Abstract
In this study, we considered connections between the content of immediate trauma narratives and longitudinal trajectories of negative symptoms, to address questions about the timing and predictive value of collected trauma narratives. Participants (N = 68) were individuals who were admitted to the emergency department of a metropolitan hospital, and provided narrative recollections of the traumatic event that brought them into the hospital that day. They were then assessed at intervals over the next 12 months for depressive and posttraumatic symptom severity. Linguistic analysis identified words involving affect (positive and negative emotions), sensory input (sight, sound, taste, touch, and smell), cognitive processing (thoughts, insights, and reasons), and temporal focus (past, present, and future) within the narrative content. In participants’ same-day narratives of the trauma, past-focused utterances predicted greater decreases in depressive symptom severity over the next year, d = −0.13, whereas cognitive process utterances predicted more severe posttraumatic symptom severity across time points, d = 0.32. Interaction analyses suggested that individuals who used fewer past-focused and more cognitive process utterances within their narratives tended to report more severe depressive and posttraumatic symptom severity across time, ds = 0.31 to 0.34. Overall, these findings suggest that, in addition to other demographics and baseline symptom severity, early narrative content can serve as an informative marker for longitudinal psychological symptoms, even before extensive narrative processing and phenomenological meaning-making have occurred.
Evidence has demonstrated that the way in which traumatic experiences are recalled and narrated is related to symptom expression (Crespo & Fernández-Lansac, 2016; O’Kearney & Perrott, 2006), but little is known about how immediate recall of a traumatic event relates to subsequent symptoms. This is important because initial markers that help predict trajectories of symptoms can lead to more appropriate and individualized interventions following trauma. Thus, in this study, we addressed two critical gaps in the literature. First, we collected individuals’ narratives of a traumatic experience within hours of the event as they awaited treatment in the emergency department (ED) of a hospital. Second, we examined how theoretically significant narrative markers, as expressed in the immediate narratives of trauma, predicted trajectories of depression and posttraumatic symptom severity across the subsequent 12 months.
Narratives provide a window into how individuals are making sense of their experiences (Fivush, 2011; McLean, Pasupathi, & Pals, 2007), and narratives of traumatic experiences have implications for adjustment (e.g., Bedard-Gilligan et al., 2015; Brewin, Dalgeish, & Joseph, 1996; Crespo & Fernández-Lansac, 2016; Helzer, Robins, & McEvoy, 1987). Coherent trauma narratives that express personal growth are linked with concurrent (Merrill, Waters, & Fivush, 2015) and longitudinal (Eid, Johnsen, & Saus, 2005) adjustment. In contrast, trauma narratives with problematic content (e.g., negative affect, rumination) relate to more severe depressive and posttraumatic symptomatology (e.g., Eid et al., 2005; Hellawell & Brewin, 2004).
To date, studies of trauma narratives have typically considered: (a) recollections with more opportunities for memory consolidation, at least 1 week from the occurrence of the trauma, and (b) concurrent, rather than longitudinal, associations between narratives and adjustment. Extant findings have emphasized four areas of narrative content related to symptoms: emotion references, sensory details, cognitive processes, and temporal focus. Recollections of traumas tend to be rich in negative emotions and sensory and/or perceptual information. Emotional and sensory utterances coincide with poorer outcomes, including more severe depression and posttraumatic symptoms (Eid et al., 2005; Hellawell & Brewin, 2004) and may be indicators of being overwhelmed by reexperiencing symptoms. Trauma narratives also include multiple cognitive processing utterances (i.e., “understand,” “cause”); however, ties between cognitive utterances and outcomes of posttraumatic stress disorder (PTSD) and depression are mixed, with studies having found both positive (D’Andrea, Chiu, Casas, & Deldin, 2012) and negative (Greenhoot, Sun, Bunnell, & Lindboe, 2013) associations between cognitive utterances in trauma narratives and psychological symptoms. Expressions of cognitive processing may indicate effortful reflection and understanding (Boals, Banks, Hathaway, & Shuettler, 2011). Alternatively, in certain contexts, cognitive process utterances may reflect a passive and ruminative means of event processing. Rumination involves repeated passive thoughts on negative events that do not contribute to resolution, and it is linked to psychological symptoms (Nolen-Hoeksema, 2000). Thus, it is important to clarify when narrative expressions of cognitive process are more likely to indicate risk for PTSD and depressive symptoms.
The temporal focus of the narrative may be critical in resolving whether cognitive processing is beneficial. Trauma recollections tend to overemphasize the present tense (Hellawell & Brewin, 2004; Jelinek, Randjbar, Seifert, Kellner, & Moritz, 2009), and references to the present coincide with greater psychological symptoms (Römisch, Leban, Habermas, & Döll-Hentschker, 2014), whereas recollections that emphasize the past tense coincide with fewer psychological symptoms (Manne, 2002). These patterns correspond with temporal self-appraisal theory and views of subjective distancing, wherein individuals are motivated to evaluate negative past events as more distant—regardless of objective time—and benefit from distancing the self from painful experiences (Peetz & Wilson, 2008; Wilson & Ross, 2003).
To date, studies of trauma narratives have usually involved delayed recollections of the traumatic event, correlated with concurrent adjustment, which has limited attempts to predict trends of risk (i.e., symptom severity). In the present study, we had the unique opportunity to recruit participants in the ED of a major trauma hospital immediately following traumatic injury, and have them narrate their experience, as well as to collect multiple baseline measures of current symptoms and lifetime history of trauma for each person. Participants’ memory of the trauma within hours of the event may provide insights on initial event processing (Fivush, Graci, & Booker, in press), indicating how individuals are beginning to structure and understand the trauma. After the initial trauma interview, participants were assessed four times across 12 months to provide reports of depressive and posttraumatic symptoms. We examined trajectories of symptoms as a function of the initial trauma narrative. Given previous research, we expected more emotional utterances, sensory/perceptual utterances, and present-tense utterances to predict more severe future symptoms. In contrast, we expected past-tense utterances to predict less severe future symptoms. Given possible maladaptive associations between heightened cognitive processing and temporal utterances that may resemble ruminative forms of reminiscing (Nolen-Hoeksema, 2000), we tested for interactions between cognitive and temporal utterances.
Method
Participants
We recruited 68 adults who were part of a larger study of biomarkers for PTSD. Participants were patients in a Level I trauma center in the ED of a metropolitan hospital in the southeastern United States. All participants had experienced a trauma within the last 13 hours. Participants were included if they were English-speaking, 18 to 65 years of age, endorsed a Criterion A trauma as defined by the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association [APA], 2000), and provided contact information for follow-up visits. Exclusion criteria included: previous hospitalization for mental health reasons, current suicidal ideation, suicide attempts in the past 3 months, current intoxication, or altered mental state during the ED visit. Participants included 28 women (41.2%) and 40 men (58.8%), all of whom were between the ages of 19 and 61 years. There were 46 (67.6%) participants who identified as Black or African American, 15 (22.1%) as White or Caucasian, one (1.5%) as Asian, four (6.0%) as multiracial, and one participant did not provide race/ethnic information. One individual had a grammar school-level education (1.5%), four had completed some high school (5.9%), 18 had completed high school (26.5%), 31 had an associate’s degree or had completed some four-year college (45.6%), 10 had a bachelor’s degree or equivalent training (14.7%), one had completed some graduate school (1.5%), and two had completed a master’s degree or equivalent (2.9%). Trauma categories included motor vehicle crashes (58.2%), physical assaults (9.0%), home accidents (e.g., ceiling collapse; 9.0%), pedestrian accidents (9.0%), motorcycle accidents (6.0%), and sexual assaults (4.4%). At baseline, participants’ data were collected from approximately 1 to 13 hr (mean min = 258.38, SD = 144.21, median min = 225.50) following the trauma experience.
Participants provided written informed consent for all parts of the study. The Institutional Review Boards of Emory University and Grady Memorial Hospital approved the study procedures.
Procedure
As part of a larger study, members of the research team (79% female assessors) approached adult patients who were waiting for outpatient ED appointments at the primary medical care clinics of Grady Memorial Hospital in Atlanta, Georgia to solicit study participation. Of participants who were approached, 82.45% were eligible to participate. Among those eligible, 45.31% consented to participate. Consenting participants completed a 1-hr long research assessment while in the emergency department, and returned for four follow-up assessments at 1, 3, 6, and 12 months after the trauma, as described below. The broader project did not include narrative assessment; therefore, only a subset of 68 participants were asked to explicitly provide a narrative of their traumatic experience. Researchers verbally administered all measures and recorded participants’ verbal responses in Research Electronic Data Capture (RedCAP), a HIPAA-compliant web-based electronic survey tool. Interviews were also recorded using a digital voice recorder; all participants gave written consent for the recording. Voice recordings were later transcribed verbatim and checked for accuracy before further use.
While still in the emergency room (ER), participants were asked, “Can you tell me briefly what happened to you that brought you into the ER today?” Each participant’s complete response was audio recorded and later transcribed. Content analysis included any spontaneously provided discussion of the event. If researchers asked for specific points of elaboration, narrative content was no longer considered spontaneous and additional information was not included for consideration (example narratives can be found in the Appendix; trends of Beck Depression Inventory-II [BDI] and PTSD Stress Symptom Interview [PSS] scores for each example narrative are included as Supplemental Figures). After transcription, we used the Linguistic Inquiry and Word Count program (LIWC; Pennebaker, Boys, Jordan, & Blackburn, 2015) to analyze proportions of words in participants’ narratives. Categories of interest included: (a) cognitive processes (i.e., “cause,” “know,” “ought”); (b) affect (i.e., “happy,” “cried”); (c) perceptual/sensory processes (i.e., “look,” “feeling”); (d) past focus (i.e., “ago,” “did,” “talked”); (e) present focus (i.e., “today,” “is,” “now”); and (f) future focus (i.e., “may,” “will,” “soon”).
These “category dictionaries” are comprised of hundreds of words based on previous versions of the LIWC, updates in published dictionaries and thesauruses, and feedback and ratings from independent judges. Each category had reliabilities tested based on representation and fit within 181,000 text samples (e.g., blogs, The New York Times, natural speech, Twitter; see Pennebaker et al., 2015, for details). Spearman-Brown reliabilities previously calculated for these categories include: Cronbach’s α = .92 for cognitive processes, Cronbach’s α = .57 for affect, Cronbach’s α = .55 for perceptual/sensory processes, Cronbach’s α = .64 for past-focused utterances, Cronbach’s α = .66 for present-focused utterances, and Cronbach’s α = .68 for future-focused utterances. Validity tests involving writings samples of the college transition and superficial topics (i.e., having a birthday) supported correlations between independent ratings of affective content, cognitive processes, and language-composition content and text analysis results (Pennebaker & Francis, 1996). Tausczik and Pennebaker (2010) have also reviewed topics of validity in text analysis tools such as the LIWC.
Measures
Baseline assessment
At the ED baseline assessment, participants completed the Standardized Trauma Interview (STI; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992) which included demographic information, reports of depressive symptoms on the BDI (Beck, Steer, & Brown, 1996), and prior posttraumatic stress symptoms and trauma history on the Posttraumatic Diagnostic Scale Self-Report (PDS; Foa, Cashman, Jaycox, & Perry, 1997).
Follow-up assessments
Participants returned for follow-up assessments at 1, 3, 6, and 12 months after the ED visit. At each follow-up, participants provided reports of depressive symptoms on the BDI and current posttraumatic symptoms on the PSS (Foa, Riggs, Dancu, & Rothbaum, 1993).
Baseline posttraumatic symptom severity and history
Participants completed the self-report version of the PDS (Foa et al., 1997). Two sections of the PDS were of particular interest in the current study: the first section, which includes a trauma events checklist from 12 possible event categories, which was used to assess trauma history and posttraumatic symptoms related to prior trauma; and the third section, which assesses the severity of 17 posttraumatic symptoms. Symptoms were rated on a 4-point scale in terms of how often each symptom occurs (0 = not at all or only one time, 3 = 5 or more times a week/almost always). Posttraumatic symptom severity was rated by the overall score-reported symptoms; scores less than 10 indicated mild symptom severity, scores between 11 and 20 indicated moderate symptom severity, scores between 21 and 35 indicated moderate-to-severe symptom severity, and scores greater than 35 indicated severe symptoms. Internal consistency has been shown to be acceptable for this measure (Cronbach’s α = .92 for total symptom severity; see Foa et al., 1997).
Depressive symptoms
The BDI (Beck et al., 1996) includes 21 items rated on a 4-point Likert scale (e.g., 0 = I do not feel sad, 3 = I am so sad and unhappy that I can’t stand it). This measure was presented at baseline and each follow-up. Participants rated their symptom severity for the past 2 weeks. Depressive symptom severity was determined by the overall score of reported symptoms: scores between 0 and 9 indicated minimal depression, scores between 10 and 18 indicated mild depression, scores between 19 and 29 indicated moderate depression, and scores between 30 and 63 indicated severe depression. Internal consistency was acceptable across time points (Cronbach’s αs = .89 to .93).
Posttraumatic stress symptoms
The PSS (Foa et al., 1993) is a semistructured interview that includes 17 items, to be answered in relation a specific traumatic event. This measure was given at each follow-up assessment, but not at baseline. Individuals were asked to report on the traumatic event that led to their ED visit, and the number of times they experienced posttraumatic stress symptoms regarding that event in the last 2 weeks (sample item, “Have you had recurrent or intrusive distressing thoughts or recollections about [the event]?”; 0 = not at all, 3 = 5 or more times). From these responses, posttraumatic symptom severity was determined, as well as whether individuals met severity cutoffs for PTSD (endorsing at least one reexperiencing symptom, three avoidance symptoms, and two arousal symptoms at a rating of 1 or greater). Internal consistency was acceptable across time points (Cronbach’s αs = .88 to .91).
Data Analysis
Preliminary analyses included descriptives and correlations. To address the main study question—if and how immediate narratives might predict trajectories of symptoms over time—a series of growth models was tested using hierarchical linear modeling (HLM; model equations can be found in the Supplementary Materials), testing covariate and narrative linguistic pattern effects on the overall intercept, linear time slope, and quadratic time slope. For each model, significant fixed effects (both covariates and linguistic patterns of interest) were retained and carried forward. Following an unconditional growth model (Model 1), we tested five covariate effects on the overall intercept (age, gender, education level, trauma history, and baseline depressive [BDI] or posttraumatic [PDS] symptoms; Model 2). Initial models included only baseline BDI scores among covariates for depression symptoms and only baseline PDS scores among covariates for posttraumatic stress symptoms. We later revisited models with both covariates, given the likelihood for comorbidity between baseline reports. The inclusion of the additional covariate did not detract from previously significant effects from linguistic markers. To avoid additional model complexity, we did not present models with both baseline BDI and PDS scores.
Significant effects were retained, and we then tested seven linguistic effects on the overall intercept (word count, affect, perceptual/sensory, past, present, future, and cognitive processing; Model 3). These same approaches were used for testing effects on the linear (Models 4 and 5) and quadratic time slopes (Models 6 and 7).
Linear time was integer-based (0, 1, 2, 3) and a random effect was included with linear time. Quadratic time was based on the linear time scale (0, 1, 4, 9). Across models, demographics, trauma history, baseline BDI- and PDS-reported symptoms, and narrative linguistic patterns were treated as invariant. The R statistical program was used for analyses (R Core Team, 2016; RStudio Team, 2015) along with the lme4 (Bates, Maechler, Bolker, & Walker, 2015), lmerTest (Kuznetsova, Brockhoff, & Christensen, 2016), and sjPlot (Lüdecke, 2017) packages.
Age, trauma history, and linguistic patterns were mean-centered and standardized to improve interpretability and limit concerns of multicollinearity when testing interaction effects (Dalal & Zickar, 2011). Hence, units for predictors were standard deviations away from the sample mean. Deviance tests determined whether changes in tested effects contributed to significant improvements in model fit. Thus, even in instances in which pseudo-R2 measures did not change drastically between models, it was possible for added new variables to significantly improve the fit of the model to the current data. No models showed significantly poorer fit when nonsignificant effects were removed (ps = .088 to .896). Effect sizes were calculated and are shown in Table 3 and 4 (Raudenbush & Xiao-Feng, 2001). We elected to use HLM because it is an approach that accurately accounts for variance and covariance across multiple levels of data and shows greater power than analyses of variance (ANOVA)-based approaches (Quené & van den Bergh, 2004). Post hoc power analyses were used to determine whether model effects appeared at risk for being insufficiently powered, even if effect sizes were sufficiently large and effect error relatively small.
Table 3.
Retained Fixed Effects on Reported Depressive Symptoms over Time
| Model Effects | ΔDev./Δdf a | AIC | R2b | Est. | SE | 95% CI | d | p | Powerc |
|---|---|---|---|---|---|---|---|---|---|
| Model 1d | -- | 1714.62 | .90 | ||||||
| Int. | 12.60 | 1.20 | [10.21, 14.99] | -- | .000 | -- | |||
| Time | −2.93 | 0.88 | [−4.66,−1.20] | −0.32 | .001 | .997 | |||
| Time2 | 0.71 | 0.26 | [0.20, 1.21] | 0.08 | .007 | .979 | |||
| Model 2e | 7.67** | 1552.07 | .90 | ||||||
| Int. | 6.87 | 1.31 | [4.28, 9.47] | -- | .000 | -- | |||
| Genderf | 3.81 | 1.48 | [0.86, 6.75] | 0.60 | .013 | .976 | |||
| Education | −2.59 | 0.72 | [−4.04, −1.15] | −0.41 | .001 | .999 | |||
| BDI - baseline | 0.43 | 0.09 | [0.25, 0.60] | 0.07 | .000 | .999 | |||
| Trauma History | 1.89 | 0.77 | [0.35, 3.43] | 0.30 | .017 | .979 | |||
| Time | −3.51 | 0.91 | [−5.31, −1.71] | −0.56 | .000 | .999 | |||
| Time2 | 0.89 | 0.27 | [0.36, 1.41] | 0.14 | .001 | .999 | |||
| Model 5g | 5.90* | 1548.36 | .90 | ||||||
| Int. | 7.21 | 1.31 | [4.62, 9.84] | -- | .000 | -- | |||
| Gender | 3.54 | 1.47 | [0.69, 6.47] | 0.56 | .019 | .992 | |||
| Education | −2.80 | 0.72 | [−4.25, −1.35] | −0.44 | .000 | .999 | |||
| BDI - baseline | 0.40 | 0.09 | [0.23, 0.58] | 0.06 | .000 | .999 | |||
| Trauma history | 1.88 | 0.77 | [0.35, 3.40] | 0.30 | .017 | .967 | |||
| Time | −3.46 | 0.90 | [−5.24, −1.67] | −0.55 | .000 | .999 | |||
| Past-focus | −0.79 | 0.32 | [−1.41, −0.16] | −0.13 | .015 | .992 | |||
| Time2 | 0.88 | 0.26 | [0.35, 1.40] | 0.14 | .001 | .999 | |||
| Model 8h | 1.25 | 1542.24 | .90 | ||||||
| Int. | 7.12 | 1.32 | [4.48, 9.79] | -- | .000 | -- | |||
| Gender | 3.73 | 1.56 | [0.59, 6.87] | 0.61 | .020 | .963 | |||
| Education | −2.85 | −1.38 | [−0.73, −4.31] | −0.47 | .000 | .999 | |||
| BDI - baseline | 0.39 | 0.09 | [0.21, 0.56] | 0.06 | .000 | .999 | |||
| Trauma history | 1.92 | 0.78 | [0.37, 3.47] | 0.32 | .016 | .973 | |||
| Cognitive | 0.27 | 0.96 | [−1.64, 2.18] | 0.04 | .780 | .006 | |||
| Past-focus | −1.01 | 1.04 | [−3.08, 1.06] | −0.17 | .337 | .288 | |||
| Cognitive × Past | −1.96 | 0.89 | [−3.73, −0.19] | −0.32 | .031 | .933 | |||
| Time | −3.26 | 0.90 | [−5.03, −1.50] | −0.54 | .000 | .999 | |||
| Cognitive | 0.26 | 0.99 | [−1.43, 2.31] | 0.04 | .796 | .995 | |||
| Past-focus | 0.44 | 0.95 | [−1.70, 2.22] | 0.07 | .643 | .034 | |||
| Cognitive × Past | 2.08 | 0.85 | [0.40, 3.77] | 0.34 | .016 | .971 | |||
| Time2 | 0.84 | 0.26 | [0.31, 1.36] | 0.14 | .002 | .999 | |||
| Cognitive | −0.12 | 0.28 | [−0.67, 0.44] | −0.02 | .677 | .027 | |||
| Past-focus | −0.18 | 0.30 | [−0.77, 0.40] | −0.03 | .536 | .085 | |||
| Cognitive × Past | −0.43 | 0.25 | [−0.93, 0.07] | −0.07 | .091 | .773 |
Note. Continuous variables aside from baseline BDI values and measures of time were standardized. Dev. = model deviance; AIC = Aikaike information criterion; BDI = Beck Depression Inventory.
Deviance tests determine whether model fit significantly improved, given the increase in model complexity.
R2 is a pseudo-R2 statistic based on Snijders & Bosker (2012).
Observed power was calculated as (d / SE) ≈ [Z1−α + Z1−β].
This model tested unconditional growth.
This model tested retained demographic effects on the overall intercept.
For gender, women receive the higher value.
This model tested retained linguistic inquiry and word count effects on the linear time slope.
This model tested interaction effects of cognitive and past-focused utterances on the overall intercept, linear time slope, and quadratic time slope.
p < .05.
p < .01.
Table 4.
Retained Effects on Reported Posttraumatic Stress Symptoms Over Time
| Model Effects | ΔDev./Δdf a | AIC | R2b | Est. | SE | 95% CI | d | p | Powerc |
|---|---|---|---|---|---|---|---|---|---|
| Model 1d | -- | 1753.84 | .93 | ||||||
| Int. | 15.56 | 1.47 | [12.69, 18.43] | -- | .000 | -- | |||
| Time | −4.58 | 0.90 | [−6.34, −2.81] | −0.40 | .000 | .999 | |||
| Time2 | 0.98 | 0.26 | [0.47, 1.49] | 0.08 | .000 | .998 | |||
| Model 2e | 7.11** | 1728.26 | .93 | ||||||
| Int. | 10.71 | 1.58 | [7.57, 13.89] | -- | .000 | -- | |||
| Genderf | 5.19 | 2.19 | [0.61, 9.78] | 0.56 | .020 | .964 | |||
| Education | −2.83 | 1.06 | [−4.97, −0.69] | −0.30 | .009 | .963 | |||
| PDS – baseline | 0.43 | 0.11 | [0.20, 0.66] | 0.05 | .000 | .999 | |||
| Time | −4.62 | 0.89 | [−6.39, −2.86] | −0.49 | .000 | .999 | |||
| Time2 | 0.99 | 0.26 | [0.48, 1.50] | 0.11 | .000 | .999 | |||
| Model 3g | 4.23* | 1723.80 | .93 | ||||||
| Int. | 11.00 | 1.49 | [8.04, 14.00] | -- | .000 | -- | |||
| Gender | 3.85 | 2.13 | [−0.57, 8.27] | 0.44 | .075 | .729 | |||
| Education | −2.71 | 0.99 | [−4.72, −0.70] | −0.31 | .008 | .973 | |||
| PDS – baseline | 0.47 | 0.11 | [0.26, 0.69] | 0.05 | .000 | .999 | |||
| Word count | −2.07 | 1.01 | [−4.07, −0.07] | −0.24 | .044 | .849 | |||
| Cognitive | 2.80 | 1.04 | [0.72, 4.88] | 0.32 | .009 | .996 | |||
| Time | −4.62 | 0.89 | [−6.38, −2.85] | −0.53 | .000 | .999 | |||
| Time2 | 0.99 | 0.26 | [0.48, 1.50] | 0.11 | .000 | .999 | |||
| Model 4h | 4.84* | 1720.96 | .93 | ||||||
| Int. | 10.04 | 1.55 | [6.96, 13.10] | -- | .000 | -- | |||
| Gender | 6.17 | 2.36 | [1.45, 10.85] | 0.72 | .011 | .963 | |||
| Education | −2.69 | 0.99 | [−4.70, −0.68] | −0.31 | .008 | .973 | |||
| PDS – baseline | 0.47 | 0.11 | [0.26, 0.69] | 0.05 | .000 | .999 | |||
| Word count | −2.07 | 1.00 | [−4.07, −0.07] | −0.24 | .043 | .846 | |||
| Cognitive | 2.81 | 1.04 | [0.73, 4.88] | 0.33 | .009 | .970 | |||
| Time | −3.88 | 0.94 | [−5.75, −2.02] | −0.45 | .000 | .999 | |||
| Gender | −1.80 | 0.80 | [−3.39, −0.20] | −0.21 | .029 | .898 | |||
| Time2 | 0.99 | 0.26 | [0.48, 1.51] | 0.12 | .000 | .999 | |||
| Model 8i | 1.28 | 1717.52 | .93 | ||||||
| Int. | 9.87 | 1.58 | [6.90, 12.82] | -- | .000 | -- | |||
| Gender | 7.07 | 2.47 | [2.40, 11.67] | 0.82 | .006 | .981 | |||
| Education | −3.03 | 1.02 | [−4.98, −1.09] | −0.35 | .004 | .988 | |||
| PDS - baseline | 0.41 | 0.11 | [0.20, 0.63] | 0.05 | .000 | .999 | |||
| Word Count | −2.10 | 1.02 | [−4.01, −0.18] | −0.24 | .045 | .834 | |||
| Cognitive | 3.40 | 1.23 | [1.09, 5.70] | 0.40 | .007 | .978 | |||
| Past-focus | −3.29 | 1.37 | [−5.87, −0.71] | −0.38 | .020 | .928 | |||
| Cognitive × Past | −2.70 | 1.18 | [−4.91, −0.49] | −0.31 | .025 | .907 | |||
| Time | −3.80 | 0.98 | [−5.65, −1.90] | −0.44 | .000 | .999 | |||
| Gender | −1.95 | 0.87 | [−3.62, −0.29] | −0.23 | .028 | .900 | |||
| Cognitive | 0.34 | 0.95 | [−1.50, 2.16] | 0.04 | .718 | .011 | |||
| Past-focus | 0.90 | 1.04 | [−1.11, 2.92] | 0.10 | .388 | .154 | |||
| Cognitive × Past | 0.92 | 0.89 | [−0.79, 2.66] | 0.11 | .302 | .261 | |||
| Time2 | 0.99 | 0.26 | [0.48, 1.51] | 0.12 | .000 | .999 | |||
| Cognitive | −0.26 | 0.28 | [−0.79, 0.29] | −0.03 | .356 | .192 | |||
| Past-focus | −0.20 | 0.31 | [−0.80, 0.40] | −0.02 | .516 | .059 | |||
| Cognitive × Past | −0.11 | 0.26 | [−0.62, 0.39] | −0.01 | .664 | .014 |
Note. Continuous variables aside from baseline Beck Depression Index values and measures of time were standardized.
Dev. = model deviance; AIC = Aikaike information criterion; PDS = Posttraumatic Diagnostic Scale.
Deviance tests determine whether model fit significantly improved, given the increase in model complexity.
R2 is a pseudo-R2 statistic based on Snijders & Bosker (2012). For gender, women receive the higher value.
Observed power was calculated as (d / SE) ≈ [Z1−α + Z1−β].
This model tested unconditional growth.
This model tested retained demographic effects on the overall intercept.
For Gender, women receive the higher value.
This model tested retained Linguistic Inquiry Word Count effects on the overall intercept.
This model tested retained demographic effects on the linear time slope.
This model tested interaction effects of cognitive and past-focused utterances on the overall intercept, linear time slope, and quadratic time slope.
p < .05.
p < .01.
Results
Preliminary Analyses
Attrition
Although all recruited participants provided background information and completed the trauma narrative activity, a subset of individuals (n = 6) did not complete all measures, such as the BDI, at baseline due to interruptions related to their medical care, or discharge from the ED. At later time points, subsets of individuals did not return for one or more follow-up sessions. However, 84.8% of individuals returned for all follow-up assessments. Aside from initial uses of affect utterances in trauma narratives, F(4, 61) = 3.43, p = .014, individuals did not show significant differences in demographics or ongoing symptoms based on the number of completed follow-ups. For this sample, data were not imputed, as HLM incorporates all available lower-level data (i.e., time-varying data among individuals; Bryk & Raudenbush, 1992). Hence, approximately 250 observations were available for models, rather than 68.
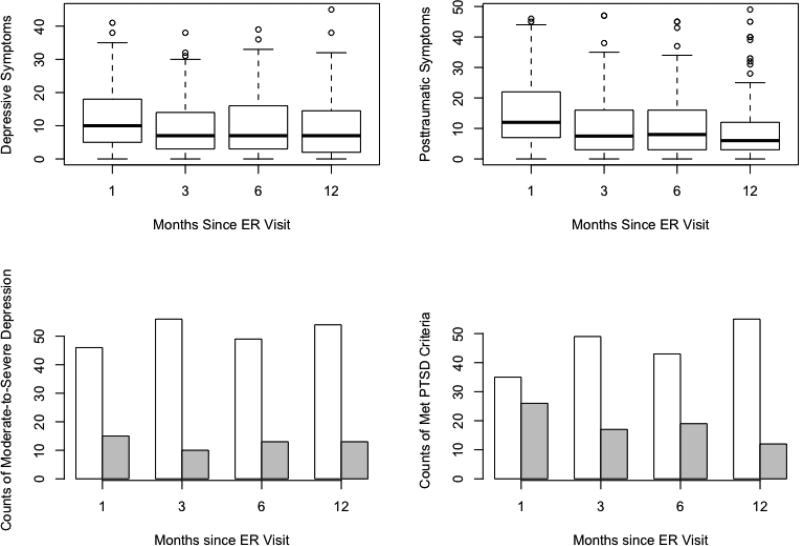
Depressive and posttraumatic symptom severity across time
The percentage of individuals who met the cutoff for moderate-to-severe depressive symptoms (BDI > 19) was 16.2% at baseline, 24.5% at 1-month follow-up, 15.2% at 3-month follow-up, 21.0% at 6-month follow-up, and 19.4% at 12-month follow-up. The percentage of participants who met the cutoff for moderate-to-severe PTSD symptoms (PDS/PSS > 21) was 8.8% at baseline, 42.6% at 1-month follow-up, 25.8% at 3-month follow-up, 30.6% at 6-month follow-up, and 17.9% at 12-month follow-up. Trends in symptoms across follow-up periods are illustrated in Figure 1.
Figure 1.
Trends of depressive and posttraumatic stress disorder (PTSD) symptoms over time. The top left and right plots present boxplots of reported depressive and posttraumatic symptoms, respectively. The bottom left plot presents the counts of individuals who met either minimal/mild (unshaded) or moderate/severe (shaded) depression cutoff criteria at each follow-up. The bottom right plot presents the counts of individuals who either did not (unshaded) or did (shaded) meet cutoffs for PTSD at each follow-up. ER = emergency room.
Preliminary generalized hierarchical linear models, in which we tested main effects of baseline cutoff criteria and linear time and using a logistic approach, suggested that initial moderate-to-severe depression and PTSD cutoffs (Logit Coefficient = 3.87, SE = 1.30, d = 1.35, p = .003; and Logit Coefficient = 5.10, SE = 1.51, d = 2.21, p < .001, respectively) predicted ongoing cutoff criteria for participants, above and beyond the influence of time. Participants who met criteria for moderate or severe baseline criteria were more likely to later meet criteria for moderate or severe depression and PTSD diagnosis, respectively. Because of the robust association with initial cutoff criteria and the limited number of total participants who met later cutoffs, we maintained focus on symptom severity trends, rather than cutoff criteria.
Table 1 presents the variable descriptives. Table 2 presents correlations. Gender, education level, trauma history, and baseline depressive and PTSD symptom severity were associated with baseline and longitudinal depressive and PTSD symptoms. Women, participants with lower education level, participants with more extensive trauma history, and participants with more severe baseline symptom severity reported more severe symptoms across time points.
Table 1.
Descriptive Statistics
| Variable | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, years | 35.67 | 12.37 | 19.00 | 61.00 | |
| Trauma history | 2.09 | 1.78 | 0.00 | 7.00 | |
| Narrative Utterances | |||||
| Word count | 79.94 | 76.97 | 3.00 | 381.00 | |
| Cognitive processes | 7.05 | 6.06 | 0.00 | 33.33 | |
| Affect | 1.26 | 2.06 | 0.00 | 9.52 | |
| Perceptual processes | 2.10 | 2.96 | 0.00 | 12.50 | |
| Past-focused | 10.78 | 5.41 | 0.00 | 40.00 | |
| Present-focused | 4.66 | 4.69 | 0.00 | 18.18 | |
| Future-focused | 12.59 | 10.08 | 0.00 | 41.00 | |
| Beck Depression Inventory | |||||
| Baseline | 62 | 9.79 | 8.89 | 0.00 | 39.00 |
| 1-month follow-up | 61 | 12.59 | 10.08 | 0.00 | 41.00 |
| 3-month follow-up | 66 | 9.48 | 8.74 | 0.00 | 38.00 |
| 6-month follow-up | 62 | 10.40 | 9.82 | 0.00 | 39.00 |
| 12-month follow-up | 67 | 9.90 | 10.16 | 0.00 | 45.00 |
| Posttraumatic Diagnostic Scale | |||||
| Baseline | 68 | 6.22 | 9.49 | 0.00 | 36.00 |
| PTSD Symptom Scale | |||||
| 1-month follow-up | 61 | 15.75 | 12.45 | 0.00 | 46.00 |
| 3-month follow-up | 66 | 11.20 | 11.07 | 0.00 | 47.00 |
| 6-month follow-up | 62 | 11.52 | 11.85 | 0.00 | 45.00 |
| 12-month follow-up | 67 | 10.39 | 12.13 | 0.00 | 49.00 |
Note. PTSD = posttraumatic stress disorder.
Table 2.
Bivariate Correlations Among Study Variables
| Variable | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | 20. | 21. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | ||||||||||||||||||||
|
| ||||||||||||||||||||
| 1. Age | −.10 | .00 | .07 | .06 | −.26* | −.18 | .03 | .01 | −.06 | .10 | .00 | −.21 | .07 | .14 | .08 | .00 | −.04 | .04 | .09 | .05 |
| 2. Gendera | -- | .16 | −.14 | −.20 | .27* | .00 | .24* | .00 | −.13 | −.13 | .32** | −.04 | .29* | .27* | .36** | .24 | .45** | .39** | .34** | .21 |
| 3. Education | -- | .06 | −.26* | −.17 | −.03 | −.05 | −.05 | −.02 | −.10 | −.06 | .39** | −.42* | −.31* | −.45* | −.42** | −.31* | −.31** | −.41** | −.39** | |
| 4. Trauma History | -- | .16 | .51** | .04 | −.19 | −.06 | .09 | −.04 | −.12 | −.30* | .25 | .32** | .17 | .18 | .20 | .21 | .21 | .34** | ||
| 5. Baseline BDI | -- | .49** | .08 | .14 | −.11 | −.10 | −.16 | .22 | −.06 | .62** | .55** | .54** | .46** | .57** | .50** | .53** | .40** | |||
| 6. Baseline PDS | -- | .08 | −.01 | −.17 | .03 | −.11 | .19 | −.22 | .27* | .42** | .38** | .44** | .40** | .47** | .43** | .50** | ||||
| Utterances | ||||||||||||||||||||
| 7. Word Count | -- | .26* | .05 | .07 | −.05 | .21 | .12 | −.16 | −.03 | .02 | −.01 | −.06 | −.11 | −.08 | −.04 | |||||
| 8. Cognitive | -- | −.05 | .03 | −.07 | .66** | .08 | .06 | .08 | .20 | .14 | .30* | .26* | .28* | .13 | ||||||
| 9. Affect | -- | .19 | −.03 | .05 | −.09 | .01 | −.06 | −.01 | .01 | .14 | −.06 | .00 | .04 | |||||||
| 10. Perception | -- | −.10 | .09 | −.08 | −.10 | −.20 | −.16 | .07 | −.11 | −.16 | .13 | −.08 | ||||||||
| 11. Past | -- | −.04 | .02 | −.02 | −.15 | −.25 | −.27* | −.19 | −.18 | −.21 | −.16 | |||||||||
| 12. Present | -- | −.03 | .14 | .04 | .15 | .20 | .34** | .16 | .19 | .08 | ||||||||||
| 13. Future | -- | −.26* | −.18 | −.24 | −.19 | −.29* | −.20 | −.26* | −.20 | |||||||||||
| BDI | ||||||||||||||||||||
| 14. 1 Month | -- | .74** | .68** | .53** | .80** | .66** | .70** | .54** | ||||||||||||
| 15. 3 Months | -- | .83** | .67** | .72** | .82** | .79** | .74** | |||||||||||||
| 16. 6 Months | -- | .85** | .72** | .77** | .90** | .84** | ||||||||||||||
| 17. 12 Months | -- | .58** | .71** | .84** | .87** | |||||||||||||||
| PSS | ||||||||||||||||||||
| 18. 1 Month | -- | .82** | .76** | .65** | ||||||||||||||||
| 19. 3 Months | -- | .86** | .82** | |||||||||||||||||
| 20. 6 Months | -- | .89** | ||||||||||||||||||
| 21. 12 Months | -- | |||||||||||||||||||
Note. BDI = Beck Depression Inventory. PDS = Posttraumatic Diagnostic Scale. PSS = PTSD Symptom Scale.
For gender, women receive the higher value.
p < .05.
p < .01.
Hierarchical Linear Models
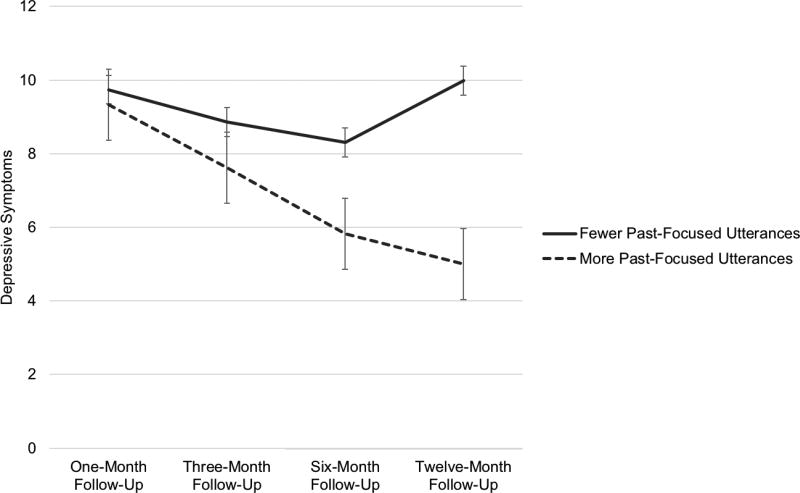
Depressive symptoms
Table 3 depicts the retained fixed effects for patterns of depressive symptoms. There were significant covariate effects on the overall intercept, such that women, participants with a lower education level, participants with more severe baseline depressive symptoms, and participants with more extensive trauma history reported greater average depressive symptoms. Adding the narrative variables to the model indicated that individuals’ uses of past-focused utterances in trauma narratives predicted larger decreases in depressive symptoms over time, over and above these baseline variables. This effect contributed to significant improvement in model fit.
Posttraumatic symptoms
Table 4 depicts the retained effects for patterns of posttraumatic symptoms across follow-ups. There were significant covariate effects on the overall intercept, such that women, participants with a lower education level, and participants with more severe baseline posttraumatic symptoms reported greater average posttraumatic symptoms across follow-ups. Adding the narrative variables to the model accounted for significant improvements in model fit, and participants who provided longer spontaneous trauma narratives reported less severe posttraumatic symptoms on average, whereas those who used more cognitive utterances in trauma narratives reported more severe posttraumatic symptoms on average. There was also a significant covariate effect on the linear time slope, such that women reported greater decreases in posttraumatic symptoms over time.
Interactions of past-focused and cognitive process utterances
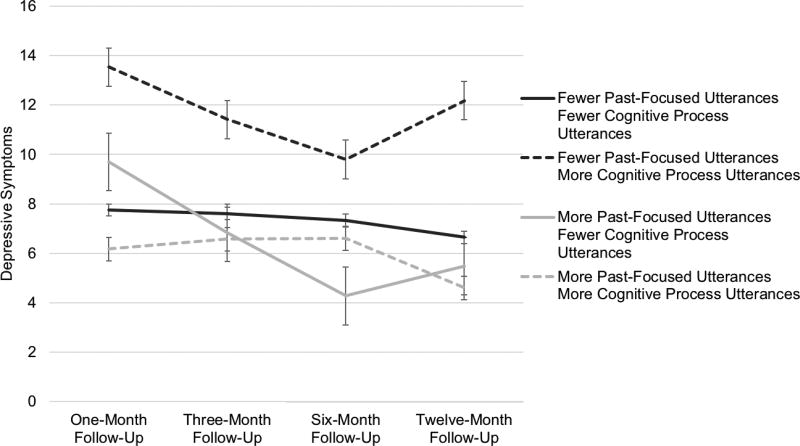
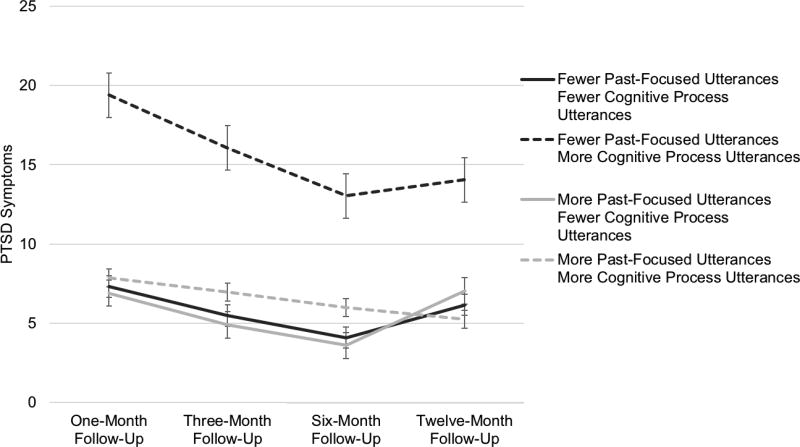
As discussed in the introduction, cognitive process words may reflect different underlying processes depending on the tense; cognitive process words used in conjunction with the present tense, rather than past tense, may signal repetitive and passive responses that are akin to rumination and may be of interest in considering depressive and posttraumatic symptom patterns (Nolen-Hoeksema, 1991, 2000). We explored simultaneous interaction effects on the overall intercept, linear time slope, and quadratic time slope. These effects were tested above and beyond significant covariates.
As shown in Table 3 and depicted in Figure 3, for depressive symptoms, significant interactions were supported on the overall intercept and linear rate of change. Participants who used fewer past-focused and more cognitive process utterances reported the highest levels of depressive symptoms across time points. Despite improvements in symptom severity at 6 months postevent among other participants, those in this group reported increases in symptoms at 12-month follow-up. As shown in Table 4 and depicted in Figure 4, for PTSD symptoms, an interaction was supported on the overall intercept. As with depressive symptoms, participants who used fewer past-focused and more cognitive process utterances reported more severe posttraumatic symptoms than individuals with other patterns of trauma utterances across time points. These trends account for initial posttraumatic symptom severity and demographic factors.
Figure 3.
Patterns of depressive symptoms given interactions of past-focused and cognitive process utterances. Starting values assume participants are men with a mean report of trauma history and education level. Trends depict effects 1 standard deviation below (fewer) or above (more) the mean.
Figure 4.
Patterns of posttraumatic stress disorder (PTSD) symptoms given interactions of past-focused and cognitive process utterances. Starting values and linear trajectories assume participants are men with a mean report of trauma history and education level and mean narrative word count. Trends depict effects 1 standard deviation below (fewer) or above (more) the mean.
Discussion
Past studies have indicated that narrative content can reflect intrusive trauma memories and be related to longitudinal depressive and posttraumatic symptom severity (e.g., Eid et al., 2005; Hellawell & Brewin, 2004; Manne, 2002). Yet, few studies collect narratives shortly after the trauma—before memory is consolidated—or utilize narrative content as a predictor of long-term symptoms. We examined narratives immediately following traumatic injury and used the linguistic content to predict trajectories of depressive and PTSD symptoms over one year. Beyond demographics and developmental history, past-oriented utterances in trauma narratives predicted greater decreases in depressive symptoms over time, whereas cognitive processing utterances in trauma narratives predicted greater average posttraumatic symptoms. Our findings support previous studies considering temporal focus (Hellawell & Brewin, 2004; Manne, 2002) and help clarify the role of cognitive process word patterns. Most important, how individuals immediately begin to create meaning from a traumatic experience predicts symptom trajectories.
That both cognitive process words and temporal focus predicted more severe symptoms over time suggests that some form of injurious cognitive reasoning or reminiscing may begin even as traumatic events occur, and may lead to distress. More specifically, individuals who used more cognitive processing utterances in the context of fewer past-focused utterances were at risk for sustained symptoms across a 12-month period. It is possible that an inability to subjectively distance the self from the experience while simultaneously focusing on internal thoughts may indicate a ruminative form of narrative reasoning immediately after the traumatic experience (Nolen-Hoeksema, 2000; Peetz & Wilson, 2008; Treynor, Gonzalez, & Nolen-Hoeksema, 2003; Wilson & Ross, 2003). That immediate narratives predicted trajectories of symptoms over a 12-month period suggests that phenomenological experiences of rumination and subjective distancing, as expressed in narratives, are worth investigating more deeply.
Surprisingly, sensory and emotional language in the immediate narratives did not relate to trends in symptom severity (e.g., Eid et al., 2005; Foa et al., 1995). However, we emphasize that current participants included few emotional and sensory words on average. Because we collected narratives immediately after the traumatic event occurred, we could examine the initial stages of narrative construction, almost concurrent with encoding of the event. At this early point, putting the experience into words may be difficult and may take individuals’ focus away from emotional and sensory experiences (e.g., Brewin & Holmes, 2003). Over time, individuals who begin to focus on these aspects in their narratives may be at greater risk. Notably, individuals who temporally distanced themselves from the immediate experience and did not focus on internal cognitive processing showed less severe symptoms over time. Future research should examine not only the immediate narrative, but changes in narrative processing in relation to trajectories of symptoms.
An additional finding concerning gender is noteworthy. Women focused on the present more than men and showed greater symptoms than men. Previous researchers have shown that women generally show higher symptoms than men and generally report more ruminative responses to negative feelings (Kessler et al., 2003; Nolen-Hoeksema, Larson, & Grayson, 1999; Olff, Langeland, Draijer, & Gersons, 2007); our results suggest that one reason for this may be that women have more difficulty temporally distancing themselves from stressful experiences.
We note a limited sample size. Though larger than many trauma samples recruited from emergency and/or intensive care departments (e.g., Buck, Kindt, van den Hout, Steens, & Linders, 2006), the current sample remains modest. We used HLM, which is sufficiently powered with a larger number of groups (here, individuals with repeated measures) and uses all available data across time. Further, although many of these individuals displayed moderate levels of symptoms, few met cutoff criteria for severe depression or PTSD. Still, the variability in symptom expression was adequate for our analyses, and this was a representative population of individuals who visited the ED for an array of injuries, and who may have needed to be assessed for further intervention. We also note that we used an empirically driven approach in analyses, testing plausible covariates and linguistic markers, but only retaining significant effects. We selected this approach given the use of a fairly novel sample and narrative timing. While we included covariates and linguistic markers that have been previously associated with depressive and PTSD symptoms, we only retained significant effects to maintain focus on the most promising variables for future studies. We also note study strengths. The use of same-day trauma narratives gave us a rare opportunity to assess recollection and narrative before extensive meaning could be established between the event and one’s broader life story (Fivush, 2011; Fivush et al., in press). Further, the longitudinal nature of this study provided insights into trajectories in psychological symptoms. This study also involved a community sample of adults who were predominantly African American, which provided insight into an understudied population.
Future research will benefit from deeper phenomenological methods and a greater focus on person-level patterns of narrative structure and content as it emerges over time. A promising set of narrative themes to consider involves dimensions of coherence (i.e., chronological and thematic coherence) as individuals reflect on traumatic experience. As can be seen in the narrative examples given in the Appendix, there is variability in the extent to which individuals situate the event, linearly order the event from a clear beginning to end, and establish additional connections between the event and their broader life experiences. Such considerations may provide additional insights for immediate trauma narratives as potential markers for trends in trauma-related symptoms.
The present study addressed gaps in trauma narrative research by recruiting individuals from an ED and asking them to narrate same-day traumatic injuries. Individuals were tracked over 12 months to test the unique predictive value of initial narrative linguistic content on trends of depressive and posttraumatic symptoms. Past-focused utterances predicted greater declines in depressive symptoms over time, whereas cognitive-process utterances predicted more severe reports of depressive symptoms across time. Participants who used fewer past-focused utterances alongside more cognitive-process utterances showed the poorest trajectories in terms of depression and PTSD across time. These patterns clarify earlier work on the role of cognitive processing in narratives by investigating subjective distancing and responses akin to rumination in narratives. That narrative markers in the immediate aftermath of trauma predict long-term trajectories of symptom severity beyond baseline symptoms and demographics suggests that initial narrative recall can inform ongoing needs for intervention following trauma.
Supplementary Material
Figure 2.
Patterns of depressive symptoms given use of past-focused utterances. Starting values assume participants are men with mean reports of trauma history and education level. Trends depict effects 1 standard deviation SD below (fewer) or above (more) the mean.
Acknowledgments
This work was supported by the National Institute of Mental Health (R01 MH094757, F32 MH101976).
We would like to acknowledge Debra Houry, M.D., and Abigail Hankin-Wei, M.D. for their generous collaborative efforts on this study. We would like to thank Cypriana Gardner for her work in transcribing the trauma narratives. For their work in the emergency department recruiting and assessing participants, we would like to thank Vasiliki Michopoulous, Alex O. Rothbaum, Thomas Crow, Heather Grinstead, Rebecca C. Roffman, Jessica Maples, Lydia Odenat, Loren M. Post, Liza C. Zwiebach, Devika Fiorillo, Kathryn Breazeale, Jessica Morgan, Natasha Mehta, Elicia D. Skelton, Taleesha S. Booker, and Jonathan Zebrowski.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [DOI] [Google Scholar]
- Bates D, Maechler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. Journal of Statistical Software. 2015;67:1–48. https://doi.org/10.18637/jss.v067.i01. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II (BDI-II) San Antonio, TX: Psychological Corporation; 1996. https://doi.org/10.1037/t00742-000. [Google Scholar]
- Bedard-Gilligan M, Duax Jakob JM, Doane LS, Jaeger J, Eftekhari A, Feeny N, Zoellner LA. An investigation of depression, trauma history, and symptom severity in individuals enrolled in a treatment trial for chronic PTSD. Journal of Clinical Psychology. 2015;71:725–740. doi: 10.1002/jclp.22163. https://doi.org/10.1002/jclp.22163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boals A, Banks JB, Hathaway LM, Schuettler D. Coping with stressful events: Use of cognitive words in stressful narratives and the meaning-making process. Journal of Social and Clinical Psychology. 2011;30:378–403. https://doi.org/10.1521/jscp.2011.30.4.378. [Google Scholar]
- Brewin CR, Dalgleish T, Joseph S. A dual representation theory of posttraumatic stress disorder. Psychological Review. 1996;103:670–686. doi: 10.1037/0033-295x.103.4.670. https://doi.org/10.1037//0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003;23:339–376. doi: 10.1016/s0272-7358(03)00033-3. https://doi.org/10.1016/s0272-7358(03)00033-3. [DOI] [PubMed] [Google Scholar]
- Bryk A, Raudenbush SW. Hierarchical linear models for social and behavioral research: Applications and data analysis methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Buck N, Kindt M, van den Hout M, Steens L, Linders C. Perceptual memory representations and memory fragmentation as predictors of post-trauma symptoms. Behavioural and Cognitive Psychotherapy. 2006;35:259–272. https://doi.org/10.1017/S1352465806003468. [Google Scholar]
- Crespo M, Fernández-Lansac V. Memory and narrative of traumatic events: A literature review. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8:149–156. doi: 10.1037/tra0000041. https://doi.org/10.1037/tra0000041. [DOI] [PubMed] [Google Scholar]
- D’Andrea W, Chiu P, Casas B, Deldin P. Linguistic predictors of post-traumatic stress disorder symptoms following 11 September 2001. Applied Cognitive Psychology. 2012;26:316–323. https://doi.org/10.1002/acp.1830. [Google Scholar]
- Dalal DK, Zickar MJ. Some common myths about centering predictor variables in moderated multiple regression and polynomial regression. Organizational Research Methods. 2011;15:33–362. https://doi.org/10.1177/1094428111430540. [Google Scholar]
- Eid J, Johnsen BH, Saus ER. Trauma narratives and emotional processing. Scandinavian Journal of Psychology. 2005;46:503–510. doi: 10.1111/j.1467-9450.2005.00482.x. https://doi.org/10.1111/j.1467-9450.2005.00482.x. [DOI] [PubMed] [Google Scholar]
- Fivush R. The development of autobiographical memory. Annual Review of Psychology. 2011;62:559–562. doi: 10.1146/annurev.psych.121208.131702. https://doi.org/10.1146/annurev.psych.121208.131702. [DOI] [PubMed] [Google Scholar]
- Fivush R, Graci ME, Booker JA. Ongoing narrative meaning-making within events and across the lifespan. Imagination, Cognition, and Personality. 2017;37:127–152. https://doi.org/10.1177/0276236617733824. [Google Scholar]
- Foa E, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of PTSD: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. https://doi.org/10.1037/1040-3590.9.4.445. [Google Scholar]
- Foa EB, Molnar C, Cashman L. Change in rape narratives during exposure therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 1995;8:675–690. doi: 10.1002/jts.2490080409. [DOI] [PubMed] [Google Scholar]
- Foa E, Riggs D, Dancu C, Rothbaum B. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–474. doi: 10.1007/BF00974317. [DOI] [Google Scholar]
- Greenhoot AF, Sun S, Bunnell SL, Lindboe K. Making sense of traumatic memories: Memory qualities and psychological symptoms in emerging adults with and without abuse histories. Memory. 2013;21:125–142. doi: 10.1080/09658211.2012.712975. https://doi.org/10.1080/09658211.2012.712975. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Robins LN, McEvoy L. Post-traumatic stress disorder in the general population: Findings of the epidemiologic catchment area survey. The New England Journal of Science. 1987;317:1630–1634. doi: 10.1056/NEJM198712243172604. https://doi.org/10.1056/nejm198712243172604. [DOI] [PubMed] [Google Scholar]
- Hellawell SJ, Brewin CR. A comparison of flashbacks and ordinary autobiographical memories of trauma: Content and language. Behaviour Research and Therapy. 2004;42:1–12. doi: 10.1016/s0005-7967(03)00088-3. https://doi.org/10.1016/s0005-7967(03)00088-3. [DOI] [PubMed] [Google Scholar]
- Jelinek L, Randjbar S, Seifert D, Kellner M, Moritz S. The organization of autobiographical and nonautobiographical memory in posttraumatic stress disorder (PTSD) Journal of Abnormal Psychology. 2009;118:288–298. doi: 10.1037/a0015633. https://doi.org/10.1037/a0015633. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (NCS-R) The Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. https://doi.org/10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest: Tests in linear mixed effects models. R package version 2.0.–.30. 2016 Retrieved from https://CRAN.R-project.org/package=lmerTest.
- Lüdecke D. sjPlot: Data visualization for statistics in social science. R package version 2.3.1. 2017 Retrieved from https://CRAN.R-project.org/package=sjPlot>.
- Manne S. Language use and post-traumatic symptomatology in parents of pediatric cancer survivors. Journal of Applied Social Psychology. 2002;32:608–629. https://doi.org/10.1111/j.1559-1816.2002.tb00233.x. [Google Scholar]
- Merrill N, Waters TEA, Fivush R. Connecting the self to traumatic and positive events: Links to identity and well-being. Memory. 2015;24:1321–1328. doi: 10.1080/09658211.2015.1104358. https://doi.org/10.1080/09658211.2015.1104358. [DOI] [PubMed] [Google Scholar]
- McLean KC, Pasupathi M, Pals JL. Selves creating stories creating selves: A process model of self-development. Personality and Social Psychology Review. 2007;11:262–278. doi: 10.1177/1088868307301034. https://doi.org/10.1177/1088868307301034. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Abnormal Psychology. 2000;109:504–511. https://doi.org/101037/10021-843X.109.3.504. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Exploring the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. https://doi.org/10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- O’Kearney R, Perrtot K. Trauma narratives in posttraumatic stress disorder: A review. Journal of Traumatic Stress. 2006;19:81–93. doi: 10.1002/jts.20099. https://doi.org/10.1002/jts.20099. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. https://doi.org/10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Peetz J, Wilson AE. The temporally extended self: The relation of past and future selves to current identity, motivation, and goal pursuit. Social and Personality Psychology Compass. 2008;2:2090–2106. https://doi.org/10.1111/j.1751-9004.2008.00150.x. [Google Scholar]
- Pennebaker JW, Boyd RL, Jordan K, Blackburn K. The development and psychometric properties of LIWC2015. Austin, TX: University of Texas at Austin; 2015. [Google Scholar]
- Pennebaker JW, Francis ME. Cognitive, emotional, and language processes in disclosure. Cognition and Emotion. 1996;10:601–626. https://doi.org/10.1080/026999396380079. [Google Scholar]
- Quené H, van den Bergh H. On multi-level modeling of data from repeated measures designs: A tutorial. Speech Communication. 2004;43:103–121. https://doi.org/10.1016/j.specom.2004.02.004. [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. Retrieved from https://www.R-project.org. [Google Scholar]
- Raudenbush SW, Xiao-Feng L. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001;6:387–401. https://doi.org/10.1037//1082-989x.6.4.387. [PubMed] [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R. Boston, MA: RStudio, Inc.; 2015. Retrieved from http://www.rstudio.com. [Google Scholar]
- Römisch S, Leban E, Habermas T, Döll-Hentschker S. Evaluation, immersion, and fragmentation in emotion narratives from traumatized and nontraumatized women. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6:465–472. https://doi.org/10.1037/a0035169. [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5:455–475. https://doi.org/10.1007/BF00977239. [Google Scholar]
- Snijders TAB, Bosker R. Multilevel analysis. An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Snijders TAB, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. 2. Los Angeles, CA: Sage; 2012. [Google Scholar]
- Tausczik YR, Pennebaker JW. The psychological meaning of words: LIWC and computerized text analysis methods. Journal of Language and Social Psychology. 2010;29:24–54. https://doi.org/10.1177/0261927X09351676. [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27:247–259. https://doi.org/10.1023/a:1023910315561. [Google Scholar]
- Wilson AE, Ross M. The identity function of autobiographical memory: Time is on our side. Memory. 2003;11:137–149. doi: 10.1080/741938210. https://doi.org/ 10.1080/09658210244000324. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.