6%) |
| Female | 11,521 (20.4%) |
| Age (year) | |
| 18–29 | 928 (1.6%) |
| 30–39 | 5,674 (10.1%) |
| 40–49 | 13,129 (23.3%) |
| 50–59 | 16,552 (29.4%) |
| 60–69 | 13,065 (23.2%) |
| 70–79 | 5,742 (10.2%) |
| 80–89 | 1,181 (2.1%) |
| 90+ | 94 (0.2%) |
| Country | |
| Canada | 2,101 (3.7%) |
| Switzerland | 2,416 (4.3%) |
| Germany | 9,070 (16.1%) |
| France | 3,665 (6.5%) |
| United Kingdom | 2,625 (4.7%) |
| Italy | 1,944 (3.4%) |
| Japan | 1,174 (2.1%) |
| United State | 19,963 (35.4%) |
| Othersa | 13,407 (23.8%) |
aOther countries where less than 1,000 participants enrolled for this analysis.
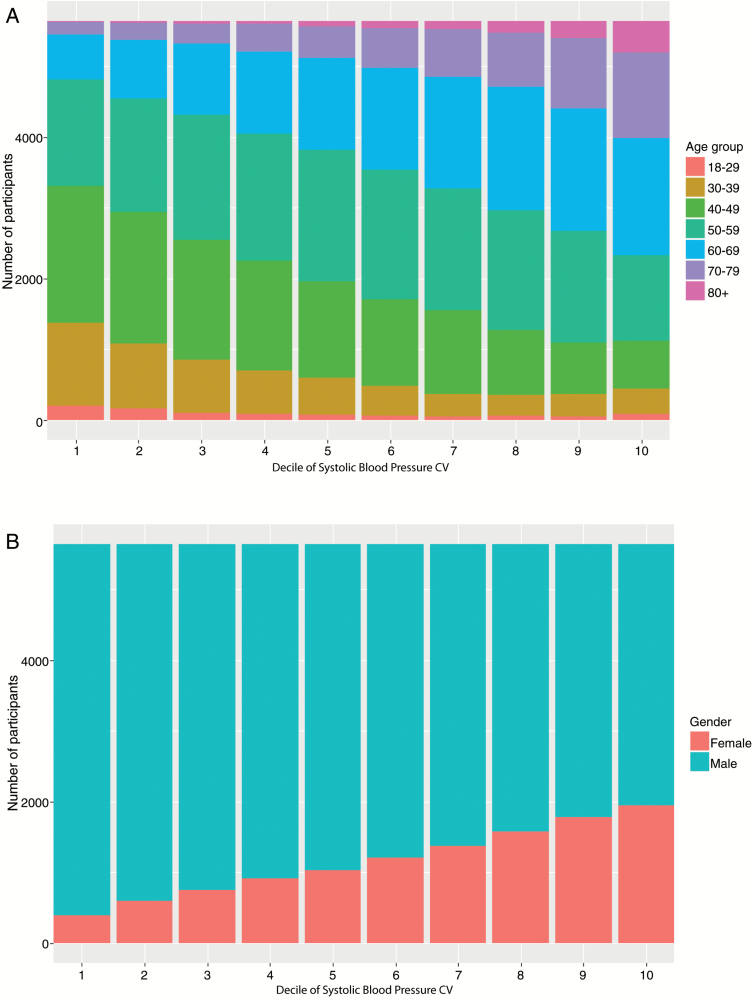
Blood pressure variability
Systolic and diastolic BPV indices such as SD, CV, and maximum and minimum BP according to participants’ gender, age, country, day of week, and season of year are presented in Table 2. For clarity, further descriptions of BPV will focus primarily on CV only because it is a BPV index independent of BP levels. The overall results were not different according to the BPV index. When analyzed by decile of BPV, the lowest decile had a mean (SD) CV of SBP was 4.8 mm Hg (0.48) and for the highest decile 13.2 mm Hg (2.12) (Supplementary Figure 2).
Table 2.
SD, CV, maximum minus minimum BP difference of systolic and/or diastolic blood pressure
| Systolic blood pressure | Diastolic blood pressure | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean SBP, mm Hg | SD, mm Hg | CV, mm Hg | MMD, mm Hg | Mean DBP, mm Hg | SD, mm Hg | CV, mm Hg | MMD, mm Hg | |
| All participants (N = 56,365) | 131.0 (10.9) | 10.5 (3.4) | 8.0 (2.4) | 58.2 (20.6) | 80.1 (8.2) | 7.0 (2.0) | 8.7 (2.5) | 38.6 (12.9) |
| Male (N = 44,844) | 131.6 (10.5) | 10.3 (3.3) | 7.8 (2.3) | 57.0 (20.2) | 80.4 (8.1) | 6.8 (2.0) | 8.5 (2.4) | 37.8 (12.4) |
| Female (N = 11,521) | 128.9 (12.0) | 11.6 (3.6) | 9.0 (2.5) | 62.9 (21.3) | 78.9 (8.4) | 7.5 (2.1) | 9.5 (2.6) | 41.9 (13.9) |
| Age 18–29 (N = 928) | 125.0 (11.2) | 9.2 (3.5) | 7.3 (2.7) | 47.7 (18.9) | 76.9 (8.7) | 7.2 (2.4) | 9.4 (2.9) | 37.0 (13.1) |
| Age 30–39 (N = 5,674) | 128.0 (11.2) | 9.2 (3.2) | 7.1 (2.3) | 48.2 (18.4) | 80.4 (8.8) | 6.9 (2.2) | 8.6 (2.6) | 36.1 (12.9) |
| Age 40–49 (N = 13,129) | 130.1 (10.6) | 9.5 (2.9) | 7.3 (2.1) | 51.6 (17.6) | 82.4 (8.2) | 6.9 (2.0) | 8.4 (2.3) | 36.9 (12.2) |
| Age 50–59 (N = 16,552) | 131.2 (10.6) | 10.4 (3.0) | 7.9 (2.2) | 57.1 (18.5) | 81.7 (7.6) | 6.9 (1.9) | 8.4 (2.3) | 38.1 (12.3) |
| Age 60–69(N = 13,065) | 132.3 (10.8) | 11.4 (3.3) | 8.6 (2.4) | 63.8 (20.1) | 78.8 (7.3) | 7.2 (2.1) | 8.8 (2.4) | 39.5 (12.6) |
| Age 70–79 (N = 5,742) | 133.0 (10.8) | 12.4 (3.7) | 9.3 (2.6) | 70.5 (21.9) | 75.1 (7.2) | 8.0 (2.3) | 9.6 (2.6) | 42.5 (13.9) |
| Age 80+ (N = 1,275) | 133.9 (11.6) | 13.9 (4.1) | 10.4 (2.9) | 79.2 (23.7) | 72.8 (7.4) | 7.0 (2.3) | 11.0 (2.9) | 48.2 (15.0) |
| Country (CA) (N = 2,101) | 130.9 (10.8) | 10.4 (3.2) | 7.9 (2.3) | 57.0 (19.5) | 79.4 (8.3) | 6.7 (1.9) | 8.5 (2.3) | 37.4 (12.4) |
| Country (CH) (N = 2,416) | 130.2 (10.6) | 10.0 (3.1) | 7.6 (2.2) | 56.3 (20.1) | 80.2 (7.9) | 6.7 (1.9) | 8.3 (2.3) | 37.8 (12.7) |
| Country (DE) (N = 9,070) | 131.6 (10.5) | 9.9 (3.0) | 7.5 (2.1) | 56.1 (19.6) | 81.1 (7.9) | 6.5 (1.8) | 8.1 (2.1) | 37.1 (12.2) |
| Country (FR) (N = 3,665) | 131.5 (11.5) | 10.7 (3.5) | 8.1 (2.4) | 58.7 (20.6) | 79.5 (8.4) | 7.1 (2.1) | 9.0 (2.6) | 39.2 (13.3) |
| Country (GB) (N = 2,625) | 132.9 (11.8) | 10.1 (3.2) | 7.6 (2.2) | 54.0 (19.3) | 80.8 (8.6) | 6.7 (1.9) | 8.3 (2.3) | 36.0 (12.3) |
| Country (IT) (N = 1,944) | 128.5 (10.8) | 10.6 (3.4) | 8.2 (2.4) | 59.8 (20.9) | 78.1 (7.8) | 6.9 (1.9) | 8.9 (2.4) | 39.2 (12.8) |
| Country (JP) (N = 1,174) | 129.5 (11.9) | 10.0 (3.1) | 7.7 (2.2) | 58.4 (19.4) | 82.3 (9.4) | 7.0 (2.0) | 8.5 (2.3) | 41.0 (12.3) |
| Country (US) (N = 19,963) | 131.3 (10.8) | 11.0 (3.6) | 8.3 (2.5) | 59.6 (21.0) | 79.8 (8.2) | 7.2 (2.1) | 9.0 (2.6) | 39.2 (13.0) |
| Country (other) (N = 13,407) | 130.3 (10.8) | 10.6 (3.4) | 8.1 (2.4) | 58.4 (20.8) | 80.1 (8.0) | 7.0 (2.0) | 8.8 (2.5) | 39.1 (13.0) |
| Weekdays (N = 55,028) | 131.2 (11.0) | 10.5 (3.4) | 7.9 (2.4) | 54.8 (20.2) | 80.3 (8.2) | 6.9 (2.1) | 8.6 (2.5) | 36.3 (12.6) |
| Weekends (N = 55,028) | 130.7 (11.1) | 10.3 (3.7) | 7.9 (2.7) | 45.9 (19.3) | 79.7 (8.3) | 6.8 (2.3) | 8.6 (2.8) | 30.1 (12.0) |
| Summera (N = 39,835) | 129.5 (11.2) | 9.7 (3.5) | 7.5 (2.6) | 43.7(19.2) | 79.1 (8.4) | 6.4 (2.2) | 8.1 (2.7) | 28.9 (12.1) |
| Winterb (N = 39,835) | 131.5 (10.9) | 10.1 (3.6) | 7.7 (2.5) | 48.7 (20.2) | 80.2 (8.2) | 6.6 (2.2) | 8.3 (2.6) | 31.9 (12.7) |
Abbreviations: CA, Canada; CH, Switzerland; CV, coefficient of variation; DE, Germany; FR, France; GB, United Kingdom; IT, Italy; JP, Japan; MMD, maximum minus minimum blood pressure difference; US, United State.
aSummer: June–August.
bWinter: November–February.
Factors associated with BPV
BPV was higher in females compared with males. CV of SBP were 7.8 (2.3) mm Hg in male and 9.0 (2.5) mm Hg in female (P < 0.001). BPV was also increased with age (P < 0.001) (Figure 1). Because the average age of females was greater than males (56.5 (13.8) years in females vs. 54.3 (12.2) years in males, P < 0.001), even after adjusting for age with a linear model, females BPV was significantly greater than males. There was also a significant difference in CV of SBP and DBP according to geographic location, again adjusted for age, gender, and mean BP (P < 0.001). Participants from the United States showed highest CV of SBP followed by Italy and France, 8.4 (2.6) mm Hg, 8.2 (2.4) mm Hg, and 8.1 (2.4) mm Hg, respectively. In multivariate analysis, BPV index were significantly associated with age, gender, geographic location, and mean SBP and DBP values (Table 3).
Figure 1.
Distribution of age (a) and gender (b) according to intraindividual CV of SBP (N = 56,365). Abbreviations: CV, coefficient of variation; SBP, systolic blood pressure.
Table 3.
Multiple linear regression analysis associated with blood pressure variability (CV of SBP)
| Unstandardized coefficients (B) | Standard error | 95% Confidence interval for B | P value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| (Intercept) | 4.043 | 0.1423 | 3.764 | 4.322 | <0.001 |
| Female | 1.079 | 0.0236 | 1.033 | 1.125 | <0.001 |
| Male | Reference | ||||
| Age 80+ | 2.807 | 0.0978 | 2.615 | 2.998 | <0.001 |
| Age 70–79 | 1.846 | 0.0799 | 1.690 | 2.003 | <0.001 |
| Age 60–69 | 1.172 | 0.0761 | 1.023 | 1.321 | <0.001 |
| Age 50–59 | 0.556 | 0.0755 | 0.408 | 0.704 | <0.001 |
| Age 40–49 | 0.032 | 0.0761 | −0.117 | 0.181 | 0.677 |
| Age 30–39 | −0.196 | 0.0791 | −0.351 | −0.042 | 0.013 |
| Age 18–29 | Reference | ||||
| Country (US) | 0.452 | 0.0511 | 0.351 | 0.552 | <0.001 |
| Country (other) | 0.356 | 0.0524 | 0.254 | 0.459 | <0.001 |
| Country (JP) | 0.235 | 0.0815 | 0.076 | 0.395 | 0.004 |
| Country (IT) | 0.431 | 0.0702 | 0.293 | 0.568 | <0.001 |
| Country (GB) | −0.157 | 0.0653 | −0.285 | −0.029 | 0.016 |
| Country (FR) | 0.159 | 0.0610 | 0.039 | 0.278 | 0.009 |
| Country (DE) | −0.206 | 0.0540 | −0.312 | −0.100 | <0.001 |
| Country (CH) | −0.133 | 0.0665 | −0.263 | −0.003 | 0.045 |
| Country (CA) | Reference | ||||
| Mean SBP | 0.018 | 0.0013 | 0.016 | 0.021 | <0.001 |
| Mean DBP | 0.006 | 0.0018 | 0.003 | 0.010 | <0.001 |
Abbreviations: CA, Canada; CH, Switzerland; DBP, diastolic blood pressure; DE, Germany; FR, France; GB, United Kingdom; IT, Italy; JP, Japan; SBP, systolic blood pressure.
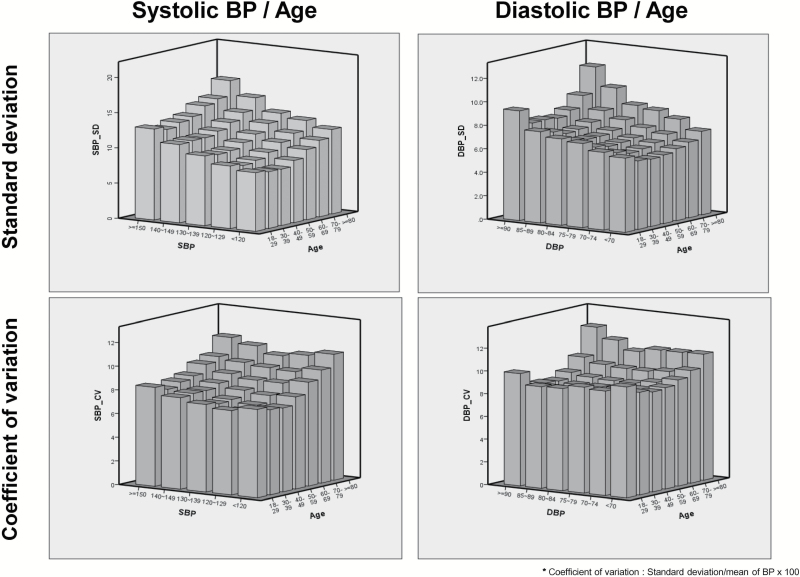
Reference values for BPV according to age and BP
Reference values of BPV index according to age and BP levels are shown in Figure 2. The BPV index increase as the increase of age and BP level. BPV index (SD, CV, and maximum and minimum BP of SBP) increased both with increasing age and mean SBP levels in the participants. Finally, the increase in BPV index with SBP was more pronounced as the participants get older (Supplementary Figure 3A–C).
Figure 2.
Reference value of intraindividual SD of SBP according to SBP levels and age. Abbreviations: BP, blood pressure; DBP, diastolic BP; SBP, systolic BP.
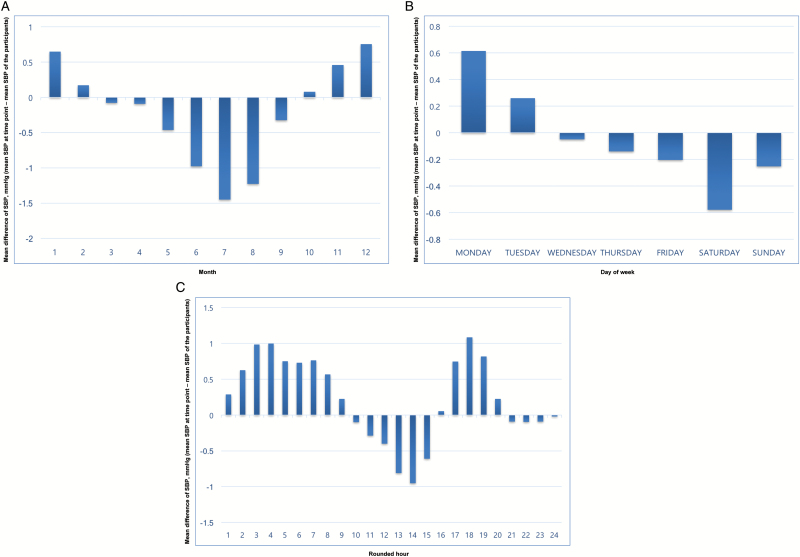
BPV according to time and seasonal variation
We have calculated the mean SBP per participant for each month, day of week, and rounded hour, and plotted in Figure 3 the mean difference of SBP (mean SBP of the time point − mean SBP) considering all the participants. BPV was varied according to month of the year. The changes in SBP showed a distinct pattern, with higher values during the winter season (November – February) than the summer season (June – August) (Figure 3a). BP values were also related to the day of the week. Most commonly, the SBP was highest on Monday, whereas minimal SBP was most common on Saturday and Sunday (Figure 3b). Compared to weekend, weekday BPV index were higher. Weekday CV of SBP was 7.95 (2.44) mm Hg and weekend CV of SBP was 7.89 (2.67) mm Hg (P < 0.001). Furthermore, CV of SBP during winter was higher than summer period (7.7 (2.5) mm Hg vs. 7.5 (2.6) mm Hg, P < 0.001). Finally, high values of SBP were more commonly observed during morning (7:00–10:00 am) and evening (17:00–19:00 pm) (Figure 3c). Few users measured their BP during the night (0:00–5:00 am), so that values may be biased.
Figure 3.
Changes in SBP according to month (a), day of week (b), and rounded hour (c). Abbreviations: SBP, systolic blood pressure.
DISCUSSION
Novel findings from our study of serial, self-monitored BPs is that BPV is higher during weekdays and winter season, supporting that environmental factors such as job stress and the outside environment influence BPV. In addition, we confirmed what has previously been shown in much smaller studies, that BPV increase with age, and that females have greater BPV than male, even after adjusting for age and BP values. The size of our data set, 20-fold larger than the next largest, also allowed for the development of real-world reference values for BPV according to age, gender, and BP values.
Beyond the absolute SBP and DBP values, a great deal of data have shown an independent link between increased BPV and target organ damage, cardiovascular events, cognitive decline, and mortality.9–12 In particular, recent studies have found that patients with higher variability in BP over time are at higher risk compared with patients with the same mean BP level.2 Although, the clinical importance of BPV has been relatively well established, it is rarely evaluated clinically due to the infrequency of office visits for BP determination and disjointed data sets. Due to these limitations, the reference values of BPV according to age, gender, and BP levels have not yet been well described. To understand how an individual’s BP responds to change, whether slow change associated with aging, or acute change associated with stress, requires a large volume of data from a variety of participants for an extended period of time.
Home BP measurements rather than office BP are recommended for the optimal assessment of BP changes.13,14 Home BP measurement, which is reliable, reproducible, and free from white-coat effect and observer dilution bias, is associated with target organ damage and offers better prognostic value than office BP measurement.15,16 Recently, home BPV measured over 7 consecutive days showed an association with future cardiovascular events.17
To know the characteristics of BPV is important to better understanding the nature of BP and its intraindividual differences. With greater knowledge of BPV, we can establish individual-based reference values, which can lead to a better understanding of interindividual variability, and potentially most importantly, what life-style and pharmaceutical interventions improve variability. An additional value to understanding a person’s typical intraindividual BPV is in the setting of remote chronic condition management programs dependent on self-monitored BP values by allowing for the determination of the validity of a BP measurement using an automated home device. Understanding natural variability in people and populations is critical to being able to differentiate between artifactual readings and critical events such as hypertensive emergencies or severe hypotensive events. Furthermore, with the genome-wide association analyses, we could identify new loci influencing BP variation.18
We were able to identify time of day, day of week, and seasonal variation of BPV in this study. Previous limitations in available data have not allowed for this level of understanding. However, in our substantially larger real-world cohort sample we were able to. The BPV was higher during the winter season and on weekdays. We were able to show that BP tends to be highest on Mondays, gradually decreasing as the week progresses to its lowest point on Saturdays. These findings suggest environmental factors such as job stress are associated with BPV. Interestingly, the time and seasonal variation of BPV can be associated with the weekly or seasonal variation of stroke or acute myocardial infarction incidence.19,20 However, we included participants from Northern hemisphere, thus the seasonality of BPV need to be studied for the Southern hemisphere.
Also, we could observe that BPV increase with age and was higher in female, which are consistent with previous results.5,10,21 Impaired baroreflex and increased arterial stiffness were considered to be underlying mechanisms; however, additional research is required to investigate the basic pathophysiology and its clinical significance. We could observe that CV of SBP was higher in US participants than other countries. Several factors such as level of job stress, environmental factor, or climate may influence BPV. Further studies are required to identify the underlying mechanism linked with geographic difference of BPV.
Our study has some notable limitations. Most notably, these are real-world data from self-monitored BP and therefore was not carried out with the typical rigor of research-specific BP programs. For example, participants were not equally distributed in age (younger), gender (male predominance), and geographic location (US predominance), which might affect the result of our study. Accordingly, the “trade-off” between quantity and quality of data should be considered in the interpretation of the results.22 In addition, we did not have any clinical information for the individuals studied, including their hypertension treatment, if any, and life-style associated factors such as smoking, exercise, work schedule, etc. Although, we suggested the reference value of BPV, it is not yet clear how to manage persons who have increased BPV, especially normotensive people. Previous studies showed that calcium channel blocker were superior to beta-blocker in reducing BPV. Thus, recommending calcium channel blocker for those patients may be a good option. Finally, we included different nature of BPV in a single data set such as within-day, day-to-day, or longer-term BPV, which should be considered for the interpretation of the results. We analyzed the device based data set, thus in case of multiple users, the chance of mixing data of multiple users should be considered.
Our study also has important strengths. The data set includes large sample size of BP measurements from all around of the world. Accordingly, we could analyze the relationship between BPV with time or seasonal variation. Furthermore, the reference value was based on a great number of individual measurements (median number of BP measurement: 146, IQR 73–321), with prior studies showing ~30 measurements are needed to minimize routine SD of BP readings, thus it can provide a solid reference range based on BP and age.23 Thus, we believe that these results can provide useful reference values of BP and BPV in the coming digital medicine era in which more patient-reported medical information from huge numbers of individuals will be examined and compiled using wearable device.
In conclusion, with the largest data set obtained in a real-world setting, we showed the characteristics of BPV and its association with day of the week and seasonal variation, and confirmed its association with age and gender previous found in more formal studies. We could also establish reference values for real-world BPV from a global, self-monitored BP data set that should help with future efforts to identify people who have greater BPV and potentially evaluate therapies that influence it beyond just BP alone.
SUPPLEMENTARY MATERIAL
Supplementary data are available at American Journal of Hypertension online.
DISCLOSURE
Matthieu Vegreville, Alexis Normand, and Nicolas Schmidt are full-time employees of Nokia Health. Other authors declared no conflict of interest.
ACKNOWLEDGMENTS
This work was supported in part by the National Institutes of Health (NIH)/National Center for Advancing Translational Sciences grant UL1TR001114 and a grant from the Qualcomm Foundation. Kwang-il Kim contributed to the study design, data interpretation, and writing of the paper. Nima Nikzad, Giorgio Quer, Nathan Wineinger, Matthieu Vegreville, Alexis Normand, Nicolas Schmidt, and Eric J Topol contributed to the study design and data interpretation. Steven Steinhubl contributed to the study design, data interpretation, and analysis and writing of the paper. As the corresponding author, Steven Steinhubl had full access to all the data in the study and was responsible for the decision to submit this manuscript for publication.
REFERENCES
- 1. Muntner P, Whittle J, Lynch AI, Colantonio LD, Simpson LM, Einhorn PT, Levitan EB, Whelton PK, Cushman WC, Louis GT, Davis BR, Oparil S. Visit-to-visit variability of blood pressure and coronary heart disease, stroke, heart failure, and mortality: a cohort study. Ann Intern Med 2015; 163:329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, McManus RJ. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ 2016; 354:i4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz KM, Tanner RM, Falzon L, Levitan EB, Reynolds K, Shimbo D, Muntner P. Visit-to-visit variability of blood pressure and cardiovascular disease and all-cause mortality: a systematic review and meta-analysis. Hypertension 2014; 64:965–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol 2013; 10:143–155. [DOI] [PubMed] [Google Scholar]
- 5. Stergiou GS, Ntineri A, Kollias A, Ohkubo T, Imai Y, Parati G. Blood pressure variability assessed by home measurements: a systematic review. Hypertens Res 2014; 37:565–572. [DOI] [PubMed] [Google Scholar]
- 6. Juhanoja E, Johansson J, Thijs L, Asayama K, Hozawa A, Ohkubo T, Stergiou G, Tsuji I, Imai Y, Jula A, Niiranen T, Staessen J. Yia 01-03 Outcome-driven reference frame for self-measured home blood pressure variability: International database of home blood pressure in relation to cardiovascular outcome (IDHOCO). J Hypertens 2016; 34 (Suppl 1) - ISH 2016 Abstract Book: p. e36. [Google Scholar]
- 7. Steinhubl SR, Muse ED, Barrett PM, Topol EJ. Off the cuff: rebooting blood pressure treatment. Lancet 2016; 388:749. [DOI] [PubMed] [Google Scholar]
- 8. Topouchian J, Agnoletti D, Blacher J, Youssef A, Chahine MN, Ibanez I, Assemani N, Asmar R. Validation of four devices: Omron M6 Comfort, Omron HEM-7420, Withings BP-800, and Polygreen KP-7670 for home blood pressure measurement according to the European Society of Hypertension International Protocol. Vasc Health Risk Manag 2014; 10:33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: findings from NHANES III, 1988 to 1994. Hypertension 2011; 57:160–166. [DOI] [PubMed] [Google Scholar]
- 10. Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010; 375:895–905. [DOI] [PubMed] [Google Scholar]
- 11. Whittle J, Lynch AI, Tanner RM, Simpson LM, Davis BR, Rahman M, Whelton PK, Oparil S, Muntner P. Visit-to-visit variability of BP and CKD outcomes: results from the ALLHAT. Clin J Am Soc Nephrol 2016; 11:471–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gosmanova EO, Mikkelsen MK, Molnar MZ, Lu JL, Yessayan LT, Kalantar-Zadeh K, Kovesdy CP. Association of systolic blood pressure variability with mortality, coronary heart disease, stroke, and renal disease. J Am Coll Cardiol 2016; 68:1375–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O’Brien E, Ohkubo T, Padfield P, Palatini P, Pickering TG, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G; ESH Working Group on Blood Pressure Monitoring . European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24:779–785. [DOI] [PubMed] [Google Scholar]
- 14. Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S; Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37:253–390. [DOI] [PubMed] [Google Scholar]
- 15. Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16:971–975. [DOI] [PubMed] [Google Scholar]
- 16. Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension 2010; 55:1346–1351. [DOI] [PubMed] [Google Scholar]
- 17. Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension 2012; 59:212–218. [DOI] [PubMed] [Google Scholar]
- 18. Hoffmann TJ, Ehret GB, Nandakumar P, Ranatunga D, Schaefer C, Kwok PY, Iribarren C, Chakravarti A, Risch N. Genome-wide association analyses using electronic health records identify new loci influencing blood pressure variation. Nat Genet 2017; 49:54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shigematsu K, Watanabe Y, Nakano H; Kyoto Stroke Registry Committee . Weekly variations of stroke occurrence: an observational cohort study based on the Kyoto Stroke Registry, Japan. BMJ Open 2015; 5:e006294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sheth T, Nair C, Muller J, Yusuf S. Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol 1999; 33:1916–1919. [DOI] [PubMed] [Google Scholar]
- 21. Imai Y, Aihara A, Ohkubo T, Nagai K, Tsuji I, Minami N, Satoh H, Hisamichi S. Factors that affect blood pressure variability. A community-based study in Ohasama, Japan. Am J Hypertens 1997; 10:1281–1289. [DOI] [PubMed] [Google Scholar]
- 22. Mayer-Schönberger V. Big data for cardiology: novel discovery?Eur Heart J 2016; 37:996–1001. [DOI] [PubMed] [Google Scholar]
- 23. Chatellier G, Day M, Bobrie G, Menard J. Feasibility study of N-of-1 trials with blood pressure self-monitoring in hypertension. Hypertension 1995; 25:294–301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.