Background
In the 10/22/17 issue of Thorax, Ruoyan Li and colleagues published an interesting analysis of 2 patients with multifocal adenocarcinoma (1). Both patients were non-smokers who presented with multiple (n=7 and 8) ground glass nodules (GGNs) which were mostly resected and confirmed to be within the adenocarcinoma spectrum, ranging from premalignant lesions [atypical adenomatous hyperplasia (AAH)] to minimally invasive lesions [adenocarcinoma in situ (AIS) or minimally invasive adenocarcinoma (MIA)] and invasive adenocarcinoma (2 lesions in patient 2 were not resected). There was no lymph node involvement or lympho-vascular invasion in either case. In the first patient, 3 of the lesions had a substantial solid component (on lung windows as seen on the CT images in the paper) and were moderately large (17–37 mm overall size). The second patient had only pure ground glass lesions that were relatively small (4–14 mm overall size).
Li et al. carried out exome sequencing of the resected lesions, with an average of 68x exome coverage depth (1). In patient 1, five lesions shared a single mutation in EGFR (p.L858R); but this was viewed as convergent evolution because this mutation is widely recognized as a frequent mutation in lung adenocarcinoma. Excluding the EGFR p.L858R variant, Li et al. found that for 6 of the lesions the detected mutations were distinct from the mutations in each of the other lesion. However, two of the lesions shared nineteen non-synonymous and seven synonymous mutations with each other. Almost all the shared mutations occurred in rarely reported genes. Of note, these two lesions were histologically dissimilar, one being papillary predominant (60%) and the other acinar predominant (90%), as well as other morphologic differences. Li et al. looked for a possible field cancerization effect through exome sequencing of normal lung tissue between the two GGOs that shared many mutations, but did not find any somatic mutations in the normal tissue.
Similarly, in patient 2, five lesions had distinct, non-overlapping mutations, but two lesions shared four non-synonymous and four synonymous mutations. One of the lesions was classified morphologically as AAH and the other as AIS (which may be more reflective of differences in size than lesion morphology, but no morphologic details were provided).
Li et al. concluded that the shared mutations identified by exome sequencing in two GGNs in each patient indicated that the two lesions originated from a common ancestor. The degree of shared mutations, particularly since these were noted in rarely reported genes, could not be explained as convergent evolution, and indicated that the two lesions represented intrapulmonary metastasis. Li et al. also concluded that the other lesions in the 2 patients were clearly separate primary tumors, although they speculated that with higher exome coverage depth some of these unrelated lesions may actually turn out to be related after all (1).
In the view of Li et al., their findings have important far reaching implications. The demonstration that intrapulmonary metastasis can occur even among GGNs—i.e., the more indolent and non- or pre-invasive part of the spectrum of adenocarcinoma—and in cases without nodal or lympho-vascular involvement undermines our concepts or how metastasis occurs. Li et al. went on to conclude that for patients with metastatic GGOs, wedge resection may not be enough (1). The unstated overall implication is that perhaps we should be more aggressive with the earliest manifestations of lung cancer—i.e., resect even small pure ground glass lesions, including AAH, and with larger resections.
Perspectives and assumptions
Li and colleague’s assessment of multiple GGNs is clearly from a genomic perspective. Inherent in their view is a number of (widely held) assumptions, which may or may not be true. First, that the genomic information gets us closest to the truth, and trumps other observations. (The fact that the lesions with shared mutations are morphologically dissimilar is discounted). It is assumed that mutations occur randomly, so that the more shared mutations there are, the lower the probability that this could have occurred by chance alone. The fact that the “related” lesions also have many discordant mutations is viewed as further evolution of each from a common ancestral clone. [However, the EGFR p.L858R mutation present in many of the lesions is not viewed this way; indeed, EGFR mutations are common mutation among lung adenocarcinomas, have been demonstrated even in adjacent normal tissue and have been taken as evidence of field cancerization (2-4)].
Can we be sure that the shared mutations between 2 tumors prove that these are the same tumor? Could similar mutations be caused by a particular etiology that affects a certain genomic target? Could cellular selection favor certain mutations (isn’t this the explanation for the widespread prevalence of EGFR mutations)? Of course, these hypotheses are undermined by the fact that most of the lesions in the Li et al. analysis had no shared mutations at all.
In 2014, the International Association for the Study of Lung Cancer (IASLC) created a special committee focusing on multiple pulmonary sites of lung cancer. This group carried out a systematic literature review and considered many perspectives: morphologic, genomic, mechanistic (scientific evidence regarding how metastasis occurs), and biologic behavior (recurrence patterns and response to treatment) (5-8). The committee concluded that, for the most part, evidence that 2 lesions are the same (i.e., metastatic) or different (i.e., separate primary tumors) must be viewed as only suggestive because of inconsistencies in the available data. Specifically, the committee concluded that “mutational profiling [by itself] should not be considered definitive and must be considered together with other information (5).” Only a different histotype (e.g., adenocarcinoma and squamous carcinoma) or different morphology by comprehensive histologic assessment (i.e., proportion of adenocarcinoma subtypes) was acceptable by themselves to define 2 lesions as different, and only comprehensive genomic hybridization (a complex research tool) was acceptable by itself to define 2 lesions as the same (7).
Regarding ground glass/lepidic (GG/L) tumors, such as were present in the patients analyzed by Li et al., the IASLC committee concluded that a detailed histologic or genomic assessment was not necessary; these lesions should be classified as multifocal adenocarcinoma and viewed as separate primary cancers (8). This was driven by several factors: excellent clinical outcomes despite the multifocal nature, easy recognition of the entity by the ground glass component and the need for a clinically applicable definition (as pure ground glass lesions should generally be observed and not resected). The IASLC committee found an average 5-year survival of 85% in multifocal GG/L tumors (which were mostly part-solid). Distant recurrence was highly unusual, and the primary form of “recurrence” was the development of a new lung primary (a new GG/L adenocarcinoma) (8).
Many studies have demonstrated that GG/L tumors (both isolated and multifocal tumors) exhibit rather indolent behavior (9-12). Most prominent perhaps are 2 prospective studies in which GGN were observed until specific criteria were met (e.g., development of growth of a solid component on mediastinal windows of ≥2 mm) (9,11). Most GGN remained stable (even after 20 years in one study) (1), only a small minority were resected, but all of these were stage I cancers with excellent survival (9,11). These studies suggest that the mere presence of a GGN should not be cause for concern.
The IASLC committee avoided explicitly defining the nature of the multifocal GG/L lesions. The committee considered multiple perspectives and types of evidence, but concluded that the level of understanding was insufficient. One can debate whether it was wise of the IASLC committee to avoid speculation in an area of uncertainty. One might view the analysis by Li et al. as potentially shedding some light on this entity.
The reality is that we are all like blind men, trying to characterize an entity that we are not (yet) able to observe in its entirety (Figure 1). We must be careful not to overemphasize a particular perspective, and not to go too far in drawing conclusions from particular observations. We must also be careful to question inherent assumptions. The biologic behavior of cancer is complex, impacted by tumor cell characteristics, host factors (e.g., microenvironment), and multiple interactions between these (cell signaling, epigenetics, immune surveillance). What we are able to observe may be a mere manifestation of a more fundamental (obscure) process; this is highlighted by the fact that EGFR mutated lung adenocarcinoma can transform into small cell lung cancer and back again when treated with an EGFR inhibitor (13).
Figure 1.
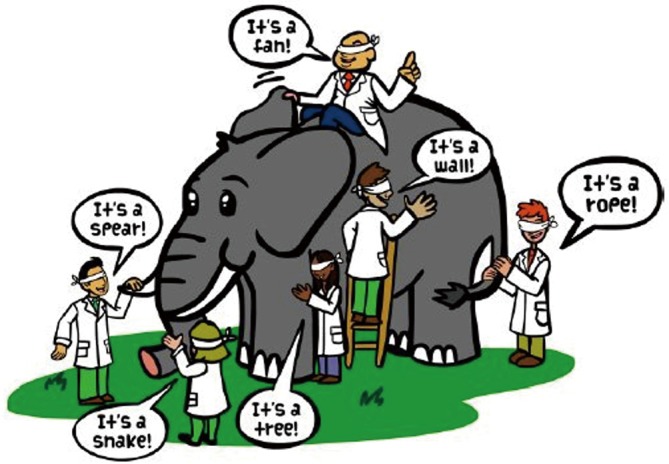
The parable of 6 blind men examining an elephant, each drawing a conclusion form a limited perspective.
Getting from here to there
If we accept a common clonality for 2 of the lesions in the Li et al. patients, what does the fact that these were detected at distinct sites (though in the same part of the lobe) mean? Is this a manifestation of metastatic dissemination, and a surrogate for poor outcome? Or is some other mechanism at play?
There is accumulating evidence in lung squamous cell carcinoma that genetically very similar lesions can spread throughout the tracheobronchial tree. It has long been clinically recognized that patients with central airway carcinomas have a high probability of additional similar lung cancers (14-16). In 1997 Franklin et al. demonstrated an identical p53 point mutation at multiple dysplastic sites in the airways of both lungs—of note, no invasive tumor was demonstrated at any site (the patient had died of benign causes) (17). More recently, a longitudinal study of serial biopsies in several patients demonstrated the appearance of carcinoma in situ lesions, genetically highly similar to a resected squamous lung cancer. These lesions developed in areas that were normal on previous biopsies, and intervening mucosa remained normal; the progression involved a distal to proximal direction, occurring over many years (some of these lesions were treated, others were not) (18). Similar findings have been reported by others (19). These studies suggest that “migration” through the respiratory epithelium can occur—this happened slowly, and not necessarily with ominous clinical impact. Is the presence of genetically similar adenocarcinoma lesions in the study by Li et al. (within the same part of a lobe but with intervening normal tissue) evidence of the same phenomenon as has been seen with squamous cell lesions? Is this a fundamentally different process than what is traditionally considered to be metastatic dissemination?
We have limited understanding of the mechanism behind the appearance of a cancer cell at a physically separate site. There is extensive data that the process of metastasis is highly complex. Tumor cells exhibit plasticity, undergo epithelial to mesenchymal transition during the multistep invasion-dissemination process (invasion, intravasation, migration, survival in the circulation), and then back again as the extravasation-colonization-metastasis-formation process continues (20-22). The various steps are influenced not only by tumor-cell-intrinsic genetic and epigenetic determinants but also a complex array of tumor-host-interactions at both the primary and metastatic sites (20-22). Tumor cells are present simultaneously in many different forms (at primary site, circulating cells, dormant forms, permissive niches etc.) and heterogeneous subpopulations with different gene expression, host-tumor interactions and potential biologic behavior. There is a complex dynamic flow of tumor cells between the primary site, circulating cells, overt metastases and back to the primary site (20-22). This extensive data makes it clear that it is overly simplistic to think of the process of metastasis as one governed by physical routes that a cancer cell could take in dispersing from a site of origin (i.e., lymphogenous, hematogenous, aerogenous).
The concept of field cancerization is appealing in the context of multifocal cancer. While there is much evidence supporting this, there is conflicting data and controversy how this leads to the development of multiple cancers (19). Does a field of injury (with related genetic alterations) provide a fertile ground for the development of multiple separate primary cancers/Does a mutant clone expand and colonize regionally adjacent areas? Does an established cancer disseminate (preferentially) to other pulmonary (permissive) sites?
Li et al. suggest that intrapulmonary metastasis might be explained by a microscopic observation known as “spread through air spaces” (STAS), in which isolated tumor cells are observed beyond the edge of the main tumor (23,24). However, STAS may be merely a marker for particular tumor characteristics rather than an actual mechanism for metastasis. STAS is strongly correlated with node involvement, lympho-vascular invasion and more aggressive tumor types (24). Furthermore, it may be an artifact; studies have demonstrated that the presence of STAS correlates with the number of cuts made of the specimen, leading some to refer to it as “STAKS—spread through a knife surface” (25,26). Or is the observation of STAS similar to the “discovery” of circulating tumor cells decades ago? We now know that circulating cells are present in essentially all patients (including stage I), are not correlated with subsequent appearance of systemic metastasis, and do not provide an assessment of the factors that govern the complex multistep process of development of systemic metastases (21,22,27). At this point we have a limited understanding of what the microscopic observation of STAS actually represents.
Blind people should leap carefully
Given the limitations in our fundamental understanding of cancer development and dissemination in general, and in particular multifocal cancer, we must be careful about how far to go in drawing conclusions for observations in two patients in the study by Li et al. We should not assume that if there are shared mutations, it must be evidence that the tumor has the ability to migrate (metastasize) or that if it can metastasize then it must be life-threatening. The observed results are that survival after resection of AAH, AIS and MIA is essentially 100%. If a proportion of multifocal GGNs are metastatic (the observations by Li et al. suggest that 10–20% might be), and this is indeed an appropriate surrogate endpoint, we would expect worse survival. Furthermore, there are many studies demonstrating that the majority of GGNs do not progress over time, and that in those that do, resection remains curative.
I think we should be particularly careful not to draw the conclusion that the observations of Li et al. imply that we need to be aggressively resect pure GGNs because some are already metastatic. This represents a huge leap, based on multiple assumptions. It ignores a great deal of evidence we have to the contrary. I think we should view the findings by Li et al. as an interesting piece of a jigsaw puzzle, but one that I cannot yet connect sufficiently to other pieces to allow the image depicted by the entirety of the puzzle to emerge. It is appropriate to speculate what it might mean. It is right to try out how well this piece of information fits or does not fit with other evidence that we have. But we should refrain from drawing extensive conclusions about the overall picture based on scrutiny of one piece of a complicated puzzle.
Acknowledgements
None.
Provenance: This is an invited Editorial commissioned by the Section Editor Jun Zhou (Department of Nuclear Medicine, Zhongshan Hospital, Fudan University, Shanghai, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- 1.Li R, Li X, Xue R, et al. Early metastasis detected in patients with multifocal pulmonary ground-glass opacities (GGOs). Thorax 2018;73:290-92. 10.1136/thoraxjnl-2017-210169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang YL, Wu CT, Lin SC, et al. Clonality and Prognostic Implications of p53 and Epidermal Growth Factor Receptor Somatic Aberrations in Multiple Primary Lung Cancers. Clin Cancer Res 2007;13:52-8. 10.1158/1078-0432.CCR-06-1743 [DOI] [PubMed] [Google Scholar]
- 3.Murphy SJ, Wigle DA, Lima JF, et al. Genomic Rearrangements Define Lineage Relationships between Adjacent Lepidic and Invasive Components in Lung Adenocarcinoma. Cancer Res 2014;74:3157-67. 10.1158/0008-5472.CAN-13-1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang X, Shigematsu H, Bekele BN, et al. EGFR Tyrosine Kinase Domain Mutations Are Detected in Histologically Normal Respiratory Epithelium in Lung Cancer Patients. Cancer Res 2005;65:7568-72. 10.1158/0008-5472.CAN-05-1705 [DOI] [PubMed] [Google Scholar]
- 5.Detterbeck FC, Nicholson AG, Franklin WA, et al. The IASLC Lung Cancer Staging Project: Summary of Proposals for Revisions of the Classification of Lung Cancers with Multiple Pulmonary Sites of Involvement in the Forthcoming Eighth Edition of the TNM Classification. J Thorac Oncol 2016;11:639-50. [DOI] [PubMed] [Google Scholar]
- 6.Detterbeck FC, Bolejack V, Arenberg DA, et al. The IASLC Lung Cancer Staging Project: Background Data and Proposals for the Classification of Lung Cancer with Separate Tumor Nodules in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:681-92. [DOI] [PubMed] [Google Scholar]
- 7.Detterbeck FC, Franklin WA, Nicholson AG, et al. The IASLC Lung Cancer Staging Project: Background Data and Proposed Criteria to Distinguish Separate Primary Lung Cancers from Metastatic Foci in Patients with Two Lung Tumors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:651-65. [DOI] [PubMed] [Google Scholar]
- 8.Detterbeck FC, Marom EM, Arenberg DA, et al. The IASLC Lung Cancer Staging Project: Background Data and Proposals for the Application of TNM Staging Rules to Lung Cancer Presenting as Multiple Nodules with Ground Glass or Lepidic Features or a Pneumonic Type of Involvement in the Forthcoming Eighth Edition of the TNM Classification. J Thorac Oncol 2016;11:666-80. [DOI] [PubMed] [Google Scholar]
- 9.Kakinuma R, Noguchi M, Ashizawa K, Kuriyama K, Maeshima AM, Koizumi N, et al. Natural History of Pulmonary Subsolid Nodules: A Prospective Multicenter Study. J Thorac Oncol 2016;11:1012-28. 10.1016/j.jtho.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 10.Kobayashi Y, Fukui T, Ito S, et al. How Long Should Small Lung Lesions of Ground-Glass Opacity be Followed? J Thorac Oncol 2013;8:309-14. 10.1097/JTO.0b013e31827e2435 [DOI] [PubMed] [Google Scholar]
- 11.Sawada S, Yamashita N, Sugimoto R, et al. Long-term out-comes of patients with ground-glass opacities detected using computed tomography. Chest 2017;151:308-15. 10.1016/j.chest.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 12.Son JY, Lee HY, Lee KS, et al. Quantitative CT Analysis of Pulmonary Ground-Glass Opacity Nodules for the Distinction of Invasive Adenocarcinoma from Pre-Invasive or Minimally Invasive Adenocarcinoma. PLoS One 2014;9:e104066. 10.1371/journal.pone.0104066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. 10.1126/scitranslmed.3002003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaissert HA, Grillo HC, Shadmehr MB, et al. Long-term survival after resection of primary adenoid cystic and squamous cell carcinoma of the trachea and carina. Ann Thorac Surg 2004;78:1889-96; discussion 1896-7. [DOI] [PubMed]
- 15.Watanabe Y, Shimizu J, Oda M, et al. Early hilar lung cancer: its clinical aspect. J Surg Oncol 1991;48:75-80. 10.1002/jso.2930480202 [DOI] [PubMed] [Google Scholar]
- 16.Terzi A, Pelosi G, Falezza G, et al. Early hilar lung cancer--clinical aspects and long term survival. Identification of a subgroup of stage IA patients with more favorable prognosis. Lung Cancer 2000;27:119-24. 10.1016/S0169-5002(99)00101-4 [DOI] [PubMed] [Google Scholar]
- 17.Franklin WA, Gazdar AF, Haney J, et al. Widely dispersed p53 mutation in respiratory epithelium. A novel mechanism for field carcinogenesis. J Clin Invest 1997;100:2133-7. 10.1172/JCI119748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pipinikas CP, Kiropoulos TS, Teixeira VH, et al. Cell migration leads to spatially distinct but clonally related airway cancer precursors. Thorax 2014;69:548. 10.1136/thoraxjnl-2013-204198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCaughan F, Pipinikas CP, Janes SM, et al. Genomic evidence of pre-invasive clonal expansion, dispersal and progression in bronchial dysplasia. J Pathol 2011;224:153-9. 10.1002/path.2887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valastyan S, Weinberg Robert  A. Tumor Metastasis: Molecular Insights and Evolving Paradigms. Cell 2011;147:275-92. 10.1016/j.cell.2011.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinberg RA. Mechanisms of malignant progression. Carcinogenesis 2008;29:1092-5. 10.1093/carcin/bgn104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wan L, Pantel K, Kang Y. Tumor metastasis: moving new biological insights into the clinic. Nat Med 2013;19:1450-64. 10.1038/nm.3391 [DOI] [PubMed] [Google Scholar]
- 23.Kadota K, Nitadori J, Sima CS, et al. Tumor Spread through Air Spaces is an Important Pattern of Invasion and Impacts the Frequency and Location of Recurrences after Limited Resection for Small Stage I Lung Adeno-carcinomas. J Thorac Oncol 2015;10:806-14. 10.1097/JTO.0000000000000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warth A. Spread through air spaces (STAS): a comprehensive update. Transl Lung Cancer Res 2017;6:501-7. 10.21037/tlcr.2017.06.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blaauwgeers H, Flieder D, Warth A, et al. P3.01-009 A Prospective Study of 'Spread through a Knife Surface' (STAKS) in Non-Small Cell Lung Cancer Resection Specimens. J Thorac Oncol 2017;12:S1123-S4. 10.1016/j.jtho.2016.11.1575 [DOI] [Google Scholar]
- 26.Blaauwgeers H, Flieder D, Warth A, et al. A Prospective Study of Loose Tissue Fragments in Non-Small Cell Lung Cancer Resection Specimens: An Alternative View to "Spread Through Air Spaces". Am J Surg Pathol 2017;41:1226-30. 10.1097/PAS.0000000000000889 [DOI] [PubMed] [Google Scholar]
- 27.Chambers AF, Groomn AC, MacDonald IC. Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer 2002;2:563-72. 10.1038/nrc865 [DOI] [PubMed] [Google Scholar]


