Abstract
We present a case of bronchial injury following bougie-assisted endotracheal intubation in a patient with difficult airway scheduled to undergo right percutaneous nephrolithotomy under general anaesthesia. The patient developed pleuritic pain along with right pleural effusion on the third postoperative day which was diagnosed by the anaesthesiologist who was following up the patient for airway trauma-associated complications. However, the patient was diagnosed to have a nephropleural fistula, a rare complication of supracostal access to percutaneous nephrolithotomy, which was managed successfully.
Keywords: anaesthesia, urological surgery
Background
The gum elastic bougie was first introduced by Dr P Hex Venn in 19731 which later became popular as the Eschmann tracheal introducer due to its unique design. The gum elastic bougie is a lengthy flexible catheter that is useful as an endotracheal tube introducer during either videolaryngoscopy or direct laryngoscopy2 and remains an essential component of most difficult airway carts.3
Despite being a reliable aid to endotracheal intubation, tracheal introducers have been known to cause airway injuries such as pharyngeal perforation, mainstem bronchus bleeding, perforation of the tracheal mucosa and tracheal abrasion associated with haemopneumothorax.4 We present a case of bougie-associated bronchial injury followed by postoperative respiratory complications due to the formation of a nephropleural fistula after an uneventful percutaneous nephrolithotomy (PCNL) under general anaesthesia.
Case presentation
A 48-year-old man with no previous comorbidities was scheduled for right-sided PCNL for staghorn renal calculus. All his investigations were normal. Airway examination revealed modified Mallampati class 3 and short neck.
Anaesthesia was induced with fentanyl and propofol followed by atracurium for muscle relaxation. In view of anticipated difficult airway, C-MAC videolaryngoscope was used for intubating the patient. Videolaryngoscopy revealed a large unliftable epiglottis completely covering the glottic aperture. The VBM single-use bougie (VBM Medizintechnik GmbH) was passed successfully in the first attempt till 25 cm mark as visualised during videolaryngoscopy. The ‘clicking sign’ was positive. But the ‘tracheal hold up sign’ was not used. Size 8.0 mm internal diameter cuffed endotracheal tube was railroaded over the bougie. On withdrawing the bougie, a drop of blood was seen at the tip. Endotracheal suctioning was done which was blood stained. There was no fall in oxygen desaturation or increase in peak airway pressures. Auscultation revealed normal breath sounds and adequate ventilation was achieved. A bronchoscopy was performed to rule out any significant injury. Mucosal injury was visualised in the right main stem bronchus just proximal to the take-off point of the upper lobe bronchus on the anterior wall (figure 1). Further endotracheal suctioning was done till a clear field was observed. It was decided to proceed with the surgical procedure since adequate ventilation could be achieved. The procedure was completed successfully using a supracostal superior calyceal access achieving complete stone clearance and a nephrostomy tube and double J (DJ) stent were left in place.
Figure 1.
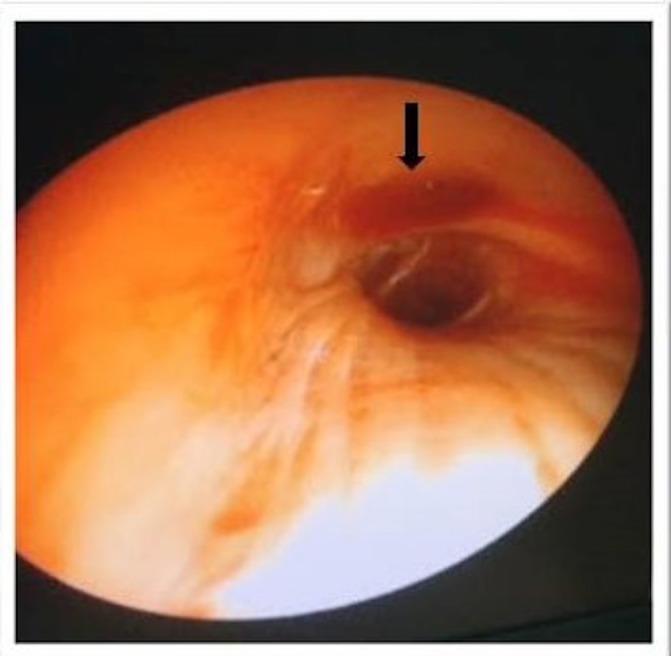
Mucosal ulceration on the anterior wall of the right bronchus.
In the postoperative room, a bedside ultrasound scan of the chest was performed and pneumothorax/haemothorax was ruled out. The patient was followed up in the postoperative period subsequently for the presence of haemoptysis or any respiratory distress. He remained asymptomatic and the nephrostomy tube was removed on day 2. On day 3, the patient started complaining of shortness of breath and chest pain on the right side of the chest. Repeat chest X-ray showed blunting of the right costophrenic angle (figure 2). Bedside lung ultrasonography was done, which revealed small fluid collection on the right side.
Figure 2.
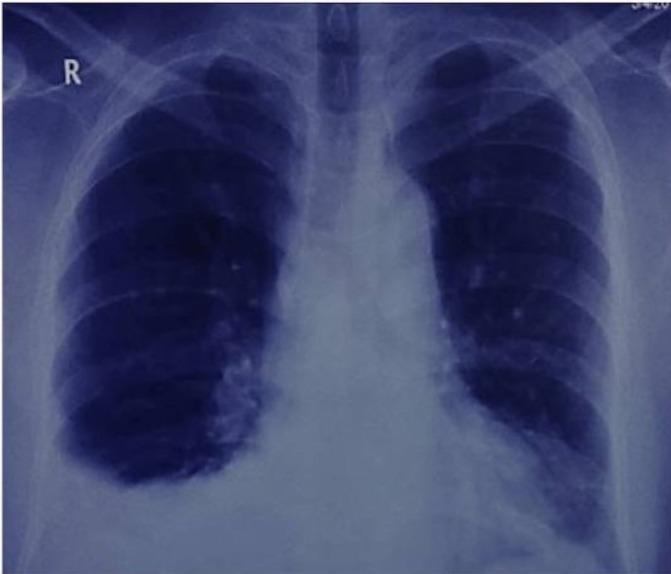
Chest X-ray showing right-sided pleural effusion.
Outcome and follow-up
After discussion with the surgical team, a diagnosis of post-PCNL nephropleural fistula was made owing to the supracostal puncture technique used for PCNL with a delayed presentation of pleural effusion which appeared after the removal of the nephrostomy tube and the uretheral catheter. The renal collecting system was decompressed by inserting a uretheral catheter to keep the bladder empty and thereby prevent reflux via the DJ stent. In view of minimal respiratory distress and small size of the collection, the patient was kept on conservative management only. Patient’s pleural effusion resolved spontaneously over the period of next 3 days. The patient was subsequently discharged on the sixth postoperative day.
Discussion
Ease of use even in the hands of novice users, portability and low cost are some of the factors which attribute to the success and continued use of a bougie in anaesthetic practice. Furthermore, it is also used for extubation of difficult airways and for placement of second generation supraglottic airway devices like the Proseal laryngeal mask airway.5 6
Conventional anesthesiology training is that during blind insertion of the bougie, the tracheal ‘click sign’ and the ‘hold up’ sign should be elicited. Tracheal clicks are produced as the bougie passes over the tracheal cartilages. Hold up sign is the resistance felt when the tip of the bougie reaches the small bronchi. However, the use of these signs has been questioned by many, and the use of bougie is not without risks. There have been reports of bronchial lacerations and development of pneumothorax or haemothorax with the use of the bougie.7–10
In our patient, airway trauma probably occurred during inadvertent advancement of the bougie while railroading the endotracheal tube over it. Another contributing factor could be the use of single-use bougie which is less flexible than the traditional Eschmann introducer. The incidence of injury is reportedly greater with the single-use devices owing to their reduced flexibility and flattened tip.8 11 However, early detection of injury and fibreoptic visualisation of the tracheobronchial tree to rule out major injury prevented significant morbidity in our patient. In the event of any significant injury, appropriate interventions could have been taken well in time to avoid patient morbidity.
Postoperative pulmonary complications are quite common after supracostal access to PCNL due to accidental puncture of pleural cavity and lung. The most common intrathoracic complications encountered include pneumothorax, haemothorax and hydrothorax.
In our patient, a postoperative chest X-ray and lung ultrasound examination were performed to rule out both immediate post-PCNL-related complications and pulmonary complications following bougie-induced airway trauma.
However, another associated complication of supracostal access that is often not recognised is the development of a nephropleural fistula which usually occurs after the removal of the nephrostomy tube and the urinary catheter.12 Nephropleural fistula is a direct and persistent communication between the intrarenal collecting system and the intrathoracic cavity which may present as late as 1–2 weeks postoperatively.
In our patient, the development of pleural effusion on the ipsilateral side of bronchial injury led to a diagnostic dilemma. It was unclear whether the effusion was due to surgical reasons, or was a grave consequence of bronchial vasculature injury. Since the patient was haemodynamically stable and did not have any other complaints except for pleuritic chest pain, he was managed conservatively by decompressing the renal collecting system. A urethral catheter was placed to help in drainage of the urine to promote closure of the fistulous connection. This report highlights an important although rare complication of PCNL, that is, nephropleural fistula which could be misdiagnosed unless one is aware. A close postoperative follow-up, a practice that is rapidly disappearing from anesthesiologists’ routine, is an extremely important aspect of patient care which positively impacts patients’ outcome.
In conclusion, bougie-assisted endotracheal intubation may lead to airway trauma especially with the single-use devices and all precautions should be taken for early detection and treatment of the complications if any. Airway injury by a bougie during difficult intubation can be prevented by avoiding the ‘hold up’ sign and should be retracted by a few centimetres before railroading the tracheal tube.4 The accidental advancement into smaller airway must be avoided by asking an assistant to hold it during the railroading.13 Innovations like traffic signal bougie may further be of benefit in preventing airway trauma.14 In addition, the diagnosis of nephropleural fistula should be kept in mind following delayed development of respiratory complications like pleuritic pain associated with pleural effusion in a patient with post-PCNL. All causes of postoperative pulmonary complications should be ruled out before presuming a diagnosis, as early recognition and management of a pleural injury is critical to avoid life-threatening situations. In the event of an intraoperative event, the patient should be followed up carefully in the postoperative period to detect any secondary complications or delayed presentation of primary complication.
Learning points.
Endotracheal tube introducer or Bougie may cause airway trauma especially with single-use device or when using the ‘hold up’ sign.
Airway trauma caused by bougies may lead to bronchial lacerations and development of pneumothorax or haemothorax.
Nephropleural fistula is a rare but known complication of percutaneous nephrolithotomy with a supracostal access which is characterised by a pleural effusion.
Both complications occurring in the same patient may delay the diagnosis and hence treatment which emphasises the importance of a close follow-up of a patient postoperatively.
Footnotes
Contributors: AP and VR were responsible for the conduct of anaesthesia and reporting of the work. RR was involved in the reporting of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Venn PH. The gum elastic bougie. Anaesthesia 1993;48:274–5. 10.1111/j.1365-2044.1993.tb06936.x8460822 [DOI] [Google Scholar]
- 2.Jain A, Gray S, Mason J, et al. Saved by the bougie. Ann Emerg Med 2017;70:479–82. 10.1016/j.annemergmed.2017.08.013 [DOI] [PubMed] [Google Scholar]
- 3.Henderson JJ, Popat MT, Latto IP, et al. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia 2004;59:675–94. 10.1111/j.1365-2044.2004.03831.x [DOI] [PubMed] [Google Scholar]
- 4.Sahin M, Anglade D, Buchberger M, et al. Case reports: iatrogenic bronchial rupture following the use of endotracheal tube introducers. Can J Anaesth 2012;59:963–7. 10.1007/s12630-012-9763-z [DOI] [PubMed] [Google Scholar]
- 5.Smith T, Vaughan D. Extubation over a bougie in difficult airways: are we missing a trick? Anaesthesia 2013;68:974–5. 10.1111/anae.12400 [DOI] [PubMed] [Google Scholar]
- 6.Brimacombe J, Keller C, Judd DV. Gum elastic bougie-guided insertion of the ProSeal laryngeal mask airway is superior to the digital and introducer tool techniques. Anesthesiology 2004;100:25–9. 10.1097/00000542-200401000-00008 [DOI] [PubMed] [Google Scholar]
- 7.Higgs A, Goddard C. Bougie trauma: insertion or railroad? Anaesthesia 2009;64:918–9. 10.1111/j.1365-2044.2009.06022.x [DOI] [PubMed] [Google Scholar]
- 8.Staikou C, Mani AA, Fassoulaki AG. Airway injury caused by a Portex single-use bougie. J Clin Anesth 2009;21:616–7. 10.1016/j.jclinane.2009.03.006 [DOI] [PubMed] [Google Scholar]
- 9.Kumar S, Walker R. Bougie-related tension pneumothorax in a neonate. Paediatr Anaesth 2009;19:800–1. 10.1111/j.1460-9592.2009.03064.x [DOI] [PubMed] [Google Scholar]
- 10.Arndt GA, Cambray AJ, Tomasson J. Intubation bougie dissection of tracheal mucosa and intratracheal airway obstruction. Anesth Analg 2008;107:603–4. 10.1213/ane.0b013e318176fe36 [DOI] [PubMed] [Google Scholar]
- 11.Hodzovic I, Latto IP, Henderson JJ. Bougie trauma – what trauma? Anaesthesia 2003;58:192–3. [DOI] [PubMed] [Google Scholar]
- 12.Lallas CD, Delvecchio FC, Evans BR, et al. Management of nephropleural fistula after supracostal percutaneous nephrolithotomy. Urology 2004;64:241–5. 10.1016/j.urology.2004.03.031 [DOI] [PubMed] [Google Scholar]
- 13.Phelan MP. Use of the endotracheal bougie introducer for difficult intubations. Am J Emerg Med 2004;22:479–82. 10.1016/j.ajem.2004.07.017 [DOI] [PubMed] [Google Scholar]
- 14.Paul A, Gibson AA, Robinson OD, et al. The traffic light bougie: a study of a novel safety modification. Anaesthesia 2014;69:214–8. 10.1111/anae.12522 [DOI] [PubMed] [Google Scholar]


