Delivering news about worsening disease can be challenging for clinicians; however, information about treatment options and prognosis are important for informed consent and decision‐making at end of life. This article focuses on changes in patients' perceptions of physician compassion, after a more optimistic vs. a less optimistic physician message followed by a negative clinical outcome.
Keywords: Physician compassion, Effect of clinical outcome, Patient perception of physician, Physician professionalism, Impression of physician
Abstract
Background.
In a previous randomized crossover study, patients perceived a physician delivering a more optimistic message (MO) as more compassionate and professional. However, the impact of the clinical outcome of the patient on patient's perception of physician's level of compassion and professionalism has not been previously studied. Our aim was to determine if the reported clinical outcome modified the patient's perception of physician compassion, professionalism, impression, and preference for physician.
Materials and Methods.
One hundred twenty‐eight advanced cancer patients in an outpatient Supportive Care Center were randomized to complete validated questionnaires about patients' perception of physician's level of compassion, professionalism, impression, and preference of physician for themselves and their family after watching scripted videos depicting a physician delivering an MO versus a less optimistic (LO) message followed by a clinical vignette depicting a worse outcome.
Results.
Median age was 61 years and 55% were female. There was no difference in compassion score after the vignette in the MO and LO groups. However, there were significantly worse overall impression and professionalism scores in both the MO and LO groups after the vignette. In the MO group, preference for the physician for themselves and their family significantly decreased after the vignette.
Conclusion.
Seeing a worse clinical outcome did not change the patients' appraisal of an inappropriately optimistic physician. However, it reduced the overall impression of both physicians that conveyed an MO or an LO message and it also resulted in less likelihood of choosing the MO physician for themselves and their family.
Implications for Practice.
The study found that a patient's perception of a physician's compassion did not change after reading a vignette describing a negative clinical outcome, regardless of whether the physician had given a more or a less optimistic message to the patient. However, the results suggested that patients perceived worse professionalism and overall physician impression scores for both more and less optimistic physicians and lower likelihood to choose the more optimistic physician for themselves and their family.
Introduction
Delivering news about worsening disease can be challenging for clinicians [1], [2], [3], [4]. However, information about treatment options and prognosis are important for informed consent and decision‐making at end of life. Weeks et al. found in 917 advanced lung or colon cancer patients that patients who believed they had more than 6 months to live favored life‐extending treatments and had more readmissions, attempted resuscitations, and death on ventilators [5]. A multi‐institutional cohort study of 325 advanced cancer patients found that patients who recognized their illness was terminal were more likely to prefer symptom‐based care and they also received end‐of‐life care consistent with their preference [6]. A concept of “good death” was described as a product of psychosocial preparation including being able to say goodbye to important people in one's life, resolving unfinished business matters, and having a general sense of completion. Aggressive treatment in the last days and weeks of life may reduce the patient's opportunity to prepare for this [7]. Preparedness for death may also decrease long‐term anxiety rates and allow for grief resolution for caregivers [8], [9].
Factors that may explain physicians’ reluctance to deliver bad news include fear of destroying hope, fear of provoking emotional distress, including the physician's own, and overestimating the patient's understanding of their disease [4], [10], [11]. In a randomized crossover study conducted by our group on 100 advanced cancer patients watching a physician deliver a less optimistic (LO) versus a more optimistic (MO) message, patients perceived the physician who delivered an LO message as less compassionate [12]. Furthermore, in the Cancer Care Outcomes Research and Surveillance study by Weeks et al., the results suggested patients perceived physicians as better communicators when they conveyed an MO view of chemotherapy [13]. These results appear to make it more difficult for physicians to deliver LO news to patients and this brings up a question of how a negative clinical outcome can alter a patient's previous viewpoint of a physician. There have been studies that suggest that patients' perception of quality of care and satisfaction of health care may be affected by clinical outcomes. Paulsen et al., in a study on lumbar spinal stenosis patients undergoing posterior decompression surgery, and Prakash, in an article related to factors of patient satisfaction in a dermatological practice, suggested that decreased patient satisfaction may result when outcomes do not occur as patients expect [14], [15].
Because patients' information preferences change over the course of a disease [10], [16], [17], it would be important to determine if knowing the clinical outcome would affect their perception of the physicians delivering the MO versus the LO messages. The primary objective of this study was to determine the change in perception of physician compassion after exposing the patient randomly to a vignette depicting that the patient had continued to decline and is enrolled in hospice. We hypothesized that the physician giving the MO message would be perceived as less compassionate once the negative outcome becomes evident and the physician giving the LO message would be perceived as more compassionate. Secondary objectives included determining demographic and clinical predictors of physician compassion, determining patients' perception of physician professionalism, impression of physician, physician's level of hopefulness, and preference of the physician for themselves or their family after the vignette.
Materials and Methods
The Institutional Review Board at The University of Texas MD Anderson Cancer Center approved this study and all patients gave written informed consent.
Patient Population
Eligible patients who attended the outpatient Supportive Care Clinic at MD Anderson Cancer Center were screened and subsequently asked to participate. Patients were included if they were 18 years or older, English‐speaking, and had a diagnosis of advanced cancer, defined as locally advanced, recurrent, or metastatic. Patients with impaired cognition as determined by the research coordinator based on the ability to understand the nature of the study and consent process and those suffering from severe psychiatric disorder or condition capable of significantly interfering with study participation as determined by the principal investigator or the attending supportive care physician were excluded. The potential participants were informed that the messages they would view were not in any way a reflection of their current disease process.
Intervention
Scripted videos were utilized to deliver the intervention following the five phases recommended by Hillet and Van Vliet: appropriateness of video‐vignette, development of valid script and manipulations, conversion to video, and administering the videos [18], [19]. The videos were created with the assistance of the University of Texas Television, including provision of the actors. These were the same videos used in the previous perception of compassion study [12].
After randomization, all patients watched one video depicting a physician actor providing either the MO or the LO message to the same patient actor. Accompanying caregivers were asked to step out or keep silent throughout the study. Each video lasted approximately 4 minutes and showed a professional physician actor discussing treatment and prognostic information with a professional patient actor with advanced cancer, who had received several lines of chemotherapy, had poor performance status, and who was not a good candidate for further therapy. In one video, the physician provided explicit information about the lack of further treatment options (Less Optimistic). In the other video, the physician added vague information about possible future treatments, including a statement considering the possibility of further treatments if the patient improved in functional status (More Optimistic).
In each video, the physician role was played by the same professional actor, with physical characteristics as male, middle‐aged, and white, which the investigators felt depicted a typical physician in our institution. In both videos, the actor acted with the same body language and delivery of both messages, including the same number of empathic statements (five) and nonverbal communication. An independent review of the videos was previously done without sound by three of the authors to ensure that the physician's expression and body posture when delivering the different messages was similar. Reviewers also compared the performance of the actor in both videos by listening only to the audio to assess for any possible voice bias. In all the videos, the patient was portrayed by the same actress: a white woman around 50–60 years of age. The actress acted the same way in both videos, with the same tone of voice and facial expressions, minimal head nodding, and a similar script, and the only difference was her response to the physician's MO versus LO message in the end of the video. In both videos, the camera angle alternated between a wide shot and medium close‐up, focusing more on the physician but alternating to the patient at times when she spoke.
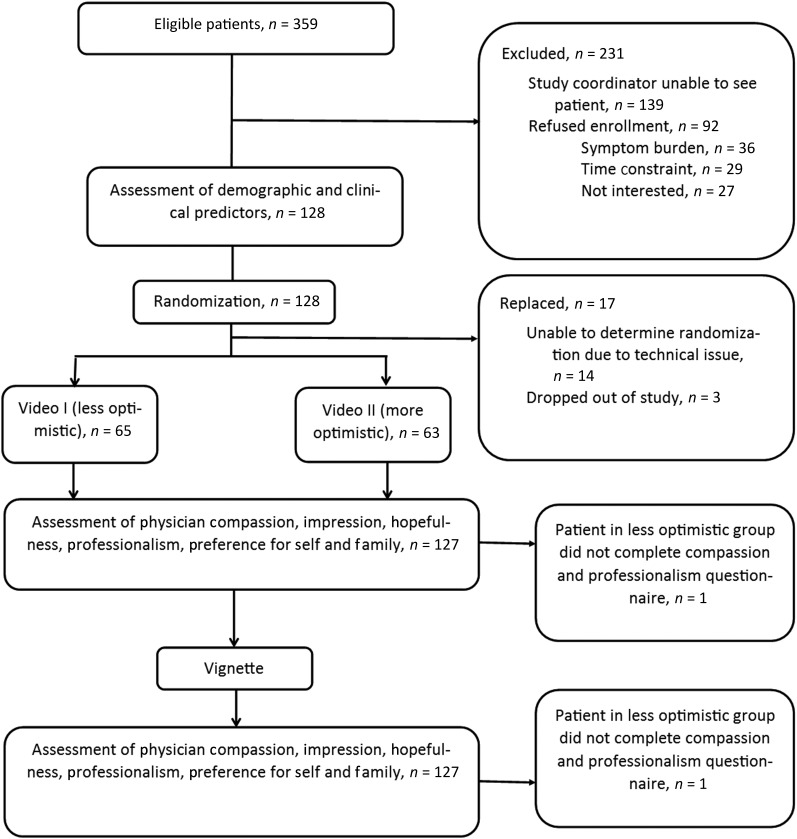
After watching the video, all patients read the same vignette stating that the patient's condition continued to worsen; she was now dependent on friends and family for her care and was enrolled in hospice care at home. Study design is depicted through consort diagram in Figure 1.
Figure 1.
Consort diagram.
Randomization and Blinding
Using the Clinical Trial Conduct website, patients were randomized equally (1:1) into the two video/doctor sequence arms. The research coordinator was blinded to the allocation sequence throughout the study. Actors and patients were blinded to the specific hypothesis of the study. In the consent process, patients were told that they will be asked to “watch one video, read a post‐video vignette, and complete three sets of surveys: one before the video, one after the video, and one after reading the post‐video vignette.” Although we used survey questionnaires, this study was an experimental design.
Study Outcome Measures
The patients completed three sets of surveys (Fig. 1). In the first set, we assessed patients' demographic, current physical and psychological factors that could influence patients' preferences, including symptom distress scores (Edmonton Symptom Assessment System), general trust in the medical profession, level of optimism‐pessimism, and spirituality/religiosity. We did not repeat other psychosocial factors (anxiety, depression, hopefulness, information preference, current health status, and disease acceptance) that showed no significant effect on patient perception of physician compassion in the previously completed randomized controlled trial [12]. After the video and then after the vignette, the patient evaluated the physician's compassion, professionalism, and preference of physician to provide care for themselves and for their family/friends.
Primary Outcome Measure
Physician Compassion Questionnaire [20–24].
Five‐item tool consisting of five 0–10 numerical rating scales assessing five dimensions: warm‐cold, pleasant‐unpleasant, compassionate‐distant, sensitive‐insensitive, and caring‐uncaring. The sum of the five scales gives a final score of 0 (best) to 50 (worst). Internal consistency is α = 0.92. The scale also includes two items on impression of the physician and physician's level of hopefulness (0 worst, 10 best, respectively), which are part of the secondary outcomes.
Secondary Outcome Measures
Edmonton Symptom Assessment System (ESAS) [25–30].
Ten‐item self‐administered measure assessing symptoms on a 0 (best) to 10 (worst) visual analogue scale. Symptoms measured include pain, fatigue, nausea, anxiety, depression, drowsiness, anorexia, shortness of breath, insomnia, and well‐being.
Trust in Medical Profession [31].
Five‐item scale developed as an abbreviated instrument to measure trust as a key element in a therapeutic relationship. It has an internal consistency of α = 0.87 and total sum of responses scored on a 5 (worst) to 25 (best) scale. Degree of trust was captured as a 10‐point scale, with a higher score signifying less trust (0 best, 10 worst). This scale was used as a baseline measure of trust in the medical profession prior to watching the videos.
Life Orientation Test‐Revised (LOT‐R) [32].
Originally, an eight‐item self‐report measure (plus four filler items) that assessed generalized expectancies for positive versus negative outcomes and had a Cronbach's α of 0.82. It was revised to a 10‐item scale by eliminating 2 items from the original scale, which dealt more with coping style than with positive expectations for future outcomes. The correlation between the original and the revised scale is 0.95.
Santa Clara Strength of Religious Faith Questionnaire [33, 34].
Ten‐item measure of strength of religious faith. It has demonstrated convergent validity and internal consistency of 0.95–0.97 and test‐retest reliability of 0.82–0.93. Scores range from 10 (low faith) to 40 (high faith).
Physician Professionalism Questionnaire [35].
Six‐item questionnaire adapted from the General Medical Council Patient Questionnaire to assess professional performance including patients' perception of the physician's trustworthiness and ability to provide care. The four items that comprised total professionalism include being polite, listening, explaining the condition and treatment to the patient, and involving the patient in treatment decisions. The physician was considered trustworthy and able if the rating was ≥4. Reliability of the original nine‐item questionnaire was α = 0.962.
Global Evaluation of Physician.
Two‐item questionnaire completed after the video and vignette assessing patients' evaluation if they prefer the video physician for themselves and their family. Each item was scored on a 1 (worst) to 5 (best) scale. This has not been validated and was formulated for the purpose of this study.
Statistical Analysis
This study estimated the patients' perception change of physician's compassion after watching the video and after reading the post‐video vignette. There are two types of video (LO vs. MO) that patients were randomly assigned to (1:1), and one post‐video vignette that all patients read after watching the video. The primary outcome is physician's compassion score and we expected that two groups’ average compassion scores after watching the video will change in opposite directions after the post‐video vignette. Assuming two group t tests with type I error rate of 5%, a total of 128 patients will give 80% power to detect the difference of 6 in the change of compassion scores between two groups (increase of 3 in MO, decrease of 3 in LO), given a common standard deviation (SD) of 12 in the change of compassion scores. Secondary outcomes included demographic and clinical measurements as predictors of physician compassion, patients' perception of physician's professionalism, and patients' preference of the physician watched.
Data were summarized using standard descriptive statistics such as mean, SD, median and range for continuous variables; and frequency and proportion for categorical variables. Association between categorical variables was examined by chi‐square test or Fisher's exact test when appropriate. Wilcoxon rank‐sum test was used to examine the difference in continuous variables between groups. Wilcoxon signed‐rank test was used to examine the change in continuous variables measured after watching the video and after reading the post‐video vignette within each group. McNemar's test was applied on paired dichotomous variables to evaluate the change on marginal homogeneity. Cohen's Kappa coefficient was used to measure agreement for categorical variables. All computations were carried out in SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
One hundred twenty‐eight patients were randomized between October 2015 and October 2016 and all were evaluable. Patient characteristics are summarized in Table 1. Median age was 61 years and 56% were female. Fourteen patients were unable to be analyzed due to a software issue that prevented us from identifying their randomization and these patients had to be replaced, one patient failed to complete the physician compassion questionnaire, and three patients dropped out of the study (Fig. 1).
Table 1. Patient demographic and clinical characteristics (n = 128).
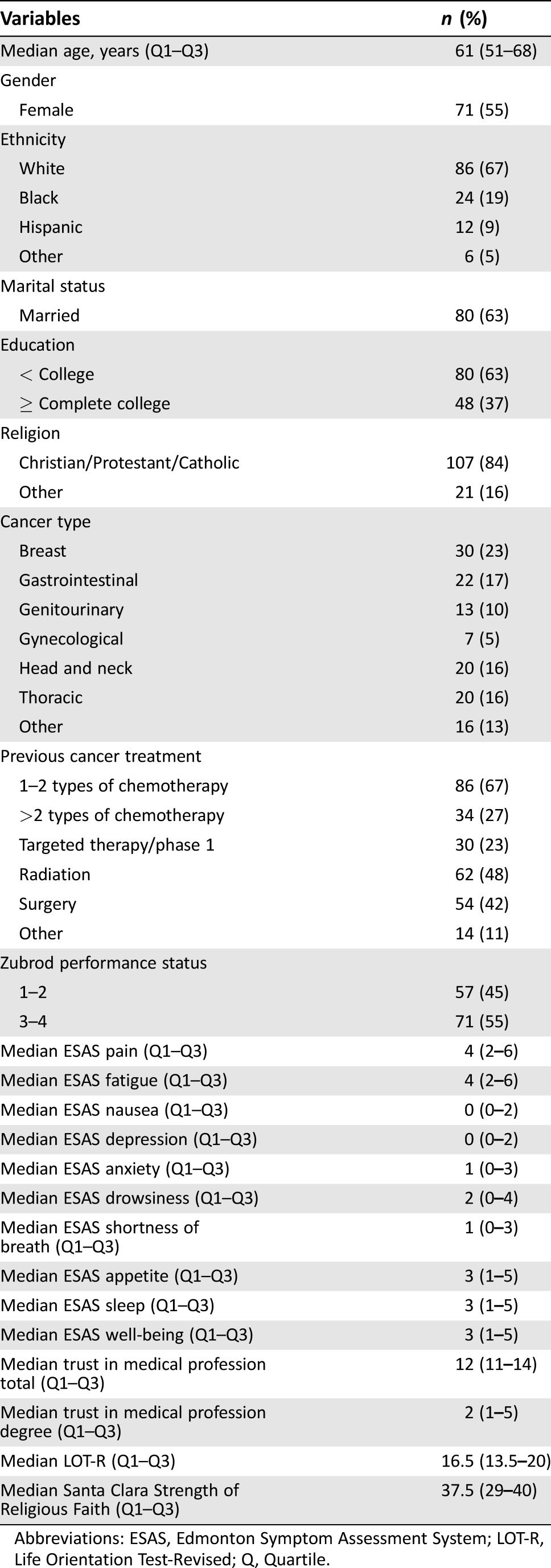
Abbreviations: ESAS, Edmonton Symptom Assessment System; LOT‐R, Life Orientation Test‐Revised; Q, Quartile.
Primary Outcome
Table 2 shows the compassion scores after the video and vignette. No significant difference was found in perception of compassion after the vignette within the MO (p = .4684) and LO (p = .1225) groups, between the MO and LO groups (p = .4036), and when all patients were combined (p = .0994).
Table 2. Compassion scores in more optimistic, less optimistic, and all patients.
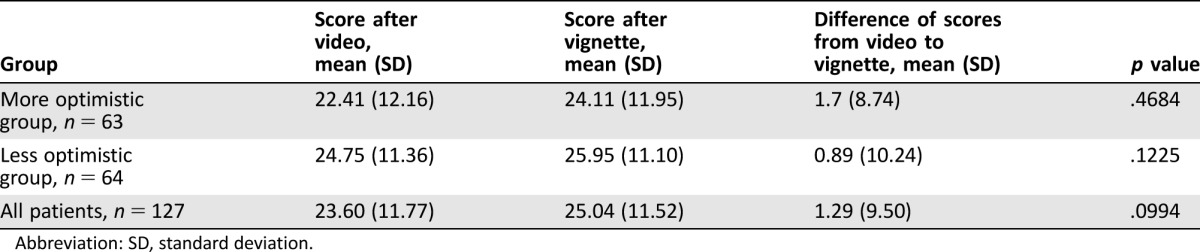
Abbreviation: SD, standard deviation.
Secondary Outcomes
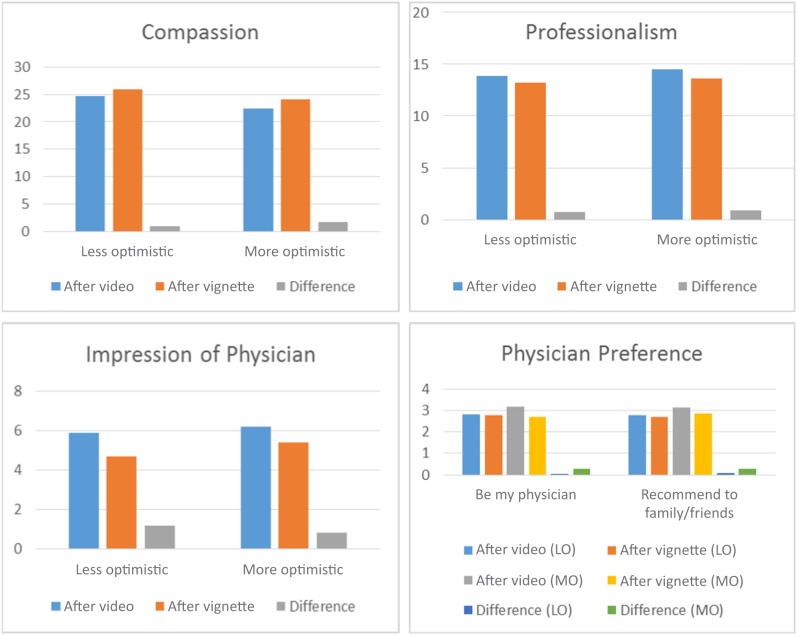
Table 3 summarizes the difference in other outcomes after the vignette. Figure 2 summarizes the compassion, professionalism, impression of physician, and physician preference mean scores within the two groups. There was a significant decrease in the impression of the physician within the MO (p < .0001) and LO (p < .0001) groups. There was a decrease in total professionalism in the MO (p = .0022) and LO (p = .0094) groups (Table 3). With all patients combined, there continued to be a significant decrease for total professionalism (p = .0001). Certain items comprising total professionalism also showed significant decrease: listening (mean difference [SD]: MO −0.21 [0.66], p = .0121; LO −0.22 [0.84], p = .0491) and explaining the condition and treatment to the patient (mean difference [SD]: MO −0.35 [0.88], p = .0013). With all patients combined, items that showed a significant decrease included the following: being polite (mean difference [SD] −0.15 [0.69], p = .0163); listening (mean difference [SD] −0.22 [0.76], p = .0016); and explaining the condition and treatment to the patient (mean difference [SD] −0.26 [0.87], p = .0009).
Table 3. Change in scores of other outcomes from video to vignette.
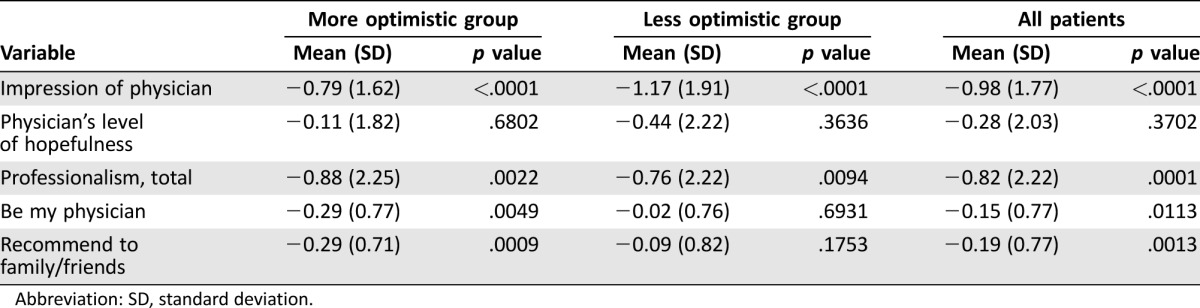
Abbreviation: SD, standard deviation.
Figure 2.
Summary of compassion, professionalism, impression, and preference scores within each group.
Abbreviations: LO, less optimistic; MO, more optimistic.
Between the MO and LO groups, there was no significant difference in change of scores of professionalism (p = .8146) and impression of the physician (p = .1596). There was also no significant difference in scores of physician's level of hopefulness, trustworthiness, and ability to provide care.
Table 3 shows that the MO message group had worse patient preference for the physician for themselves and their family, whereas there was no significant decrease among the LO message group. The observed deterioration in scores for the total group was due to the deterioration in the MO message group.
Total trust in medical profession scores showed significant association with perception of physician compassion (p = .0545). There were no other demographic and clinical predictors that were found to have a significant association with physician compassion, including ESAS, LOT‐R, and Santa Clara Strength of Religious Faith Questionnaire.
Discussion
In this randomized controlled trial, we found that a vignette showing a clinical outcome did not significantly change the compassion score. Our initial hypothesis was that there would be an increase in compassion for the LO group and worsening in perception of compassion in the MO group after the negative clinical outcome. However, the outcome did not change the perception of compassion. This finding suggests that patients' perception of physician compassion is not affected by the clinical outcome.
On the other hand, there was significant deterioration in impression and perception of professionalism for both physicians after patients read the vignette describing the negative outcome. These findings suggest that it was the negative patient outcome rather than the inaccurately optimistic message that resulted in the deterioration in physician image. More research is needed to better characterize the impact of both excessively optimistic message and negative outcomes in patient perception of compassion.
Our finding showing that patients were less likely to choose for themselves and their family the physician with the MO message suggests that there may be a higher level of dissatisfaction, although at the same time, the perception of compassion was not significantly different. We believe this is an important finding because as society becomes more results‐driven and patient experience becomes an important component of health care evaluation, those patients who experience a negative outcome may likely be dissatisfied with their physician.
Robinson et al., in audio‐recorded encounters between 51 oncologists and 141 advanced cancer patients, described that oncologists made more optimistic statements than pessimistic ones. On the other hand, they also described that there was better understanding by patients of the chance of cure when the physician provided a statement of pessimism, such as not having good chemotherapy options and the possibility that those that are available could likely cause more harm than benefits [36]. In a study on 590 patients with metastatic, progressive solid malignancies with median survival of 5.4 months, Enzinger et al. also demonstrated the association between realistic prognostic disclosures and more realistic patient estimate of life expectancy [37]. Our current findings suggest that a negative outcome does not significantly affect the perception of compassion. However, it negatively impacted the perception of the physician, professionalism, and likelihood of physician preference. Further research is necessary to understand the complex association between the content of the message, clinical outcome, and overall impression of compassion and professionalism.
One possible explanation for the waning scores of both groups after the clinical vignette might be the way in which a poor patient outcome and bad news impacts the patient's expectations, which may be one of the more distressing aspects in cancer care. Other authors have described the impact of patient expectations on patient satisfaction as well as their understanding of treatment goals and prognosis [13], [38], [39].
One limitation of the study is that the video only demonstrated one encounter between the patient and the physician. It is possible that the impact of the clinical outcome on patients' perception of professionalism, overall impression, and likelihood to choose the physician might be less when a long‐term relationship has been established and good rapport is present between physician and patient. However, in clinical practice, it is not uncommon that conversations between prognosis and outcome take place after a limited number of encounters. Our study addresses these situations and focuses on relationship impact on that rapport when the clinical outcome is not favorable. Similarly, although the clinical vignette/outcome can be given in another visit, we were concerned about potential bias of recall of the videos between clinic visits by the patient. We were reassured by the observations that the outcome did modify the opinion of the two physicians and that the vignette had the ability to promote change in patients' opinions. More research would be needed to continue to study the appropriate timing of demonstrating the intervention in video studies. Another limitation may be that the clinical outcome may not have been grave enough to influence a complete change of perception of physician compassion and other attributes. It would be interesting to study if an outcome that is considerably worse than hospice, such as death of the patient, was presented and its effect on scoring of the different physician attributes. In addition, the study was conducted on patients with advanced cancer who have had multiple courses of treatments and may have been personally exposed to the delivery of bad news on multiple occasions. It is possible that the results would be different for healthy patients or patients at earlier stages in the disease trajectory. Finally, certain studies conducted in different patient populations suggest that patients preferred either a shared or an active decision‐making preference over a passive one [36], [40]. However, studies have found that patients who preferred a certain decision‐making strategy were satisfied with the way decisions were made in their care even when actual decision‐making may be different from their preferred role [41], [42]. Further studies investigating the preferred and perceived decision‐making role of patients and their influence in perception of different physician attributes would be worthwhile.
Conclusion
The perception of physician compassion did not change after a worse clinical outcome. However, there was a worse perception of professionalism and overall impression in both groups after a worse clinical outcome. In the MO message group, the outcome also decreased preference of physician for themselves or their family.
Acknowledgments
This study was supported by Departmental funds. We thank Susan Frisbee‐Hume, Janet Williams, Vera de la Cruz, Julio Allo, Kresnier Perez, and Margeaux Epner for their assistance during this study, especially for provision of study material and collection/assembly of data.
Contributed equally
Author Contributions
Conception/design: Kimberson Tanco, Ahsan Azhar, Wadih Rhondali, Alfredo Rodriguez‐Nunez, Walter Baile, Eduardo Bruera
Provision of study material or patients: Eduardo Bruera
Collection and/or assembly of data: Kimberson Tanco, Ahsan Azhar, Diane Liu, Jimin Wu, Eduardo Bruera
Data analysis and interpretation: Kimberson Tanco, Ahsan Azhar, Diane Liu, Jimin Wu, Eduardo Bruera
Manuscript writing: Kimberson Tanco, Ahsan Azhar, Eduardo Bruera
Final approval of manuscript: Kimberson Tanco, Ahsan Azhar, Wadih Rhondali, Alfredo Rodriguez‐Nunez, Diane Liu, Jimin Wu, Walter Baile, Eduardo Bruera
Disclosures
The authors indicated no financial relationships.
References
- 1. Bruera E. Process and content of decision making by advanced cancer patients. J Clin Oncol 2006;24:1029–1030. [DOI] [PubMed] [Google Scholar]
- 2. Kearney MK, Weininger RB, Vachon ML et al. Self‐care of physicians caring for patients at the end of life: “Being connected… a key to my survival”. JAMA 2009;301:1155–1164, E1. [DOI] [PubMed] [Google Scholar]
- 3. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363:312–319. [DOI] [PubMed] [Google Scholar]
- 4. Friedrichsen M, Milberg A. Concerns about losing control when breaking bad news to terminally ill patients with cancer: physicians' perspective. J Palliat Med 2006;9:673–682. [DOI] [PubMed] [Google Scholar]
- 5. Weeks JC, Cook EF, O'Day SJ et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences. JAMA 1998;279:1709–1714. [DOI] [PubMed] [Google Scholar]
- 6. Mack JW, Weeks JC, Wright AA et al. End‐of‐life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 2010;28:1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Steinhauser KE, Christakis NA, Clipp EC et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284:2476–2482. [DOI] [PubMed] [Google Scholar]
- 8. Valdimarsdottir U, Helgason AR, Furst CJ et al. Awareness of husband's impending death from cancer and long‐term anxiety in widowhood: a nationwide follow‐up. Palliat Med 2004;18:432–443. [DOI] [PubMed] [Google Scholar]
- 9. Hauksdottir A, Steineck G, Furst CJ et al. Long‐term harm of low preparedness for a wife's death from cancer–a population‐based study of widowers 4–5 years after the loss. Am J Epidemiol 2010;172:389–396. [DOI] [PubMed] [Google Scholar]
- 10. Russell BJ, Ward AM. Deciding what information is necessary: do patients with advanced cancer want to know all the details? Cancer Manag Res 2011;3:191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Meier DE, Back AL, Morrison RS. The inner life of physicians and care of the seriously ill. JAMA 2001;286:3007–3014. [DOI] [PubMed] [Google Scholar]
- 12. Tanco K, Rhondali W, Perez‐Cruz P et al. Patient perception of physician compassion after a more optimistic versus a less optimistic message: A randomized controlled trial. JAMA Oncol 2015;1:176–183. [DOI] [PubMed] [Google Scholar]
- 13. Weeks JC, Catalano PJ, Cronin A et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Paulsen RT, Bouknaitir JB, Fruensgaard S et al. Prognostic factors for satisfaction after decompression surgery for lumbar spinal stenosis. Neurosurgery 2017. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15. Prakash B. Patient satisfaction. J Cutan Aesthet Surg 2010;3:151–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mistry A, Wilson S, Priestman T et al. How do the information needs of cancer patients differ at different stages of the cancer journey? A cross‐sectional survey. JRSM Short Rep 2010;1:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Parker SM, Clayton JM, Hancock K et al. A systematic review of prognostic/end‐of‐life communication with adults in the advanced stages of a life‐limiting illness: Patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage 2007;34:81–93. [DOI] [PubMed] [Google Scholar]
- 18. Hillen MA, van Vliet LM, de Haes HC et al. Developing and administering scripted video vignettes for experimental research of patient‐provider communication. Patient Educ Couns 2013;91:295–309. [DOI] [PubMed] [Google Scholar]
- 19. van Vliet LM, Hillen MA, van der Wall E et al. How to create and administer scripted video‐vignettes in an experimental study on disclosure of a palliative breast cancer diagnosis. Patient Educ Couns 2013;91:56–64. [DOI] [PubMed] [Google Scholar]
- 20. Fogarty LA, Curbow BA, Wingard JR et al. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol 1999;17:371–379. [DOI] [PubMed] [Google Scholar]
- 21. Bruera E, Palmer JL, Pace E et al. A randomized, controlled trial of physician postures when breaking bad news to cancer patients. Palliat Med 2007;21:501–505. [DOI] [PubMed] [Google Scholar]
- 22. Strasser F, Palmer JL, Willey J et al. Impact of physician sitting versus standing during inpatient oncology consultations: Patients' preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage 2005;29:489–497. [DOI] [PubMed] [Google Scholar]
- 23. Rhondali W, Perez‐Cruz P, Hui D et al. Patient‐physician communication about code status preferences: A randomized controlled trial. Cancer 2013;119:2067–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kret DD. The qualities of a compassionate nurse according to the perceptions of medical‐surgical patients. Medsurg Nurs 2011;20:29–36. [PubMed] [Google Scholar]
- 25. Bruera E, Kuehn N, Miller MJ et al. The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care 1991;7:6–9. [PubMed] [Google Scholar]
- 26. Moro C, Brunelli C, Miccinesi G et al. Edmonton symptom assessment scale: Italian validation in two palliative care settings. Support Care Cancer 2006;14:30–37. [DOI] [PubMed] [Google Scholar]
- 27. Nekolaichuk C, Watanabe S, Beaumont C. The Edmonton Symptom Assessment System: A 15‐year retrospective review of validation studies (1991–2006). Palliat Med 2008;22:111–122. [DOI] [PubMed] [Google Scholar]
- 28. Vignaroli E, Pace EA, Willey J et al. The Edmonton Symptom Assessment System as a screening tool for depression and anxiety. J Palliat Med 2006;9:296–303. [DOI] [PubMed] [Google Scholar]
- 29. Watanabe SM, Nekolaichuk CL, Beaumont C. The Edmonton Symptom Assessment System, a proposed tool for distress screening in cancer patients: Development and refinement. Psychooncology 2012;21:977–985. [DOI] [PubMed] [Google Scholar]
- 30. Kang JH, Kwon JH, Hui D et al. Changes in symptom intensity among cancer patients receiving outpatient palliative care. J Pain Symptom Manage 2013;46:652–660. [DOI] [PubMed] [Google Scholar]
- 31. Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res 2005;5:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self‐mastery, and self‐esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67:1063–1078. [DOI] [PubMed] [Google Scholar]
- 33. Plante TG, Boccaccini MT. The Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychol 1997;45:375–387. [Google Scholar]
- 34. Sherman AC, Simonton S, Adams DC et al. Measuring religious faith in cancer patients: Reliability and construct validity of the Santa Clara Strength of Religious Faith questionnaire. Psychooncology 2001;10:436–443. [DOI] [PubMed] [Google Scholar]
- 35. Campbell JL, Richards SH, Dickens A et al. Assessing the professional performance of UK doctors: An evaluation of the utility of the General Medical Council patient and colleague questionnaires. Qual Saf Health Care 2008;17:187–193. [DOI] [PubMed] [Google Scholar]
- 36. Robinson TM, Alexander SC, Hays M et al. Patient‐oncologist communication in advanced cancer: Predictors of patient perception of prognosis. Support Care Cancer 2008;16:1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Enzinger AC, Zhang B, Schrag D et al. Outcomes of prognostic disclosure: Associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol 2015;33:3809–3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bjertnaes OA, Sjetne IS, Iversen HH. Overall patient satisfaction with hospitals: Effects of patient‐reported experiences and fulfilment of expectations. BMJ Qual Saf 2012;21:39–46. [DOI] [PubMed] [Google Scholar]
- 39.PEBC's Ovarian Oncology Guidelines Group . A systematic review of patient values, preferences and expectations for the treatment of recurrent ovarian cancer. Gynecol Oncol 2017;146:392–398. [DOI] [PubMed] [Google Scholar]
- 40. Singh JA, Sloan JA, Atherton PJ et al. Preferred roles in treatment decision making among patients with cancer: A pooled analysis of studies using the Control Preferences Scale. Am J Manag Care 2010;16:688–696. [PMC free article] [PubMed] [Google Scholar]
- 41. Noguera A, Yennurajalingam S, Torres‐Vigil I et al. Decisional control preferences, disclosure of information preferences, and satisfaction among Hispanic patients with advanced cancer. J Pain Symptom Manage 2014;47:896–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med 2001;52:1865–1878. [DOI] [PubMed] [Google Scholar]