Abstract
Background
Standard management has been recommended for obstructive sleep apnea (OSA) by several guidelines, but patient choice in the practical setting is unclear.
Methods
A survey nested in two prospective cohort studies of OSA (enrollment: 2001–2010) in China. The last interview was conducted between July 2014 and May 2015, using a comprehensive 10-point questionnaire administered in a face-to-face or telephone interview, and assessed (I) whether the participant had received any OSA treatment; (II) why he or she had decided for or against treatment; (III) what treatment was received; (IV) whether the participant used continuous positive airway pressure (CPAP) or OA daily; and (V) the perceived efficacy of therapy.
Results
A total of 4,097 subjects with a mean age of 45 years [37–55] responded to this survey, with a response rate of 79.4% (4,097/5,160); 2,779 subjects (67.8%) did not receive any treatment: 1,485 (53.4%) believed that their condition was not serious, despite severe OSA in 53.7% of the patients. A multivariate regression showed that the decision to receive treatment was associated with: age between 45–59 years [odds ratio (OR) 0.805, 95% CI: 0.691–0.936; P<0.001], female gender (OR 0.492, 95% CI: 0.383–0.631; P<0.001), severe OSA (OR 1.92, 95% CI: 1.01–3.64; P<0.001), hypertension (OR 1.414, 95% CI: 1.209–1.654; P<0.001) and diabetes (OR 1.760, 95% CI: 1.043–2.972; P=0.034). In subjects receiving treatment (n=1,318), 50.9% reported negative perceptions about the treatments.
Conclusions
Nearly two thirds of Chinese patients choose not to receive treatment after OSA diagnosis, and nearly half are negative about their treatments for OSA. This requires clinical attention, and warrants further study in different geographic settings.
Keywords: Obstructive sleep apnea, treatment, choice
Introduction
Obstructive sleep apnea (OSA) is associated with a number of mental, cardiovascular and metabolic disorders, possibly due to haemodynamic disturbances, systemic inflammation, and altered sympathetic activities in the patients (1-3). Estimated prevalence of OSA varies considerably, and could range from 9% to 37% in men and from 4% to 50% in women (4). Specifically in a recent population-based study, the prevalence of moderate-to-severe OSA, as defined by apnea- hypopnea index (AHI) score ≥15, was 49.7% in men and 23.4% in women (5). Increasing efforts have been made in promoting physician/patient awareness of this global epidemic, but so far, OSA remains under-diagnosed around the world (6-9).
It actually make the situation even worse that evidence suggests a substantial but un-clarified proportion of patients opt not to receive intervention even after knowing their disease status regardless of a wide spectrum of treatment options available, including continuous positive airway pressure (CPAP) devices and oral appliances (OAs), behavioural and/or adjunctive treatments (10,11). For example, a study in Australia showed that only 32.7% (51/159) of snoring and sleep apnea patients reported subsequent more than one treatment (12).
Population-based studies have indicated that at least 50 million patients in China suffer OSA (6,13). However, the number of patients who actually received proper treatment, and the types of treatments, remain unknown. The current study is a survey nested in two large cohort studies conducted in China during the past 10 years. We aimed to assess patient choice for treatment in subjects with OSA.
Methods
Subjects
The study subjects were from either of two ongoing prospective cohort studies, the State Key Laboratory of Respiratory Disease Study and the Shanghai Sleep Health Study, which examine the development of cardiovascular diseases in OSA patients (14,15). The two studies had enrolled, between January 2001 and July 2010, a total of 5,160 adults with newly diagnosed OSA who visited or were referred to the two centers for further evaluation of sleep problems (1,336 in the State Key Laboratory of Respiratory Disease Study and 3,824 in the Shanghai Sleep Health Study). The diagnosis and severity of OSA had been confirmed based on AHI score on polysomnography using the American Academy of Sleep Medicine criteria: mild: 5–15; moderate: 16–30; severe: >30 (16). Upon enrollment, complete demographic data included age, gender, body-mass index (BMI), marital status, level of education, medical history, medications, alcohol use, smoking habits and socioeconomic status. Sleep-related complaints and habits were evaluated using Epworth Sleepiness scale (ESS) and Berlin Questionnaire (BQ) for Sleep-disordered Breathing (17). All subjects received a 2-day standard education in group sessions, delivered by trained research assistants, on the pathophysiology, possible consequence and treatment options of OSA. The education session was designed by a panel of experts including several authors of this manuscript (LJS, WJL, HLY, JYZ), tested and refined in a pilot group of audience for clear communication. The education sessions explained to the patients about physiopathology of OSA, and emphasized on the compliance once the treatment begins, but did not endorse any specific treatments.
Between January 2014 and May 2015, we conducted the present survey using dataset of the pooled study population from these two prospective cohorts. During our study, 67 patients refused to participate, 13 had deceased, 963 were untraceable and 20 did not complete the survey before the study was closed. Our survey was approved by the Human Ethics Committees of the First Affiliated Hospital of Guangzhou Medical University (GYFYY-20001218) and the Sixth Affiliated Hospital of Shanghai Jiao Tong University (JDFLY-20001128). Written informed consent was obtained from all participants.
Study methods
In the present survey, a comprehensive 10-point questionnaire was administered in a face-to-face or telephone interview and assessed (I) whether the participant had received any OSA treatment; (II) why he or she had decided for or against treatment; (III) what treatment was received; (IV) whether the participant used CPAP or OA daily; and (V) the perceived efficacy of therapy. Surgical treatment included UPPP and revised UPPP, septoplasty, endoscopic sinus surgery, turbinate reduction surgery, simple tonsillectomy, multi-level or stepwise surgery, radiofrequency ablation, and palatal implants. Behavioural therapy was defined as weight loss, exercise, positional therapy, or avoiding alcohol and sedatives before bedtime. Adjunctive therapy was defined as bariatric surgery, pharmacotherapy, oxygen therapy, acupuncture or massage. Integrated treatment was defined as any combination of two or more of surgery, CPAP/OA, behavioural therapy and adjunctive therapy (10,11).
All patients were invited for re-examination with PSG during the survey. CPAP recipients were categorized as good users if they used CPAP regularly for more than 4 h/night for >70% of the recorded period. Those who did not meet the above criteria were labeled as non-users (17). For patients with available PSG data, treatment success was defined as AHI reduction down to below 5 or by >50% in comparison to the value at the time of diagnosis (18,19).
Statistical analysis
All statistical analyses were performed using SPSS 21.0 (IBM, Chicago, IL, USA). Categorical variables were reported as n (%), and analyzed using chi-squared test. Continuous variables were reported as mean ± SD or median (interquartile range), and analyzed using Student’s t-test or non-parametric test. Severity of OSA between those who received treatment vs. no treatment was compared using the Wilcoxon test. Logistic regression was used to identify factors associated with the decision to receive treatment. Statistical significance was defined as P<0.05 (two-sided).
Results
A total of 4,097 subjects responded to this survey, yielding a response rate of 79.4% (4,097/5,160). Of our study population, OSA severity was mild in 756, moderate in 884, and severe in 2,457 subjects (Table 1). Despite this profile, only a total of 1,318 patients (32.2%) chose to receive treatment because they frequently experienced prolonged periods of breathlessness during sleep (920, 69.8%); their bed-partner or roommates could not tolerate the loud snoring (180, 13.7%); they suffered at least two traffic accidents per year (as they responded to one of ESS questions) (80, 6.1%); they acted grumpy, impatient, or irritable (62, 4.7%); they had sexual problems (40, 3.0%); or they had tonsillitis, nasal diseases, morning headaches, dry mouth or other frequently reported consequences of sleeping disorders (36, 2.7%).
Table 1. Demographics of patients with OSA who received treatment and no treatment.
| Characteristic | Total (n=4,097) | Treatment (n=1,318) | No treatment (n=2,779) | P value* |
|---|---|---|---|---|
| Sex | <0.001 | |||
| Men | 3,565 (87.01) | 1,231 (93.40) | 2,334 (83.99) | |
| Women | 532 (12.99) | 87 (6.60) | 445 (16.01) | |
| Age, year | 45 [37–55] | 43 [36–53] | 47 [37–57] | <0.001 |
| 18–44 | 1,955 (47.72) | 719 (54.55) | 1,236 (44.48) | |
| 45–59 | 1,478 (36.08) | 472 (35.81) | 1,006 (36.20) | |
| 60–74 | 580 (14.16) | 111 (8.42) | 469 (16.88) | |
| 75–89 | 84 (2.05) | 16 (1.21) | 68 (2.45) | |
| BMI, kg/m2 | 27 [24–29] | 27 [24–29] | 27 [24–29] | 0.170 |
| Neck circumference, cm | 40 [37–42] | 40 [38–43] | 40 [37–42] | 0.030 |
| Waist circumference, cm | 95 [89–100] | 96 [90–101] | 95 [89–100] | 0.002 |
| Follow-up [years] | 8 [6–9] | 7 [6–11] | 8 [6–9] | 0.028 |
| ≥5 to <8 | 1,961 (47.86) | 670 (50.83) | 1,291 (46.46) | |
| ≥8 to <11 | 1,445 (35.27) | 444 (33.69) | 1,001 (36.02) | |
| ≥11 | 691 (16.87) | 204 (15.48) | 487 (17.52) | |
| AHI, events/h | 39 [20–63] | 51 [28–71] | 33 [17–58] | <0.001 |
| 5–15 | 756 (18.45) | 154 (11.68) | 602 (21.66) | |
| 15.1–30 | 884 (21.58) | 199 (15.10) | 685 (24.65) | |
| >30 | 2,457 (59.97) | 965 (73.22) | 1,492 (53.69) | |
| ESS ≥10 | 1,480 (36.12) | 478 (36.27) | 1,002 (36.06) | 0.896 |
| Berlin score ≥2 | 1,612 (39.35) | 588 (44.61) | 1,024 (36.85) | <0.001 |
| Hypertension | 1,128 (27.53) | 423 (32.09) | 705 (25.37) | <0.001 |
| Diabetes | 74 (1.81) | 29 (2.20) | 45 (1.62) | 0.192 |
| Cardiovascular disease | 12 (0.29) | 4 (0.30) | 8 (0.29) | 1.000 |
| Stroke | 14 (0.34) | 4 (0.30) | 10 (0.36) | 1.000 |
| Smoking | 1,853 (45.23) | 588 (44.61) | 1,265 (45.52) | 0.586 |
| Alcohol use | 1,855 (45.28) | 604 (45.83) | 1,251 (45.02) | 0.626 |
| Occupation | <0.001 | |||
| Student/retired | 356 (8.69) | 67 (5.08) | 289 (10.40) | |
| Farmer/worker | 187 (4.56) | 48 (3.64) | 139 (5.00) | |
| Freelancer | 929 (22.68) | 284 (21.55) | 645 (23.21) | |
| Businessman | 1,939 (47.33) | 688 (52.20) | 1,251 (45.02) | |
| Office clerks | 686 (16.74) | 231 (17.53) | 455 (16.37) | |
| Monthly salary, RMB | <0.001 | |||
| <2,000 | 331 (8.08) | 64 (4.86) | 267 (9.61) | |
| 2,000–4,999 | 941 (22.97) | 297 (22.53) | 644 (23.17) | |
| 5,000–9,999 | 1,064 (25.97) | 338 (25.64) | 726 (26.12) | |
| 10,000–19,999 | 850 (20.75) | 295 (22.38) | 555 (19.97) | |
| ≥20,000 | 911 (22.24) | 324 (24.58) | 587 (21.12) | |
| Education level– | <0.001 | |||
| High school or lower | 867 (21.16) | 215 (16.31) | 652 (23.46) | |
| Undergraduate | 1,355 (33.07) | 447 (33.92) | 908 (32.67) | |
| Postgraduate | 1,875 (45.77) | 656 (49.77) | 1,219 (43.86) |
Data are n (%) or average (range). *, Comparison between treatment and no treatment. OSA, obstructive sleep apnea; AHI, apnea hypopnea index; BMI, body mass index; ESS, Epworth Sleepiness Scale.
Among the 2779 patients (67.8%) who did not receive treatment at all or withdrew after only brief treatment, 1,485 (53.4%) patients reported that their condition was not sufficiently serious to treat. Others stated inconvenience (425, 15.3%; particularly for CPAP), busy daily schedule (380, 13.7%), no trust in the treatment (332, 12.0%), and financial burden (157, 6.0%).
Factors associated with treatment vs. not
In univariate analyses, the following socio-economic factors differed between subjects who received treatment vs. those who did not receive treatment: gender, age, occupation and education, neck and waist circumferences, BQ score, and co-morbid hypertension, and OSA severity (Table 1). Logistic regression analysis identified the following independent predictors for receiving treatment: age between 45–59 years [odds ratio (OR) 0.805, 95% CI: 0.691–0.936; P<0.001], female gender (OR 0.492, 95% CI: 0.383–0.631, P<0.001), severe OSA (OR 1.92, 95% CI: 1.01–3.64, P=0.029), hypertension (OR 1.414, 95% CI: 1.209–1.654, P<0.001) and diabetes (OR 1.760, 95% CI: 1.043–2.972, P=0.034) (Table 2).
Table 2. Logistic regression to identify factors associated with patient decision to receive treatment.
| Variable | Regression coefficient | Standard error | Wald statistic | P | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Sex | −0.710 | 0.127 | 31.001 | <0.001 | 0.492 | 0.383 | 0.631 |
| Age, year | – | – | 62.022 | <0.001 | – | – | – |
| 18–44 | −0.217 | 0.077 | 7.895 | 0.005 | 0.805 | 0.691 | 0.936 |
| 45–59 | −0.915 | 0.124 | 54.231 | <0.001 | 0.401 | 0.314 | 0.511 |
| 60–74 | −1.089 | 0.304 | 12.844 | <0.001 | 0.336 | 0.185 | 0.610 |
| AHI, events/h | – | – | 106.613 | <0.001 | – | – | – |
| 5–15 | 0.149 | 0.123 | 1.468 | 0.226 | 1.161 | 0.912 | 1.477 |
| 15.1–30 | 0.848 | 0.101 | 69.934 | <0.001 | 2.335 | 1.914 | 2.849 |
| Hypertension | 0.347 | 0.080 | 18.767 | <0.001 | 1.414 | 1.209 | 1.654 |
| Diabetes | 0.565 | 0.267 | 4.477 | 0.034 | 1.760 | 1.043 | 2.972 |
AHI, apnea hypopnea index; OR, odds ratio; CI, confidence interval.
OSA severity and treatment choice
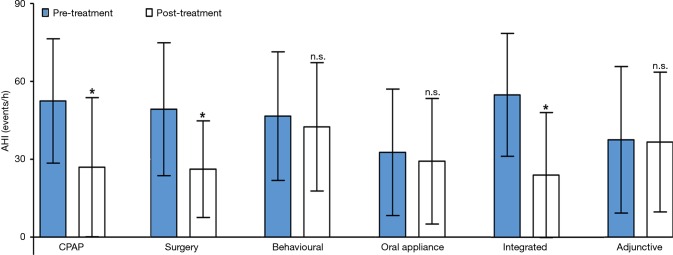
Percentage of the patients receiving treatment was 11.69%, 15.10%, and 73.21% in subjects with mild, moderate and severe OSA, respectively (χ2=−11.770, P<0.05): those with severe disease were more likely to receive treatment (Table 3). The most common types of treatments were surgery and CPAP (Figure 1).
Table 3. Treatment choices in patients stratified by OSA severity.
| Treatment choice | Mild OSA | Moderate OSA | Severe OSA | χ2 | P value |
|---|---|---|---|---|---|
| Treatment | 20.37 [154] | 22.51 [199] | 39.28 [965] | −11.770 | <0.001 |
| CPAP | 21.43 [33] | 27.14 [54] | 34.51 [333] | ||
| Surgery | 51.30 [79] | 47.74 [95] | 46.63 [450] | ||
| Behavioural | 10.39 [16] | 12.06 [24] | 9.02 [87] | ||
| OA | 7.79 [12] | 7.54 [15] | 1.66 [16] | ||
| Adjunctive | 5.84 [9] | 2.01 [4] | 1.24 [12] | ||
| Integrated | 3.25 [5] | 3.52 [7] | 6.94 [67] | ||
| No treatment | 79.63 [602] | 77.49 [685] | 60.72 [1,492] | – | – |
| Total | 100.00 [756] | 100.00 [884] | 100.0 [2,457] | – | – |
Values are presented as percentage [n], unless otherwise indicated. OSA, obstructive sleep apnea; CPAP, continuous positive airway pressure; OA, oral appliance.
Figure 1.
Patient choice in OSA patients. OSA, obstructive sleep apnea; CPAP, continuous positive airway pressure.
Treatment response, compliance and effectiveness
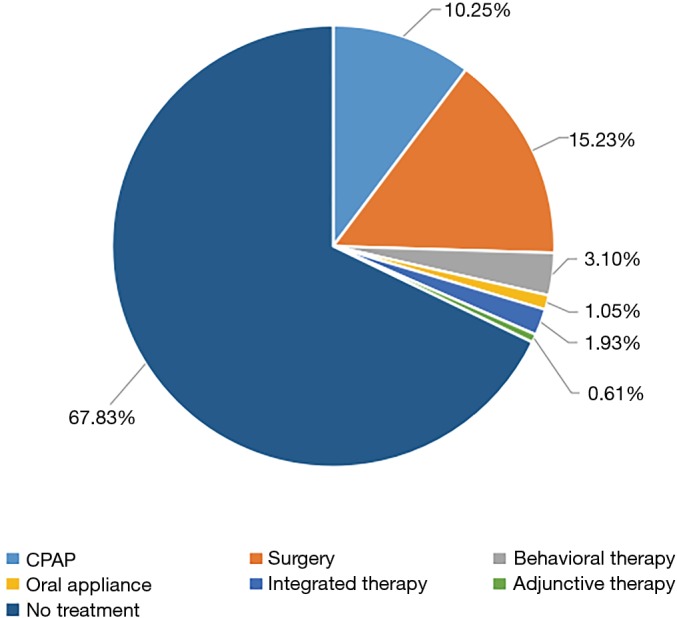
Among the 1,318 patients who received treatment, the AHI decreased from 49.3 (SD: 25.6) to 26.2 (SD: 18.6) (P<0.001), 52.5 (SD: 23.9) to 26.9 (SD: 26.8) (P<0.001), 54.9 (SD: 23.7) to 24.0 (SD: 24.0) (P<0.001) after surgery (n=624), CPAP (n=420) and integrated treatment (n=79), respectively. The AHI did not differ significantly between baseline (at the time of enrollment into the two prospective studies) and after treatment with OA (n=43), behavioural therapy (n=127), adjunctive therapy (n=25) (Figure 2).
Figure 2.
Change in AHI before and after treatment. Behavioural therapy was defined as weight loss, exercise, positional therapy, or avoiding alcohol and sedatives before bedtime. Adjunctive therapy was defined as bariatric surgery, pharmacotherapy, oxygen therapy. Integrated treatment was defined as any combination of two or more of surgery, CPAP/OA, behavioural therapy and adjunctive therapy. *P<0.05. ns, not significant; AHI, apnea hypopnea index; CPAP, continuous positive airway pressure; OA, oral appliance.
Among the 420 CPAP recipients, 247 (58.8%) used the equipment regularly. The remaining 173 patients (41.2%) initially received CPAP but withdrew from the treatment later for the following reasons: 24 (13.9%) reported symptoms resolution; 64 (37.0%), inconvenience; 33 (19.1%), no symptom improvement; 30 (17.3%), intolerance; 16 (9.3%), partner complaining of equipment noise; and 6, equipment failure.
Successful treatment was identified in 50.0% (210/420) of patients with CPAP, 48.72% (304/624) with surgery, 4.7% (2/43) with OA, 67.1% (53/79) with integrated treatment, 3.9% (5/127) with behavioural and 8.0% (2/25) with adjunctive therapies. Alternatively, a total of 742 (56.3%) from the 1318 patients who received treatment denied any therapeutic effectiveness.
At the time of our survey, all untreated patients reported similar clinical status at the last interview in comparison to the initial diagnosis.
Discussion
Our study revealed that around two-thirds of OSA patients chose to stay untreated or withdrew after only brief treatment of the condition. Previous studies showed that about 15–30% of patients are not willing to undertake CPAP treatment even before the titration stage (20). Estimates of treatment compliance range from 28% to 83% during 1 week to 4 years follow-up (21,22). However, there is limited information about further treatment in patients who failed to undertake or comply with CPAP. A study in Australia where CPAP was invented showed that only 32.7% of a general population-based sample reported receiving treatment for snoring and/or OSA (12).
According to our survey, a large part of patients with moderate to severe OSA but minimal symptoms did not perceive their condition serious enough to warrant medical attention. Only 36.12% of all patients had ESS score >10, unparalleled with distribution of OSA severity. Lower ESS score might be explained by several aspects: (I) the majority of the study sample was <60 years of age (83.79%); (II) taking naps after lunch is considered as a norm in China; (III) majority of Chinese people do not drive a car; (IV) relatively low literacy level (23). These findings were consistent with previous studies showing poor correlation between polysomnographic measures with excessive daytime somnolence, patient-perceived sleep quality, depression, and quality of life (24-27). Our data first confirmed that patients who consider their condition not sufficiently serious, but not PSG-measured OSA severity, was the main factor that may have contributed to their decision for OSA treatment. Thus, the determination of effect modifiers and predictive ability of various AHI threshold values and symptoms represent a great challenge in OSA.
Only 10.3% (420/4,097) patients chose CPAP even though it is first-line treatment for OSA. Of the 2,779 patients who refused or withdrew treatment, 15.3% complained that CPAP was inconvenient, and 41.2% of the patients who initially received CPAP withdrew shortly. Our results are consistent with a previous study showing that many patients reject CPAP or tolerate it only partially (20,21). Alternatively, OAs is recommended in case of initial CPAP refusal or CPAP failure, and also as a first-line treatment in mild to moderate OSA. A recent randomized controlled trial suggested that mandibular advancement splints may be as useful as CPAP across a range of OSA severity, although there is limited information on longer-term compliance (28). However, only 4.7% of OA users adhered regularly because of occasional temporomandibular joint pain. Thus, more convenient and comfortable forms of treatment are needed. These findings indicate that, in the real world of clinical practice, OSA patients poorly comply with therapy prescribed based on guidelines or expert consensus.
It was surprising that the most commonly chosen treatments in this study was surgery. Patients used it as initial therapy rather than salvage therapy, in contrast to official guidelines that emphasize the lack of demonstrated benefit of surgery (29,30). Currently in China, PSG is available at top-tier hospitals but not in primary care centers, and when it is available, it usually resides in a single department, limiting access for patients being treated in other departments. In many Chinese clinical settings, guidance about OSA treatment may not reflect the latest knowledge and instead may reflect more the physician’s own attitudes (29-31). Many physicians are unfamiliar with upper airway examinations and surgical indications; as a result, they may not necessarily refer a patient with obstructive nasal polyps or related lesions for CPAP titration. Some do not recommend surgery because of the risk of certain complications and potentially unsatisfactory long-term efficacy. Although we could not confirm our speculation, it is also possible that the reputed techniques boosted by an institution could influence the patient choice and physician decision about OSA treatment options. Another key factor in OSA treatment is the financial burden: in China, PSG, CPAP and OA must be paid out-of-pocket or through an employer-sponsored health plan. OSA diagnosis and treatment should be professionalized as a bona fide subspecialty in China, with experts trained in possible treatments over an entire year. Implementing such a process will be difficult in China, as it could be in other parts of the world, but it may contribute to improving awareness and effective treatment of the disease.
Logistic regression analysis identified the following independent predictors for receiving treatment: sex, age, severe OSA, hypertension and diabetes. Man, an age of ≤44 years or severe OSA was associated with increased patient intention to receive treatment, possibly due to heightened self-image and attention to health issues. OSA patients who are comorbid with diabetes or hypertension were also more likely to receive treatment. One possible explanation for this finding is the symptomatic worsening of hypertension or diabetes by OSA. Observational studies have shown significantly fewer cardiovascular events in patients adherent to CPAP therapy than in those who are not (31), but the need for large trials has lingered. In contrast, using data subset from the Sleep Heart Health Study, Kapur et al. showed that only male patients and those with increased BMI were more likely to receive OSA treatment. It is worth reminding that, male gender and obesity are two of well-publicized risk factors for OSA, thereby more frequently prompting for physician recognition and referral for further management should be attempted (32). Overly focusing on common risk factors of OSA or treatment as in Kapur’s study, or treatment predictors as in ours, could lead to a low rate of physician diagnosis, or a low level of enhanced medical education on OSA for those without these profiles, and hence a low rate of OSA treatment and subsequent compliance in a large population.
The strength of the current study included relatively large sample size, PSG-based OSA diagnosis and severity, and availability of long-term data about treatment compliance. Also, the survey was based on two large OSA cohort studies that had been ongoing for over 10 years. The fact that Guangzhou and Shanghai are the two most developed metropolitan areas with mature health care system and well-educated general population suggested that the treatment rate is even lower across the entire country than reported in the present study.
Limitations of the present study included several aspects. First, there is lack of consideration of social factors, such as spouse attitude and living conditions. Second, detailed data involving CPAP, OA and surgery for the entire study population were not available. Third, we did not obtain information about patients’ adherence to behavioural, adjunctive and integrated therapy, access to regular physicians, or physicians’ knowledge of OSA treatment, which made it impossible to investigate more potential reasons for suboptimal treatment. Last but not least, as usually with a survey among OSA patients, part of our data were subjected to recall bias. We speculated that these limitations should not greatly compromise the value of our work, but would inspire more future studies in depicting a clear picture of patient choice and compliance for OSA treatment in China.
To our knowledge, this is one of few surveys with large sample size, PSG-based diagnosis and an observation from a large cohort with long-term follow-up data. It was surprising that majority of patients did not treat after OSA diagnosis, but we speculate that it may not be unique for China, rendering further studies necessary in different geographic settings. In-depth reflections should be given on why patient education has been so underemphasized in clinical practice, and how future guidelines could better focus on patient involvement in the diagnosis and management in addition to standard objective criteria.
In conclusion, nearly two thirds of Chinese patients choose not to receive treatment after OSA diagnosis, and nearly half are negative about their treatments for OSA. This requires clinical attention, and warrants further study in different geographic settings.
Acknowledgements
Funding: This study was funded by the National Natural Science Foundation of China (81271066, 81570904) and the Guangdong Province Science and Technology Plan (2013B060100005).
Ethical Statement: Our survey was approved by the Human Ethics Committees of the First Affiliated Hospital of Guangzhou Medical University (GYFYY-20001218) and the Sixth Affiliated Hospital of Shanghai Jiao Tong University (JDFLY-20001128). Written informed consent was obtained from all participants.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Kendzerska T, Mollayeva T, Gershon AS, et al. Untreated obstructive sleep apnea and the risk for serious long-term adverse outcomes: a systematic review. Sleep Med Rev 2014;18:49-59. 10.1016/j.smrv.2013.01.003 [DOI] [PubMed] [Google Scholar]
- 2.Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA 2012;307:2169-76. 10.1001/jama.2012.3418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNicholas WT, Bonsigore MR; Management Committee of EU COST ACTION B26. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 2007;29:156-78. 10.1183/09031936.00027406 [DOI] [PubMed] [Google Scholar]
- 4.Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis 2015;7:1311-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 2015;3:310-8. 10.1016/S2213-2600(15)00043-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ip MS, Lam B, Tang LC, et al. A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong: prevalence and gender differences. Chest 2004;125:127-34. 10.1378/chest.125.1.127 [DOI] [PubMed] [Google Scholar]
- 7.Young T, Evans L, Finn L, et al. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997;20:705-6. 10.1093/sleep/20.9.705 [DOI] [PubMed] [Google Scholar]
- 8.Fuhrman C, Fleury B, Nguyên XL, et al. Symptoms of sleep apnea syndrome: high prevalence and underdiagnosis in the French population. Sleep Med 2012;13:852-8. 10.1016/j.sleep.2012.04.005 [DOI] [PubMed] [Google Scholar]
- 9.Lane JM, Tare A, Cade BE, et al. Common variants in CLOCK are not associated with measures of sleep duration in people of european ancestry from the sleep heart health study. Biol Psychiatry 2013;74:e33-5. 10.1016/j.biopsych.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein LJ, Kristo D, Strollo PJ, Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5:263-76. [PMC free article] [PubMed] [Google Scholar]
- 11.Kushida CA, Morgenthaler TI, Littner MR, et al. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea with oral appliances: an update for 2005. Sleep 2006;29:240-3. 10.1093/sleep/29.2.240 [DOI] [PubMed] [Google Scholar]
- 12.Marshall NS, Bartlett DJ, Matharu KS, et al. Prevalence of treatment choices for snoring and sleep apnea in an Australian population. J Clin Sleep Med 2007;3:695-9. [PMC free article] [PubMed] [Google Scholar]
- 13.Ip MS, Lam B, Lauder IJ, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest 2001;119:62-9. 10.1378/chest.119.1.62 [DOI] [PubMed] [Google Scholar]
- 14.McEvoy RD, Antic NA, Heeley E, et al. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N Engl J Med 2016;375:919-31. 10.1056/NEJMoa1606599 [DOI] [PubMed] [Google Scholar]
- 15.Guan J, Yi H, Zou J, et al. Distinct severity stages of obstructive sleep apnoea are correlated with unique dyslipidaemia: large-scale observational study. Thorax 2016;71:347-55. 10.1136/thoraxjnl-2015-207403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iber C, Ancoli-Israel S, Chesson AL, et al. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Westchester: AASM, 2007.
- 17.Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med 2013;188:613-20. 10.1164/rccm.201307-1282ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Partinen M, Jamieson A, Guilleminault C. Long-term outcome for obstructive sleep apnea syndrome patients. Mortality. Chest 1988;94:1200-4. 10.1378/chest.94.6.1200 [DOI] [PubMed] [Google Scholar]
- 19.Ramar K, Dort LC, Katz SG, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med 2015;11:773-827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collard P, Pieters T, Aubert G, et al. Compliance with nasal CPAP in obstructive sleep apnea patients. Sleep Med Rev 1997;1:33-44. 10.1016/S1087-0792(97)90004-6 [DOI] [PubMed] [Google Scholar]
- 21.Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath 2010;14:323-35. 10.1007/s11325-010-0391-y [DOI] [PubMed] [Google Scholar]
- 22.Jonas DE, Amick HR, Feltner C, et al. Screening for Obstructive Sleep Apnea in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2017;317:415-33. 10.1001/jama.2016.19635 [DOI] [PubMed] [Google Scholar]
- 23.Shi YW, Wang GF, Zhang C, et al. Application Value of Epworth Sleepiness Scale in the Screening of Obstructive Sleep Apnea Hypopnea Syndrome. Chinese Journal of Respiratory & Critical Care Medicine 2009;8:456-60. [Google Scholar]
- 24.Weaver EM, Kapur V, Yueh B. Polysomnography vs. self-reported measures in patients with sleep apnea. Arch Otolaryngol Head Neck Surg 2004;130:453-8. 10.1001/archotol.130.4.453 [DOI] [PubMed] [Google Scholar]
- 25.Wells RD, Day RC, Carney RM, et al. Depression predicts self-reported sleep quality in patients with obstructive sleep apnea. Psychosom Med 2004;66:692-7. 10.1097/01.psy.0000140002.84288.e1 [DOI] [PubMed] [Google Scholar]
- 26.Peters T, Grüner C, Durst W, et al. Sleepiness in professional truck drivers measured with an objective alertness test during routine traffic controls. Int Arch Occup Environ Health 2014;87:881-8. 10.1007/s00420-014-0929-6 [DOI] [PubMed] [Google Scholar]
- 27.Arnardottir ES, Bjornsdottir E, Olafsdottir KA, et al. Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J 2016;47:194-202. 10.1183/13993003.01148-2015 [DOI] [PubMed] [Google Scholar]
- 28.Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2013;187:879-87. 10.1164/rccm.201212-2223OC [DOI] [PubMed] [Google Scholar]
- 29.Qaseem A, Holty JE, Owens DK, et al. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American College of Physicians. Ann Intern Med 2013;159:471-83. 10.7326/0003-4819-159-11-201312030-00009 [DOI] [PubMed] [Google Scholar]
- 30.Capasso R, Kezirian E, Jacobowitz O, et al. Management of obstructive sleep apnea in adults. Ann Intern Med 2014;160:367. 10.7326/L14-5005 [DOI] [PubMed] [Google Scholar]
- 31.Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, et al. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med 2012;156:115-22. 10.7326/0003-4819-156-2-201201170-00006 [DOI] [PubMed] [Google Scholar]
- 32.Kapur V, Strohl KP, Redline S, et al. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath 2002;6:49-54. 10.1055/s-2002-32318 [DOI] [PubMed] [Google Scholar]